Published online Jun 16, 2024. doi: 10.4253/wjge.v16.i6.318
Revised: February 15, 2024
Accepted: May 7, 2024
Published online: June 16, 2024
Processing time: 168 Days and 16.1 Hours
At present, laparoscopic cholecystectomy (LC) is the main surgical treatment for gallstones. But, after gallbladder removal, there are many complications. Therefore, it is hoped to remove stones while preserving the function of the gallbladder, and with the development of endoscopic technology, natural orifice transluminal endoscopic surgery came into being.
To compare the quality of life, perioperative indicators, adverse events after LC and transgastric natural orifice transluminal endoscopic gallbladder-preserving surgery (EGPS) in patients with gallstones.
Patients who were admitted to The First Affiliated Hospital of Xinjiang Medical University from 2020 to 2022 were retrospectively collected. We adopted propen
A total of 662 cases were collected, of which 589 cases underwent LC, and 73 cases underwent EGPS. Propensity score matching was performed, and 40 patients were included in each of the groups. In the EGPS group, except the gastr
Whether EGPS or LC, it can improve the patient’s symptoms, and the EGPS has less impact on the patient’s defecation. It needed to, prospective, multicenter, long-term follow-up, large-sample related studies to prove.
Core Tip: Laparoscopic cholecystectomy (LC) is now the gold standard for treating gallstones. However, long-term complications of LC such as postcholecystectomy syndrome, bile duct injury, intestinal dysbiosis, tumor may occur. Some experts want to remove the gallstones while preserving the function of the gallbladder, natural orifice transluminal endoscopic surgery came into being. This study compared transgastric natural orifice transluminal endoscopic gallbladder-preserving surgery with traditional LC.
- Citation: Zhang MY, Zheng SY, Ru ZY, Zhang ZQ. Analysis of quality of life in patients after transgastric natural orifice transluminal endoscopic gallbladder-preserving surgery. World J Gastrointest Endosc 2024; 16(6): 318-325
- URL: https://www.wjgnet.com/1948-5190/full/v16/i6/318.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i6.318
Gallstones is a common digestive disease worldwide, with a gradual increase in incidence[1], which global prevalence of about 10% to 20%[2]. The initial surgical treatment for gallstones was open cholecystectomy, which later evolved into small-incision cholecystectomy, and laparoscopic cholecystectomy (LC) is now the preferred treatment option. Human gallbladder has many physiological functions, including storage, contraction and relaxation, enrichment, absorption, secretion, the adjustment, the function of the bacteriological bank, antibacterial, immune and protection[3]. After gallbladder removal, symptoms such as postcholecystectomy syndrome[4], bile duct injury[5], intestinal dysbiosis[6], tumor[7] may occur. Therefore, it is desirable to remove the gallstones while preserving the function of the gallbladder. With the development of endoscopic technology, natural orifice transluminal endoscopic surgery (NOTES) came into being, the combination of the two provides a new idea for the treatment of gallstones. In this study, patients with gallstones were compared with the changes in symptoms before and after LC and transgastric natural orifice transluminal endoscopic gallbladder-preserving surgery (EGPS).
We conducted a retrospective analysis of clinical data from patients who underwent LC or EGPS of The First Affiliated Hospital of Xinjiang Medical University between Jan 2020 and Dec 2022.
Inclusion criteria: (1) Diagnosed with gallstones by ultrasound, computed tomography or magnetic resonance imaging before surgery; (2) Patients over the age of 18 years; and (3) No absolute surgical contraindications.
Exclusion criteria: (1) Combined with other malignant tumors; (2) With severe organ damage or complications; (3) With serious or unstable diseases of the cardiac, pulmonary, rheumatic immune or endocrine system; (4) With gallbladder polyps, gallbladder adenomyomatosis, chronic atrophic cholecystitis; (5)With other organic digestive system diseases; (6) With the history of other major abdominal surgery; (7) With uncontrolled psychiatric disorders such as depression, dysthymia, anxiety, bipolar disorder, chizophrenia etc.; and (8) Could not be contacted or loss of information.
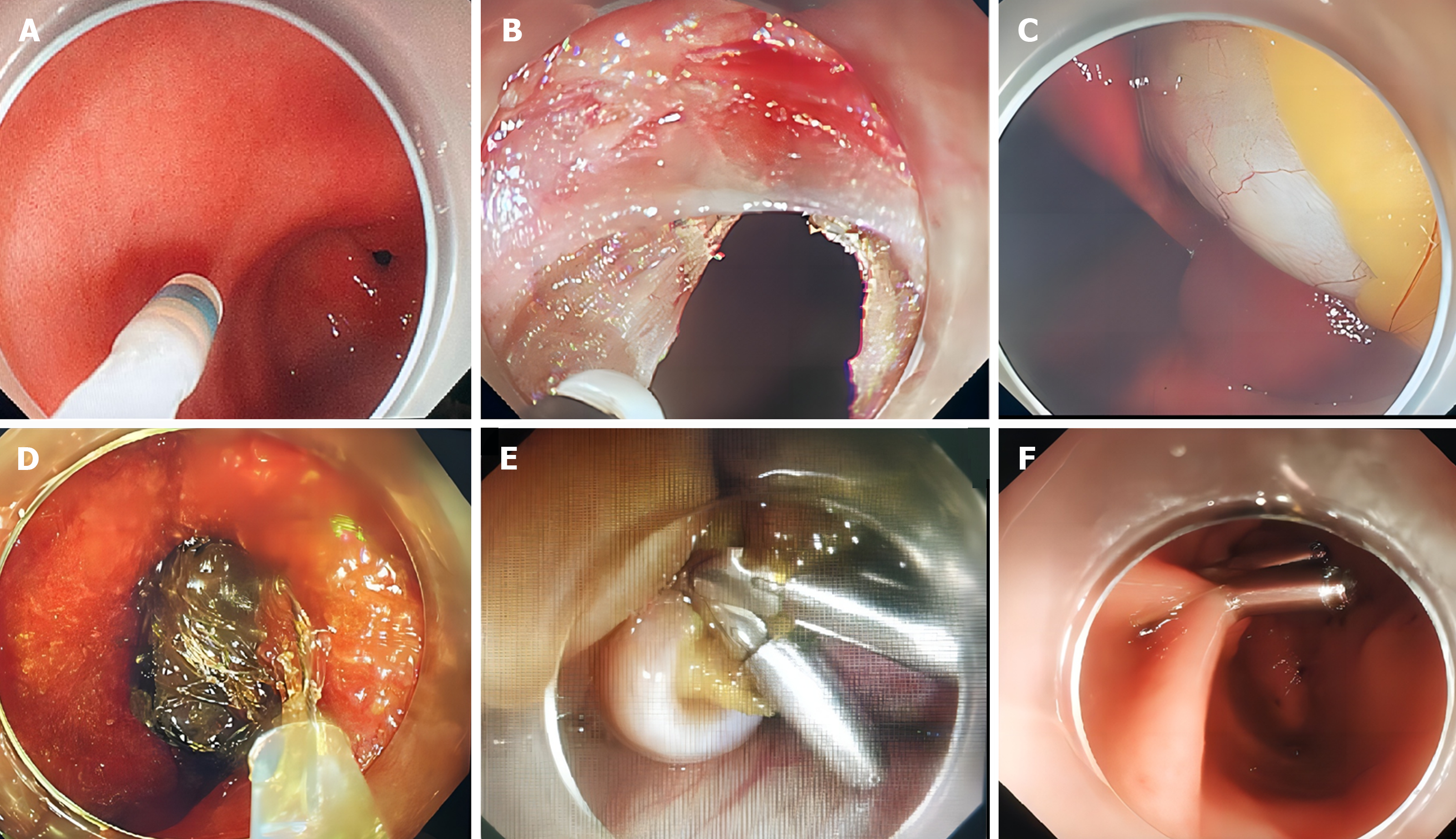
EGPS: The procedure was performed by one experienced physician, with the patient under general anesthesia in the supine position. The gastroscope was advanced into the anterior wall of the stomach, a full-thickness incision about 1.5 cm was made by Hook and IT knives, the endoscope entered the abdominal cavity and identified the gallbladder. Using the Hook and IT knife cut a full-thickness incision in the gallbladder wall. Bile was aspirated, and the gallbladder cavity was flushed by normal saline repeatedly,. the gallstones were removed by using a stone removal basket (E151186, GMBH FLEX, Germany). The gallbladder cavity was flushed with normal saline and aspirated again to ensure that all the gallstones were removed. The gallbladder incision was closed with endoclips (HX-610-090, Olympus, Tokyo, Japan). Flushed the abdominal cavity with saline, and the fluid was aspirated completely. Then, the endoscope was withdrawn into the gastric cavity, used endoclips and endoloops (HX-400U-30, OLYMPUS, Tokyo, Japan) closed the incision (Figure 1).
According to the inclusion and exclusion criteria, a total of 662 cases were collected, including 589 cases of LC (LC group) and 73 cases of transgastric EGPS (EGPS group).
The primary objective of this study was to compare patients' postoperative gastrointestinal symptom efficacy, surgery duration, hospital stay, postoperative short-term adverse events, postoperative analgesic requirements, and costs. Secondary objectives are to determine the gallstone recurrence rate and stone recurrence factors after EGPS.
Baseline data, were collected for all patients including gender, age, body mass index (BMI) and number of gallstones, preoperative and postoperative the Chinese version of Gastrointestinal Quality of Life Index (CGIQLI)[8] of patients. Short-term adverse events after LC include biliary fistula, bile duct injury, intestinal fistula, intestinal injury, delayed wound healing, and gallbladder fossa effusion, etc. Short-term adverse events after EGPS include gastric fistula, biliary fistula, and intestinal fistula, etc.
There are already studies[8] to demonstrate that the performance characteristics of the CGIQLI are equivalent to the English version, the CGIQLI. The CGIQLI is a valid tool to evaluate adults with chronic gastrointestinal problems among the Chinese-speaking population[8]. The CGIQLI has four subscales. The physical well-being subscale includes item 8, item 15, item 16, item 18, item 19, item 20, item 21, item 22, item 23, item 33. The mental well-being subscale includes item 10, item 11, item 12, item 13, and item 14. The gastrointestinal digestion subscale includes item 1, item 2, item 3, item 4, item 5, item 6, item 27, item 28, item 32, item 35. The gastrointestinal defecation subscale includes item 7, item 26, item 30, item 31, item 34, and item 36.
The data were analyzed by SPSS 23.0. The measurement data were tested for normality, that conform to the normal distribution are expressed as the mean ± SD, and were compared with the independent-sample t test or paired-sample t test; the skewed distribution is expressed as the median [interquartile range (IQR)], compared with the Mann-Whitney test. Comparison of enumeration data were performed using either the Pearson's chi-squared test or the Fisher's precision probability test. We used a 1:1 propensity score matching (PSM) with the EGPS groups and LC groups, and the caliper value was fixed at 0.05 for the propensity matching score. We used logistic regression models for the calculation of propensity scores. The study cohort was matched for clinical baseline indicators, including age, gender, BMI, number of gallstones, preoperative CGIQLI score and follow-up time.
There were statistical differences in age, preoperative CGIQLI scores and scores of each subscale scores between the two groups before propensity score matching. 40 patients were included in the two groups after matching, and there was no statistically difference from baseline information, preoperative scores and follow-up time between the two groups (Table 1). The median surgery duration was 100 (IQRs, 85-115) min in the EGPS group, which was longer than that in the LC group, with a median time of 67 (IQRs, 40-95) min. The median length of hospital stay in the EGPS group was 8 (IQRs, 7-10) d vs 5 (IQRs, 3-7) d in the LC group. The mean cost was 24084 ± 5740 RMB in the EGPS group vs 18421 (IQRs, 15532-21311) RMB in the LC group (Table 2).
| Characteristics | Before propensity score matching | After propensity score matching | ||||
| LC group (n = 589) | EGPS group (n = 73) | P value | LC group (n = 40) | EGPS group (n = 40) | P value | |
| Sex | 0.576 | 0.251 | ||||
| Male | 205 | 23 | 18 | 13 | ||
| Female | 384 | 50 | 22 | 27 | ||
| Age | 52 (41, 60) | 43 (33, 52) | 0.000 | 43 ± 12 | 44 ± 11 | 0.817 |
| BMI | 25 (23, 28) | 22 (20, 25) | 0.267 | 25 ± 4 | 25 ± 3 | 0.681 |
| Number of gallstones | 0.355 | 0.644 | ||||
| Single | 199 | 26 | 16 | 14 | ||
| Multiple | 390 | 47 | 24 | 26 | ||
| Preoperative CGIQLI score | 130 (127, 132) | 135 (133, 137) | 0.000 | 134 (131, 136) | 133 (132, 135) | 0.526 |
| Physical well-being | 35 (34, 37) | 37 (35.5, 38) | 0.000 | 37 (35, 38) | 36 (35, 37) | 0.345 |
| Mental well-being | 17 (16, 17) | 19 (19, 20) | 0.000 | 19 (19, 19) | 19(19, 19) | 0.690 |
| Gastrointestinal digestion | 35 (34, 36) | 36 (34, 37) | 0.000 | 35 (34, 36) | 35 (34, 36) | 0.692 |
| Gastrointestinal defecation | 23 (22, 24) | 24 (24, 24) | 0.003 | 24 (23, 24) | 24 (24, 24) | 0.653 |
| Follow-up time | 692 (544, 842) | 676 (590, 810) | 0.610 | 718 (488, 898) | 747 ± 154 | 0.256 |
| LC group (n = 589) | EGPS group (n = 73) | P value | |
| Hospital stay (d) | 5 (3, 7) | 8 (7, 10) | 0.000 |
| Surgery duration (min) | 67 (50, 95) | 100 (85, 117) | 0.000 |
| Cost (RMB) | 18421 (15532, 21311) | 24084 ± 5740 | 0.000 |
| Short-term adverse event | 3 | 1 | 0.374 |
There were statistical differences in total scores and subscale scores between the patients in the groups. There was no statistical difference in preoperative total scores between the two groups after PSM. The total score of the patients in both groups was improved after surgery compared with that before operation (P < 0.05). In the EGPS groups, physical well-being, mental well-being and gastrointestinal digestion demonstrated significant difference than preoperative scoring. Gastrointestinal defecation was no statistical change compared with pre-operation. In LC group, physical well-being, gastrointestinal digestion and gastrointestinal defecation demonstrated significant difference than preoperative scoring (Table 3). There was no statistical difference in physical well-being, mental well-being and gastrointestinal digestion subscale scores between the groups in the postoperative comparison between the LC group and EGPS group, but there was a statistical difference in the subscale score of gastrointestinal digestion (Table 4).
| Preoperative | Postoperative | P value | |
| EGPS group | |||
| Total CGIQLI score | 133 (132, 135) | 141 (140, 142) | 0.000 |
| Physical well-being | 36 (35, 37) | 40 (40, 40) | 0.000 |
| Mental well-being | 19(19, 19) | 20 (20, 20) | 0.000 |
| Gastrointestinal digestion | 35 (34, 36) | 38 (37, 38) | 0.000 |
| Gastrointestinal defecation | 24 (24, 24) | 24 (24, 24) | 0.603 |
| LC group | |||
| Total CGIQLI score | 134 (131, 136) | 140 (137, 142) | 0.001 |
| Physical well-being | 37 (35, 38) | 40 (39, 40) | 0.000 |
| Mental well-being | 19 (19, 19) | 20 (19, 20) | 0.081 |
| Gastrointestinal digestion | 35 (34, 36) | 38 (37, 39) | 0.000 |
| Gastrointestinal defecation | 24 (23, 24) | 24 (23, 24) | 0.004 |
| EGPS group | LC group | P value | |
| Preoperative total CGIQLI score | 134 (131, 136) | 133 (132, 135) | 0.526 |
| Physical well-being | 37 (35, 38) | 36 (35, 37) | 0.345 |
| Mental well-being | 19 (19, 19) | 19(19, 19) | 0.690 |
| Gastrointestinal digestion | 35 (34, 36) | 35 (34, 36) | 0.692 |
| Gastrointestinal defecation | 24 (23, 24) | 24 (24, 24) | 0.653 |
| Postoperative total CGIQLI score | 141 (140, 142) | 140 (137, 142) | 0.063 |
| Physical well-being | 40 (40, 40) | 40 (39, 40) | 0.094 |
| Mental well-being | 20 (20, 20) | 20 (19, 20) | 0.253 |
| Gastrointestinal digestion | 38 (37, 38) | 38 (37, 39) | 0.685 |
| Gastrointestinal defecation | 24 (24, 24) | 24 (23, 24) | 0.002 |
Among the 589 patients included in the LC group, 1 patient had intraperitoneal hemorrhage, 2 patients had postoperative intestinal fistula, they were discharged after reoperation. Among the 73 patients included in the EGPS group, 1 patient suffered gastric fistula (Table 2).
IV Flurbiprofen axil (100 mg) was routinely given after LC. Patients after EGPS were not routinely given analgesics, and the nonsteroidal anti-inflammatory drugs was given when the Numerical Rating Scale was more than three points.
Among the 73 patients included in the EGPS group, 1 patient underwent LC one year after EGPS because of recurrent acute cholecystitis. There were 6 patients with recurrent gallbladder stones, 2 of these 6 patients had recurrence of stones 6 months after surgery, 1 case of 13-month stone recurrence, 1 case of 14-month stone recurrence, and the remaining 2 cases of recurrence of stones at 20 months and 23 months after surgery, respectively. The risk factors of recurrence after EGPS were also analyzed (Table 5). In this study, recurrence after EGPS was not correlated with the gender, age, BMI, number of stones, and preoperative CGIQLI total score.
| No recurrence group (n = 67) | Recurrence group (n = 6) | P value | |
| Sex | 0.371 | ||
| Male | 20 | 3 | |
| Female | 47 | 3 | |
| Age | 42 (33, 51) | 50.8 ± 11.4 | 0.074 |
| BMI | 25.0 ± 3.6 | 25.5 ± 1.9 | 0.730 |
| Number of gallstones | 1.000 | ||
| Single | 24 | 2 | |
| Multiple | 43 | 4 | |
| Preoperative total CGIQLI score | 135 (133, 137) | 136.5 ± 11.7 | 0.163 |
In 2015, Liu et al[9] reported transrectal NOTES cholelithotomy firstly, and in 2018, Wang et al[10] reported transgastric NOTES cholelithotomy. Some scholars[11] believe that NOTES cholelithotomy has the advantages of small wound, less pain, faster recovery, fewer complications, and low tumor recurrence rate, and there are currently three approaches to cholelithotomy: transgastric approach, transintestinal approach, and transvaginal approach. Among them, the prospect of transgastric NOTES has good prospects, the indications are wide, which is worthy of further study.
With the help of CGIQLI, this study compared the efficacy of gastrointestinal symptoms after different surgeries. Before PSM, there were no significant differences in gender, BMI, number of gallstones, and follow-up time between the two groups, the age of the EGPS group was younger than the LC group, and CGIQLI scores was higher than the LC group, so it was considered that the two groups were not completely comparable before surgery. In order to eliminate interfering factors between groups, the PSM was carried out, which can effectively balance the distribution and composition of characteristic variables among the comparison groups. However, propensity score matching can lead to some problems such as overmatching. At the same time, some sample may be lost after matching, and only 40 sets of data were included after matching in our study. There were no statistically significant differences in gender, age, BMI, number of gallstones, follow-up time, total score and four subscales between the two groups after PSM.
At the follow-up after nearly two years after surgery, the scores of patients in both groups improved compared with those before surgery. Therefore, we believed that both Cholecystectomy and gallbladder-sparing surgery have the potential to improve the quality of life of patients. The effect of defecation was smaller in EGPS, and the mental well-being improvement patients was not obvious in LC.
Secondly, there was no significant difference in total score and physical well-being, mental well-being and gastr
However, EGPS carries a risk of stone recurrence. Among the 73 patients with gallbladder conserving who were included, 6 cases of recurrent gallstones occurred during the postoperative follow-up time, with a recurrence rate of 8.2%. Among the 6 patients who relapsed, 3 were males and 3 were females, with a mean age of 50.8 ± 11.4 years. The recurrence factors after EGPS were analyzed: the recurrence after gallbladder preservation was not correlated with the gender, age, BMI, number of stones, and preoperative GIQIL score. Study has reported[15] that gallbladder contraction, thickness of the gallbladder wall beyond 3 mm and gallstone incarceration are important risk factors for recurrent[15]. Pan[16] showed that family history of gallstones, a greasy diet, and number of gallstones were independent influencing factors for stone recurrence. Our conclusions are inconsistent with Pan's conclusions, and it is considered that it may be related to the less sample (177 cases included in Pan's study), the relatively short follow-up time [the follow-up time of Pan's study was 45.0 (17.5-74.0) months], and different surgical methods. Our center will further conduct a larger sample and longer follow-up period of study. All the patients in this study were accompanied by chronic cholecystitis, with a gallbladder wall thickness of 3-4 mm; and some patients completed the gallbladder contraction test (33 cases, 45.2%), and the gallbladder contraction function of the patients who completed the gallbladder contraction test was 45% ± 22%.It has been reported that advanced age, female gender, rapid weight loss, obesity, diet, dyslipidemia, type 2 diabetes, metabolic syndrome, estrogen replacement therapies, estrogen oral contraceptives, genetic factors, and have been found to be associated with increased gallstone occurrence[17]. Gu et al[18] suggested that personalized gallstone prevention strategies could be developed by screening people at high risk of gallstones in the population. It is possible to screen high-risk groups strictly grasp the guidelines for gallbladder conserving surgery, and on the other hand, formulate individualized plans for gallbladder patients after surgery, including guidance on daily living styles such as low-fat diet, behavioral changes, etc[19]. It was reported that the incidence of gastric fistula and intestinal fistula after EGPS was 13.6% (3/22) 73 patients had no intestinal fistula after surgery, 1 patient had abdominal pain and abdominal distention after surgery, abdominal tenderness and rebound tenderness obviously in physical examination. After gastrointestinal decompression, the patient's symptoms did not improve significantly, and the related indicators of blood image infection were higher than before; so, gastroscopy was performed again, see that the endoclips in the incision was fixed in place, the original stoma was after inflation, we considered it was gastric fistula. We used endoclips and endoloops closed the incision again. Patient was fasted, we gave proton pump inhibitors through. We observed the drainage fluid through the nasogastric tube. Then the patient was discharged after surgery again. In this case, these adverse events were considered suture-related.
In our experience, stones less than 3 cm can be safe. If the stone larger than 3 cm, it will be difficult to take the stone with basket on the one hand, and through the oropharynx on the other.
The limitation of this study is that this study was conducted in a single center, and selection bias cannot be ruled out. This study was retrospective, and there was a risk of recall bias. At present, our center only performs EGPS, so it is not possible to make further comparisons of different approaches to cholelithotomy. The limited number of patients and short follow-up duration of the patients also may lead to bias.
In conclusion, both LC and EGPS can improve the quality of life of patients with gallstones, and the diarrhea problem after LC is more obvious than that of EGPS. The recurrence after gallbladder preservation in this study was not correlated with the gender, age, BMI, number of stones, and preoperative score of the patients, which was inconsistent with the conclusions of previous studies, and may be related to the different procedure, the less sample size, the shorter follow-up time. It is hoped that further large-sample, multicenter, prospective, and long-term follow-up studies will be conducted to analyze and evaluate the postoperative quality of life, the rate of stone recurrence, and the factors of stone recurrence.
| 1. | Kratzer W, Klysik M, Binzberger A, Schmidberger J; EMIL-Study group. Gallbladder stone incidence and prevalence in Germany: a population-based study. Z Gastroenterol. 2021;59:859-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 2. | Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, van Erpecum KJ, van Laarhoven CJ, Wang DQ. Gallstones. Nat Rev Dis Primers. 2016;2:16024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 590] [Cited by in RCA: 514] [Article Influence: 57.1] [Reference Citation Analysis (0)] |
| 3. | Guo SH. [Ten physiological functions of the human gallbladder]. Zhonghua Gandan Waike Zazhi. 2021;397-400. [DOI] [Full Text] |
| 4. | Zackria R, Lopez RA. Postcholecystectomy Syndrome. 2023 Aug 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024. [PubMed] |
| 5. | Barrett M, Asbun HJ, Chien HL, Brunt LM, Telem DA. Bile duct injury and morbidity following cholecystectomy: a need for improvement. Surg Endosc. 2018;32:1683-1688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 6. | Li YD, Liu BN, Zhao SH, Zhou YL, Bai L, Liu EQ. Changes in gut microbiota composition and diversity associated with post-cholecystectomy diarrhea. World J Gastroenterol. 2021;27:391-403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (3)] |
| 7. | Nogueira L, Freedman ND, Engels EA, Warren JL, Castro F, Koshiol J. Gallstones, cholecystectomy, and risk of digestive system cancers. Am J Epidemiol. 2014;179:731-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 98] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 8. | Lien HH, Huang CC, Wang PC, Chen YH, Huang CS, Lin TL, Tsai MC. Validation assessment of the Chinese (Taiwan) version of the Gastrointestinal Quality of Life Index for patients with symptomatic gallstone disease. J Laparoendosc Adv Surg Tech A. 2007;17:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Liu B, Du B, Pan Y. Video of the Month: Transrectal Gallbladder-Preserving Cholecystolithotomy via Pure Natural Orifice Transluminal Endoscopic Surgery: First Time in Humans. Am J Gastroenterol. 2015;110:1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Wang YL, Xia SH, Li H, Gao F, Qi LN, Xia WZ, Yang SX, Li J. [Transgastric natural orifice transluminal endoscopic gallbladder-preserving surgery: Report of three cases]. Shijie Huaren Xiaohua Zazhi. 2018;26:1423-1428. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Chen JH, Cheng ZY, Jiang WL, Shen J, Zong GZ, Zhao QY, Xiao WQ, Shen SE, Wang CY, Zhong YS, Wang LW, Wan R. [Current status and development of natural orifice translumenal endoscopic surgery for gallbladder-preserving stone extraction]. Zhonghua Xiaohua Neijing Zazhi. 2023;40:683-686. [DOI] [Full Text] |
| 12. | Chang JY, Jung HK, Moon CM, Kim SE, Shim KN, Jung SA, Min SK. Development of functional gastrointestinal disorder symptoms following laparoscopic cholecystectomy: a prospective cohort study. Front Med (Lausanne). 2023;10:1248465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Poon D, Law GR, Major G, Andreyev HJN. A systematic review and meta-analysis on the prevalence of non-malignant, organic gastrointestinal disorders misdiagnosed as irritable bowel syndrome. Sci Rep. 2022;12:1949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 14. | Sarashina-Kida H, Negishi H, Nishio J, Suda W, Nakajima Y, Yasui-Kato M, Iwaisako K, Kang S, Endo N, Yanai H, Asagiri M, Kida H, Hattori M, Kumanogoh A, Taniguchi T. Gallbladder-derived surfactant protein D regulates gut commensal bacteria for maintaining intestinal homeostasis. Proc Natl Acad Sci U S A. 2017;114:10178-10183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Zhang XT, Liu HY. [Risk factors of recurrent cholecystolithiasis after cholecystolithotomy with gallbladder conservation evaluated by ultrason-ic measurement[J]]. Yixue Yingxiangxue Zazhi. 2022;32:1751-1754. |
| 16. | Pan WC. Clinical follow-up results and analysis after endoscopic cholelithotomy. Jilin: Jilin University, 2022. |
| 17. | Pak M, Lindseth G. Risk Factors for Cholelithiasis. Gastroenterol Nurs. 2016;39:297-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 87] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 18. | Gu LG, Zheng YM, Xu C, Gao X, Zhou Z, Huang Y, Chu X, Zhao J, Su J, Song WN. [Progress in risk factors for gallstone formation and prevention strategies for stony stage]. Zhonghua Waike Zazhi. 2023;50:557-561. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Ullah S, Zhang JY, Liu D, Zhao LX, Liu BR. Transgastric versus transrectal: Which access route is the best for NOTES gallbladder-preserving gallstone therapy? J Dig Dis. 2023;24:491-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |