Published online Nov 16, 2024. doi: 10.4253/wjge.v16.i11.617
Revised: August 29, 2024
Accepted: October 16, 2024
Published online: November 16, 2024
Processing time: 149 Days and 19 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) is a key procedure for diagnosing and treating biliary and pancreatic disorders. Although effective, it carries risks, including rare but severe complications such as air embolism.
We report a case of a 58-year-old man who developed extensive air embolism during ERCP. He previously underwent a Whipple procedure and experienced a sudden drop in vital signs and loss of consciousness. Immediate intervention with hyperbaric oxygen therapy and supportive care led to gradual recovery. Imaging confirmed widespread air embolism, which resolved with continued treatment.
Air embolism is a rare, critical complication of ERCP, especially in patients with prior surgery such as pancreaticoduodenectomy. Early detection and prompt treatment, including hyperbaric oxygen therapy, are crucial for favorable out
Core Tip: This case report presents a rare but severe complication of endoscopic retrograde cholangiopancreatography, where a patient with a history of pancreaticoduodenectomy developed extensive systemic air embolism. Rapid diagnosis and timely administration of hyperbaric oxygen therapy were critical in achieving a positive clinical outcome. This report underscores the importance of early recognition and intervention to prevent life-threatening consequences in similar cases.
- Citation: Li JH, Luo ZK, Zhang Y, Lu TT, Deng Y, Shu RT, Yu H. Systemic air embolism associated with endoscopic retrograde cholangiopancreatography: A case report. World J Gastrointest Endosc 2024; 16(11): 617-622
- URL: https://www.wjgnet.com/1948-5190/full/v16/i11/617.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i11.617
Endoscopic retrograde cholangiopancreatography (ERCP) is a widely utilized procedure for the diagnosis and treatment of biliary and pancreatic disorders[1]. While it is an effective procedure, complications such as pancreatitis, cholangitis, bleeding, and perforation are well documented. A less common but severe complication is air embolism, which can lead to life-threatening conditions if not promptly recognized and treated[2]. This case report describes a patient who developed extensive air embolism during ERCP, emphasizing the importance of early detection and appropriate mana
A 58-year-old man presented with obstructive jaundice, occurring 6 months after undergoing a Whipple procedure (pancreaticoduodenectomy) for pancreatic cancer.
The patient reported progressive jaundice over the past few weeks, accompanied by generalized weakness and mild upper abdominal discomfort. These symptoms led to admission for further evaluation and management. The patient had been experiencing intermittent episodes of jaundice since his Whipple procedure, which were previously managed conservatively.
Six months ago, the patient underwent a Whipple procedure (pancreaticoduodenectomy) for pancreatic cancer, which involved removal of the head of the pancreas, part of the duodenum, gallbladder, and a portion of the bile duct to treat the cancer. The surgery was successful without immediate complications, but his postoperative course was complicated by intermittent jaundice and episodes of biliary obstruction, which were managed conservatively with supportive care, including fluid management and monitoring of liver function tests. Preoperatively, the patient presented with symptoms such as jaundice, weight loss, and abdominal pain, and imaging confirmed a mass at the head of the pancreas. Despite his diagnosis, his baseline health was good, with no history of chronic liver disease, cardiovascular conditions, diabetes, or significant comorbidities. Despite his balanced diet, the patient reported decreased appetite and significant weight loss in the months leading up to his cancer diagnosis.
The patient denied any history of similar conditions in his family, and no known genetic predispositions were reported.
The patient presented with jaundice but remained hemodynamically stable, exhibiting a blood pressure of 135/85 mmHg, a heart rate of 78 beats per minute, a respiratory rate of 18 breaths per minute, and an oxygen saturation of 98% on room air. The abdominal examination demonstrated mild tenderness in the right upper quadrant, with no palpable masses or signs of ascites detected. There were no signs of acute distress, hepatosplenomegaly, or peripheral edema. Neurological and cardiovascular examinations were unremarkable.
Initial laboratory investigations showed elevated levels of total bilirubin (5.2 mg/dL) and direct bilirubin (4.0 mg/dL), along with raised alkaline phosphatase (230 U/L). Mild elevations were noted in alanine aminotransferase (78 U/L) and aspartate aminotransferase (65 U/L). Serum amylase, lipase levels, complete blood count, coagulation profile, and renal function were normal.
A contrast-enhanced CT scan of the abdomen revealed dilated intrahepatic bile ducts, indicating biliary obstruction. There was no evidence of an obvious mass, stone, or new metastatic lesions. The pancreaticojejunal and hepaticojejunal anastomoses were patent, and mild dilation of the pancreatic duct was noted.
During ERCP, the patient was diagnosed with an extensive systemic air embolism.
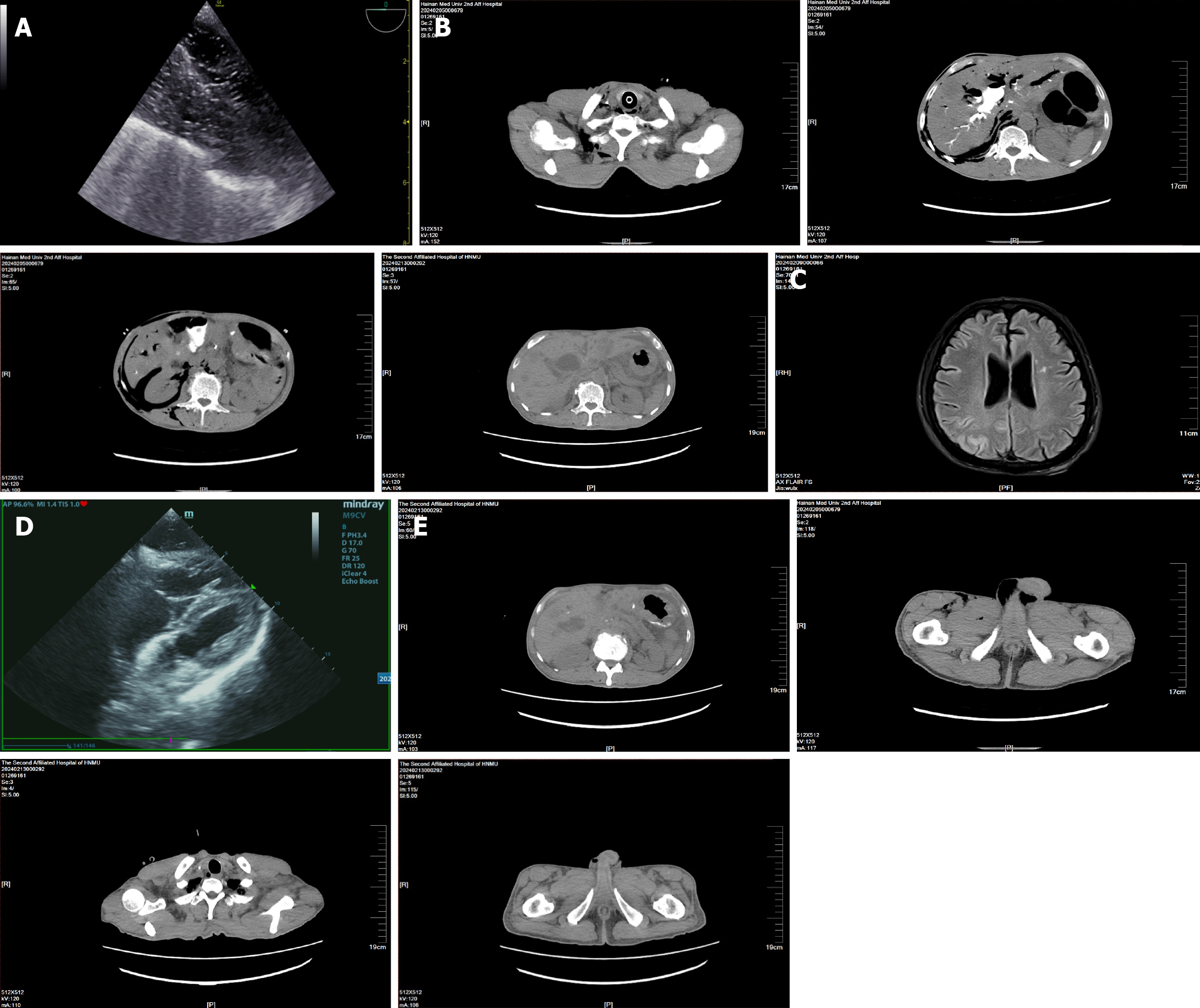
During ERCP, the patient suddenly became unconscious, with a precipitous drop in blood pressure to 60/40 mmHg and a heart rate decrease to 42 beats/min. Additionally, oxygen saturation dropped significantly to 54%. Immediate resuscitation measures were initiated, including intubation and manual bag ventilation. Intravenous medications were administered via cannulation of the right internal jugular vein (refer to Table 1). These interventions stabilized the patient’s condition, with blood pressure rising to 100/40 mmHg, heart rate to 90 beats/min, and oxygen saturation to 92%. A contrast-enhanced CT angiography (Figure 1B) further demonstrated multiple air collections in the right thoracic, abdominal wall, mediastinum, right pleural cavity, liver, alongside the inferior vena cava, retroperitoneal abdominal cavity, around the right kidney, right inguinal and scrotal areas, and proximal right thigh.
| Time | Drug | Dosages |
| Immediate | Adrenaline | 1 mg |
| Immediate | Dopamine | 3 mg |
| Immediate | Norepinephrine | 18 µg |
| 5 hours later | Norepinephrine | 18 µg |
| 5.5 hours later | Meropenem | 1 g q8h |
| 5.5 hours later | Metronidazole | 0.4 g q8h |
| 5.5 hours later | Glutathione | 1.2 g qd |
| 5.5 hours later | Ademetionine | 1 g qd |
Transthoracic echocardiography revealed the presence of air within the heart chambers (Figure 1A). The original video at the time of examination is provided as Video 1, Video 2, and Video 3. Prompt treatment with hyperbaric oxygen therapy was initiated, starting with 2.8 atmospheres absolute (ATA) (atmospheres absolute) for 2.5 hours, followed by continued therapy at 2.2 ATA for 3 hours. The goal was to promote reabsorption of the air embolism, reduce the volume of air, minimize cerebral edema, and enhance tissue oxygenation. Broad-spectrum antibiotics (meropenem 1 g q8h, metronidazole 0.4 g q8h) were administered to prevent infection, and hepatoprotective agents (glutathione 1.2 g qd, ademetionine 1 g qd) were provided to support liver function.
Following initial treatment, the patient’s condition gradually stabilized. He regained consciousness and began respon
Two days after ERCP, repeat contrast-enhanced computed tomography angiography indicated further reduction in air embolism, with no new complications noted. After ruling out contraindications, percutaneous transhepatic cholangiography drainage was performed to address biliary obstruction, and the patient continued to recover without complications.
The patient was discharged in stable condition, with follow-up imaging showing continued improvement. At the 2-month follow-up, he reported no specific complaints, and repeat imaging confirmed the absence of residual air embolism or biliary obstruction (Figure 1E).
The occurrence of air embolism in this patient was likely multifactorial, with significant contributions from surgical history and the procedural aspects of ERCP. The patient had previously undergone a Whipple procedure (pancreaticoduodenectomy), which typically involves extensive manipulation of the retroperitoneal space. This surgical intervention can lead to adhesions between the intestines and surrounding tissues, placing them in close proximity to major vascular structures such as the inferior vena cava. These adhesions may have created a conduit for air to enter the venous system during the ERCP procedure[3].
Additionally, the patient's history of pancreatic malignancy with multiple liver metastases could have exacerbated the risk of air embolism. Tumor invasion or metastatic deposits near the inferior vena cava might compromise the integrity of the vascular wall, although direct invasion of the tumor into the vena cava, as theorized, would likely present with significant bleeding, which was not observed in this case.
During ERCP, the introduction of positive pressure air to improve visibility and cleanse the ducts is a routine practice. However, in patients with altered anatomy due to previous surgery, such as the Whipple procedure, there is an increased risk that air could inadvertently enter the venous system[4]. In this case, it is hypothesized that air entered through incomplete anastomoses between the pancreatic and bile ducts or through abnormal channels created by surgical adhesions. Once in the biliary system, the air could have traveled through the hepatic veins into the inferior vena cava, subsequently reaching the right side of the heart.
Ultrasonography confirmed the presence of air predominantly in the right side of the heart, supporting the theory of venous air embolism originating from the inferior vena cava. The accumulation of air in the retroperitoneal and right abdominal areas further supports this pathway.
In the echocardiogram (Figure 1D), an echogenic area was observed posterior to the heart, which may correspond to the presence of air in the pericardial or surrounding thoracic structures. This finding is consistent with the spread of air embolism through the venous system and its subsequent accumulation in both cardiac and extracardiac compartments. The presence of air in these areas suggests that the embolism was extensive, involving not only the intracardiac chambers but also the pericardium and possibly adjacent mediastinal structures. This observation corroborates the hypothesis that air entered through the inferior vena cava and dispersed throughout the thoracic cavity, including pericardial and mediastinal spaces.
Post-ERCP air embolism is a rare but well-known adverse event, with an incidence rate of 3.32 cases per 100000 procedures[5-7]. Hyperbaric oxygen therapy is an effective treatment for such air embolisms, promoting gas reabsorption to reduce the volume of air embolisms, thereby minimizing bubbles, alleviating cerebral edema, reducing endothelial damage caused by bubble-induced platelet aggregation, accelerating the reabsorption of nitrogen, preventing the release of free radicals, and increasing blood oxygen concentration to enhance tissue oxygenation and mitigate ischemic re
We extend our gratitude to the Intensive Care Unit, Department of Cardiovascular Medicine, at Hainan Medical Uni
| 1. | Chuang J, Kuang R, Ramadugu A, Patel D, Sharma S, Shrestha K, Burlen J, Nawras A. Fatal Venous Gas Embolism During Endoscopic Retrograde Cholangiopancreatography After Simultaneous Deployment of 2 Self-Expandable Metallic Stents. ACG Case Rep J. 2022;9:e00873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 2. | Okano N, Ito K, Takuma K, Hara S, Igarashi Y. Prevention and management of ERCP-related complications. Mini-invasive Surg. 2021;5:29. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Fromer IR, Horvath B, Prielipp RC, Kloesel B. Vascular Air Emboli During the Perioperative Period. Curr Anesthesiol Rep. 2020;10:436-448. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Olaiya B, Adler DG. Air embolism secondary to endoscopy in hospitalized patients: results from the National Inpatient Sample (1998-2013). Ann Gastroenterol. 2019;32:476-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Lanke G, Adler DG. Gas embolism during endoscopic retrograde cholangiopancreatography: diagnosis and management. Ann Gastroenterol. 2019;32:156-167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 6. | Afreen LK, Bryant AS, Nakayama T, Ness TJ, Jones KA, Morgan CJ, Wilcox CM, Phillips MC. Incidence of Venous Air Embolism During Endoscopic Retrograde Cholangiopancreatography. Anesth Analg. 2018;127:420-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Guo JL, Wang HB, Wang H, Le Y, He J, Zheng XQ, Zhang ZH, Duan GR. Transesophageal echocardiography detection of air embolism during endoscopic surgery and validity of hyperbaric oxygen therapy: Case report. Medicine (Baltimore). 2021;100:e26304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Chen Y, Wang L, You W, Huang F, Jiang Y, Sun L, Wang S, Liu S. Hyperbaric oxygen therapy promotes consciousness, cognitive function, and prognosis recovery in patients following traumatic brain injury through various pathways. Front Neurol. 2022;13:929386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |