Published online Oct 16, 2024. doi: 10.4253/wjge.v16.i10.557
Revised: September 10, 2024
Accepted: September 19, 2024
Published online: October 16, 2024
Processing time: 87 Days and 23 Hours
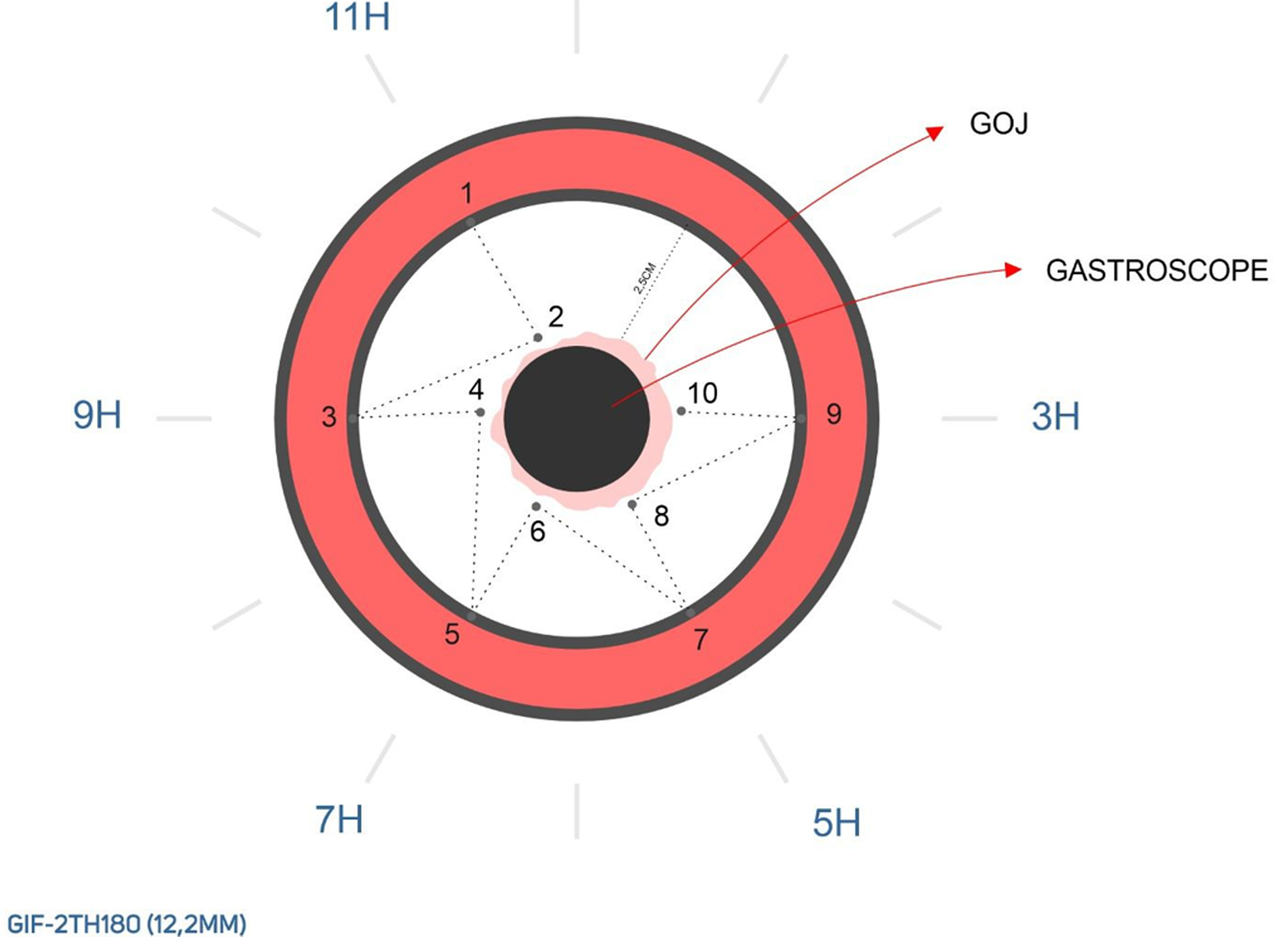
Gastric fundoplication with endoscopic technique (GFET) is an innovative approach to managing gastroesophageal reflux disease (GERD). This minimally invasive procedure utilizes the GEN-2 Apollo endosuture device and Olympus H2T180 gastroscope to perform partial fundoplication by strategically placing Prolene 2-0 sutures at the 11, 7, 5, 1, and 3 o’clock positions around the gastroesophageal junction.
To evaluate whether GFET enhances the lower esophageal sphincter function by creating comprehensive plication to improve the barrier against reflux.
This single-center prospective study included patients undergoing GFET. Before beginning GFET, pH metrics and subsequent manometric measurements were obtained. An analysis of variance was performed to determine statistically significant differences between quality of life (QOL) and DeMeester scores at the time of the procedure and 6 and 12 months postoperatively. Pearson’s χ2 test was performed to identify statistically significant differences between categorical variables at the time of the procedure and 6 and 12 months postoperatively.
Eighteen participants were enrolled (11 males and 7 females; mean age, 35 years). More than 70% had an initial Hill grade of IIb. One adverse event was recorded after the procedure. One patient underwent valve reinforcement at 12 months. The mean QOL score was markedly higher at the time of the procedure (39.9 ± 4.0) compared to those at 6 and 12 months postoperatively (P < 0.001). Scores at 12 months were slightly higher than those at 6 months. The highest mean QOL score was observed at the time of the procedure, followed by those at 6 and 12 months postoperatively (P < 0.001). A similar trend was noted for the mean DeMeester scores (P < 0.001).
GFET is a minimally invasive alternative to traditional surgical interventions and endoscopic techniques for managing GERD. Further research is warranted to validate its long-term efficacy and effectiveness over existing treatments.
Core Tip: Gastric fundoplication with endoscopic technique (GFET) is an innovative and minimally invasive method of treating gastroesophageal reflux disease (GERD). This procedure uses the GEN-2 Apollo endosuture device and Olympus H2T180 gastroscope and involves placing sutures around the gastroesophageal junction to strengthen the lower esophageal sphincter. This technique aims to reduce reflux without surgery. Most patients experienced significant improvements in their quality of life and GERD symptoms over the course of 12 months. GFET is associated with minimal side effects; therefore, it appears to be a promising and safe option for GERD management.
- Citation: Gadour E, Hoff AC. Gastric fundoplication with endoscopic technique: A novel approach for gastroesophageal reflux disease treatment. World J Gastrointest Endosc 2024; 16(10): 557-565
- URL: https://www.wjgnet.com/1948-5190/full/v16/i10/557.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i10.557
Gastroesophageal reflux disease (GERD), commonly referred to as heartburn, occurs when the lower esophageal sphincter (LES) transiently relaxes, thus allowing gastric contents to flow into the esophagus[1]. This condition can progress to pathological GERD and significantly affect the quality of life (QOL) by causing sleep disturbances, recurrent aspirations, persistent chronic coughing, acid reflux, and severe epigastric pain[1,2]. In older children and adults, GERD can lead to complications such as stenosis and Barrett’s esophagus. Although several foods and drinks have been associated with GERD, large amounts of fatty and spicy foods, as well as chocolate, are mainly associated with GERD[3]. The etiology of pathologic GERD has been associated with congenital malformations of the gastroenteric anatomy, such as esophageal atresia, diaphragmatic hernia, hiatal hernia, and upside-down stomach[1]. Several risk factors are associated with GERD, including age[4], smoking[5], obesity[6,7], and drug-related and stress-related factors.
Globally, the incidence of GERD among the general population is more than 20%, and this incidence is increasing[8,9]. Fortunately, several therapeutic interventions for GERD are available, including lifestyle modifications, pharmacological treatments, and surgical and endoscopic techniques. However, the application of these interventions relies on several factors such as disease severity, patient preferences, and the response to the initial interventions. Conservative and non-invasive interventions, such as lifestyle modifications and proton pump inhibitors (PPIs), are usually preferred and are effective in most cases[1,10,11].
Conventionally, surgical interventions such as laparoscopic Nissen fundoplication have been the gold standard intervention for GERD[12]. Despite the effectiveness of this technique, surgery is significantly invasive, and several unwanted consequences that are largely attributable to overcorrection of the reflux mechanism, such as bloating and belching difficulties, can occur; therefore, laparoscopic surgery is unappealing to many patients[12,13]. Consequently, further attention has been focused on the invention and optimization of alternative interventions, resulting in the development of several endoscopic procedures such as transoral incisionless fundoplication (TIF) and the GERDX™ procedure[14]. Additionally, the Stretta procedure, which involves radiofrequency and endoscopic techniques, has been proposed[15].
Endoscopic techniques have several advantages, including minimal invasion, reduced pain, reduced length of stay in the hospital, and less susceptibility to complications such as infections and incisional hernias[16-18]. Therefore, we present evaluated patients who had undergone gastric fundoplication with endoscopic technique (GFET), which is an endoscopic method that involves suture placement at the 1, 3, 5, 7, and 11 o’clock positions of the fundus (Figures 1 and 2) and is similar to the GERDX™ procedure.
The placement of sutures at the 1, 3, 5, 7, and 11 o’clock positions is hypothesized to create comprehensive and circumferential plication, enhance the pressure barrier at the LES, and prevent reflux more effectively than the traditional and existing endoscopic methods. This minimally invasive approach reduces the risk of infection, postoperative pain, and the hospital stay associated with open or laparoscopic surgery. By optimizing suture placement, we aimed to more effectively improve symptom relief and reduce the incidence of heartburn, regurgitation, and other GERD-related symptoms. More robust plication is also expected to minimize complications, such as slippage or loosening sutures, thus providing durable and long-lasting treatment. This endoscopic approach aligns with patient preferences for less invasive treatments, provides quicker recovery, allows fewer lifestyle disruptions, and requires fewer repeat procedures and long-term medications, thereby significantly enhancing the QOL. To evaluate whether GFET enhances the LES function by creating comprehensive plication to improve the barrier against reflux.
This single-center prospective study was conducted in Brazil between July 2023 and July 2024. Ethical approval for the study was received and, the study was registered under Angioskope number AN00172-3.
Thirty patients were recruited for this study. All patients were older than 18 years (mean age, 35.4 ± 5.4 years). Four patients were absent at the start of the study; therefore, they were excluded. Twenty-six patients were enrolled in the study. All patients signed consent forms before the study commenced. Unfortunately, eight patients were lost during follow-up, primarily because they refused to undergo repeated manometric tests. The same endoscopist previously examined all patients.
Before beginning GFET, pH metrics and subsequent manometric measurements were obtained using 36-channel high-resolution impedance spectrometry (ALACER-Multiplex). Before the procedure, endoscopy was performed to rule out unexpected anatomical abnormalities. No hiatal hernias or allergic reactions to medications were observed during the study. Participants included in the trial did not have a history of anti-reflux surgery.
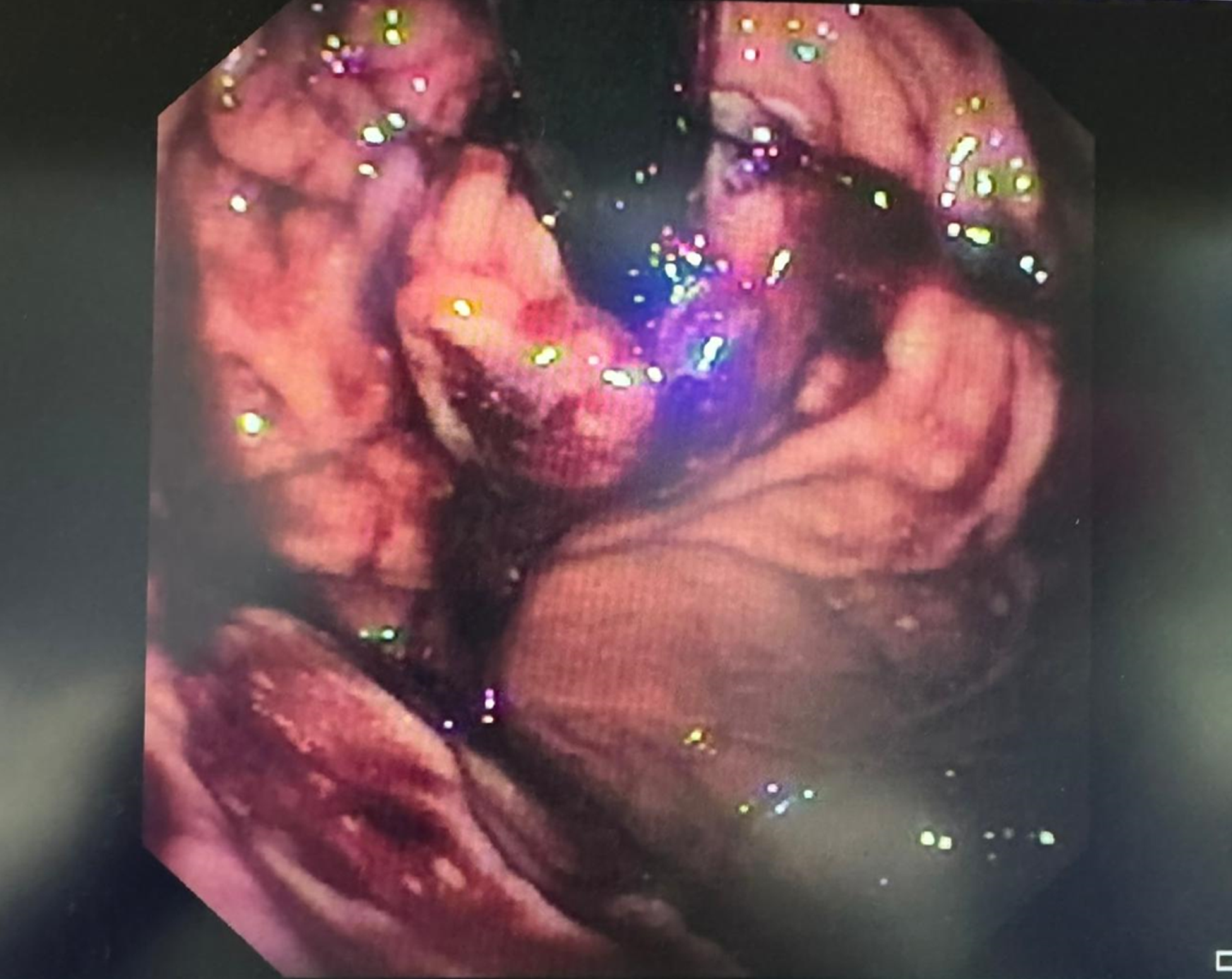
GFET was performed using the GEN-2 Apollo endosuture device and Olympus H2T180 gastroscope. An initial endoscopy was performed to map and identify anatomical structures before beginning the procedure. All patients were placed under general anesthesia, and ample lubrication was applied to the gastroscope and working channel. The gastroscope was advanced through the oropharynx into the esophagus and stomach. A jaw thrust maneuver was used to facilitate the passage of the endosuture device and gastroscope through the esophagus. Upon reaching the stomach, both devices were independently retroflexed under direct vision. The Apollo endosuture device was rotated to the 11 o’clock position and slightly opened, and the helical retractor was advanced into the gastroesophageal junction (GOJ) on the esophageal side. With traction applied on the helical retractor, the Apollo endosuture was closed, and Prolene 2-0 sutures were placed to attach the fundus to the esophagus. Four additional sutures were placed at this location. The helical retractor was then detached, and the endosuture device was rotated to the 7, 1, and 3 o’clock positions, where four sutures were placed at each position, creating 2- to 3-cm partial fundoplication. The devices were then straightened and removed under direct visualization. The TIF procedure inspired the feasibility principle, which aimed to mimic the same valve using a similar device but with the use of Prolene 2-0 full-thickness sutures instead of plastic clips. All cinching was performed in retroflexion using the Olympus H2T180 gastroscope and GEN-2 Apollo endosuture to assess the valve. After GFET, the Apollo GEN-2 device was detached and upper endoscopy with the Olympus H2T180 device was conducted to assess the valve. No difficulties were observed at the GOJ. In accordance with the same protocol used during TIF, a vascular surgeon was always present in the operating room to provide assistance in case adverse events occurred.
During the procedure, second-generation cephalosporin, a β-lactam antimicrobial, was used to counter any possible infections. Subsequently, paracetamol was administered for pain. Patients were administered 1 g of sucralfate and 40 mg of Vonoprazan twice daily during the first 2 weeks after the procedure. During the first week after the procedure, a liquid normocaloric diet enriched with proteins. During the second week after the procedure, a liquid diet was allowed. During the third week after the procedure, a soft diet was introduced. During the fourth week after the procedure, a regular diet was allowed.
Data were recorded using Microsoft Excel (Redmond, WA, United States) and analyzed using SPSS version 27 (IBM Corp., Armonk, NY, United States). Categorical variables are presented as frequencies and percentages, whereas continuous variables (including age and QOL scores) are presented as means with standard deviations. An analysis of variance was performed to identify statistically significant differences between the QOL and DeMeester scores at the time of the procedure and 6 and 12 months postoperatively. Pearson’s χ2 test was performed to identify statistically significant differences between categorical variables (QOL, GERD at the time of endoscopy, and use of anti-GERD medications) recorded at the time of the procedure and 6 and 12 months postoperative. P < 0.05 was considered statistically significant for all analyses.
Eighteen participants were enrolled in the study (11 males and 7 female patients). Their mean age was 35 years, and over 70% of the participants had an initial Hill grade of IIb. Only one adverse event was recorded following the procedure (oozing at the 11 o’clock position). Only one patient underwent valve reinforcement at 12 months (Table 1).
| Characteristic | Value |
| Sex | |
| Male | 11 (61.1) |
| Female | 7 (38.9) |
| Age, years (mean ± SD) | 35.4 ± 5.4 |
| Initial Hill grade | |
| IIa | 4 (22.2) |
| IIb | 14 (77.8) |
| Adverse events | 1 (5.6) |
| Valve reinforcement at 12 months postoperatively | 1 (5.6) |
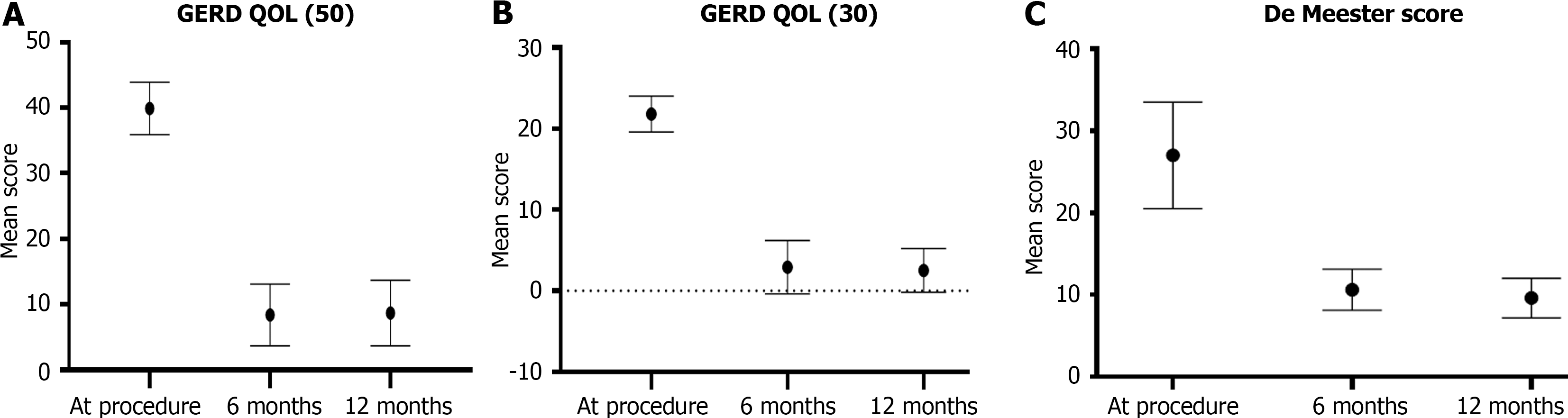
A comparison of GERD-related QOL scores at the time of the procedure and those at 6 and 12 months postoperatively revealed that the mean QOL score at the time of procedure (39.9 ± 4.0) was markedly higher than those at 6 and 12 months postoperatively (P < 0.001) (Table 2). However, the scores at 12 months were slightly higher than those at 6 months postoperatively (Figure 3A). A comparison of the QOL scores revealed that the mean score was highest at the time of the procedure, followed by those at 6 and 12 months postoperatively (P < 0.001) (Figure 3B). A similar trend was noted for the mean DeMeester scores (P < 0.001) (Figure 3C; Table 2).
| Score | At the time of the procedure | 6 months | 12 months | P value |
| GERD-related QOL (50) | 39.9 ± 4.0 | 8.4 ± 4.7 | 8.7 ± 5.0 | < 0.001 |
| GERD-related QOL (30) | 21.8 ± 2.2 | 2.9 ± 3.3 | 2.5 ± 2.7 | < 0.001 |
| DeMeester | 27.0 ± 6.5 | 10.6 ± 2.5 | 9.6 ± 2.4 | < 0.001 |
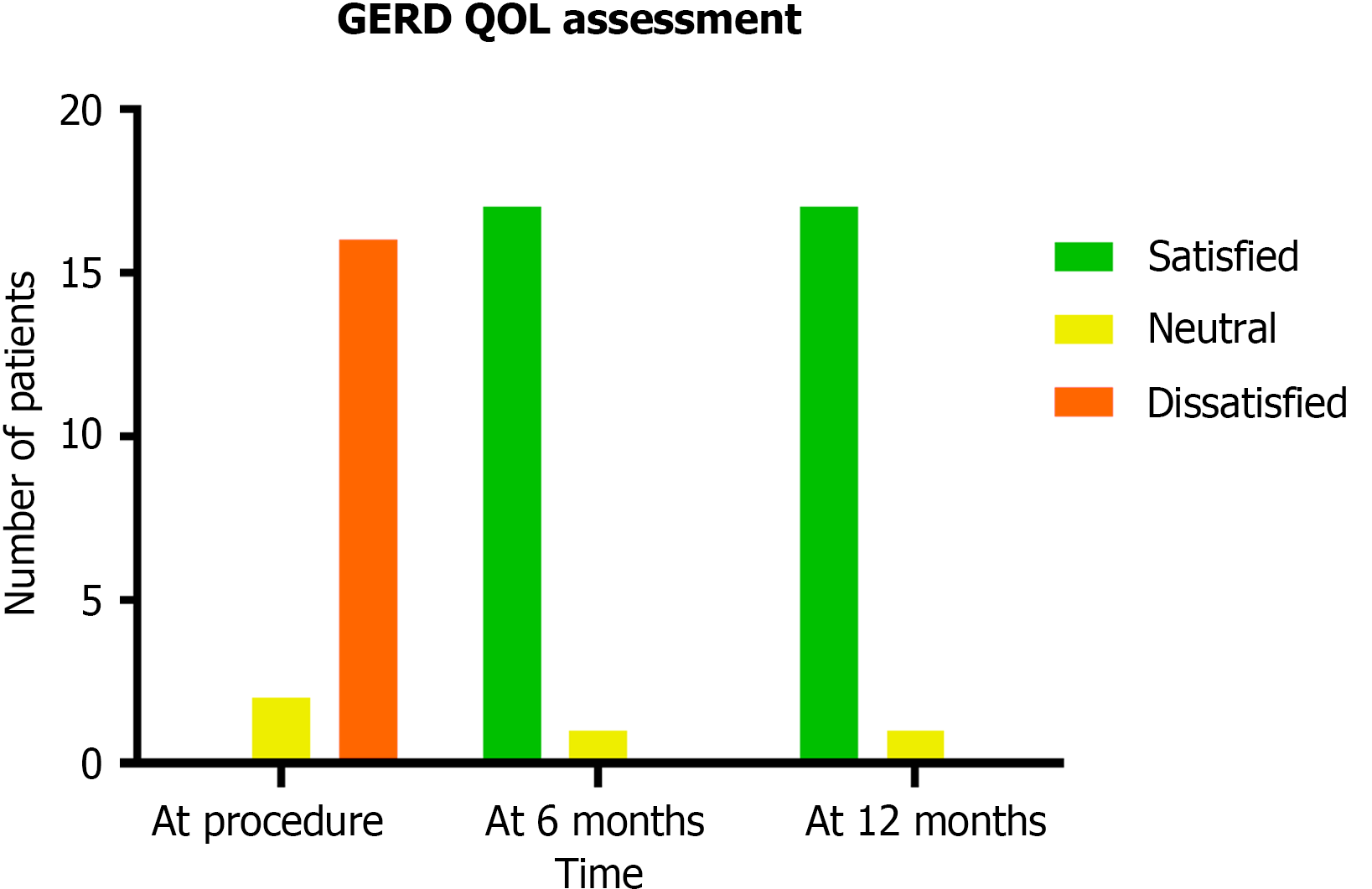
A comparison of GERD-related QOL at the time of the procedure and 6 and 12 months postoperatively revealed that patient satisfaction was increased at 6 and 12 months postoperatively (P < 0.001). All patients were dissatisfied at the time of the procedure; however, no patients were dissatisfied at 6 and 12 months (Figure 4; Table 3).
| Assessment, n | At the time of the procedure | 6 months | 12 months | P value |
| Satisfied | 0 | 17 | 17 | < 0.001 |
| Neutral | 2 | 1 | 1 | |
| Dissatisfied | 16 | 0 | 0 |
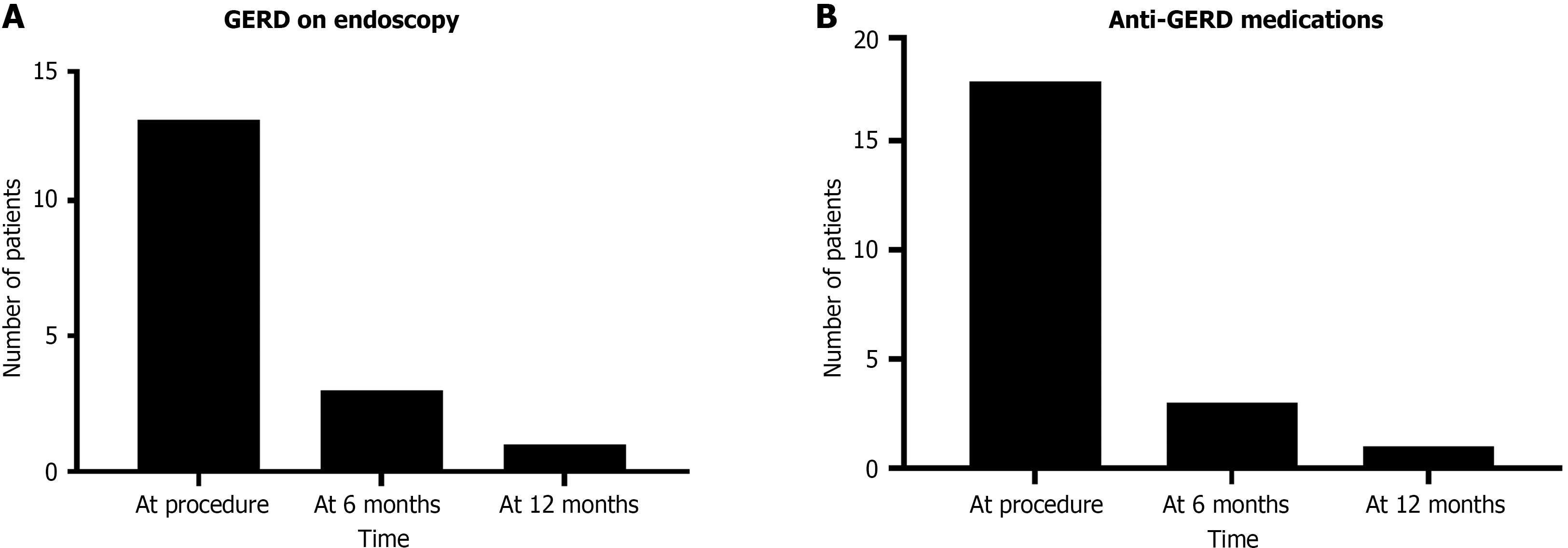
An evaluation of the treatment efficacy of GFET revealed that GERD was detected in 13 patients at the time of the procedure, in 3 patients at 6 months postoperatively, and in 1 patient at 12 months postoperatively. This decline in GERD detection was statistically significant (P < 0.001) (Figure 5A). At the time of the procedure, all patients were using anti-GERD medications; however, only three and one patients were using anti-GERD medications at 6 months and 12 months postoperatively, respectively (Figure 5B). This decline in anti-GERD medication use was also statistically significant (P < 0.001) (Table 4).
| Characteristic, n | At the time of the procedure | 6 months | 12 months | P value |
| GERD during endoscopy | 13 | 3 | 1 | < 0.001 |
| Anti-GERD medications | 18 | 3 | 1 | < 0.001 |
In this study, we assessed the efficacy of GFET. Our findings demonstrated significant improvements in patient outcomes, comparable to those achieved with TIF and the GERDX™ procedure. GFET resulted in marked improvements in GERD-related QOL scores. Substantial reductions in the mean QOL scores at 6 and 12 months postoperatively were observed. These improvements were statistically significant and aligned with the positive outcomes associated with TIF and the GERDX™ procedure, which are known for their ability to enhance QOL and symptom relief[19]. However, the application of the GERDX™ procedure is limited, as it has only been used in two studies by Weitzendorfer et al[20] and Weitzendorfer et al[21] and a prospective clinical trial by Tschoner et al[22].
Furthermore, GFET resulted in a notable reduction in GERD symptoms. Endoscopic detection of GERD decreased significantly, from 13 patients at the time of the procedure to 1 patient at 12 months postoperatively. This trend is consistent with the efficacy of TIF and the GERDX™ procedures, which significantly reduced GERD symptoms and esophageal acid exposure[14,20].
A comparison of GFET and the GERDX™ procedure revealed that both procedures involve strategic placement of sutures around the GOJ to create a stronger and more circumferential pressure barrier than those in other procedures. However, GFET uses Prolene 2-0 sutures placed at specific positions, thus potentially offering enhanced durability and effectiveness through full-thickness sutures, whereas GERDX™ uses a similar but distinct endoscopic suturing system[22]. The outcomes of our study suggest that GFET may offer comparable, if not superior, long-term symptom relief and durability. Moreover, a comparison between GFET and TIF revealed notable differences, including the use of Prolene 2-0 sutures in GEFT vs the use of plastic fasteners in TIF[14]. Both techniques aim to create partial fundoplication, but the use of full-thickness sutures with GFET may provide more robust attachment and longer-lasting results[23].
This study indicated that GFET significantly improves QOL and reduces GERD symptoms and medication use, thus paralleling the positive outcomes reported for TIF. The minimally invasive nature and favorable safety profile of GFET, with low complication rates and only one adverse event recorded, are consistent with the outcomes reported for both TIF the GERDX™ procedure[22].
Additionally, GFET led to a substantial decrease in the use of anti-GERD medications. All patients used these medications at the time of the procedure; however, only one patient continued using the medications at 12 months postoperatively. This reduction in medication use is similar to that observed with TIF. Patients who underwent TIF often experience reduced dependence on PPIs and other GERD treatments postoperatively[19]. However, a study by Ebright et al[19] found that only 63% of patients discontinued PPIs. Seven cases of grade 2 complications and one grade 3 complication were identified after TIF; however, we observed only one case of complication with GFET[19].
GFET appears to be a viable and effective alternative to existing endoscopic treatment methods for GERD because it allows significant improvements in patient outcomes and is minimally invasive. Further long-term studies are recommended to validate these findings and explore the potential advantages of GFET over TIF and the GERDX™ procedure.
Despite these positive outcomes, this study had some limitations. The small sample size and single-center design may have affected the generalizability of the results.
GFET, which utilizes the GEN-2 Apollo endosuture device and specific suture placement, significantly improved GERD-related QOL, reduced GERD symptoms, and decreased the need for anti-GERD medications. These results suggest that GFET is a viable and minimally invasive option for managing GERD, offering substantial benefits over traditional surgical and endoscopic methods. Multicenter studies involving larger populations and long-term follow-up are necessary to confirm these findings and optimize the technique.
| 1. | Höllwarth ME, Solari V. Gastroesophageal Reflux Disease. Pediatric Surgery. Switzerland: Springer Cham, 2023. [DOI] [Full Text] |
| 2. | Zhang D, Liu S, Li Z, Wang R. Global, regional and national burden of gastroesophageal reflux disease, 1990-2019: update from the GBD 2019 study. Ann Med. 2022;54:1372-1384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 94] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 3. | Chatila AT, Nguyen MTT, Krill T, Roark R, Bilal M, Reep G. Natural history, pathophysiology and evaluation of gastroesophageal reflux disease. Dis Mon. 2020;66:100848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Wang JH, Luo JY, Dong L, Gong J, Tong M. Epidemiology of gastroesophageal reflux disease: a general population-based study in Xi'an of Northwest China. World J Gastroenterol. 2004;10:1647-1651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 113] [Cited by in RCA: 117] [Article Influence: 5.6] [Reference Citation Analysis (1)] |
| 5. | Watanabe Y, Fujiwara Y, Shiba M, Watanabe T, Tominaga K, Oshitani N, Matsumoto T, Nishikawa H, Higuchi K, Arakawa T. Cigarette smoking and alcohol consumption associated with gastro-oesophageal reflux disease in Japanese men. Scand J Gastroenterol. 2003;38:807-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | De Giorgi F, Palmiero M, Esposito I, Mosca F, Cuomo R. Pathophysiology of gastro-oesophageal reflux disease. Acta Otorhinolaryngol Ital. 2006;26:241-246. [PubMed] |
| 7. | El-Serag H. The association between obesity and GERD: a review of the epidemiological evidence. Dig Dis Sci. 2008;53:2307-2312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 206] [Cited by in RCA: 187] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 8. | Newberry C, Lynch K. The role of diet in the development and management of gastroesophageal reflux disease: why we feel the burn. J Thorac Dis. 2019;11:S1594-S1601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 9. | Lei WY, Vaezi MF, Naik RD, Chen CL. Mucosal impedance testing: A new diagnostic testing in gastroesophageal reflux disease. J Formos Med Assoc. 2020;119:1575-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Ahmed A, Clarke JO. Proton Pump Inhibitors (PPI). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2024. [PubMed] |
| 11. | Ness-Jensen E, Hveem K, El-Serag H, Lagergren J. Lifestyle Intervention in Gastroesophageal Reflux Disease. Clin Gastroenterol Hepatol. 2016;14:175-82.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 218] [Cited by in RCA: 182] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 12. | Lundell L. Complications after anti-reflux surgery. Best Pract Res Clin Gastroenterol. 2004;18:935-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Tian ZC, Wang B, Shan CX, Zhang W, Jiang DZ, Qiu M. A Meta-Analysis of Randomized Controlled Trials to Compare Long-Term Outcomes of Nissen and Toupet Fundoplication for Gastroesophageal Reflux Disease. PLoS One. 2015;10:e0127627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 14. | Fernando HC. Endoscopic fundoplication: patient selection and technique. J Vis Surg. 2017;3:121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | The Gastro Clinic. STRETTA Relief for Chronic GERD. Available from: https://www.gastroclinic.com/technology/stretta/. |
| 16. | Lopes G, Wu Y, Kudaba I, Kowalski D, Cho BC, Castro G, Srimuninnimit V, Bondarenko I, Kubota K, Lubiniecki GM, Zhang J, Kush DA, Mok T. Pembrolizumab (pembro) versus platinum-based chemotherapy (chemo) as first-line therapy for advanced/metastatic NSCLC with a PD-L1 tumor proportion score (TPS) ≥ 1%: Open-label, phase 3 KEYNOTE-042 study. J Clin Oncol. 2018;36:LBA4-LBA4. [RCA] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 121] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 17. | Akcelik A, Miller C, Bakhos C, Abbas A, Petrov R. Endoscopic interventions in the management of the gastroesophageal reflux: a narrative review. Ann Esophagus. 2023;6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Lee DP, Chang KJ. Endoscopic Management of GERD. Dig Dis Sci. 2022;67:1455-1468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 19. | Ebright MI, Sridhar P, Litle VR, Narsule CK, Daly BD, Fernando HC. Endoscopic Fundoplication: Effectiveness for Controlling Symptoms of Gastroesophageal Reflux Disease. Innovations (Phila). 2017;12:180-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Weitzendorfer M, Spaun GO, Antoniou SA, Witzel K, Emmanuel K, Koch OO. Clinical feasibility of a new full-thickness endoscopic plication device (GERDx™) for patients with GERD: results of a prospective trial. Surg Endosc. 2018;32:2541-2549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 21. | Weitzendorfer M, Spaun GO, Antoniou SA, Tschoner A, Schredl P, Emmanuel K, Koch OO. Interim Report of a Prospective Trial on the Clinical Efficiency of a New Full-thickness Endoscopic Plication Device for Patients With GERD: Impact of Changed Suture Material. Surg Laparosc Endosc Percutan Tech. 2017;27:163-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Tschoner A, Punkenhofer P, Spaun G, Koch O, Fuegger R. 235 5-Year Follow-Up of a Prospective Clinical Trial of an Endoscopic Full-Thickness Plication Device (Gerdx™) for the Treatment of Gerd. Diseases of the Esophagus. 2021;34. [DOI] [Full Text] |
| 23. | Huang X, Chen S, Zhao H, Zeng X, Lian J, Tseng Y, Chen J. Efficacy of transoral incisionless fundoplication (TIF) for the treatment of GERD: a systematic review with meta-analysis. Surg Endosc. 2017;31:1032-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 88] [Article Influence: 11.0] [Reference Citation Analysis (0)] |