Published online May 16, 2024. doi: 10.4253/wjge.v16.i5.244
Revised: April 15, 2024
Accepted: April 24, 2024
Published online: May 16, 2024
Processing time: 53 Days and 7.5 Hours
Constipation is a significant sociomedical problem, which can be caused by vari
Core Tip: Constipation is a common medical problem, especially in the elderly population. Diagnosis of constipation includes history, physical examination, and basic laboratory analyses. Colonoscopy is not a necessary diagnostic method for all patients with constipation. It is indicated if alarm symptoms and signs are present. Colonoscopy in patients with constipation is often compromised by factors that cause “difficult colonoscopy,” as well as poor bowel preparation. Colonoscopy under sedation is of great importance, but it cannot replace a good examination technique. If a total colonoscopy is not possible, it is necessary to repeat the examination or perform a virtual colonoscopy.
- Citation: Popovic DD, Filipovic B. Constipation and colonoscopy. World J Gastrointest Endosc 2024; 16(5): 244-249
- URL: https://www.wjgnet.com/1948-5190/full/v16/i5/244.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i5.244
Constipation is a common problem in everyday medical practice. It has been described to affect 11%-20% of the adult population annually[1]. The prevalence of constipation increases with age[2]; moreover, it is estimated that about 50% of the population aged ≥ 80 years has constipation[2]. While there is no single definition, constipation is most often defined by less than three bowel movements per week[3,4]. Since there are different types of constipation (functional constipation, irritable bowel syndrome - C type, functional defecation disorders, etc.), there are also a variety of diagnostic criteria.
Colonoscopy is the “gold standard” method for the exploration of the colon, and most often includes an examination of the terminal ileum. In addition to being a diagnostic method, colonoscopy is also a therapeutic method. Namely, it is possible to perform polypectomies, endoscopic mucosal resections, endoscopic submucosal dissections, endoscopic hemostasis, dilation and stenting of strictures, and endoscopic tattooing, etc. Colonoscopic treatment of precancerous lesions reduces mortality from colorectal cancer[5].
For the colonoscopy to be performed adequately, in addition to good preparation and good examination technique, it is necessary to know the indications and contraindications for colonoscopy. Based on the recommendations of the American Society for Gastrointestinal Endoscopy (ASGE), gastrointestinal endoscopy (including colonoscopy) is performed if endoscopy findings will change the therapeutic approach, in the case that the attempt to treat a suspected benign disease has had no effect, and if endoscopy is the initial therapeutic modality or endoscopy is an alternative another (usually more invasive) method[6]. The most important fact is that endoscopy is performed only if its findings will change the therapeutic approach. Namely, if the findings of endoscopy have no effect on further treatment, its application only exposes the patient to risk (it must not be forgotten that this is an invasive method) and increases the cost of treatment without any benefit. Based on ASGE recommendations, the most important indications for colonoscopy are[6,7]: (1) Iron deficiency anemia; (2) Gastrointestinal bleeding; (3) Chronic diarrheal syndrome; (4) Early detection of colorectal neoplasia; (5) Evaluation of pathological findings diagnosed by another method (e.g., ultrasonography, contrast radiography, computed tomography (CT), nuclear magnetic resonance); and (6) Use of interventional endoscopic procedures.
In addition to the above, there are other indications for colonoscopy, but constipation is not included among them. Therefore, the question is whether colonoscopy is indicated for patients with constipation. For most patients with constipation, colonoscopy is not a necessary diagnostic method[8]. Namely, adequate diagnostics can be carried out with a detailed medical history, physical examination, and basic laboratory analyses. This is clear if we know that constipation is most often a consequence of functional disorders. Colonoscopy is indicated for patients who, in addition to constipation, have some of the alarm symptoms or signs. Alarm symptoms and signs may suggest the presence of serious organic diseases, and require a detailed examination. The most significant alarm symptoms/signs are[9-12]: (1) Age > 50 years; (2) Gastrointestinal bleeding; (3) New-onset constipation; (4) Palpable mass in the abdomen and rectum; (5) Weight loss; (6) Anemia; (7) Inflammatory bowel disease; and (8) Family history positive for colorectal neoplasia.
They are supported by the results of the published studies. Pepin and Ladabaum[13] conducted a study of 563 patients undergoing colonoscopy. They analyzed the colonoscopic findings of patients with constipation as the only indication for colonoscopy and patients with constipation and some other symptom/sign (most often an alarm one). Patients who have only constipation have a frequency of colorectal cancer at 0% and malignant polyps at 0.4% (n = 1)[6]. In the group of patients with constipation and some other indications for colonoscopy, the frequency of colorectal cancer is significantly higher at 2.4% (n = 8)[6]. Ratnasingham et al[14], in a total of 100 colonoscopies in patients with constipation, detected colon cancer in 1 patient, adenomas in 3, and hyperplastic polyps in 2. In that study, the frequency and reason for incomplete colonoscopy were analyzed. Colonoscopy was incomplete in 37% of cases[14]. The most common reasons were discomfort (51.4%) and poor bowel preparation (27%)[14]. A relatively high percentage of incomplete colonoscopies in that study can be explained by the heterogeneous structure of the endoscopists. Namely, endoscopies were performed by surgeons, gastroenterologists, specialist registrars, or specialist endoscopy nurse practitioners[14].
Most endoscopists do not like having constipated patients for colonoscopy. There are two reasons. Namely, based on the recommendations of the European Association for Gastrointestinal Endoscopy (ESGE), two important measures of endoscopy performance are the cecal intubation rate and the adequacy of preparation[15]. Based on these recommendations, a cecal intubation rate and adequate preparation should be ≥ 90%[15]. Due to the motility and bowel configuration in constipated patients, this is not always possible to achieve. A “difficult colonoscopy” is any colonoscopy in which the endoscopist has difficulty in achieving cecal intubation without significant effort or discomfort to the patient[16]. Factors associated with difficult colonoscopy are[17-20]: (1) Female sex; (2) Younger age or age ≥ 60 years; (3) Lower body mass index; (4) Constipation; (5) Diverticular disease; (6) Inflammatory bowel disease; (7) Previous abdominal or pelvic surgery (especially hysterectomy); (8) Anterior abdominal wall hernia; (9) Hypersensitivity to pain or anxiety; and (10) Colonoscopy in private practice.
In a study by Moon et al[21], it was proven that the predictors of “difficult colonoscopy,” as assessed by the time required for cecum intubation, are female sex, body mass index that is higher or lower than the normal range, and the involvement of a fellow in the colonoscopy procedure. In this study, constipation did not significantly affect cecal intubation time. However, in a study by Anderson et al[22], it was concluded that constipation in men as well as the use of laxatives are predictors of “difficult colonoscopy.” The opinion of the authors of this manuscript is that chronic constipation is associated with difficult colonoscopy. The main reason for a “difficult colonoscopy” is the formation of loops. There are different types of loops, such as N, alpha, reverse alpha, and gamma[23]. The most common colon segment for forming loops is the sigmoid colon. Since most parts of the colon are mobile, and patients with constipation may have an elongated colon, it is understandable why loops are more easily formed in it.
If loops are not detected and resolved in an adequate manner, perforation may occur. Perforation is a rare complication of colonoscopy, which is less common in diagnostic (0.019%-0.8%) than in therapeutic (0.1%-3%) colonoscopy[24]. It can occur as a result of mechanical trauma, barotrauma, and use of electrosurgery, as well as other miscellaneous reasons[2]. The most common localization of perforation is the rectosigmoid colon (53%), followed by the cecum (24%)[2].
The effect of deep sedation on the risk of colonic perforation is quite controversial[25]. In a study by Adeyemo et al[26], among a sample of 118,004 colonoscopies, it was concluded that the use of propofol was associated with an increased risk of colonic perforation. However, Bielawska et al[27], among a sample of 3059045 colonoscopies, did not find an increased risk of perforation if the colonoscopy was performed under anesthesia. The author of this Manuscript (Dusan Dj Popovic) prefers colonoscopy without sedation, including for the group of patients with constipation. A colonoscopy without anesthesia provides better feedback (e.g., bloating, pain), allows more frequent changes in the patient's position, and perhaps most importantly, allows conversation with the patient during the procedure. Pre- and intra-procedural conversation with the patient make the procedure much easier. Of course, anesthesia is very important in certain groups of patients, especially if they have predictors of “difficult colonoscopy,” but it cannot be a substitute for good and careful colonoscopy technique. To make the colonoscopy procedure easier, good examination technique is essential. Good colonoscopy technique implies adequate psychological preparation of the patient, careful insertion of the endoscope with minimal air insufflation, and early detection and resolution of loops.
For a colonoscopy to be performed properly, in addition to an adequate indication, an experienced colonoscopist and good bowel preparation are also necessary. Some of the predictors of poor bowel preparation for colonoscopy, in addition to chronic constipation, are male sex, inpatient colonoscopy, some diseases (stroke, dementia, liver cirrhosis), use of tricyclic antidepressants, non-compliance with preparation instructions, etc.[28,29]. Poor bowel preparation reduces the performance of colonoscopy, primarily reducing the adenoma detection rate, as well as increasing the risk of complications.
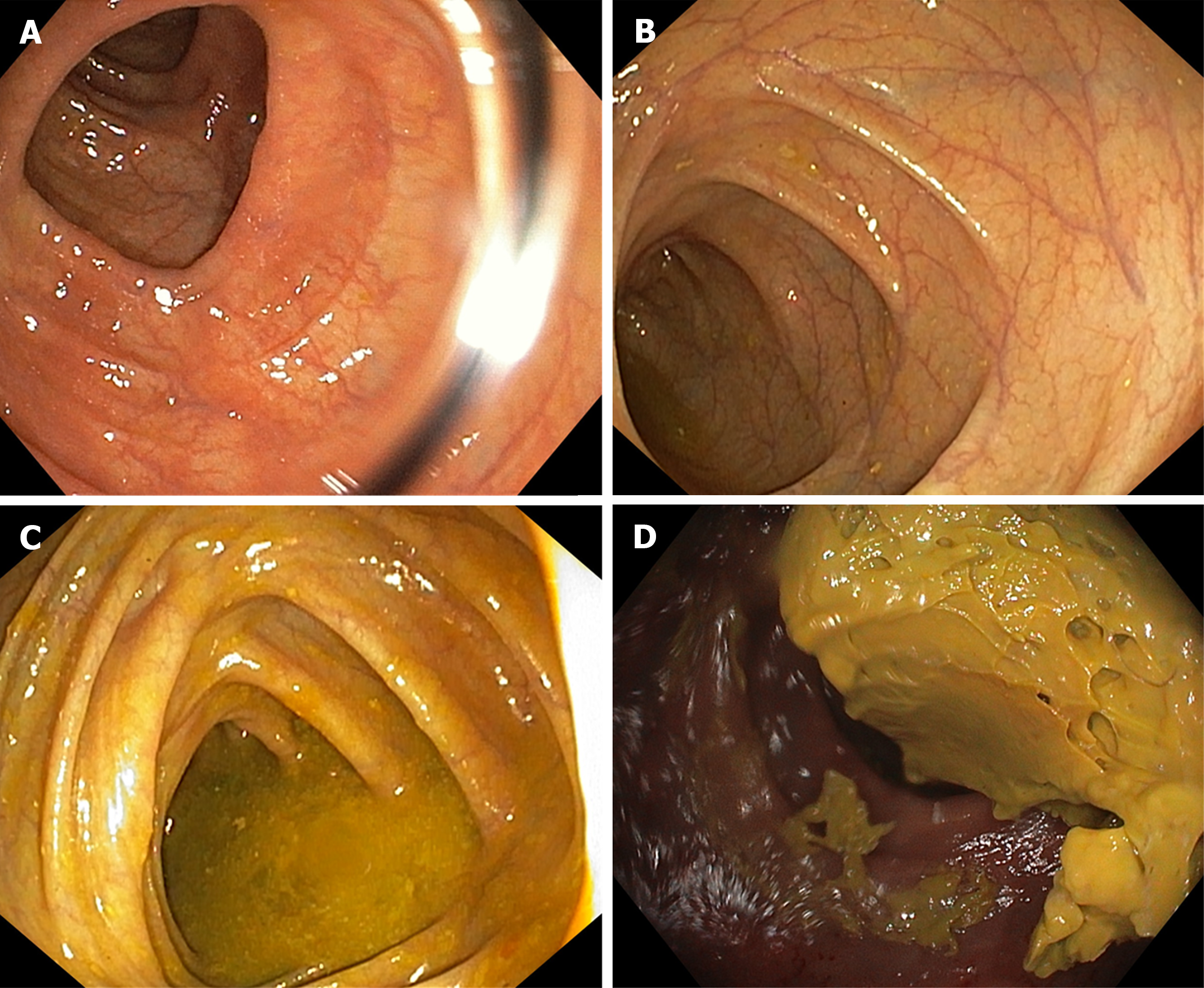
The quality of bowel preparation can be assessed using different, validated scales. The most commonly used one is the Boston Bowel Preparation Scale (BBPS) (Figure 1). Based on this scale, the preparation is scored in the range of 0-3, where a score of 0 represents an unprepared bowel and a score of 3 a clean bowel[30]. The score is determined for each segment of the colon (right colon, transverse, and left colon). The sum is the total BBPS score. The preparation is adequate if the BBPS is ≥ 6[31].
To improve preparation for colonoscopy, ESGE recommends the use of improved preparation guidelines[32]. In the study by Wang et al[33], it was concluded that the use of medication guidance and targeted educational guidance leads to a significant improvement in the quality of bowel preparation and reduces the frequency of side effects in patients with constipation.
Different agents can be used for bowel preparation: High-volume polyethylene glycol (PEG) preparations, low-volume PEG preparations, and non-PEG-based preparations (sodium picosulfate, magnesium citrate, trisulfate, etc.)[32]. The most commonly used agent for colonoscopy preparation is PEG. PEG works as an osmotic laxative. Since it is minimally absorbed in the colon, it osmotically attracts water into the lumen, thus softening the stool and stimulating peristalsis[34].
Based on the recommendations of the ESGE, it is recommended to use the preparation in a split dose, which means that half of the amount of the preparation is taken the day before the examination and the other half on the day of the examination[32]. If the colonoscopy is scheduled for the afternoon, the entire amount of preparation can be taken on the day of the examination[32]. For better bowel preparation, it is advised that the day before the colonoscopy, patients consume food with less than 10 g fiber, and the use of simethicone is also recommended[32]. The use of other preparations as well as the routine use of enemas is not recommended[32]. It is an interesting fact that ESGE does not have specific recommendations for the preparation of patients with constipation, although it is known that this group of patients is the most difficult to prepare for colonoscopy[32].
In a meta-analysis conducted by Dang et al[28], it was concluded that the administration of sodium phosphate (NaP) is superior to PEG in the preparation of patients with constipation [odds ratio (OR) 1.87, 95%CI 1.06–3.32, P = 0.003]. As the authors of that meta-analysis apostrophized, further studies are necessary in which the diagnosis of constipation would be standardized and in which the NaP would be standardized to more accurately assess the effectiveness of both treatments[28]. It would be interesting to see the impact of the combined application of these preparations.
Improvement of bowel preparation in patients with constipation can also be achieved by adding different laxatives to the standard preparation (e.g., bisacodyl, lactulose, lubiprostone)[29]. If laxatives (bisacodyl, lactulose, senna), prokinetics (mosapride), or probiotics are added to the standard preparation (PEG or NaP), the quality of the bowel preparation improves (OR 2.19, 95%CI 1.16–4.17; P = 0.02)[35]. Although there are no current recommendations for the preparation of patients with constipation, in daily practice, prolonged preparation (usually 2 d), counseling of increased fluid intake, and sometimes the addition of bisacodyl to the preparation, are most often used. A case has been described where adequate preparation required 5 d of a clear liquid diet and 5 gallons of PEG[19]. However, each patient with con
Sometimes, despite all preparation measures and adequate examination techniques, it is not possible to perform a total colonoscopy in all patients with constipation. According to the author of the Manuscript (Dusan Dj Popovic), two approaches are rational in that case. One is to repeat the colonoscopy under anesthesia, the next day, by the same or a more experienced endoscopist, and the other is to refer the patient directly to a virtual colonoscopy. It would be ideal to perform CT colonography on the same day to avoid re-preparation of the patient for the examination. Ratnasingham et al[14] described that only one colorectal cancer was detected in a sample of 100 patients with constipation and that the method was successful in all patients. Based on these results, the authors suggest that CT colonography may be an acceptable first-line method in constipated patients.
Which of these two approaches will be chosen depends on several factors: General condition of the patient and comorbidities, availability of methods, and personnel, etc. However, if there is a clinical suspicion of the existence of an organic cause of constipation in the proximal, unexamined parts of the colon, it is always best to try the colonoscopy again. What must always be kept in mind is that CT colonography is associated with exposure to a significant dose of radiation and does not allow for the application of interventional procedures.
Constipation is a significant sociomedical problem, which can be caused by various reasons. A colonoscopy is not a necessary diagnostic method for all patients with constipation. It is indicated if alarm symptoms and signs are present. Most endoscopists do not like to deal with patients with constipation. There are two reasons: The difficulty of endoscopy and the adequacy of preparation. If a total colonoscopy is not possible, it is necessary to repeat the examination or perform a virtual colonoscopy.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: Serbia
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Machado NC, Brazil S-Editor: Li L L-Editor: A P-Editor: Cai YX
| 1. | Schiller LR. Chronic constipation: new insights, better outcomes? Lancet Gastroenterol Hepatol. 2019;4:873-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 2. | Rai V, Mishra N. Colonoscopic Perforations. Clin Colon Rectal Surg. 2018;31:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Barbara G, Barbaro MR, Marasco G, Cremon C. Chronic constipation: from pathophysiology to management. Minerva Gastroenterol (Torino). 2023;69:277-290. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel Disorders. Gastroenterology. 2016;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1781] [Cited by in RCA: 1901] [Article Influence: 211.2] [Reference Citation Analysis (3)] |
| 5. | Zauber AG, Winawer SJ, O'Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, Shi W, Bond JH, Schapiro M, Panish JF, Stewart ET, Waye JD. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1952] [Cited by in RCA: 2288] [Article Influence: 176.0] [Reference Citation Analysis (2)] |
| 6. | Early DS, Ben-Menachem T, Decker GA, Evans JA, Fanelli RD, Fisher DA, Fukami N, Hwang JH, Jain R, Jue TL, Khan KM, Malpas PM, Maple JT, Sharaf RS, Dominitz JA, Cash BD; ASGE Standards of Practice Committee. Appropriate use of GI endoscopy. Gastrointest Endosc. 2012;75:1127-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 179] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 7. | Popović D. Gastroenterološki pristup krvarenju iz digestivnog trakta. Beograd: Medicinski fakultet Univerziteta u Beogradu CIBID, 2022: 25-27. |
| 8. | Black CJ, Ford AC. Chronic idiopathic constipation in adults: epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust. 2018;209:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 131] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 9. | Milosavljevic T, Popovic DD, Mijac DD, Milovanovic T, Krstic S, Krstic MN. Chronic Constipation: Gastroenterohepatologist's Approach. Dig Dis. 2022;40:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Brandt LJ, Prather CM, Quigley EM, Schiller LR, Schoenfeld P, Talley NJ. Systematic review on the management of chronic constipation in North America. Am J Gastroenterol. 2005;100 Suppl 1:S5-S21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 176] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 11. | Cho YS, Lee YJ, Shin JE, Jung HK, Park SY, Kang SJ, Song KH, Kim JW, Lim HC, Park HS, Kim SJ, Cha RR, Bang KB, Bang CS, Yim SK, Ryoo SB, Kye BH, Ji WB, Choi M, Sung IK, Choi SC; Korean Society of Neurogastroenterology and Motility. 2022 Seoul Consensus on Clinical Practice Guidelines for Functional Constipation. J Neurogastroenterol Motil. 2023;29:271-305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 12. | Sadler K, Arnold F, Dean S. Chronic Constipation in Adults. Am Fam Physician. 2022;106:299-306. [PubMed] |
| 13. | Pepin C, Ladabaum U. The yield of lower endoscopy in patients with constipation: survey of a university hospital, a public county hospital, and a Veterans Administration medical center. Gastrointest Endosc. 2002;56:325-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Ratnasingham K, Lo T, Jamal K, Varatharajan L, Tabbakh Y, Kaderbhai H, West NJ. The role of colonoscopy and CT colonography in patients presenting with symptoms of constipation. Br J Radiol. 2017;90:20160147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Kaminski MF, Thomas-Gibson S, Bugajski M, Bretthauer M, Rees CJ, Dekker E, Hoff G, Jover R, Suchanek S, Ferlitsch M, Anderson J, Roesch T, Hultcranz R, Racz I, Kuipers EJ, Garborg K, East JE, Rupinski M, Seip B, Bennett C, Senore C, Minozzi S, Bisschops R, Domagk D, Valori R, Spada C, Hassan C, Dinis-Ribeiro M, Rutter MD. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2017;49:378-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 487] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 16. | Watson RR. Accessing a Difficult Colon. Gastroenterol Hepatol (N Y). 2021;17:79-81. [PubMed] |
| 17. | Wei MT, Friedland S. Strategies to manage the difficult colonoscopy. World J Gastrointest Endosc. 2023;15:491-495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Shah HA, Paszat LF, Saskin R, Stukel TA, Rabeneck L. Factors associated with incomplete colonoscopy: a population-based study. Gastroenterology. 2007;132:2297-2303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 267] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 19. | Rex DK. How I Approach Colonoscopy in Anatomically Difficult Colons. Am J Gastroenterol. 2020;115:151-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Prospective evaluation of factors predicting difficulty and pain during sedation-free colonoscopy. Dis Colon Rectum. 2005;48:1295-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 89] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | Moon SY, Kim BC, Sohn DK, Han KS, Kim B, Hong CW, Park BJ, Ryu KH, Nam JH. Predictors for difficult cecal insertion in colonoscopy: The impact of obesity indices. World J Gastroenterol. 2017;23:2346-2354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Anderson JC, Messina CR, Cohn W, Gottfried E, Ingber S, Bernstein G, Coman E, Polito J. Factors predictive of difficult colonoscopy. Gastrointest Endosc. 2001;54:558-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 179] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 23. | Roberts-Thomson IC, Teo E. Colonoscopy: Art or science? J Gastroenterol Hepatol. 2009;24:180-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Cai SL, Chen T, Yao LQ, Zhong YS. Management of iatrogenic colorectal perforation: From surgery to endoscopy. World J Gastrointest Endosc. 2015;7:819-823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 25. | Sidhu R, Turnbull D, Haboubi H, Leeds JS, Healey C, Hebbar S, Collins P, Jones W, Peerally MF, Brogden S, Neilson LJ, Nayar M, Gath J, Foulkes G, Trudgill NJ, Penman I. British Society of Gastroenterology guidelines on sedation in gastrointestinal endoscopy. Gut. 2024;73:219-245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 40] [Article Influence: 40.0] [Reference Citation Analysis (1)] |
| 26. | Adeyemo A, Bannazadeh M, Riggs T, Shellnut J, Barkel D, Wasvary H. Does sedation type affect colonoscopy perforation rates? Dis Colon Rectum. 2014;57:110-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Bielawska B, Hookey LC, Sutradhar R, Whitehead M, Xu J, Paszat LF, Rabeneck L, Tinmouth J. Anesthesia Assistance in Outpatient Colonoscopy and Risk of Aspiration Pneumonia, Bowel Perforation, and Splenic Injury. Gastroenterology. 2018;154:77-85.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 28. | Dang JT, Moolla M, Dang TT, Shaw A, Tian C, Karmali S, Sultanian R. Sodium phosphate is superior to polyethylene glycol in constipated patients undergoing colonoscopy: a systematic review and meta-analysis. Surg Endosc. 2021;35:900-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Shahini E, Sinagra E, Vitello A, Ranaldo R, Contaldo A, Facciorusso A, Maida M. Factors affecting the quality of bowel preparation for colonoscopy in hard-to-prepare patients: Evidence from the literature. World J Gastroenterol. 2023;29:1685-1707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 30] [Article Influence: 15.0] [Reference Citation Analysis (10)] |
| 30. | Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009;69:620-625. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 930] [Cited by in RCA: 925] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 31. | Kaminski MF, Thomas-Gibson S, Bugajski M, Bretthauer M, Rees CJ, Dekker E, Hoff G, Jover R, Suchanek S, Ferlitsch M, Anderson J, Roesch T, Hultcranz R, Racz I, Kuipers EJ, Garborg K, East JE, Rupinski M, Seip B, Bennett C, Senore C, Minozzi S, Bisschops R, Domagk D, Valori R, Spada C, Hassan C, Dinis-Ribeiro M, Rutter MD. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. United European Gastroenterol J. 2017;5:309-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 177] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 32. | Hassan C, East J, Radaelli F, Spada C, Benamouzig R, Bisschops R, Bretthauer M, Dekker E, Dinis-Ribeiro M, Ferlitsch M, Fuccio L, Awadie H, Gralnek I, Jover R, Kaminski MF, Pellisé M, Triantafyllou K, Vanella G, Mangas-Sanjuan C, Frazzoni L, Van Hooft JE, Dumonceau JM. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2019. Endoscopy. 2019;51:775-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 356] [Article Influence: 59.3] [Reference Citation Analysis (4)] |
| 33. | Wang H, Wang Y, Yuan JH, Wang XY, Ren WX. Pre-colonoscopy special guidance and education on intestinal cleaning and examination in older adult patients with constipation. World J Gastrointest Surg. 2022;14:778-787. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (1)] |
| 34. | Izzy M, Malieckal A, Little E, Anand S. Review of efficacy and safety of laxatives use in geriatrics. World J Gastrointest Pharmacol Ther. 2016;7:334-342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (2)] |
| 35. | Ding L, Duan J, Yang T, Jin C, Luo J, Ma A. Advanced intestinal regulation improves bowel preparation quality in patients with constipation: A systematic review and network meta-analysis. Front Pharmacol. 2022;13:964915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |