Published online Jul 16, 2024. doi: 10.4253/wjge.v16.i7.424
Revised: May 14, 2024
Accepted: May 27, 2024
Published online: July 16, 2024
Processing time: 83 Days and 12.6 Hours
Video-capsule endoscopy (VCE) is an efficient tool that has proven to be highly useful in approaching several gastrointestinal diseases. VCE was implemented in Colombia in 2003, however current characterization of patients undergoing VCE in Colombia is limited, and mainly comes from two investigations conducted before the SARS-CoV-2 pandemic period.
To describe the characteristics of patients undergoing VCEs and establish the main indications, findings, technical limitations, and other outstanding features.
A descriptive study was carried out using data from reports of VCE (PillCam SB3 system) use in a Gastroenterology Unit in Bogotá, Colombia between September 2019 and January 2023. Demographic and clinical variables such as indication for the VCE, gastric and small bowel transit times (GTT, SBTT), endoscopic prepara
A total of 133 VCE reports were analyzed. Most were in men with a median age of 70 years. The majority had good preparation (96.2%), and there were technical limitations in 15.8% of cases. The main indications were unexplained anemia (91%) or occult bleeding (23.3%). The median GTT and SBTT were 14 and 30 minutes, respectively. The frequencies of bleeding stigma (3.79%) and active bleeding (9.09%) were low, and the most frequent abnormal findings were red spots (28.3%), erosions (17.6%), and vascular ectasias (12.5%).
VCE showed high-level safety. The main indication was unexplained anemia. Active bleeding was the most frequent finding. Combined with artificial intelligence, VCE can improve diagnostic precision and targeted therapeutic interventions.
Core Tip: Video-capsule endoscopy (VCE) has proven to be a highly useful and efficient diagnostic tool, not only for obscure and occult bleeding, but also for small bowel diseases. VCE was implemented in Colombia in 2003. However, the current characterization of patients undergoing VCE in Colombia is limited. This research could be useful in promoting the training and use of VCEs as a diagnostic tool, and potentially, as an intervention coadjutant in developing countries.
- Citation: Mejía MC, Piñeros LG, Pombo LM, León LA, Velásquez JA, Teherán AA, Ayala KP. Clinical and demographic features of patients undergoing video-capsule endoscopy management: A descriptive study. World J Gastrointest Endosc 2024; 16(7): 424-431
- URL: https://www.wjgnet.com/1948-5190/full/v16/i7/424.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i7.424
In the general population, the incidence of gastrointestinal bleeding (GIB) is 2.1 per 1000 person-years [95% confidence interval (CI): 1.96-2.25], with 75% of cases occurring in the upper gastrointestinal tract[1,2]. GIB may be overt, obscure, or occult, and in the first two scenarios, video-capsule endoscopy (VCE) has proven to be highly useful and an efficient diagnostic tool[3-5].
Compared to other invasive and noninvasive diagnostic procedures, VCE has demonstrated superiority in user satisfaction and comfort, low complication rates, and improved diagnostic efficiency. It should be noted that, for this procedure, efficiency is influenced by adequate intestinal preparation and the clinical indication[6-9].
VCE is indicated in patients with GIB or small bowel digestive problems, including unexplained iron-deficiency anemia, polyposis syndromes, intestinal malabsorption, suspicion of neoplastic disease, and in the follow-up of small intestine transplantation[4]. In addition, it is indicated in patients with evident bleeding and negative results on conventional endoscopy or colonoscopy or problems originating in the colon, such as inflammatory bowel disease, polyposis and other neoplasms, celiac disease, among others[5,10].
In Colombia, in the 5 years between 2015 and 2019 prior to the SARS-CoV-2 pandemic, visits for inflammatory and polyposis intestinal diseases (ICD-10: K50-K52) increased by 3.47 times (year 2015: 3981 visits, year 2019: 13827 visits). Despite the observed and expected decrease during 2020 owing to social restrictions during the pandemic (7517 visits), the visits increased by 1.51 times between 2020 and 2022[11].
VCE was implemented in Colombia in 2003 and, similar to what has been established in other studies, it proved to be useful in the diagnostic approach of patients with obscure GIB, occult obscure GIB, and manifest obscure GIB[12,13]. However, the current characterization of patients undergoing VCE in Colombia is limited and mainly comes from two investigations conducted before the SARS-CoV-2 pandemic period.
The aim of this research was to describe the demographic and clinical characteristics of the adult population undergoing VCE (PillCam SB3 system) between the last trimester of 2019 and the first trimester of 2023, in a Gastroenterology Unit in Bogotá and identify the main indications, described findings, technical limitations, and other relevant characteristics were established.
A descriptive retrospective study was carried out using data from reports of VCEs performed on patients who attended the gastroenterology unit of the Hospital Universitario Clínica San Rafael between September 2019 and January 2023. The digital file of the PillCam SB3 system contains a series of images for each endoscopic record, which were read and reported in a standard format by gastroenterologists. The study data were extracted from those reports, and an anonymized database was created. Therefore, this study was classified as low risk according to the local ethical regulations in force.
Demographic variables (age, sex) and clinical variables such as indications for performing the VCEs (unexplained anemia, occult bleeding, Crohn’s disease), gastric and small bowel transit times (GTT, SBTT), quality of endoscopic preparation, and the presence of VCEs with limited results were described. Additionally, endoscopic findings and the frequency of VCEs with suggestive findings (stigmata, active bleeding) were assessed.
Quantitative data were reported as median (IQR) and qualitative data as count and proportion (RStudio 2022.07.2) (ref GitHub). Data were described independently for patients with normal and abnormal VCE results. The chi-square test for independence or the Fisher's exact test was used to determine the significance of the association between normal and abnormal results with tests classified as limited, and between the indication for VCEs and the types of bleeding observed (stigmata vs active bleeding) (JASP Team (2022), Version 0.16.4, computer software). Forest, heatmap, and boxplot graphs were drawn to describe the frequency of abnormal findings in VCEs (RStudio 2022.07.2; JASP Team (2022), Version 0.16.4, computer software).
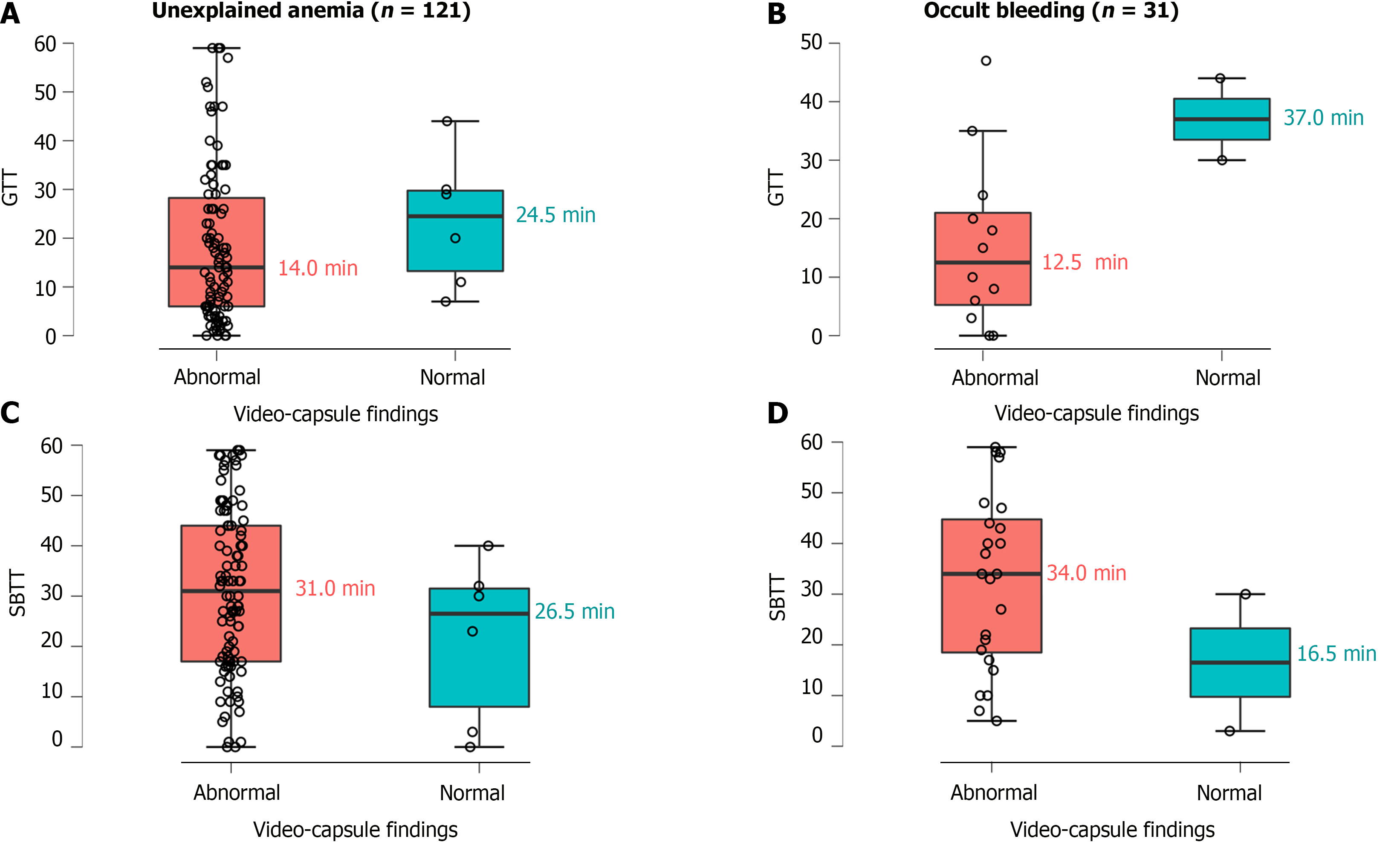
During the study period, 133 cases of VCEs were identified, primarily indicated by unexplained anemia. Approximately 95% of the VCEs revealed abnormal findings and were predominantly observed in males or patients with a median age of 74 years (minimum: 19 years, maximum: 93 years). In half of the reports, the median GTT was 14 min and the median SBTT was 30 min. However, in patients with abnormal findings, the median GTT was lower and the median SBTT was higher than in those with normal findings (Table 1). Additionally, it was observed that patients with unexplained anemia or occult bleeding who had abnormal findings also had lower median GTT and higher median SBTT values (Figure 1).
| Variables | Normal findings, n of 7 (5.26%) | Abnormal findings, n of 126 (94.7%) | Overall, n of 133 |
| Age1 in yr | 70.0 (53.5-77.5) | 74.5 (61.4-81.6) | 73.9 (61.2-81.7) |
| Sex | |||
| Male | 2 (28.6) | 70 (55.6) | 72 (54.1) |
| Female | 5 (71.4) | 56 (44.4) | 61 (45.9) |
| Indications | |||
| Unexplained anemia | 7 (100) | 114 (90.5) | 121 (91.0) |
| Occult bleeding | 3 (42.9) | 28 (22.8) | 31 (23.3) |
| Crohn’s disease | 0 (0.0) | 1 (0.8) | 1 (0.75) |
| GTT1 in min | 24.5 (13.2-29.7) | 13.0 (5.5-26.0) | 14 (6-29) |
| SBTT1 in min | 26.5 (8.0-31.5) | 30.0 (17.0-44.2) | 30 (17-44) |
| Patient preparation | |||
| Good | 7 (100) | 121 (96.0) | 128 (96.2) |
| Deficient | 0 (0.0) | 5 (4.0) | 5 (3.8) |
| Limited test | 2 (28.6) | 19 (15.1) | 21 (15.8) |
| Bleeding stigmata | 0 (0.0) | 5 (4.08) | 5 (3.79) |
| Active bleeding | 0 (0.0) | 12 (9.05) | 12 (9.09) |
Signs of bleeding stigmata were identified in fewer than 5% of VCE reports, and active bleeding was observed in fewer than 10% (Table 1). On the other hand, the frequencies of bleeding stigmata and active bleeding were higher in patients with unexplained anemia (Table 2). However, the differences between the frequency of unexplained anemia and the frequency of bleeding stigmata (P = 0.065) or active bleeding (P = 0.334) were not significant were not significant (chi-square; Fisher exact test). Likewise, differences in the frequency of occult bleeding and the frequency of bleeding signs (P = 1) or active bleeding were not significant (Fisher’s exact test, Table 2). The median number of abnormal findings per patient was 3 (2-4) and ranged from 0 to 6. It is noteworthy that the median age in patients without abnormal findings was lower than in patients with abnormal findings (70 years vs 75 years of age).
| Variable | Bleeding stigmata, n of 5 (%) | Active bleeding, n of 12 (%) | P value |
| Occult bleeding | 2 (40.0) | 1 (8.3) | 0.382 |
| Unexplained anemia | 3 (60.0) | 11 (91.7) |
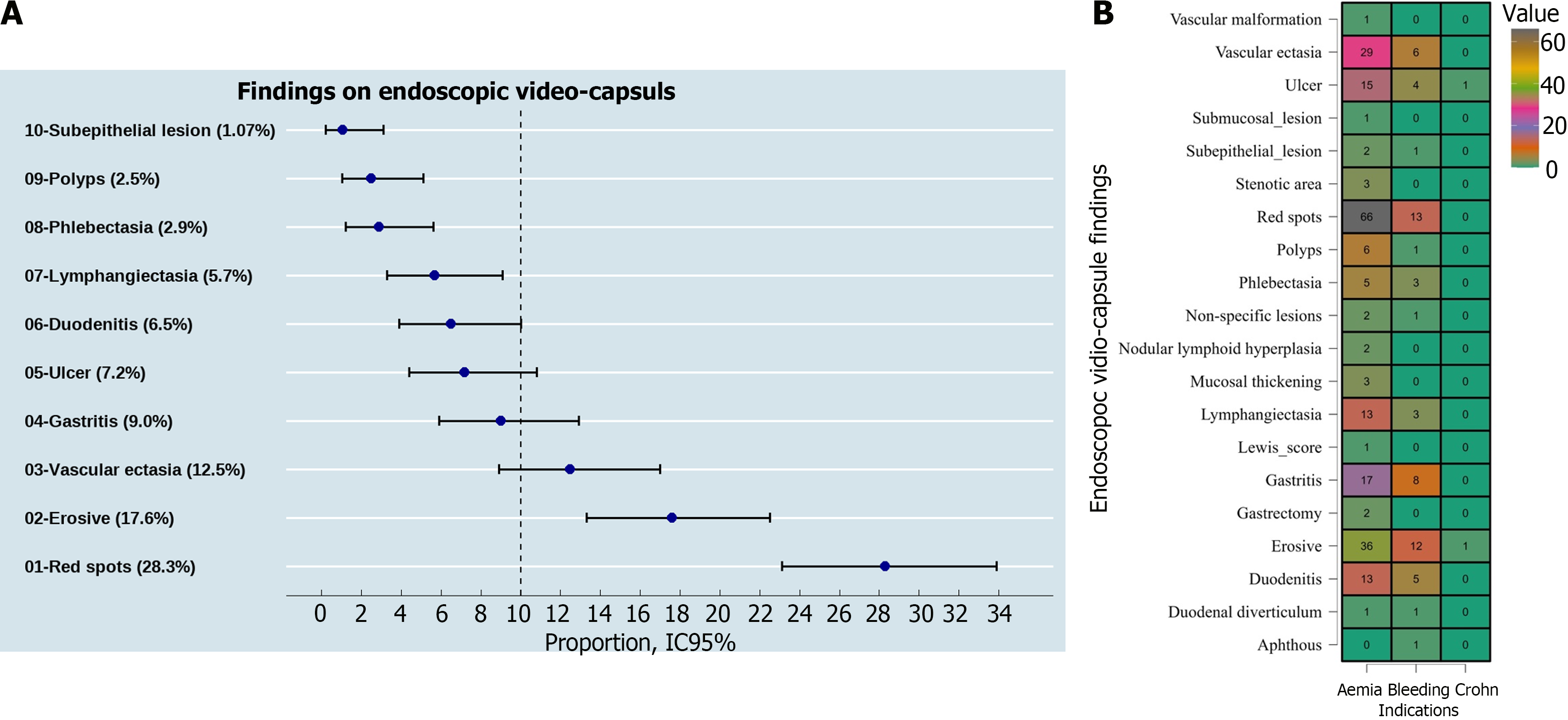
Figure 2 shows the most frequently identified abnormal findings in the VCE reports. At least one out of every ten reports showed red spots, erosions, and vascular ectasias. In addition, subepithelial lesions and polyps were the least frequent among the top 10 endoscopic findings (Figure 2A). When classified by the indication of the VCE, a similar distribution was observed for the three main findings (Figure 2B).
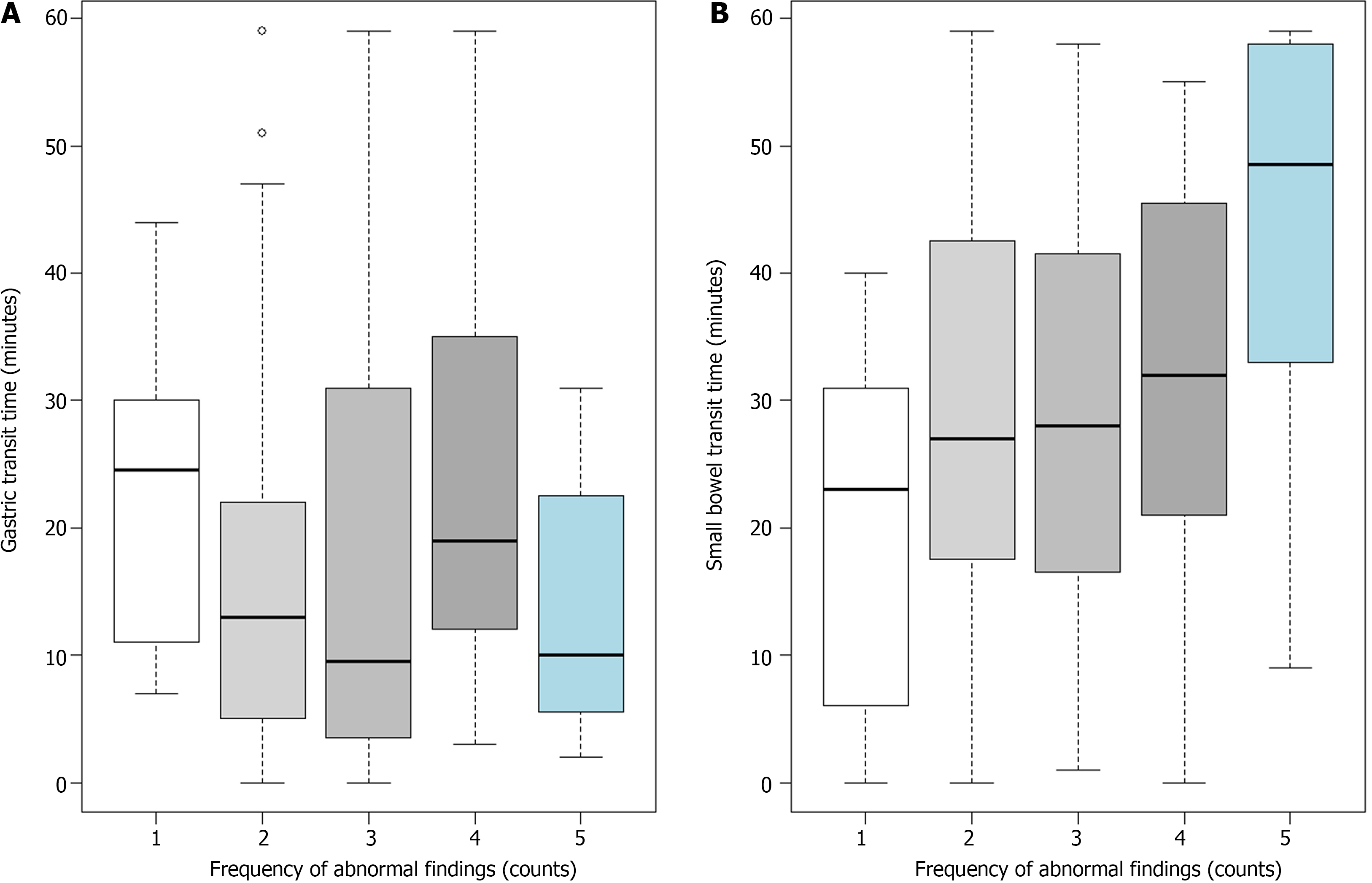
Finally, Figure 3 shows the relationship between the number of abnormal findings observed in the VCE (X-axis) and the GTT or SBTT (Y-axis). A potential inverse relationship between the number of abnormal findings and the median GTT was observed. The median GTT in patients without abnormal findings was 24.5 min. In patients with 1-3 abnormal findings, it was 9.5 to 19 min. In patients with 4-6 abnormal findings, it was 10 min. On the other hand, a potential direct relationship was observed between the number of abnormal findings and the median SBTT. The median GTT in patients without abnormal findings was 23 min. In patients with 1-3 abnormal findings, it was 27-32 minutes. In patients with 4-6 abnormal findings, it was 48.5 min.
In this descriptive study, the demographic and clinical features (indications, findings, complications) of patients undergoing VCEs were described in a gastroenterology unit of a level IV complexity hospital in Bogotá. Most patients included in this study(91%, data not shown) attended after the year 2019, during the pandemic, or in post-pandemic period by SARS-CoV-2. The gastroenterology unit routinely performs 20 procedures per day, and approximately 400 procedures per month, distributed according to clinical indication and therapeutic limitations. It is worth mentioning that VCE accounts for 10%-15% of all procedures (40-60/mo), and in 2020-2022, the frequency decreased to 27-55 VCEs per year. VCE is a commonly used method to evaluate the small bowel, allowing detailed and minimally invasive visualization of its mucosal surface in the gastrointestinal tract[14]. Indications for VCE have also been extended to the diagnostic approach of BID and colorectal neoplasia. Over time, image resolution, diagnostic performance, safety, and patient comfort have improved[5,10,14].
A systematic review of 24 studies that included a total of 1960 patients determined that in studies including only patients with iron-deficiency anemia, the detection rate of VCE was 66.6% (95%CI: 61.0-72.3)[15]. In our series, at least 92% of the patients with abnormal findings (red spots, vascular ectasias, erosions, among others) had a diagnosis of unexplained anemia or occult bleeding as VCE indications. Possibly, the median age and morbidity of our patient population explain the frequency of abnormal findings. Angiectasias can be documented in 30%-60% of those over 40-years-old, followed by findings associated with NSAIDs enteropathies, celiac disease, and tumors, among others. It is worth noting that in Stone et al[17], the mean age of the patient series (62.9 years) was lower than ours, and patients with Crohn's disease, manifest and obscure GIB were excluded[5,16,17].
Subepithelial lesions and polyps were observed among the top 10 endoscopic findings of this series,. However, according to the demographic and clinical characteristics of the series, Cameron erosions, fundic varices, peptic ulcers, Dieulafoy's lesion, neoplasms, Meckel's diverticulum, and Crohn's disease can be identified. These findings integrate a group of etiologies not previously visualized in other endoscopic studies, which may explain upper and lower GIB[4,5,10,16]. To describe endoscopic findings, the internationally established terminology of the consensus of nomenclature and description of the most common vascular lesions (red spots, phlebectasia, angiectasia, vascular ectasia, other findings) was used. However, it should be made clear that most of the descriptions made in this series were subjective and conditioned by the observers' experience[18].
Time to completion of VCE is an important consideration. Guidelines suggest that the procedure be performed 24-72 h after the onset of bleeding, even in hospitalized patients. It should be noted that critically ill patients may have a longer transit time, a factor that increases the rate of incomplete results[19,20]. Our study included both outpatient and hospitalized patients. However, the lack of complete medical histories and information from hospital record data, as well as information about previous endoscopic studies such as upper gastrointestinal endoscopy, colonoscopy, and others, are study limitations.
Currently, real-time viewers are incorporated into several VCE systems. In 97% to 100% of healthy individuals, capsule transit through the stomach occurs 4 h after ingestion; However, patients with renal disease, hypothyroidism, or diabetic gastropathy, who consume psychotropic or narcotic drugs, have some degree of retention and benefit from real-time monitoring as a preventive measure to intervene in case of retention[21].
In this study, the median GTT was 24 min in patients with normal findings and 13 min in those. with some type of lesion, similar to what has been described in literature. Capsule retention was not recorded, but transit alteration as it goes through from the esophagus to the gastric cavity was documented, so endoscopy equipment was advanced to the gastric cavity, hence the importance of continuous monitoring. This establishes the relevance of chronic NSAID consumption, constitutional symptoms, bleeding window, and diseases such as diabetes, hiatal hernias, or neoplasms that alter transit and affect the diagnostic performance of VCE.
In this study of 133 VCEs, the majority were performed in men over 65-years-old, the main indication was unexplained anemia, the most frequent findings were active bleeding, red spots, erosions, and vascular ectasias, and the least frequent were subepithelial lesions and polyps. VCE has emerged as a high-performance diagnostic and safe tool. It has become the gold standard for diagnosing small bowel diseases, and the spectrum of this noninvasive technology has reached the entire gastrointestinal tract. Its main indications are related to the study of anemia and obscure GIB, as well as for monitoring patients with Crohn's disease. These technological advances have been developed to improve patient safety and comfort. In the future, along with artificial intelligence, they will be useful to diagnose, treat, or perform specific therapeutic interventions.
We thank to Research Center of the Fundación Universitaria Juan N. Corpas for methodological and technical assistance.
| 1. | Vora P, Pietila A, Peltonen M, Brobert G, Salomaa V. Thirty-Year Incidence and Mortality Trends in Upper and Lower Gastrointestinal Bleeding in Finland. JAMA Netw Open. 2020;3:e2020172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Antunes C, Copelin II EL. Upper Gastrointestinal Bleeding. Updated 2023 Apr 7. Treasure Island (FL): StatPearls Publishing, 2023. |
| 3. | Ohmiya N. Management of obscure gastrointestinal bleeding: Comparison of guidelines between Japan and other countries. Dig Endosc. 2020;32:204-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Akyüz F, Ersoy O, Erzin Y, Çavuş B, Bakkaloğlu O, Akın E, Kav T, Akyüz Ü, Pata C. Small Bowel Video Capsule Endoscopy Guidance in Practice: Expert Opinion Report. Turk J Gastroenterol. 2023;34:2-19. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Koulaouzidis A, Baatrup G. Current status of colon capsule endoscopy in clinical practice. Nat Rev Gastroenterol Hepatol. 2023;20:557-558. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Tamilarasan AG, Tran Y, Paramsothy S, Leong R. The diagnostic yield of pan-enteric capsule endoscopy in inflammatory bowel disease: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2022;37:2207-2216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 7. | Mi J, Han X, Wang R, Ma R, Zhao D. Diagnostic Accuracy of Wireless Capsule Endoscopy in Polyp Recognition Using Deep Learning: A Meta-Analysis. Int J Clin Pract. 2022;2022:9338139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Sulbaran M, Bustamante-Lopez L, Bernardo W, Sakai CM, Sakai P, Nahas S, Moura EGH. Systematic review and meta-analysis of colon capsule endoscopy accuracy for colorectal cancer screening. An alternative during the Covid-19 pandemic? J Med Screen. 2022;29:148-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Bang CS, Lee JJ, Baik GH. Computer-Aided Diagnosis of Gastrointestinal Ulcer and Hemorrhage Using Wireless Capsule Endoscopy: Systematic Review and Diagnostic Test Accuracy Meta-analysis. J Med Internet Res. 2021;23:e33267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Enns RA, Hookey L, Armstrong D, Bernstein CN, Heitman SJ, Teshima C, Leontiadis GI, Tse F, Sadowski D. Clinical Practice Guidelines for the Use of Video Capsule Endoscopy. Gastroenterology. 2017;152:497-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 281] [Article Influence: 35.1] [Reference Citation Analysis (0)] |
| 11. | Sistema Integrado de Información de la Protección Social. Base de datos en internet. [cited 18 Jan 2023]. In: Bogotá-Colombia: SISPRO [Internet]. Available from: https://www.sispro.gov.co/Pages/Home.asp. |
| 12. | Galiano MT, Sánchez-Arciniegas F, Pineda-Ovalle LF. Clinical experience of using the video capsule endoscopy (VCE) as a diagnostic method in small intestine pathology. Rev Col Gastroenterol. 2009;24:17-25. |
| 13. | Juliao-Baños F, Galiano MT, Camargo J, Mosquera-Klinger G, Carvajal J, Jaramillo C, Sabbagh L, Cure H, García F, Velasco B, Manrique C, Parra V, Flórez C, Bareño J. Clinical utility of the small bowel capsule endoscopy in the study of small bowel diseases in Colombia: Results of a national registry. Gastroenterol Hepatol. 2021;44:346-354. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Melson J, Trikudanathan G, Abu Dayyeh BK, Bhutani MS, Chandrasekhara V, Jirapinyo P, Krishnan K, Kumta NA, Pannala R, Parsi MA, Sethi A, Trindade AJ, Watson RR, Maple JT, Lichtenstein DR. Video capsule endoscopy. Gastrointest Endosc. 2021;93:784-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Koulaouzidis A, Rondonotti E, Giannakou A, Plevris JN. Diagnostic yield of small-bowel capsule endoscopy in patients with iron-deficiency anemia: a systematic review. Gastrointest Endosc. 2012;76:983-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 16. | Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110:1265-87; quiz 1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 447] [Article Influence: 44.7] [Reference Citation Analysis (1)] |
| 17. | Stone J, Grover K, Bernstein CN. The Use of Capsule Endoscopy For Diagnosis of Iron Deficiency Anemia: A Retrospective Analysis. J Clin Gastroenterol. 2020;54:452-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Leenhardt R, Li C, Koulaouzidis A, Cavallaro F, Cholet F, Eliakim R, Fernandez-Urien I, Kopylov U, McAlindon M, Németh A, Plevris JN, Rahmi G, Rondonotti E, Saurin JC, Tontini GE, Toth E, Yung D, Marteau P, Dray X. Nomenclature and semantic description of vascular lesions in small bowel capsule endoscopy: an international Delphi consensus statement. Endosc Int Open. 2019;7:E372-E379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 19. | O'Grady J, Murphy CL, Barry L, Shanahan F, Buckley M. Defining gastrointestinal transit time using video capsule endoscopy: a study of healthy subjects. Endosc Int Open. 2020;8:E396-E400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 20. | Mohan N, Jarrett S, Pop A, Rodriguez D, Dudnick R. Effect of small bowel transit time on accuracy of video capsule endoscopy in evaluating suspected small bowel bleeding. World J Gastrointest Pharmacol Ther. 2022;13:88-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Pennazio M, Rondonotti E, Despott EJ, Dray X, Keuchel M, Moreels T, Sanders DS, Spada C, Carretero C, Cortegoso Valdivia P, Elli L, Fuccio L, Gonzalez Suarez B, Koulaouzidis A, Kunovsky L, McNamara D, Neumann H, Perez-Cuadrado-Martinez E, Perez-Cuadrado-Robles E, Piccirelli S, Rosa B, Saurin JC, Sidhu R, Tacheci I, Vlachou E, Triantafyllou K. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2022. Endoscopy. 2023;55:58-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 150] [Article Influence: 75.0] [Reference Citation Analysis (0)] |