Published online Jun 16, 2024. doi: 10.4253/wjge.v16.i6.343
Revised: February 23, 2024
Accepted: April 29, 2024
Published online: June 16, 2024
Processing time: 155 Days and 23.2 Hours
Incomplete congenital duodenal obstruction (ICDO) is caused by a congenitally perforated duodenal web (CPDW). Currently, only six cases of balloon dilatation of the PDW in newborns have been described.
To present our experience of balloon dilatation of a perforated duodenal memb
Five newborns who underwent balloon dilatation of the CPDW along a prein
In all cases, good anatomical and clinical results were obtained. In three cases, a follow-up study was conducted after 1 year. The average time to start enteral feeding per os was significantly earlier in the study group (4.4 d) than in the laparotomic group (21.2 days; P < 0.0001). The time spent by patients in the intensive care unit and hospital after balloon dilatation was also significantly shorter. We determined the selection criteria for possible and effective CPDW balloon dilatation in newborns as follows: (1) Presence of dynamic radiographic signs of the passage of a radiopaque substance beyond the zone of narrowing or radiographic signs of pneumatisation of the duodenum and small bowel distal to the web; (2) presence of endoscopic signs of CPDW; (3) successful cannulation with a guidewire performed parallel to the endoscope, with holes in the congenital duodenal web; and (4) successful positioning of the balloon performed along a freestanding guidewire on the web.
Strictly following selection criteria for newborns with ICDO caused by CPDW ensures that endoscopic balloon dilatation using a pre-installed guidewire is safe and effective and shows good 1-year follow-up results.
Core Tip: Congenital perforated duodenal web is the most common cause of incomplete congenital duodenal obstruction (ICDO). The clinical picture of ICDO may be absent, leading to its late diagnosis. Since 1986, approximately 70 cases of endoscopic treatment of congenital perforated duodenal membrane have been described in the literature, with only 6 cases in newborns. This study presents five successful cases of endoscopic treatment of congenital perforated duodenal web in newborns, including their one-year follow-up outcomes.
- Citation: Marakhouski K, Malyshka E, Nikalayeva K, Valiok L, Pataleta A, Sanfirau K, Svirsky A, Averin V. Balloon dilation of congenital perforated duodenal web in newborns: Evaluation of short and long-term results. World J Gastrointest Endosc 2024; 16(6): 343-349
- URL: https://www.wjgnet.com/1948-5190/full/v16/i6/343.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i6.343
Duodenal atresia (DA) occurs at a frequency of 1 in 7000–10000 live births and accounts for approximately 60% of cases of small intestinal atresia[1]. Type I DA, where the internal septum is a membrane with no mesenteric defects, occurs in 90% of all cases of DA[2]. The duodenal web develops after incomplete recanalisation of the duodenal lumen at 8-10 wk of gestation. It is believed to have formed from the mucosal and submucosal layers of the intestine[3]. The congenital duodenal web (CDW) is localised in the descending part (D2) of the duodenum in 85%-90% of cases[4]; less often, it is localised in the third or fourth parts (D3, D4) of the duodenum[5]. Part of the CDW is represented by a variant of the perforated duodenal membrane. A congenital perforated membrane is one of the most difficult to diagnose conditions because it does not create a complete obstruction; it passes food from the stomach and duodenal bulb distally in some quantity. The clinical picture of a congenitally perforated duodenal web (CPDW) may be unclear and may depend on the size and thickness of the hole in the membrane. A CPDW can cause an incomplete congenital duodenal obstruction (ICDO). The diagnosis of such conditions can shift significantly from the neonatal period[6].
The first endoscopic treatment for ICDO caused by the presence of a perforated duodenal web in a 2-month-old child weighing 3100 g using an endoscopic technique was described by Okamatsu in 1989[7]. Currently, approximately 50 cases of endoscopic treatment of ICDO in different age groups, including adults, have been published worldwide[8-18]. Experts in paediatric endoscopy consider that it is practically proven that the successful endoscopic treatment of ICDO due to the congenital perforated web is possible[19].
However, only six cases of balloon dilatation of a CPDW in newborns have been described in the literature at present. Four of these were performed and described by van Rijn et al[9] in 2006 and one by Asabe et al[10] in 2008. van Rijn et al[9] used a preinstalled guidewire in his work. One more newborn baby was described by Wang X et al[20] in August 2023; the technique of balloon dilatation through an endoscope was used in this case. In other cases of balloon dilatation, which were performed in older children, the technique ‘through the scope’ was used. At present, there are no standardised approaches for endoscopic surgery and patient selection.
At our centre, the first attempt to dissect the duodenal membrane using endoscopic access was performed in 2005. Subsequently, 18 endoscopic duodenal lumen restorations were performed at the Republican Scientific and Practical Center for Pediatric Surgery (RSPCPS) between 2006 and 2021. The endoscopic membrane incision technique was used in this study, and 13 control patients underwent endoscopic techniques only. In cases of complications due to endoscopic treatment of ICDO, conversion to laparotomy was performed, which occurred in almost one-third (27.7%) of cases. This was probably due to the incorrect selection of patients for method use and the presence of methodological mistakes.
Our next step was to analyse the experience of unsuccessful attempts at endoscopic treatment of ICDO caused by CPDW and endoscopic recognition of the intralumenal picture of congenital duodenal obstruction (CDO) or ICDO[21,22]. Based on this analysis, the mandatory criteria for successful restoration of the duodenal lumen were determined. In particular, it was accepted that endoscopic repair of the duodenal lumen is possible if the following conditions are present: (1) Pneumatisation of the distal small intestine and colon or passage of contrast through the CDW under radiography; (2) successful cannulation of the web orifice with a guidewire; and (3) dissection of the membrane using electrocautery only if the membrane was located in the descending part of the duodenum (or D2).
Therefore, in this study, we aimed to present our experience of balloon dilatation of a perforated duodenal membrane in newborns with ICDO caused by CPDW at the (RSPCPS), Minsk, Belarus.
Five newborns with ICDO caused by CPDW were included in this study. All patients underwent balloon dilatation along a preinstalled guidewire with endoscopic access at the RSPCPS, between the period 2021 to 2023. The group consisted of three girls (60%) and two boys (40%). The average weight at birth was 3586.0 g (95%CI: 3199.4–3972.6 g) and average gestational age was 39.2 wk (95%CI: 38.6–39.7 wk).
CDO/ICDO was suspected prenatally at a gestational age of 20–35 wk in all the patients in the study group. For patients without typical obstruction symptoms, an abdomen X-ray and small bowel follow through were performed; the examination showed a dilated duodenum, a ‘double bubble’ pattern, and pneumatisation/contrast passing to the distal part of the small bowel and colon. Diagnostic measures were performed to exclude ICDO due to duodenal and/or intestinal fixation and rotation disorders, predisposing the patient to volvulus and intestinal necrosis.
Endoscopy was performed using a GIF-XP190N, 5.4 mm outer diameter EXERA III (Olympus, Tokyo, Japan). During endoscopy, we attempted to cannulate the visible hole in the membrane with a guidewire. After successful cannulation, X-ray control of the guidewire position in the ‘after web’ part of the duodenum was performed. The endoscope was removed, and the guidewire was left in the distal duodenum web position. A high-pressure balloon dilatator (CRE PRO wireguided 6-7-8 mm; Boston Scientific, Cork, Ireland) was then passed along the pre-installed guidewire (Jagwire, straight tip, 0.035 in; Boston Scientific, Cork, Ireland). The balloon was positioned on the membrane and inflated to a starting size of 6 mm under visual control using an endoscope passed through a parallel guidewire. The total time for balloon dilatation was 5 min 8 mm for each session.
Full video recording and archiving of each intervention were performed using a second-generation Videcap (Belarus) system for follow-up control. Data of the patients in the study group are presented in Table 1.
| Patient | Sex | Birth weight (g) | Gestational age at birth (wk) | Diagnosis | Concomitant pathology |
| SKR | M | 3920 | 38 | Prenatally, 20 wk | Hypoplasia of the 12th left rib |
| VAA | F | 3310 | 40 | Prenatally, 30 wk | Anaemia |
| XMR | M | 3890 | 39 | Prenatally, 35 wk | Subaortic ventricular septal defect. Moderate stenosis of the branches of the pulmonary artery. Situs inversus |
| SIG | M | 3260 | 39 | Prenatally, 33 wk | Anaemia |
| SUM | F | 3550 | 39 | Prenatally, 30 wk | None |
Nineteen patients with CDO who underwent laparotomy were selected as the comparison group. The causes of CDO were the duodenal web, DA, and annular pancreas. The sex ratio of the comparison group was as follows: Girls, 8 (42.1%); boys, 11 (57.9%). In 14 cases, CDO was diagnosed prenatally. The average birth weight was 2813.9 g (95%CI: 2476.2–3151.7 g), and the gestational age was 37.1 wk (95%CI: 36.2–37.9 wk), and in both cases, the Shapiro–Wilk test confirmed the normality of the distribution. The postnatal diagnosis of CDO was established based on a clinical picture, ultrasound, and radiographic examination.
All patients of the comparison group underwent correction of a congenital defect using laparotomic access, of which six patients underwent duodenotomy and excision of the membrane, and 13 patients underwent duodeno-duodenoanastomosis, according to Kimura.
The MedCalc® Statistical Software version 20.218 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2023) was used for statistical data analysis. Descriptive statistics, including the arithmetic mean and median with a 95%CI, were used to summarise the data. Independent variables were analysed using Mann–Whitney test and t-test. Results were considered significant at P values < 0.05.
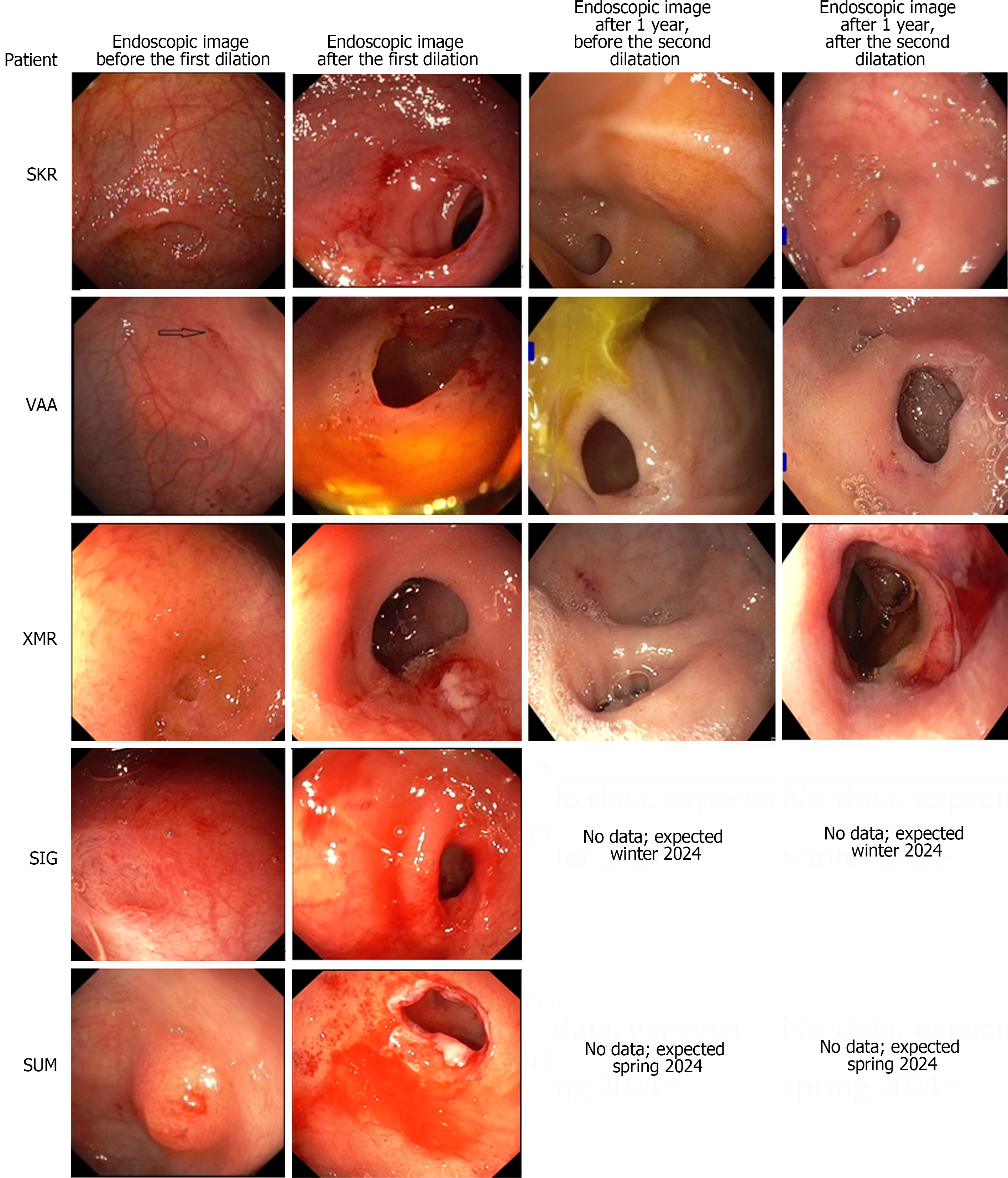
Balloon dilatation along a pre-installed guidewire was performed in five newborn patients as an initial treatment for ICDO due to the presence of a CPDW (Table 2). No postoperative complications occurred in any of the patients. Clinical assessment and endoscopy with a second dilation of the web through the endoscope were performed in three cases at 11, 13, and 15 months of age. The second balloon dilatation was performed one year after the first one (Figure 1). The children were under outpatient observation at the RSPCPS at a frequency of once every 3 months.
| Patient | Topography of the duodenal web | Balloon diameter for first dilatation (Fr) | Age at first dilatation (days after birth) | The starting day per os nutrition after dilatation (d) | Time spent in hospital/time spent in ICU (d) | Postoperative complications | Age at the time of the second endoscopy and balloon dilatation (months) | Balloon diameter for second dilatation (Fr) | Weight during the control examination (g) |
| SKR | D3 | 24 | 4 | 1 | 15/8 | No | 13 | 30-33-26 | 10500 |
| VAA | D2 | 24 | 4 | 3 | 14/7 | No | 11 | 30-33-26 | 10200 |
| XMR | D2 | 24 | 2 | 1 | 18/10 | No | 15 | 30-33-26 | 11000 |
| SIG | D2 | 18, 21, 24 | 4 | 2 | 20/13 | No | In progress | ||
| SUM1 | D2 | 18, 21, 24 | 2 | 7 | 1/8 | No | In progress | ||
A comparative analysis of the data from both groups of patients revealed several features. The gestational age and weight of patients who underwent balloon dilatation were significantly higher, i.e., the balloon dilation group was made up of patients at a lower risk. The average time to start enteral feeding per os after dilatation was 2.8 d, which was significantly earlier than that in the group with laparotomic access. The time spent in the intensive care unit and hospital after balloon dilatation was also significantly shorter (Table 3).
| Patient data | Patients with ICDO who underwent balloon dilatation of a perforated web, 95%CI | Patients with ICDO/CDO who underwent laparotomy surgery, 95%CI | Р value1 |
| Gestational age (wk) | 39.0 (38.6–39.7) | 37.0 (34.0–38.0) | 0.0093; Mann–Whitney |
| Birth weight (g) | 3586.0 (3199.4–3972.6) | 2813.9 (2476.2–3151.7) | 0.0269 |
| Time to start enteral feeding per os after surgery (d) | 2.8 (-0.29–5.89) | 21.2 (18.1–24.3) | < 0.0001 |
| Time spent in the intensive care unit (d) | 9.2 (6.2356–12.1644) | 20.5 (17.5–23.5) | 0.0025 |
| Total time spent in hospital (d) | 16.9 (12.4–21.1) | 30.4 (27.4–33.3) | 0.0003 |
Endoscopic treatment of the duodenal membrane was first performed more than 30 years ago[7]. The immediate results obtained during the treatment of ICDO due to the presence of CPDW seem promising; however, the lack of sufficient experience in the application of this technique and the lack of long-term follow-up results leave a number of questions. The first is the selection of patients for whom endoscopic techniques are safe and effective. Our experience of observing patients after endoscopic dissection of the web with electrocautery suggests that, in some cases, the dissected zone narrowed during the late postoperative period. These questions will only be answered with the accumulated experience of endoscopic treatment of ICDO due to the presence of CPDW in newborns and the increasing number of patients who undergo the surgery. At present, the treatment of newborns is represented by isolated cases in the literature.
Based on all our attempts at endoscopic treatment of ICDO due to the presence of a CPDW and their follow-up, we observed the following: (1) Performing balloon dilatation in the neonatal period is safer but is no less effective than the use of endoscopic membrane incision; and (2) endoscopic duodenal repair in the neonatal period provides better long-term results than the same technique performed at an older age.
van Rijn et al[9] stated that the weakness of their study was the lack of dynamic observation of the dilated web. In our study, three of the five patients were followed-up 1 year after primary dilatation, and in the first year of life, the parents of all three children had no complaints. The weights of the children corresponded to the norms for this age group (Table 2). The diameter of the dilated hole also did not narrow (Figure 1).
However, despite its simplicity, this operation is associated with a high risk of complications. As a result, one case of balloon dilatation was excluded from the analysis due to an operator’s mistake in meeting the criteria necessary for successful restoration of the duodenal lumen in a newborn with a gestational age of 34 wk and body weight of 2000 g. Duodenal perforation occurred during balloon dilation in this patient, and a conversion to laparotomy was performed for duodenotomy with excision of the duodenal membrane.
After studying publications and based on our own clinical experience at the RSPCPS, the Minsk criteria were adopted, under which, in our opinion, balloon dilatation of the congenital perforated membrane in newborns is possible and will be effective. The criteria are as follows: (1) The presence of dynamic radiographic signs of the passage of a radiopaque substance beyond the zone of narrowing or the presence of radiographic signs of pneumatisation of the duodenum and small bowel distal to the membrane; (2) the presence of endoscopic signs of a congenital duodenal perforated web; (3) successful cannulation achieved using a guidewire installed parallel to the endoscope and holes in the congenital duodenal web; and (4) successful positioning of the balloon along a freestanding guidewire on the web.
Strictly following the selection criteria for newborn patients with ICDO caused by a CPDW allowed us to consider the method of endoscopic balloon dilatation using a pre-installed guidewire as safe and effective in the newborns with a 1-year follow up period.
| 1. | Best KE, Tennant PW, Addor MC, Bianchi F, Boyd P, Calzolari E, Dias CM, Doray B, Draper E, Garne E, Gatt M, Greenlees R, Haeusler M, Khoshnood B, McDonnell B, Mullaney C, Nelen V, Randrianaivo H, Rissmann A, Salvador J, Tucker D, Wellesly D, Rankin J. Epidemiology of small intestinal atresia in Europe: a register-based study. Arch Dis Child Fetal Neonatal Ed. 2012;97:F353-F358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 86] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Adams SD, Stanton MP. Malrotation and intestinal atresias. Early Hum Dev. 2014;90:921-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 3. | Eksarko P, Nazir S, Kessler E, LeBlanc P, Zeidman M, Asarian AP, Xiao P, Pappas PJ. Duodenal web associated with malrotation and review of literature. J Surg Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Melek M, Edirne YE. Two cases of duodenal obstruction due to a congenital web. World J Gastroenterol. 2008;14:1305-1307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Materne R. The duodenal wind sock sign. Radiology. 2001;218:749-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Huang MH, Bian HQ, Liang C, Wei WQ, Duan XF, Yang J. Gastroscopic treatment of membranous duodenal stenosis in infants and children: report of 6 cases. J Pediatr Surg. 2015;50:413-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Okamatsu T, Arai K, Yatsuzuka M, Ishikawa M, Matsumura M, Okamoto S, Gomi A, Suzuki M, Kanno S. Endoscopic membranectomy for congenital duodenal stenosis in an infant. J Pediatr Surg. 1989;24:367-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Nose S, Kubota A, Kawahara H, Okuyama H, Oue T, Tazuke Y, Ihara Y, Okada A. Endoscopic membranectomy with a high-frequency-wave snare/cutter for membranous stenosis in the upper gastrointestinal tract. J Pediatr Surg. 2005;40:1486-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | van Rijn RR, van Lienden KP, Fortuna TL, D'Alessandro LC, Connolly B, Chait PG. Membranous duodenal stenosis: initial experience with balloon dilatation in four children. Eur J Radiol. 2006;59:29-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Asabe K, Oka Y, Hoshino S, Tsutsumi M, Yokoyama M, Yukitake K, Nagakawa K, Yoshizato T, Kawarabayashi T, Shirakusa T. Modification of the endoscopic management of congenital duodenal stenosis. Turk J Pediatr. 2008;50:182-185. [PubMed] |
| 11. | Beeks A, Gosche J, Giles H, Nowicki M. Endoscopic dilation and partial resection of a duodenal web in an infant. J Pediatr Gastroenterol Nutr. 2009;48:378-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Mochizuki K, Obatake M, Kosaka T, Tokunaga T, Eguchi S, Kanematsu T. Endoscopic balloon dilatation for congenital membranous stenosis in the jejunum in an infant. Pediatr Surg Int. 2011;27:91-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Bittencourt PF, Malheiros RS, Ferreira AR, Carvalho SD, Filho PP, Tatsuo ES, Mattos FF, Melo SO, Albuquerque W, Arantes V, Alberti LR. Endoscopic treatment of congenital duodenal membrane. Gastrointest Endosc. 2012;76:1273-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Bleve C, Costa L, Bertoncello V, Ferrara F, Zolpi E, Chiarenza SF. Endoscopic resection of a duodenal web in an 11-month-old infant with multiple malformations. Endoscopy. 2015;47 Suppl 1 UCTN:E210-E211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Kamal N, Hogan C, Midulla PS, DiMaio CJ. Successful Endoscopic Needle-Knife Catheter Membranotomy of a Congenital Duodenal Web. J Pediatr Gastroenterol Nutr. 2015;61:e22-e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Poddar U, Jain V, Yachha SK, Srivastava A. Congenital duodenal web: successful management with endoscopic dilatation. Endosc Int Open. 2016;4:E238-E241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Luffy R, Troendle DM. Endoscopic Management of Duodenal Web. J Pediatr Gastroenterol Nutr. 2019;69:e117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 18. | Goring J, Isoldi S, Sharma S, Torroni F, Marven S, De Angelis P, Thomson M. Natural orifice endoluminal technique (NOEL) for the management of congenital duodenal membranes. J Pediatr Surg. 2020;55:282-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Schluckebier D, Afzal NA, Thomson M. Therapeutic Upper Gastrointestinal Endoscopy in Pediatric Gastroenterology. Front Pediatr. 2021;9:715912. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Wang X, Lin K, Liu H, Hu Z, Ye G, Sheng Q, Lv Z. Endoscopic Balloon Dilatation-Based Membrane Resection for Membranous Duodenal Stenosis: A Feasibility and Safety Study (With Video). J Pediatr Gastroenterol Nutr. 2023;77:e36-e41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |