Published online Apr 16, 2024. doi: 10.4253/wjge.v16.i4.178
Peer-review started: December 29, 2023
First decision: January 23, 2024
Revised: January 28, 2024
Accepted: March 6, 2024
Article in press: March 6, 2024
Published online: April 16, 2024
Processing time: 104 Days and 4 Hours
Obesity is a chronic, progressive, and relapsing disease of excess adiposity that contributes to more than two hundred medical conditions and is projected to affect more than half the adult population of the United States by the year 2030. Given the limited penetrance of traditional bariatric surgery, as well as the cost and adherence barriers to anti-obesity medications, there is growing interest in the rapidly evolving field of endoscopic bariatric therapies (EBTs). EBTs are minimally invasive, same-day, per-oral endoscopic procedures and include endoscopic sleeve gastroplasty, intragastric balloons, and endoscopic bariatric revisional procedures. This field represents an exciting and innovative subspecialty within gastroenterology. However, building a successful endoscopic bariatric practice requires intentional, coordinated, and sustained efforts to overcome the numerous obstacles to entry. Common barriers include acquisition of the technical and cognitive skillset, practice limitations including the availability of nutrition counseling, facility capabilities, direct-to-consumer marketing, and financial pressures such as facility and anesthesia fees. As the highest-volume center for metabolic and bariatric endoscopy in the United States, we provide insights into successfully establishing an endoscopic bariatric program.
Core Tip: In this editorial, we outline and examine the key components of building an endoscopic bariatric program including the endoscopic skillset, the cognitive approach, equipment needs, marketing and financial considerations, program infrastructure, and the practice model.
- Citation: Maselli DB, Donnangelo LL, Coan B, McGowan CE. How to establish an endoscopic bariatric practice. World J Gastrointest Endosc 2024; 16(4): 178-186
- URL: https://www.wjgnet.com/1948-5190/full/v16/i4/178.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i4.178
Obesity is a chronic, progressive, relapsing, and multifactorial disease[1]. It is characterized by excess adiposity that leads to metabolic and mechanical dysfunction, driving over two hundred weight-related medical conditions[2]. By 2030, nearly one in two adults in the United States will be affected by obesity, which underscores the pressing need for acceptable treatment options[3]. Patients with obesity warrant multiple therapeutic options that can be tailored to their specific needs and risk tolerance. The therapeutic landscape is evolving but still faces certain challenges. Metabolic and bariatric surgery reaches only 1%-2% of the eligible adult population in the United States, primarily due to concerns about invasiveness and risk[4-6]. Incretin-based agents have revolutionized anti-obesity pharmacotherapy but have limitations of cost, tolerability, reliable access, and high probability of weight recurrence following discontinuation[7-10].
Endoscopic bariatric therapies (EBTs) have emerged in the past decade as a viable alternative within the multidisciplinary approach to obesity management, particularly for those seeking a less invasive option than surgery[11,12]. EBTs are minimally-invasive, same-day, per-oral procedures that facilitate clinically meaningful weight loss in adults with obesity. These include primary obesity therapies, including intragastric balloons (IGBs)[13,14] and endoscopic sleeve gastroplasty (ESG)[15,16], as well as revisional therapies for weight return after metabolic and bariatric surgery, such as transoral outlet reduction (TORe)[17,18] and vertical sleeve gastrectomy revision (VSG-R)[19] (Table 1). The commercially available EBTs have been thoroughly presented in recent reviews[20,21]. Existing procedures target gastric restriction, acting through visceroceptive pathways to enhance satiety and satiation to facilitate weight loss[22-25]. The future of EBT will very likely additionally involve metabolically-oriented small bowel-targeted therapies[26,27].
| Endoscopic bariatric therapies |
| Food and Drug Administration authorized |
| ESG with Apollo ESGTM |
| Transoral outlet reduction with Apollo reviseTM |
| Orbera® intragastric balloon |
| Spatz3 intragastric balloon |
| Off-label or experimental procedures |
| Endoscopic gastroplasty with Endomina®* |
| Primary obesity surgery endoluminal 2.0 procedure with incisionless operating platform®* |
| Endoscopic revision of vertical sleeve gastrectomy (with Apollo OverStitchTM, Endomina®, or the incisionless operating platform®) |
The metabolic and bariatric endoscopy field (or “endobariatrics”) represents an exciting and growing subspecialty of gastroenterology; however, thoughtful, disciplined, and methodical effort is required to build a successful endobariatric program while overcoming the frequent barriers that may arise (Table 2). As the highest-volume center for metabolic and bariatric endoscopy in the United States, we provide insights into this endeavor.
| Common barriers |
| Lack of practice, administration, departmental, or partner support |
| Endoscopist skillset, specifically endoscopic suturing |
| Facility limitations, particularly the need for general anesthesia capability |
| Cost-prohibitive facility fees |
| Difficulty establishing a cash-pay model |
| Need for nutrition support |
| Inadequate marketing (limited patient awareness) |
| Poor patient intake process |
| External pressures (anti-obesity medication growth and competitive forces) |
Nearly every aspect of the gastrointestinal tract has pathology directly or indirectly impacted by obesity[28,29] and endobariatrics transforms the gastroenterologist from bystander to facilitator in improving those pathways. An appeal of EBT is the interplay between complex medical management and highly technical advanced endoscopic procedures. The bariatric endoscopist must be adept in both areas.
The endoscopic skillset centers on endoscopic suturing. Presently, this is conducted using the Overstitch Endoscopic Suturing System (Boston Scientific, Marlborough, MA, United States). For many gastroenterologists, endoscopic suturing represents an entirely new and different skill set. Mastering endoscopic suturing will present the first challenge in pursuing a career in EBTs. With a dearth of formalized fellowships in EBT, a reasonable way to achieve these skills is through precepted/proctored cases with experts and dedicated suturing courses. Existing courses run by device manufacturers and professional societies, including the American Society for Gastrointestinal Endoscopy, offer structured didactic and wet-lab training. After learning the fundamentals of endoscopic suturing, proficiency, in our experience, requires between 30 and 50 cases per procedure type (e.g., ESG, TORe, and VSG-R), consistent with existing literature[30]. In contrast, IGB placement and extraction can be mastered with a significantly more abbreviated training process, given the overlap with fundamental endoscopic skills. Until more formal EBT fellowship programs develop, training and education in EBTs are likely to remain mostly independent and self-driven[31,32].
The cognitive skillsets of a bariatric endoscopist center around knowledge of obesity, its pathogenesis, path
It is incumbent on the bariatric endoscopist to rigorously track outcomes longitudinally for patients undergoing EBTs, including both safety and efficacy data. These should satisfy, at a minimum, the expert consensus thresholds for clinical adoption of EBT: a serious adverse event rate < 5% and an excess weight loss (EWL) exceeding 25%[12]. While EBTs are safely performed at higher ranges of body mass index (BMI)[15,17,35], it is more commonly performed in class I and II obesity. At this BMI range, EWL may outpace total body weight loss (TBWL); therefore, we recommend tracking TBWL and targeting > 10% TBWL at one year, as this threshold is associated with substantial improvement in obesity-related comorbidities and mortality[36,37]. For a high-volume center, this degree of weight loss is readily achievable with ESG[15,16,38], TORe[17] and VSG-R[19].
While increased physician skillset and longitudinal follow-up can augment the likelihood of sustained success, patients undergoing EBT are not immune from non-response, weight loss plateau, and weight recurrence[39]. The bariatric endoscopist must be comfortable with this reality, the attendant patient dissatisfaction associated with these outcomes in a self-pay model, and the appropriate management steps. ABOM certification can increase one’s ability to recognize contributing medical and behavioral factors and discuss and manage anti-obesity medications. Repeat suturing (for ESG)[40], conversion to ESG (after IGB)[41], and repeat ablation and/or suturing (for TORe)[17,42] are all feasible in these circumstances for the bariatric endoscopist comfortable with such techniques; however, this does present challenges with how to select candidates judiciously based on initial success and their willingness to adhere to strict nutritional follow up[40,41]. Finally, conversion from restrictive gastric EBTs to metabolic and bariatric surgeries is also an option, underscoring the importance of maintaining strong working relationships with bariatric surgeons as part of the multidisciplinary care model for obesity[43,44].
Demographically, patients seeking EBTs resemble those who seek traditional metabolic and bariatric surgery. In a survey of 101 consecutive adults seeking ESG or IGB at our center, nearly 9 in 10 were women, the mean age was 43.2 ± 9.7 years, the mean BMI was 38.8 ± 5.6 kg/m2, and 76.2% had at least one obesity-associated medical problem[11]. The respondents’ weight loss history was also instructive: 63.7% had attempted weight loss ten or more times, 66.3% had used commercial weight loss programs, 66.3% had used over-the-counter weight loss drugs, and 70.3% had used prescription anti-obesity medications. These observations underscore the intractable, chronic, and relapsing nature of obesity, the distressing effects it can have on both health and well-being, and the compassion and understanding that bariatric endoscopists must have to meet patients where they are.
This survey also revealed the importance of a thorough consultation with an experienced medical professional to provide patients with realistic expectations of EBT. Patients may overestimate the weight loss outcomes of EBT treatments, with nearly two-thirds believing they are as effective as traditional bariatric surgery, a view that is not supported by the literature[15,45,46]. Additionally, patients may underestimate risk, with approximately half of respondents failing to recognize that EBTs could induce serious adverse events. Thus, in our practice, about half of the duration of a consult is spent systematically disclosing the technical aspects, benefits, risks, recovery, and alternatives to EBT therapy. These are then provided in detail in a written consent form that patients review and sign before procedure day.
Incorporation of EBT into the gastroenterologist’s practice may be dictated by the existing practice structure. Reasonable approaches include the mixed practice of general gastroenterology and EBTs (perhaps suited for ambulatory private practices) or interventional endoscopy (common in academic/hospital-affiliated centers). Alternatively, the “all in” approach entirely focuses on EBT at the exclusion of other routine endoscopic procedures. We favor the all-in approach as this facilitates a high-volume clinical practice and allows the physician to focus on the medical management of obesity. However, this approach may be impractical or financially unfeasible until one’s practice is well established. Notably, the gastroenterologist should avoid the temptation to “dabble” in EBTs, which may pose diminished efficacy and heightened risk to patients due to inconsistent experience, harming both the patient and the field of EBT.
Regardless of practice type, universal features should be consistent across venues (Table 3). At a minimum, these ought to include: (1) ABOM-certified physician(s) to provide a comprehensive approach to obesity management; (2) consistent volume of EBTs to ensure safety and efficacy; and (3) longitudinal support with a nutrition team[47]. Finally, while safe, EBTs do have rare but serious risks, including gastrointestinal bleeding, which may require emergent endoscopic intervention, as well as interventions that a gastroenterologist cannot typically manage alone—such as a gastric leak, intraabdominal abscess, or perforation—and the need for these services should influence whether EBT can be responsibly offered in the context of any particular call system and practice model[48,49]. While complications from suture-based EBTs are rare beyond the first three weeks from the procedure, IGBs may present with adverse events (e.g., ulceration, gastrointestinal bleeding, hyperinflation, migration with small bowel obstruction, and viscus perforation) at any point during the dwell time; we therefore recommend that centers offering IGBs have unfettered direct access to an on-call physician who can help triage concerning signs of symptoms[13,46,50,51].
| Key components |
| Medical personnel |
| Bariatric endoscopist with obesity medicine certification and sufficient procedural training |
| Advanced practice provider(s) |
| Longitudinal nutrition support |
| Licensed and registered dietitian(s) |
| Certified health and wellness coach(es) |
| Patient intake coordinator(s) |
| Marketing support |
| Facilities |
| General anesthesia capability |
| Experienced pre-op and recovery nurses |
| Anesthesiologist/anesthetists skilled in managing patients with obesity |
| Endoscopy technician |
EBT is a dynamic, rapidly evolving field, and equipment needs will evolve. For now, most endoscopic suturing procedures are performed using the OverStitchTM or OverStitch SXTM Endoscopic Suturing Systems (Boston Scientific, Marlborough, MA, United States). The former is compatible with specific dual-channel endoscopes, and the latter is compatible with single-channel endoscopes. For optimal performance of the TORe procedure, argon plasma coagulation is necessary for ablation of the gastrojejunal anastomosis prior to suturing. Additional EBT-specific equipment requirements are listed in Table 4.
| Equipment commonly used |
| Required |
| Dual-channel endoscope(s) or single-channel gastroscope(s) (if using OverStitch SXTM) |
| Carbon dioxide insufflator |
| Argon plasma coagulation |
| Endoscopic scissors |
| Hemostatic clips for control of intraprocedural bleeding |
| Endoscopic retrieval net (for removal of foreign bodies or large clots) |
| Through-the-scope esophageal balloons (for transoral outlet reduction and subsequent dilations of stenotic outlets if needed) |
| Grasping forceps (for foreign body removal or suturing assistance) |
| Optional but recommended |
| Endoscopic overtube |
| Hemostatic powder or similar agent (e.g., Hemospray®, PuraStat®) |
| Infiltration pump for intragastric balloon insertion |
| Sequential compression devices for venous thromboembolism prevention |
While no current Food and Drug Administration-authorized procedure requires fluoroscopy, the evolution of EBT to target the metabolically-enriched region of the small intestine suggests that the bariatric endoscopist should reasonably consider fluoroscopic capabilities as an advantage in the coming years[26,52].
In the abovementioned survey study of patients seeking EBTs at our center, the properties of an endobariatric practice that respondents deemed “very important” included physician experience (81.2% of respondents), ease of communication with the facility (74.3%), trust in medical staff (73.3%), quality of nutritional support (67.3%), the online reputation of the facility (67.3%), quality of psychological support (58.4%), self-pay price (52.4%), and wait time to procedure (45.5%)[11]. Emerging EBT programs can use these priorities as a rubric for successful patient recruitment and retention.
The patient intake model will be distinct from traditional gastroenterology and surgical centers, primarily due to the self-pay nature of EBT and the current lack of medical provider familiarity with the field[52]. The largely self-referral, self-pay model demands a more tailored level of service from team members who are personable, available, and skilled, as patients often require multiple touchpoints and significant time investment from their initial point of contact to their procedure day, regardless of practice setting. To facilitate the consultation process, this may require additional and intensive medical training of employees without medical background such that patients can be: (1) Appropriately screened for the correct procedure(s); (2) appropriately screened out for absolute contraindications; and (3) provided a basic overview of EBT procedures, as many patients may lack familiarity with the specialty. Beyond managing intake, scheduling, and financing, these team members also facilitate pre-procedural steps, including bloodwork, organization of peri-procedural medications, and subspecialty evaluations/clearances when needed for comorbid disease.
The initial patient consultation can be conducted with the bariatric endoscopist or an advanced practice provider. It should focus on the patient’s medical, surgical, and social history, with emphasis on their history of obesity and prior weight loss endeavors, as well as concomitant issues that can impact and potentially contraindicate EBT, which are similar to those of metabolic and bariatric surgery, such as disordered eating, substance use disorders, untreated mood/psychiatric disorders, and significant end-organ dysfunction[53]. The technical aspects, benefits, risks, recovery, and logistical components of the EBT of interest should be discussed, as well as alternative options (other EBTs, anti-obesity medications, and metabolic and bariatric surgery, when appropriate). The need for behavioral change and longitudinal follow-up should be emphasized, as well as realistic expectations for the degree and trajectory of weight loss. Our published experience showed that patients tend to overestimate weight loss and underestimate risk prior to consultation with an EBT provider[42].
The procedure-day clinical care team should involve a bariatric endoscopist, registered nurses (pre-procedure intake nurse, circulating nurse, recovery nurse), an anesthesia provider, and an endoscopy technician. Additional staff may be needed to coordinate patient arrivals/departures and to clean endoscopes. After the procedure, medical follow-up can be balanced between the bariatric endoscopist and advanced practice providers to monitor patients’ recovery during the early post-procedural course and for non-response, weight loss plateaus, or weight recurrence over the long term.
As emphasized above, we believe registered dieticians are mandatory members of an EBT practice[54]. Obesity is a chronic, progressive, multifactorial, relapsing condition, and any intervention aimed at weight loss should be offered and supported in conjunction with longitudinal aftercare focused on behavior change[1]. While many gastroenterologists have experience with nutrition, dieticians bring an additional, practical skillset that goes beyond understanding physiology to help patients enact meaningful lifestyle changes. In a study of 284 patients undergoing TORe at our practice, the strongest predictor of weight loss at one year, out of a variety of procedural, patient, and practice components, was the number of follow-up visits the patient attended[17]. Registered dieticians can be integrated into a practice through virtual outsourcing, local outsourcing (e.g., hospital nutrition department), or internal hiring. While these appear in order of increasing difficulty to arrange, their long-term cost decreases, volume permitting. We recommend that all patients considering undergoing an EBT meet with a dietician individually to review expectations of modified diets that follow the procedure to facilitate tissue healing, as well as to provide additional methods of screening for relevant elements of a patient’s history that may impact their recovery and weight loss, such as concomitant disordered eating or alcohol use disorder.
The self-pay nature of EBT and the existing lack of familiarity with EBT within the medical field[52] make marketing a critical and challenging aspect of an EBT program. Referrals from other medical professionals tend to be lower yield than in traditional gastroenterology practice, though this may change as provider familiarity increases and insurance coverage for EBT becomes possible. For now, the direct-to-patient approach has proven most fruitful. This should include a dedicated website or program-specific landing page that describes the available procedures and aftercare and heavy investment in social media, Google advertisements, and targeted digital marketing. Traditional marketing with print, signage, or radio may be helpful, but depends on the local market. Marketing may require a significant time and effort commitment from the bariatric endoscopist but is pivotal to building trust and rapport with patients exploring a relatively novel field.
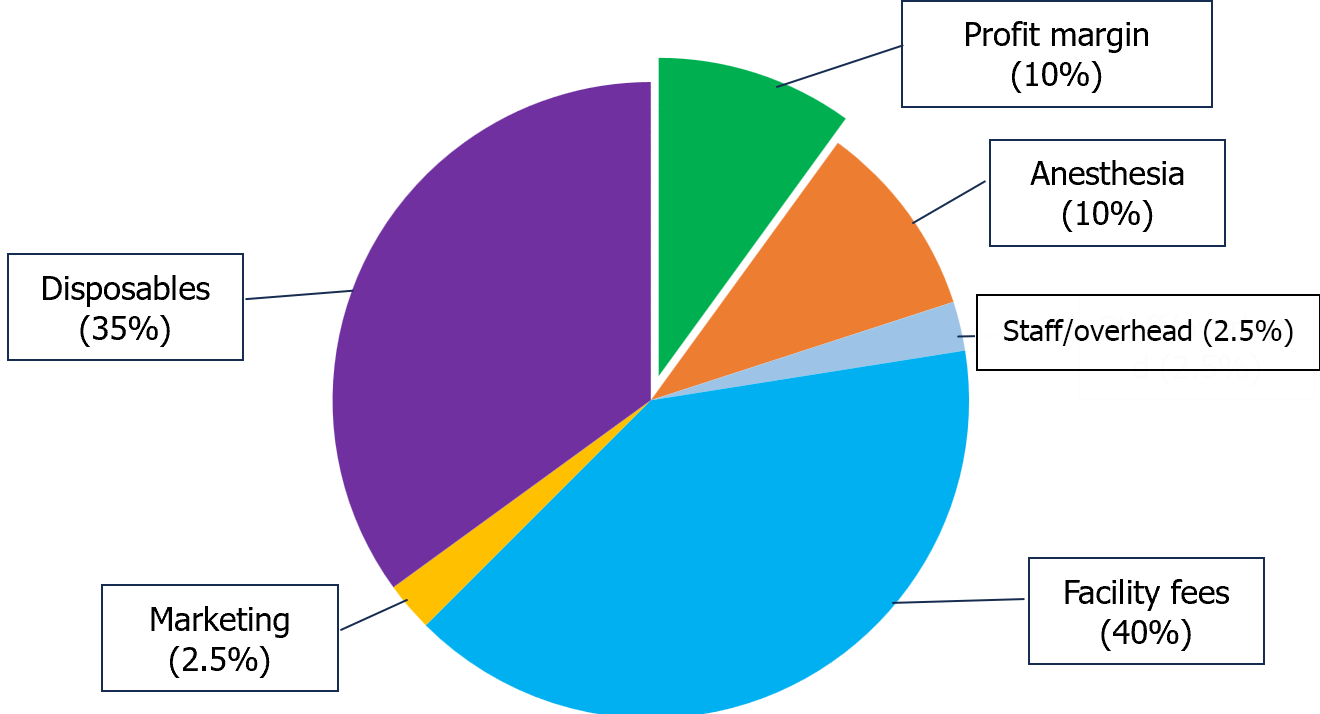
The combination of disposable equipment, marketing, and infrastructure contributes to an EBT program's financial considerations. A significant aspect of cost per procedure is the facility fee and anesthesia costs (general anesthesia capabilities are required for EBT). These must be rigorously negotiated to keep costs low. The sum of these elements for a particular patient—their procedure and aftercare—make the margins in EBT far narrower than one might expect for a self-pay procedure (Figure 1).
EBT is an exciting and evolving opportunity for gastroenterologists to care for patients impacted by obesity through both endoscopic and cognitive skills. For the metabolic and bariatric endoscopist, it requires an effortful dedication to specific procedural skills (e.g., full-thickness suturing technique, recognition of anatomy, management of intra-procedural adverse events) to maximize safety and efficacy, as well as a commitment to the cerebral aspects of obesity physiology (e.g., through ABOM certification and continuing obesity education) to ensure patients are receiving comprehensive, longitudinal care. The success of the patient and practice requires the involvement of multiple team members, especially registered dieticians, as well as an engaging, adaptable patient intake team. As the field continues to evolve in reimbursement and toward applications beyond obesity to related comorbidities and novel technologies (e.g., small bowel therapies), the bariatric endoscopist and EBT practice should be prepared to adapt to a rapidly changing landscape.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy, No. 141707.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arumugam VA, India S-Editor: Zhang H L-Editor: A P-Editor: Cai YX
| 1. | Bray GA, Kim KK, Wilding JPH; World Obesity Federation. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18:715-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 884] [Article Influence: 110.5] [Reference Citation Analysis (1)] |
| 2. | Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2406] [Cited by in RCA: 2534] [Article Influence: 158.4] [Reference Citation Analysis (0)] |
| 3. | Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, Long MW, Gortmaker SL. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. N Engl J Med. 2019;381:2440-2450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 756] [Cited by in RCA: 1294] [Article Influence: 215.7] [Reference Citation Analysis (0)] |
| 4. | Imbus JR, Voils CI, Funk LM. Bariatric surgery barriers: a review using Andersen's Model of Health Services Use. Surg Obes Relat Dis. 2018;14:404-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 5. | Gasoyan H, Tajeu G, Halpern MT, Sarwer DB. Reasons for underutilization of bariatric surgery: The role of insurance benefit design. Surg Obes Relat Dis. 2019;15:146-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 109] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 6. | Wharton S, Serodio KJ, Kuk JL, Sivapalan N, Craik A, Aarts MA. Interest, views and perceived barriers to bariatric surgery in patients with morbid obesity. Clin Obes. 2016;6:154-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Wilding JPH, Batterham RL, Davies M, Van Gaal LF, Kandler K, Konakli K, Lingvay I, McGowan BM, Oral TK, Rosenstock J, Wadden TA, Wharton S, Yokote K, Kushner RF; STEP 1 Study Group. Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022;24:1553-1564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 457] [Article Influence: 152.3] [Reference Citation Analysis (0)] |
| 8. | Aronne LJ, Sattar N, Horn DB, Bays HE, Wharton S, Lin WY, Ahmad NN, Zhang S, Liao R, Bunck MC, Jouravskaya I, Murphy MA; SURMOUNT-4 Investigators. Continued Treatment With Tirzepatide for Maintenance of Weight Reduction in Adults With Obesity: The SURMOUNT-4 Randomized Clinical Trial. JAMA. 2024;331:38-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 290] [Article Influence: 290.0] [Reference Citation Analysis (0)] |
| 9. | Rubino D, Abrahamsson N, Davies M, Hesse D, Greenway FL, Jensen C, Lingvay I, Mosenzon O, Rosenstock J, Rubio MA, Rudofsky G, Tadayon S, Wadden TA, Dicker D; STEP 4 Investigators. Effect of Continued Weekly Subcutaneous Semaglutide vs Placebo on Weight Loss Maintenance in Adults With Overweight or Obesity: The STEP 4 Randomized Clinical Trial. JAMA. 2021;325:1414-1425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 675] [Article Influence: 168.8] [Reference Citation Analysis (0)] |
| 10. | Palanca A, Ampudia-Blasco FJ, Calderón JM, Sauri I, Martinez-Hervás S, Trillo JL, Redón J, Real JT. Real-World Evaluation of GLP-1 Receptor Agonist Therapy Persistence, Adherence and Therapeutic Inertia Among Obese Adults with Type 2 Diabetes. Diabetes Ther. 2023;14:723-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 11. | Maselli DB, Kucera A, Chapman CG, Coan B, Waseem A, Wooley C, McGowan CE. The Endoscopic Bariatric Patient: Characteristics, Beliefs, and Fears. iGIE. 2023 DOI: 10.1016/j.igie.2023.12.004. |
| 12. | ASGE/ASMBS Task Force on Endoscopic Bariatric Therapy. A pathway to endoscopic bariatric therapies. Surg Obes Relat Dis. 2011;7:672-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Abu Dayyeh BK, Maselli DB, Rapaka B, Lavin T, Noar M, Hussan H, Chapman CG, Popov V, Jirapinyo P, Acosta A, Vargas EJ, Storm AC, Bazerbachi F, Ryou M, French M, Noria S, Molina D, Thompson CC. Adjustable intragastric balloon for treatment of obesity: a multicentre, open-label, randomised clinical trial. Lancet. 2021;398:1965-1973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 70] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 14. | Bazerbachi F, Vargas EJ, Abu Dayyeh BK. Endoscopic Bariatric Therapy: A Guide to the Intragastric Balloon. Am J Gastroenterol. 2019;114:1421-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Maselli DB, Hoff AC, Kucera A, Weaver E, Sebring L, Gooch L, Walton K, Lee D, Cratty T, Beal S, Nanduri S, Rease K, Gainey CS, Eaton L, Coan B, McGowan CE. Endoscopic sleeve gastroplasty in class III obesity: Efficacy, safety, and durability outcomes in 404 consecutive patients. World J Gastrointest Endosc. 2023;15:469-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (3)] |
| 16. | Abu Dayyeh BK, Bazerbachi F, Vargas EJ, Sharaiha RZ, Thompson CC, Thaemert BC, Teixeira AF, Chapman CG, Kumbhari V, Ujiki MB, Ahrens J, Day C; MERIT Study Group, Galvao Neto M, Zundel N, Wilson EB. Endoscopic sleeve gastroplasty for treatment of class 1 and 2 obesity (MERIT): a prospective, multicentre, randomised trial. Lancet. 2022;400:441-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 169] [Article Influence: 56.3] [Reference Citation Analysis (0)] |
| 17. | Maselli DB, Chittajallu V, Wooley C, Waseem A, Lee D, Secic M, Donnangelo LL, Coan B, McGowan CE. Transoral outlet reduction: Outcomes of endoscopic Roux-en-Y gastric bypass revision in 284 patients at a community practice. World J Gastrointest Endosc. 2023;15:602-613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 18. | Jirapinyo P, Kumar N, AlSamman MA, Thompson CC. Five-year outcomes of transoral outlet reduction for the treatment of weight regain after Roux-en-Y gastric bypass. Gastrointest Endosc. 2020;91:1067-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 19. | Maselli DB, Alqahtani AR, Abu Dayyeh BK, Elahmedi M, Storm AC, Matar R, Nieto J, Teixeira A, Al Khatry M, Neto MG, Kumbhari V, Vargas EJ, Jaruvongvanich V, Mundi MS, Deshmukh A, Itani MI, Farha J, Chapman CG, Sharaiha R. Revisional endoscopic sleeve gastroplasty of laparoscopic sleeve gastrectomy: an international, multicenter study. Gastrointest Endosc. 2021;93:122-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 20. | Shenoy A, Schulman AR. Advances in endobariatrics: past, present, and future. Gastroenterol Rep (Oxf). 2023;11:goad043. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | McCarty TR, Thompson CC. The current state of bariatric endoscopy. Dig Endosc. 2021;33:321-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | Abu Dayyeh BK, Acosta A, Camilleri M, Mundi MS, Rajan E, Topazian MD, Gostout CJ. Endoscopic Sleeve Gastroplasty Alters Gastric Physiology and Induces Loss of Body Weight in Obese Individuals. Clin Gastroenterol Hepatol. 2017;15:37-43.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 197] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 23. | Rapaka B, Maselli DB, Lopez-Nava G, Bautista-Castaño I, Matar R, Jaruvongvanich V, Vargas EJ, Storm AC, Acosta A, Abu Dayyeh BK. Effects on physiologic measures of appetite from intragastric balloon and endoscopic sleeve gastroplasty: results of a prospective study. Chin Med J (Engl). 2022;135:1234-1241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 24. | Vargas EJ, Rizk M, Gomez-Villa J, Edwards PK, Jaruvongvanich V, Storm AC, Acosta A, Lake D, Fidler J, Bharucha AE, Camilleri M, Abu Dayyeh BK. Effect of endoscopic sleeve gastroplasty on gastric emptying, motility and hormones: a comparative prospective study. Gut. 2023;72:1073-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 25. | Cifuentes L, Camilleri M, Acosta A. Gastric Sensory and Motor Functions and Energy Intake in Health and Obesity-Therapeutic Implications. Nutrients. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 26. | Simons M, Sharaiha RZ. Updates in metabolic bariatric endoscopy. Dig Endosc. 2024;36:107-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 27. | McCarty TR, Thompson CC. Bariatric and Metabolic Therapies Targeting the Small Intestine. Tech Innov Gastrointest Endosc. 2020;22:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 28. | Emerenziani S, Guarino MPL, Trillo Asensio LM, Altomare A, Ribolsi M, Balestrieri P, Cicala M. Role of Overweight and Obesity in Gastrointestinal Disease. Nutrients. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 29. | Nam SY. Obesity-Related Digestive Diseases and Their Pathophysiology. Gut Liver. 2017;11:323-334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 30. | Saumoy M, Schneider Y, Zhou XK, Shukla A, Kahaleh M, Aronne L, Sharaiha RZ. A single-operator learning curve analysis for the endoscopic sleeve gastroplasty. Gastrointest Endosc. 2018;87:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 31. | Jirapinyo P, Thompson CC. Training in Bariatric and Metabolic Endoscopic Therapies. Clin Endosc. 2018;51:430-438. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 32. | Jirapinyo P, Thompson CC. Development of a novel endoscopic suturing simulator: validation and impact on clinical learning curve (with video). Gastrointest Endosc. 2024;99:41-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 33. | Talumaa B, Brown A, Batterham RL, Kalea AZ. Effective strategies in ending weight stigma in healthcare. Obes Rev. 2022;23:e13494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 113] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 34. | Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16:319-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 732] [Cited by in RCA: 774] [Article Influence: 77.4] [Reference Citation Analysis (0)] |
| 35. | Gala K, Brunaldi V, McGowan C, Sharaiha RZ, Maselli D, Vanderwel B, Kedia P, Ujiki M, Wilson E, Vargas EJ, Storm AC, Abu Dayyeh BK. Performance of Endoscopic Sleeve Gastroplasty by Obesity Class in the United States Clinical Setting. Clin Transl Gastroenterol. 2024;15:e00647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 36. | Ryan DH, Yockey SR. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017;6:187-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 386] [Cited by in RCA: 477] [Article Influence: 59.6] [Reference Citation Analysis (0)] |
| 37. | Mariam A, Miller-Atkins G, Pantalone KM, Iyer N, Misra-Hebert AD, Milinovich A, Bauman J, Mocarski M, Ramasamy A, Smolarz BG, Hobbs TM, Zimmerman RS, Burguera B, Kattan MW, Rotroff DM. Associations of weight loss with obesity-related comorbidities in a large integrated health system. Diabetes Obes Metab. 2021;23:2804-2813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 38. | Hedjoudje A, Abu Dayyeh BK, Cheskin LJ, Adam A, Neto MG, Badurdeen D, Morales JG, Sartoretto A, Nava GL, Vargas E, Sui Z, Fayad L, Farha J, Khashab MA, Kalloo AN, Alqahtani AR, Thompson CC, Kumbhari V. Efficacy and Safety of Endoscopic Sleeve Gastroplasty: A Systematic Review and Meta-Analysis. Clin Gastroenterol Hepatol. 2020;18:1043-1053.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 158] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 39. | Hajifathalian K, Simmons O, Abu-Hammour M, Hassan K, Sharaiha RZ. Efficacy of endoscopic resuturing versus pharmacotherapy to treat weight recidivism after endoscopic sleeve gastroplasty. Gastrointest Endosc. 2023;98:944-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 40. | Lopez-Nava G, Asokkumar R, Negi A, Normand E, Bautista I. Re-suturing after primary endoscopic sleeve gastroplasty (ESG) for obesity. Surg Endosc. 2021;35:2523-2530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 41. | Maselli DB, Waseem A, Lee D, Wooley C, Donnangelo LL, Coan B, McGowan CE. Performance Characteristics of Endoscopic Sleeve Gastroplasty in Patients with Prior Intragastric Balloon: Results of a Propensity Score Matched Study. Obes Surg. 2023;33:2711-2717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 42. | Jaruvongvanich V, Vantanasiri K, Laoveeravat P, Matar RH, Vargas EJ, Maselli DB, Alkhatry M, Fayad L, Kumbhari V, Fittipaldi-Fernandez RJ, Hollenbach M, Watson RR, Gustavo de Quadros L, Galvao Neto M, Aepli P, Staudenmann D, Brunaldi VO, Storm AC, Martin JA, Gomez V, Abu Dayyeh BK. Endoscopic full-thickness suturing plus argon plasma mucosal coagulation versus argon plasma mucosal coagulation alone for weight regain after gastric bypass: a systematic review and meta-analysis. Gastrointest Endosc. 2020;92:1164-1175.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 43. | Alqahtani AR, Elahmedi M, Alqahtani YA, Al-Darwish A. Laparoscopic Sleeve Gastrectomy After Endoscopic Sleeve Gastroplasty: Technical Aspects and Short-Term Outcomes. Obes Surg. 2019;29:3547-3552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 44. | Alqahtani A, Al-Darwish A, Mahmoud AE, Alqahtani YA, Elahmedi M. Short-term outcomes of endoscopic sleeve gastroplasty in 1000 consecutive patients. Gastrointest Endosc. 2019;89:1132-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 138] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 45. | Lopez-Nava G, Asokkumar R, Rull A, Corbelle F, Beltran L, Bautista I. Bariatric endoscopy procedure type or follow-up: What predicted success at 1 year in 962 obese patients? Endosc Int Open. 2019;7:E1691-E1698. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 46. | Singh S, de Moura DTH, Khan A, Bilal M, Chowdhry M, Ryan MB, Bazarbashi AN, Thompson CC. Intragastric Balloon Versus Endoscopic Sleeve Gastroplasty for the Treatment of Obesity: a Systematic Review and Meta-analysis. Obes Surg. 2020;30:3010-3029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 47. | Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, Kushner RF, Lindquist R, Pessah-Pollack R, Seger J, Urman RD, Adams S, Cleek JB, Correa R, Figaro MK, Flanders K, Grams J, Hurley DL, Kothari S, Seger MV, Still CD. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis. 2020;16:175-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 312] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 48. | Li P, Ma B, Gong S, Zhang X, Li W. Efficacy and safety of endoscopic sleeve gastroplasty for obesity patients: a meta-analysis. Surg Endosc. 2020;34:1253-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 49. | Singh S, Hourneaux de Moura DT, Khan A, Bilal M, Ryan MB, Thompson CC. Safety and efficacy of endoscopic sleeve gastroplasty worldwide for treatment of obesity: a systematic review and meta-analysis. Surg Obes Relat Dis. 2020;16:340-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 50. | Gudur AR, Geng CX, Podboy A. Early safety and efficacy comparison of endoscopic bariatric interventions. Surg Obes Relat Dis. 2023;19:1148-1153. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 51. | Swei E, Almuhaidb A, Sullivan S, Al-Shahrani A, D'Souza FR, Altayar O, Bell S, Maday R, Wagh MS, Mullady D, Bennett M, Early D, Kushnir V. Comparison of the Efficacy and Safety of the FDA-approved Intragastric Balloon Systems in a Clinical Setting. J Clin Gastroenterol. 2023;57:578-585. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 52. | Badurdeen D, Farha J, Fayad L, Abbarh S, Singh G, Jovani M, Hedjoudje A, Adam A, Alqahtani A, Neto MG, Kumbhari V. The Attitude of Practitioners Towards Endoscopic Sleeve Gastroplasty. J Clin Gastroenterol. 2022;56:756-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 53. | Benalcazar DA, Cascella M. Obesity Surgery Preoperative Assessment and Preparation. 2022 Jul 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 54. | Negi A, Asokkumar R, Ravi R, Lopez-Nava G, Bautista-Castaño I. Nutritional Management and Role of Multidisciplinary Follow-Up after Endoscopic Bariatric Treatment for Obesity. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |