Published online Jun 16, 2024. doi: 10.4253/wjge.v16.i6.350
Revised: April 25, 2024
Accepted: May 10, 2024
Published online: June 16, 2024
Processing time: 109 Days and 11.3 Hours
Elective cholecystectomy (CCY) is recommended for patients with gallstone-related acute cholangitis (AC) following endoscopic decompression to prevent recurrent biliary events. However, the optimal timing and implications of CCY remain unclear.
To examine the impact of same-admission CCY compared to interval CCY on patients with gallstone-related AC using the National Readmission Database (NRD).
We queried the NRD to identify all gallstone-related AC hospitalizations in adult patients with and without the same admission CCY between 2016 and 2020. Our primary outcome was all-cause 30-d readmission rates, and secondary outcomes included in-hospital mortality, length of stay (LOS), and hospitalization cost.
Among the 124964 gallstone-related AC hospitalizations, only 14.67% underwent the same admission CCY. The all-cause 30-d readmissions in the same admission CCY group were almost half that of the non-CCY group (5.56% vs 11.50%). Patients in the same admission CCY group had a longer mean LOS and higher hospitalization costs attributable to surgery. Although the most common reason for readmission was sepsis in both groups, the second most common reason was AC in the interval CCY group.
Our study suggests that patients with gallstone-related AC who do not undergo the same admission CCY have twice the risk of readmission compared to those who undergo CCY during the same admission. These readmis
Core Tip: Utilizing the National Readmission Database, we examined the outcomes of index admission cholecystectomy (CCY) vs interval CCY in patients with gallstone-related acute cholangitis (AC). This study revealed that patients undergoing CCY during the same hospital admission for AC exhibited significantly lower 30-d readmission rates than those receiving interval CCY. This approach not only reduces the frequency of subsequent acute hospital visits but also highlights the potential cost benefits by lowering hospitalization expenses. These findings advocate for a reevaluation of current clinical practices concerning the timing of CCY post- endoscopic retrograde cholangiopancreatography, suggesting that earlier interventions could enhance patient outcomes and optimize resource utilization.
- Citation: Sohail A, Shehadah A, Chaudhary A, Naseem K, Iqbal A, Khan A, Singh S. Impact of index admission cholecystectomy vs interval cholecystectomy on readmission rate in acute cholangitis: National Readmission Database survey. World J Gastrointest Endosc 2024; 16(6): 350-360
- URL: https://www.wjgnet.com/1948-5190/full/v16/i6/350.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i6.350
Gallstone-related acute cholangitis (AC) is a common gastrointestinal emergency that requires prompt recognition and treatment to prevent multi-organ failure and irreversible shock. The most common etiology of AC is biliary obstruction secondary to gallstones, accounting for up to 70% of the cases[1]. The majority of these patients require endoscopic retrograde cholangiopancreatography (ERCP) for biliary decompression. The estimated mortality rate following an acute episode of AC ranges from 5%-10%, with higher rates observed in patients who require emergent ERCP[2]. Despite successful decompression of the biliary tract after an ERCP, there is a risk of recurrent biliary events due to the presence or formation of stones in the gallbladder, which can lead to recurrent cholangitis, rehospitalizations, and increased mortality[1,3,4]. Therefore, elective cholecystectomy (CCY) is recommended in these patients after an ERCP, but there is a lack of consensus about the optimal timings of CCY[3,4].
The 2007 Tokyo guidelines recommend elective CCY after successful biliary decompression in stable patients with AC (Grade B recommendation)[5]. However, no updates were made in the 2013 or 2018 guidelines to address the timing of the elective CCY and whether it needs to be performed during the same admission or interval admission[1,6]. Similarly, the European Society of Gastrointestinal Endoscopy 2019 guidelines also endorse the Tokyo 2018 guidelines and do not provide any specific timeframe regarding CCY after AC[7]. However, the American Society of Gastrointestinal Endoscopy recommends that elective CCY be performed as soon as possible after the resolution of AC, but the timing should be individualized based on the patient’s condition and other factors. Therefore, the time to perform elective CCY in these patients remains highly discretionary to the performing surgeon and depends on perioperative risk assessment at the individual level[8]. Although studies have shown that early elective CCY during the same hospitalization after therapeutic ERCP in patients with AC can decrease the risk of recurrent biliary events by 15%-20%[9-11]. It is estimated that the same admission elective CCY following an ERCP is performed only in 28.6% to 37.2% of patients who present with choledocholithiasis[12,13]. Hence, there remains a lack of consensus on the optimal timing of CCY after ERCP in patients with an acute episode of gallstone-related AC. Therefore, we aimed to examine the impact of the same admission CCY after an ERCP on readmission rate, mortality, and resource utilization in patients with gallstone-related AC at a national level.
In this study, we utilized the National Readmission Database (NRD), which is a part of the Healthcare Cost and Utilization Project (HCUP), as our data source. The NRD is the largest publicly available readmission database in the United States, covering approximately 32 million hospital discharges across geographically dispersed 31 states[14]. It provides clinical and demographic data, including patient and hospital-level information related to index hospitalization and readmissions. The patient-level data includes demographics such as gender, age, median income by zip quartile, primary and secondary diagnoses at discharge, procedures performed during the hospitalization, length of stay (LOS), and total hospitalization charges, and the hospital-level data includes information about ownership, teaching status, hospital size based on the number of beds, and rural/urban location. The NRD allocates a specific identification number to each patient, which is used to identify all admissions (index or readmissions) for that patient in a calendar year. The discharge diagnoses and procedure codes are identified using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD10-CM), and Procedure Coding System (PCS). The study is considered exempt from the institutional review board, as the data source is from the NRD, a publicly available de-identified database.
We identified all patients hospitalized for gallstone-related AC in the NRD between 2016 and 2020. We grouped them into two cohorts based on whether they underwent the same admission CCY or interval CCY following biliary decompression with an ERCP. Patients who did not undergo index hospitalization for CCY after AC were assumed to have later undergone CCY. The ICD-10 and PCS codes used to select patients are provided in the Supplementary Table 1. Patients under 18 years of age and those admitted on an elective basis were excluded from the study. All the index hospitalizations in December were also excluded to accurately calculate the 30-d readmission rate as NRD keeps a calendar year hospitalization record from January 1 to December 31 without crossing over to the previous or the following year.
The primary outcome of our study was the all-cause 30-d readmission rate for patients admitted with gallstone-related AC and the most common reasons leading to these readmissions. Readmission was defined as any non-traumatic admission within 30 d of the index admission, and only the first readmission was considered for patients with multiple readmissions. We excluded patients who died during index hospitalization to calculate readmission outcomes accurately. Our secondary outcomes were all-cause mortality for the index hospitalization and readmissions, along with the mean LOS and hospitalization costs associated with the index hospitalization and subsequent readmissions.
The database itself has patient-related variables such as age, gender, median household income based on zip code, primary insurance payer (including Medicare, Medicaid, private insurance, self-pay, and uninsured status) as well as hospital characteristics such as size based on the number of beds (large, medium, and small), urban vs rural location, and teaching status. To assess the burden of comorbidities in both groups, including hypertension, diabetes mellitus, chronic kidney disease, end-stage renal disease (ESRD), chronic obstructive pulmonary disease (COPD), and congestive heart failure (CHF), we utilized the variables present in the Deyo’s modification of Charlson Comorbidity Index (CCI)[15]. The NRD provides information about the total hospitalization charges that hospitals bill for each hospitalization. However, the total hospitalization cost reimbursed by the primary payer is calculated using the cost-to-charge ratio files provided by the HCUP[16].
We used STATA (version 16.0; StataCorp, College Station, TX, United States) for statistical analysis, which allows statistical operations involving complex survey-based studies aligned with the NRD design, including stratification, clustering, and weighing. We dealt with the missing values by pairwise deletion. Baseline demographics were compared using the χ2 test for categorical variables and Student’s t-test for continuous variables. We set the threshold for statistical significance at a P value of 0.05. Survival analysis was performed with the time from discharge to readmission as a time variable and death as a failure. Patients were censored on the 30th d of discharge if they were alive. Univariate Cox regression analysis was used to calculate the unadjusted hazard ratio (HR) for the predictors of readmissions. A multivariate Cox regression model was built to adjust for potential confounding factors with a cutoff P value of less than 0.2 on univariate analysis.
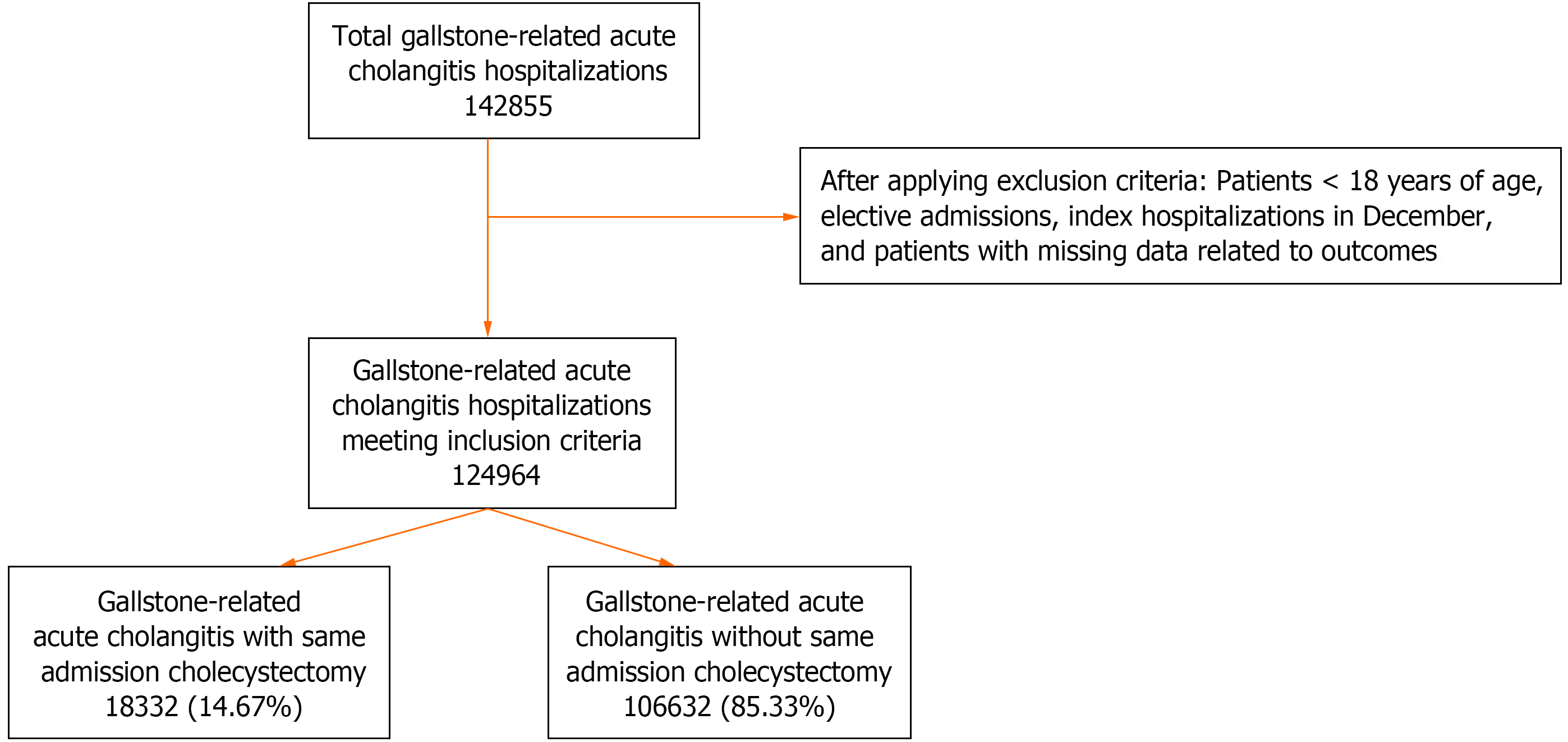
In this study, 142855 hospitalizations were initially identified in patients with gallstone-related AC between 2016 and 2020. After applying the study criteria, 124964 patients were included in the analysis (Figure 1). Table 1 presents the baseline characteristics of the patients and hospitals for index hospitalization and 30-d readmission. Only 18332 (14.67%) of the included patients underwent the same admission CCY following an ERCP. Patients who received the same admission CCY were younger, with a mean age of 66.89 years, compared to those who received interval-CCY (mean age 69.89 years, P < 0.01), and had a higher proportion of male patients (52.94% vs 51.52%, P < 0.01). Patients who underwent interval-CCY had a higher CCI score of > 3 (45.85% vs 27.10%, P < 0.01) than those in the same admission CCY group. Patients in the interval-CCY group also had a higher prevalence of individual comorbidities, such as COPD (18.2% vs 17.83%, P < 0.01), ESRD (2.2% vs 1.6%, P < 0.01), and CHF (16.97% vs 13.33%, P < 0.1), than those who received the same admission CCY. Medicare was the primary insurer in both the same admission CCY and interval-CCY groups (64.54% vs 61.12%, respectively), followed by private insurance (22.74% vs 19.99%, respectively). More than two-thirds of the patients who received the same admission CCY were admitted to the teaching hospitals (77.36%) (Table 1).
| Patient characteristics | AC with same admission CCY | AC with interval CCY | ||||
| Index admission | 30-d readmission | P value | Index admission | 30-d readmission | P value | |
| No. of patients (n) | 18332 | 1019 | 106632 | 12265 | ||
| Male, n (%) | 9704 (52.94) | 534 (52.37) | 0.82 | 54937 (51.52) | 6787 (55.34) | < 0.01 |
| Mean age (yr) | 66.9 | 68.28 | 69.89 | 69.08 | ||
| Charlson Comorbidity Index | < 0.01 | < 0.01 | ||||
| 0 | 6205 (33.85%) | 268 (26.33%) | 22862 (21.44%) | 1748 (14.25%) | ||
| 1 | 3668 (20.01%) | 124 (12.2%) | 15003 (14.07%) | 1326 (10.81%) | ||
| 2 | 3487 (19.02%) | 165 (16.23%) | 19866 (18.63%) | 2177 (17.75%) | ||
| 3 or more | 4968 (27.10%) | 461 (45.22%) | 48891 (45.85%) | 7013 (57.18%) | ||
| Median income based on Zip codes | 0.89 | 0.03 | ||||
| $1-$38999 | 4498 (24.54%) | 252 (24.75%) | 24078 (22.58%) | 2807 (22.89%) | ||
| $39000-$47999 | 5316 (29%) | 299 (29.38%) | 29782 (27.93%) | 3258 (26.56%) | ||
| $48000-$62999 | 4810 (26.24%) | 277 (27.22%) | 27575 (25.86%) | 3097 (25.25%) | ||
| > $ 63000 | 3703 (20.2%) | 190 (18.64%) | 25186 (23.62%) | 3101 (25.28%) | ||
| Primary payer, n (%) | 0.05 | 0.12 | ||||
| Medicare | 11831 (64.54) | 727 (71.34) | 73704 (69.12) | 8372 (68.26) | ||
| Medicaid | 1727 (9.42) | 88 (8.68) | 9458 (8.87) | 1208 (9.85) | ||
| Private | 4168 (22.74) | 174 (17.03) | 21316 (19.99) | 2452 (19.99) | ||
| Others | 601 (3.28) | 30 (2.94) | 2133 (2) | 231 (1.88) | ||
| Comorbid conditions | ||||||
| Hypertension | 7272 (39.67%) | 461 (45.23%) | < 0.01 | 41640 (39.05%) | 4706 (38.37%) | 0.34 |
| Diabetes mellitus | 2576 (14.05%) | 220 (21.62%) | < 0.01 | 15622 (14.65%) | 1859 (15.16%) | 0.36 |
| End stage renal disease | 295 (1.61%) | 38 (3.69%) | < 0.01 | 2346 (2.2%) | 438 (3.57%) | < 0.01 |
| Chronic obstructive pulmonary disease | 3269 (17.83%) | 227 (22.31%) | < 0.01 | 19407 (18.2%) | 2395 (19.53%) | 0.03 |
| Congestive heart failure | 2444 (13.33%) | 284 (27.84%) | < 0.01 | 18095 (16.97%) | 2495 (20.34%) | < 0.01 |
| Nicotine dependence | 4739 (25.85%) | 320 (31.38%) | < 0.01 | 28034 (26.29%) | 3383 (27.58%) | 0.04 |
| Alcohol dependence | 326 (1.78%) | 11 (1.08%) | < 0.01 | 1749 (1.64%) | 156 (1.27%) | 0.04 |
| Hospital characteristics | ||||||
| Hospital teaching status | < 0.01 | 0.10 | ||||
| Non-teaching | 4148 (22.63%) | 288 (28.31%) | 17754 (16.65%) | 2150 (17.53%) | ||
| Teaching | 14181 (77.36%) | 730 (71.68%) | 88867 (83.34%) | 10114 (82.46%) | ||
| Hospital bed size | 0.34 | 0.04 | ||||
| Small | 2656 (14.49%) | 156 (15.37%) | 13286 (12.46%) | 1582 (12.9%) | ||
| Medium | 4823 (26.31%) | 235 (23.04%) | 26072 (24.45%) | 2806 (22.88%) | ||
| Large | 10848 (59.18%) | 628 (61.58%) | 67263 (63.08%) | 7874 (64.2%) | ||
| Hospital location | 0.20 | 0.81 | ||||
| Rural | 2561 (13.97%) | 176 (17.28%) | 11399 (10.69%) | 1325 (10.80%) | ||
| Urban | 15769 (86.02%) | 843 (82.71%) | 95222 (89.30%) | 10939 (89.19%) | ||
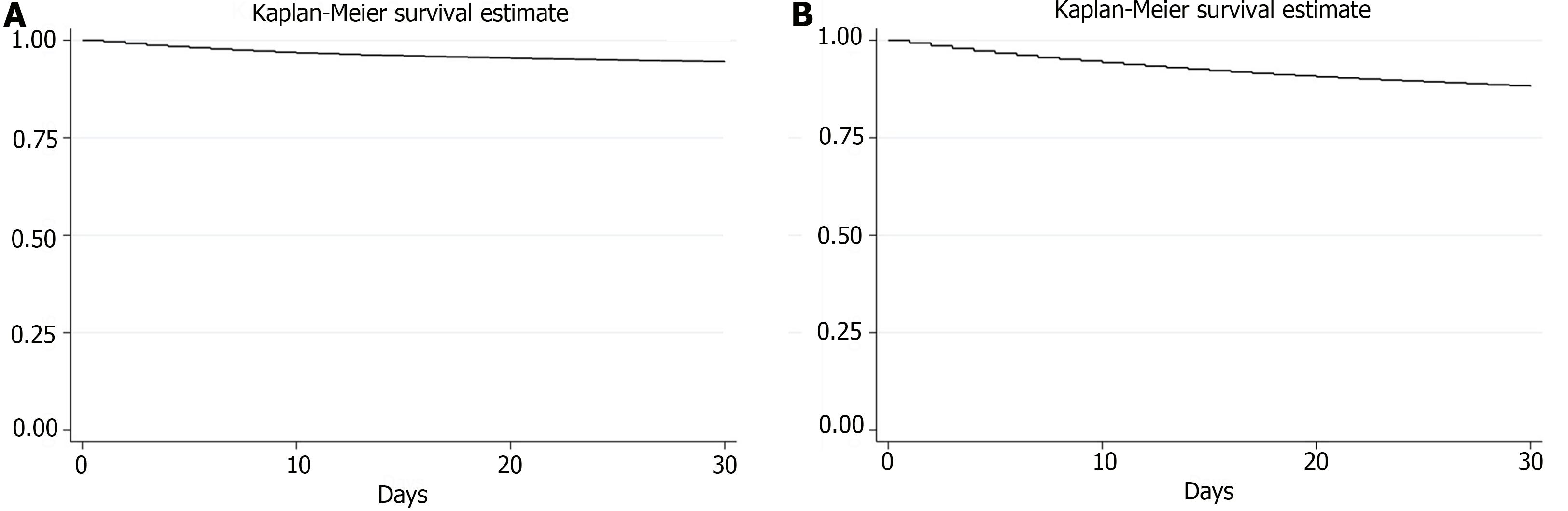
The 30-d all-cause readmission rate was lower in the same-admission CCY group (5.56%, n = 1019) compared to the interval-CCY group (11.50%, n = 12265). Figure 2 shows the Kaplan-Meier survival curves for both the same-admission CCY and interval-CCY groups. Although sepsis was the most common cause of readmission in both groups, cholangitis was the second common cause in the interval-CCY group (Table 2). In multivariate analysis, the independent predictors for readmission were CCI > 3 [adjusted HR = 1.75; 95% confidence interval (CI): 1.04-2.94; P < 0.01], ESRD (HR = 2.18; 95%CI: 1.25-3.81; P < 0.01), and CHF (HR = 1.87; 95%CI: 1.31-2.66; P < 0.01) in the same admission CCY group (Table 3). In the interval-CCY group, the independent predictors of readmission were CCI > 3 (HR = 1.27; 95%CI: 1.22-1.32; P < 0.01), ESRD (HR = 1.41; 95%CI: 1.15-1.73; P < 0.01), and hospital bed size (HR = 1.12; 95%CI: 1.01-1.26; P < 0.01) (Table 4).
| Acute cholangitis with same admission CCY | Acute cholangitis with interval CCY |
| Sepsis (A419) | Sepsis (A419) |
| Acute kidney failure (N179) | Other cholangitis (K8309) |
| Acute pancreatitis without necrosis or infection (K8590) | Malignant neoplasm of the head of the pancreas (C250) |
| Melena (K921) | Obstruction of the bile duct (K831) |
| Hypertensive heart and chronic kidney disease with heart failure (I130) | Sepsis due to Escherichia coli (A4151) |
| Bivariate logistic regression | Multivariate logistic regression | |||||
| Adjusted HR | 95%CI | P value | Adjusted HR | 95%CI | P value | |
| Female | 1.01 | 0.82-1.25 | 0.88 | - | - | - |
| Age (mean) | 1.01 | 0.99-1.01 | 0.14 | 0.99 | 0.98-1.00 | 0.34 |
| Charlson comorbidity index | ||||||
| 1 | Reference | |||||
| 2 | 1.47 | 1.06-2.04 | < 0.01 | 1.48 | 0.94-2.33 | 0.08 |
| 3 or more | 2.49 | 1.89-3.27 | < 0.01 | 1.75 | 1.04-2.94 | 0.03 |
| Median income based on the zip code | ||||||
| $1-$38999 | Reference | |||||
| $39000-$47999 | 0.98 | 0.74-1.30 | 0.92 | - | - | - |
| $48000-$62999 | 0.96 | 0.72-1.29 | 0.83 | - | - | - |
| > $63000 | 0.89 | 0.65-1.21 | 0.47 | - | - | - |
| Primary payer | ||||||
| Medicare | Reference | |||||
| Medicaid | 0.76 | 0.52-1.12 | 0.17 | 0.85 | 0.50-1.46 | 0.57 |
| Private | 0.68 | 0.52-0.90 | < 0.01 | 0.73 | 0.48-1.10 | 0.14 |
| Others | 0.51 | 0.26-1.12 | 0.05 | 0.69 | 0.30-1.60 | 0.39 |
| Comorbidities | ||||||
| Diabetes mellitus | 1.45 | 1.11-1.91 | < 0.01 | 1.07 | 0.74-1.55 | 0.69 |
| Hypertension | 1.24 | 1.01-1.52 | 0.03 | 1.2 | 0.88-1.64 | 0.24 |
| Chronic kidney disease | 1.1 | 1.04-1.16 | < 0.01 | 0.98 | 0.90-1.07 | 0.8 |
| End stage renal disease | 3.31 | 2.03-5.39 | < 0.01 | 2.18 | 1.25-3.81 | < 0.01 |
| Congestive heart failure | 2.37 | 1.85-3.02 | < 0.01 | 1.87 | 1.31-2.66 | < 0.01 |
| Chronic pulmonary obstructive disease | 1.5 | 1.18-1.91 | < 0.01 | 1.09 | 0.79-1.52 | 0.57 |
| Hospital teaching status | ||||||
| Non-teaching | Reference | |||||
| Teaching | 0.81 | 0.65-1.01 | 0.05 | 1.11 | 0.69-1.77 | 0.65 |
| Hospital bed size | ||||||
| Small | Reference | |||||
| Medium | 0.94 | 0.66- 1.33 | 0.72 | 0.64 | 0.42-0.99 | 0.04 |
| Large | 1.19 | 0.87-1.63 | 0.25 | 0.92 | 0.64-1.31 | 0.64 |
| Hospital location | ||||||
| Rural | Reference | |||||
| Urban | 0.76 | 0.58-0.99 | 0.04 | 0.61 | 0.37-1.02 | 0.06 |
| Outcomes | ||||||
| Intensive care unit | 1.98 | 1.38-2.83 | < 0.01 | 1.29 | 0.56-2.96 | 0.54 |
| Acute respiratory failure | 2.45 | 1.46-4.11 | < 0.01 | 1.51 | 0.85-2.7 | 0.15 |
| Septic shock | 1.23 | 0.49-3.09 | < 0.64 | - | - | - |
| Bivariate logistic regression | Multivariate logistic regression | |||||
| Adjusted HR | 95%CI | P value | Adjusted HR | 95%CI | P value | |
| Female | 1.01 | 0.82-1.25 | 0.88 | 0.87 | 0.80-0.94 | < 0.01 |
| Age (mean) | 1.01 | 0.99-1.01 | < 0.14 | 0.99 | 0.98-0.99 | < 0.01 |
| Charlson comorbidity index | ||||||
| 1 | Reference | |||||
| 2 | 1.47 | 1.06-2.04 | 0.12 | - | - | - |
| 3 or more | 2.49 | 1.89-3.27 | < 0.01 | 1.27 | 1.22-1.32 | < 0.01 |
| Median income based on the zip code | ||||||
| $1-$38999 | Reference | |||||
| $39000-$47999 | 0.98 | 0.74-1.30 | 0.92 | - | - | - |
| $48000-$62999 | 0.96 | 0.72-1.29 | 0.83 | - | - | - |
| > $63000 | 0.89 | 0.65-1.21 | 0.47 | - | - | - |
| Primary payer | ||||||
| Medicare | Reference | |||||
| Medicaid | 0.76 | 0.52-1.12 | 0.17 | 1.06 | 0.92-1.22 | 0.38 |
| Private | 0.68 | 0.52-0.90 | < 0.01 | 0.97 | 0.87-1.09 | 0.69 |
| Others | 0.51 | 0.26-1.12 | 0.05 | 0.91 | 0.67-1.24 | 0.57 |
| Comorbidities | ||||||
| Diabetes mellitus | 1.45 | 1.11-1.91 | < 0.01 | 0.93 | 0.85-1.03 | 0.2 |
| Hypertension | 1.24 | 1.01-1.52 | 0.03 | 1.00 | 0.92-1.09 | 0.88 |
| Chronic kidney disease | 1.1 | 1.04-1.16 | < 0.01 | 0.99 | 0.97-1.02 | 0.71 |
| End stage renal disease | 3.31 | 2.03-5.39 | < 0.01 | 1.41 | 1.15-1.73 | < 0.01 |
| Congestive heart failure | 2.37 | 1.85-3.02 | < 0.01 | 1.06 | 0.96-1.18 | 0.19 |
| Chronic obstructive pulmonary disease | 1.5 | 1.18-1.91 | < 0.01 | 0.95 | 0.85-1.05 | 0.32 |
| Hospital teaching status | ||||||
| Non-teaching | Reference | |||||
| Teaching | 1.11 | 1.03-1.20 | < 0.01 | 0.98 | 0.84-1.15 | 0.85 |
| Hospital bed size | ||||||
| Small | Reference | |||||
| Medium | 1.08 | 0.98-1.21 | 0.11 | 1.02 | 0.90-1.17 | 0.66 |
| Large | 1.23 | 1.12-1.35 | < 0.01 | 1.12 | 1.01-1.26 | 0.03 |
| Hospital location | ||||||
| Rural | Reference | |||||
| Urban | 1.13 | 1.03-1.25 | < 0.01 | 1.06 | 0.89-1.27 | 0.49 |
| Complications | ||||||
| Intensive care unit | 1.98 | 1.38-2.83 | < 0.01 | 1.01 | 0.79-1.29 | 0.74 |
| Acute respiratory failure | 2.45 | 1.46-4.11 | < 0.01 | 1.13 | 0.85-1.49 | 0.38 |
| Septic shock | 1.23 | 0.49-3.09 | < 0.64 | 1.29 | 0.93-1.80 | 0.12 |
During the index admissions, inpatient mortality was lower in the same admission-CCY group (1.18% vs 3.17%, P < 0.01) compared to the interval-CCY group, as well as during readmissions (2.53% vs 4.52%, P < 0.01). Although the same admission CCY group had longer lengths of stay during index admission (mean LOS 7.4 d vs 6.5 d, P < 0.01), they had shorter lengths of stay during readmission (mean LOS 5.3 d vs 5.7 d, P < 0.01). In addition, the same admission CCY group had a lower proportion of patients who developed acute respiratory failure (1.86% vs 2.14%, P < 0.01), septic shock (0.9% in CCY vs 1.39% in non-CCY, P < 0.01) and required less intensive care utilization (4.51% vs 7%, P < 0.01) as compared to the interval-CCY group. In terms of hospitalization costs, the overall cost was higher in the same admission CCY group for the index admission ($29522 vs $24014, P < 0.01). However, for readmissions, the interval-CCY group had higher costs ($17672 vs $14166, P < 0.01), as shown in Table 5.
| Outcomes | Index hospitalizations | 30-d readmissions | ||||
| Same admission CCY | Interval CCY | P value | Same admission CCY | Interval CCY | P value | |
| Mortality, n (%) | 216 (1.18) | 3380 (3.17) | < 0.01 | 25 (2.53%) | 554 (4.52%) | < 0.01 |
| Intensive care utilization | 827 (4.51%) | 7454 (6.99%) | < 0.01 | 34 (3.36%) | 464 (3.78%) | < 0.01 |
| Acute respiratory failure | 330 (1.86%) | 2282 (2.14%) | < 0.01 | 21 (2.1%) | 172 (1.4%) | < 0.01 |
| Septic shock | 165 (0.9%) | 1482 (1.39%) | < 0.01 | 15 (1.51%) | 229 (1.87%) | < 0.01 |
| Mean length of stay (d) | 7.39 | 6.51 | < 0.01 | 5.3 | 5.7 | < 0.01 |
| Mean hospitalization cost | $29522 | $24014 | < 0.01 | $14166 | $17672 | < 0.01 |
In this study, we examined practice trends at the national level for performing CCY after ERCP following an episode of gallstone-related AC. We found that patients with gallstone-related- AC who did not undergo the same admission CCY had a higher risk of a 30-d readmission rate as compared to the patients who underwent CCY during the same hospitalization. Sepsis was the most common cause of readmissions in both groups, and AC was the second most common cause of readmissions in the non-CCY group. In comparison to all-cause inpatient mortality, patients in the interval-CCY group had a higher mortality rate during the index hospitalization and rehospitalizations, most likely related to the increased comorbidity burden in these patients. Regarding resource utilization, the findings suggest that inpatient LOS and hospitalization costs were higher in the same admission CCY group, which is attributable to the surgery performed during the index hospitalization. However, this additional surgical procedure appeared to prevent half of the readmissions, which would have resulted in high hospitalization costs and mortality. This suggests that, although the initial hospitalization cost may be higher for the same admission CCY group, the cost savings associated with reduced readmissions may ultimately make this approach more cost-effective and improve patient outcomes.
Several studies have investigated the appropriate timing for CCY following gallstone-related biliary events, such as acute cholecystitis and choledocholithiasis, concluding that early CCY helps prevent recurrent biliary events. A retrospective analysis of a large database conducted in 2017, which included over 4500 hospitalized patients with choledocholithiasis, demonstrated that patients who underwent delayed CCY had a tenfold greater risk of recurrent biliary events than those who underwent early CCY. The study also showed that early CCY after acute cholecystitis might shorten the hospital stay post-surgery[9,10]. In comparison, other studies have reported that delayed or interval CCY is linked to an increased likelihood of recurring biliary events[14]. For instance, Schiphorst et al[9] reported the recurrence rate of biliary symptoms of 20% as early as 22 d in patients who awaited planned CCY.
There is still no concrete evidence on the optimal timing for performing the procedure in patients diagnosed with AC related to gallstones[13]. Severance et al[17] conducted a retrospective review of 127 patients with gallstone-related AC to determine the role of early CCY (within 72 h after ERCP) vs delayed CCY (72 h after ERCP) and found that patients who underwent delayed CCY had a higher rate of readmission (13.2 vs 8.3, P = 0.4); however, the results were not statistically different due to the small sample size[17]. In a recently published single-center retrospective study, patients with acute gallstone cholangitis who underwent the same admission CCY were found to have significantly lower 30-d (2.2% vs 42.6%, P < 0.001) and 90-d readmission rates (2.2% vs 30.9%, P < 0.01) compared to patients who underwent ERCP alone[3].
In terms of mortality, previous studies have highlighted an increased mortality rate associated with interval or delayed CCY, which aligns with our study findings as well[3]. For instance, a retrospective cohort study conducted in 2019 revealed not only a higher risk of developing recurrent acute cholecystitis but also an elevated rate of postoperative complications associated with delayed CCY[13]. These findings can be explained by postulating that patients in the delayed CCY group may have severe clinical presentations or were not ideal surgical candidates, as evidenced by a higher comorbidity burden. Patients undergoing urgent decompression of the common bile duct are still under physiological stress secondary to ongoing sepsis related to the AC, which can significantly increase the risk of morbidity and mortality associated with the procedure[18]. However, the study mentioned above demonstrated that early CCY after AC was safe and not linked to higher operative times or increased conversion rates to open surgery, irrespective of Tokyo grade[19]. Regarding disposition, the majority of patients in both cohorts were admitted to tertiary care hospitals. Patients with AC are generally sick and require biliary decompression procedures to get better. Most community hospitals in the United States do not have the availability of endoscopic or surgical biliary decompression procedures because of limited resources, which is the most likely reason why the majority of these patients are admitted or transferred to teaching hospitals.
There are relatively few studies comparing resource utilization, including LOS and hospitalization cost, between the two groups. A recently published retrospective study conducted by Hoilat et al[3] included patients admitted to a high-volume tertiary referral teaching hospital between January 2015 and 2021. The study reported that patients who underwent CCY during the same index admission had a nearly two-day shorter LOS than those who underwent ERCP alone. However, the results were not statistically significant. The study also found that performing laparoscopic CCY during the index admission was associated with a reduction in 30-d and 90-d readmission rates without prolonging the hospital stay[3]. In contrast to these findings, the results from our study showed an increased LOS in patients who underwent the same admission CCY and higher mean hospitalization cost in the index hospitalization, most likely due to the increased LOS and cost associated with surgery. However, in comparison, the readmissions in the delayed or interval CCY group incurred a collective total cost of $118 million vs 7.12 million in the same admission CCY group. Although the most common reason for readmissions in both groups included sepsis, recurrent AC was the second most common reason in the non-CCY group. The use of a large database based on ICD-10 coding further limited our ability to explore the secondary sources of sepsis in both groups. However, we can assume that the cause of sepsis was most likely unrelated to AC.
The optimal timing of early CCY after an AC episode remains a topic of debate, leaving clinicians to ponder and use their clinical judgment. Delayed CCY in some cases may be attributed to hesitancy to conduct a CCY in the early stages after the AC episode due to the concern of increased systemic inflammation, which may increase the chances of complications. For these reasons, surgeons often prefer to allow the patient to be discharged and for a “cool-down” period before performing the CCY. In contrast, multiple recent studies have shown that early CCY following AC was not associated with longer procedure times and higher complication rates. A lower complication rate was observed when early laparoscopic CCY took place, and a lower conversion rate to open CCY regardless of the Tokyo grade[19-22].
There are several limitations to this study that must be considered when interpreting the findings. First, this is a retrospective cross-sectional study, and as with all cross-sectional studies, causality cannot be established, and only associations can be inferred. Second, this database study relies on accurate ICD-10 coding and is subject to coding errors that could affect the accuracy of the data. Additionally, the database does not include information on vital signs, laboratory results, or imaging findings, limiting the ability to determine the Tokyo grading of AC and estimate the disease severity. However, our primary focus was on studying practice trends and outcomes among patients with AC regardless of grade. Furthermore, since the National Inpatient Sample and NRD have inpatient hospitalization data, no information was available for patients who underwent outpatient CCY after index admission. We could not assess factors such as social barriers to readmission or discharge, medication compliance, or accessibility to outpatient resources. The NRD also does not record out-of-state readmissions, which could have led to underestimating the readmission rate. There are other decompression approaches available for biliary decompression, but since the latest Tokyo 2018 guidelines endorses endoscopic drainage as the preferred method for biliary decompression in cases of AC, we studied this approach. Finally, the patients selected for this study who did not undergo CCY during the index hospitalization may have introduced a selection bias, as they could represent a sicker group of patients. Despite the limitations mentioned above, this is the first large-scale study to explore the practice trends in the timing of performing CCY in patients with gallstone-related AC at a national level regardless of hospital size, type, and geographical location, giving it more generalizability and validity. Although the results indicate the potential advantages of same admission CCY over an interval or delayed CCY in terms of preventing readmission-related costs and improving patient outcomes, nevertheless, these findings do not replace individual risk assessments to determine the surgical candidacy of a patient based on clinical presentation and comorbidities. However, this topic demands further investigation to examine the long-term outcomes and cost-effectiveness of the same admission CCY, and further prospective research at a detailed level is required.
Performing CCY during the same admission for patients with gallstone-related AC significantly reduced the risk of 30-d readmissions compared with interval CCY. This approach may offset higher initial costs and improve overall patient outcomes by potentially preventing readmissions. This study highlights the importance of considering same-admission CCY for patients with gallstone-related AC to reduce readmission and associated costs. Further research is needed to explore the long-term outcomes and cost-effectiveness of this strategy, along with prospective studies to validate these findings across different patient populations and healthcare settings.
| 1. | Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, Hata J, Liau KH, Miura F, Horiguchi A, Liu KH, Su CH, Wada K, Jagannath P, Itoi T, Gouma DJ, Mori Y, Mukai S, Giménez ME, Huang WS, Kim MH, Okamoto K, Belli G, Dervenis C, Chan ACW, Lau WY, Endo I, Gomi H, Yoshida M, Mayumi T, Baron TH, de Santibañes E, Teoh AYB, Hwang TL, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Higuchi R, Kitano S, Inomata M, Deziel DJ, Jonas E, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:17-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 424] [Article Influence: 60.6] [Reference Citation Analysis (0)] |
| 2. | Shineha R, Inoue Y, Ikka T, Kishimoto A, Yashiro Y. A Comparative Analysis of Attitudes on Communication Toward Stem Cell Research and Regenerative Medicine Between the Public and the Scientific Community. Stem Cells Transl Med. 2018;7:251-257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Hoilat GJ, Hoilat JN, Abu-Zaid A, Raleig J, Tot J, Mandal A, Sostre V, Carvounis C, Sapkota B. Impact of early cholecystectomy on the readmission rate in patients with acute gallstone cholangitis: a retrospective single-centre study. BMJ Open Gastroenterol. 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Lee YS, Cho KB, Park KS, Lee JY, Lee YJ. Procalcitonin as a Decision-Supporting Marker of Urgent Biliary Decompression in Acute Cholangitis. Dig Dis Sci. 2018;63:2474-2479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Takada T, Kawarada Y, Nimura Y, Yoshida M, Mayumi T, Sekimoto M, Miura F, Wada K, Hirota M, Yamashita Y, Nagino M, Tsuyuguchi T, Tanaka A, Kimura Y, Yasuda H, Hirata K, Pitt HA, Strasberg SM, Gadacz TR, Bornman PC, Gouma DJ, Belli G, Liau KH. Background: Tokyo Guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Surg. 2007;14:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 97] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 6. | Takada T, Strasberg SM, Solomkin JS, Pitt HA, Gomi H, Yoshida M, Mayumi T, Miura F, Gouma DJ, Garden OJ, Büchler MW, Kiriyama S, Yokoe M, Kimura Y, Tsuyuguchi T, Itoi T, Gabata T, Higuchi R, Okamoto K, Hata J, Murata A, Kusachi S, Windsor JA, Supe AN, Lee S, Chen XP, Yamashita Y, Hirata K, Inui K, Sumiyama Y; Tokyo Guidelines Revision Committee. TG13: Updated Tokyo Guidelines for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 188] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 7. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 372] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 8. | Gomi H, Takada T, Hwang TL, Akazawa K, Mori R, Endo I, Miura F, Kiriyama S, Matsunaga N, Itoi T, Yokoe M, Chen MF, Jan YY, Ker CG, Wang HP, Wada K, Yamaue H, Miyazaki M, Yamamoto M. Updated comprehensive epidemiology, microbiology, and outcomes among patients with acute cholangitis. J Hepatobiliary Pancreat Sci. 2017;24:310-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 9. | Schiphorst AH, Besselink MG, Boerma D, Timmer R, Wiezer MJ, van Erpecum KJ, Broeders IA, van Ramshorst B. Timing of cholecystectomy after endoscopic sphincterotomy for common bile duct stones. Surg Endosc. 2008;22:2046-2050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Huang RJ, Barakat MT, Girotra M, Banerjee S. Practice Patterns for Cholecystectomy After Endoscopic Retrograde Cholangiopancreatography for Patients With Choledocholithiasis. Gastroenterology. 2017;153:762-771.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Reinders JS, Goud A, Timmer R, Kruyt PM, Witteman BJ, Smakman N, Breumelhof R, Donkervoort SC, Jansen JM, Heisterkamp J, Grubben M, van Ramshorst B, Boerma D. Early laparoscopic cholecystectomy improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis. Gastroenterology. 2010;138:2315-2320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Wang CC, Tsai MC, Wang YT, Yang TW, Chen HY, Sung WW, Huang SM, Tseng MH, Lin CC. Role of Cholecystectomy in Choledocholithiasis Patients Underwent Endoscopic Retrograde Cholangiopancreatography. Sci Rep. 2019;9:2168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Li VK, Yum JL, Yeung YP. Optimal timing of elective laparoscopic cholecystectomy after acute cholangitis and subsequent clearance of choledocholithiasis. Am J Surg. 2010;200:483-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Agency for Healthcare Research and Quality. Agency for Healthcare Research and Quality. Introduction the HCUP Nationwide Readmissions Database (NRD) 2020. [cited 15 December 2023]. Available from: https://www.hcup-us.ahrq.gov/db/nation/nrd/Introduction_NRD_2020.pdf. |
| 15. | Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32099] [Cited by in RCA: 38229] [Article Influence: 1006.0] [Reference Citation Analysis (0)] |
| 16. | Agency for Healthcare Research and Quality. HCUP Cost-to-Charge Ratio (CCR) for the National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2020. [cited 15 December 2023]. Available from: https://www.hcup-us.ahrq.gov/db/ccr/ip-ccr/ip-ccr.jsp. |
| 17. | Severance SE, Feizpour C, Feliciano DV, Coleman J, Zarzaur BL, Rozycki GF. Timing of Cholecystectomy after Emergent Endoscopic Retrograde Cholangiopancreatography for Cholangitis. Am Surg. 2019;85:895-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Poon RT, Liu CL, Lo CM, Lam CM, Yuen WK, Yeung C, Fan ST, Wong J. Management of gallstone cholangitis in the era of laparoscopic cholecystectomy. Arch Surg. 2001;136:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Discolo A, Reiter S, French B, Hayes D, Lucas G, Tan L, Scanlan J, Martinez R. Outcomes following early versus delayed cholecystectomy performed for acute cholangitis. Surg Endosc. 2020;34:3204-3210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Friis C, Rothman JP, Burcharth J, Rosenberg J. Optimal Timing for Laparoscopic Cholecystectomy After Endoscopic Retrograde Cholangiopancreatography: A Systematic Review. Scand J Surg. 2018;107:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Trejo-Ávila M, Solórzano-Vicuña D, García-Corral R, Bada-Yllán O, Cuendis-Velázquez A, Delano-Alonso R, Herrera-Esquivel J, Valenzuela-Salazar C. Laparoscopic cholecystectomy after endoscopic treatment of choledocholithiasis: a retrospective comparative study. Updates Surg. 2019;71:669-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Abe T, Amano H, Hanada K, Bekki T, Minami T, Yonehara S, Noriyuki T, Nakahara M. Efficacy and safety of early cholecystectomy for comorbid acute cholecystitis and acute cholangitis: Retrospective cohort study. Ann Med Surg (Lond). 2019;38:8-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |