Published online May 16, 2023. doi: 10.4253/wjge.v15.i5.386
Peer-review started: February 17, 2023
First decision: March 28, 2023
Revised: April 10, 2023
Accepted: April 18, 2023
Article in press: April 18, 2023
Published online: May 16, 2023
Processing time: 88 Days and 7 Hours
Large appendiceal orifice polyps are traditionally treated surgically. Recently, endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) have been utilized as alternative resection techniques.
To evaluate the efficacy and safety of endoscopic resection techniques for the management of large appendiceal orifice polyps.
This was a retrospective observational study conducted to assess the feasibility and safety of EMR and ESD for large appendiceal orifice polyps. This project was approved by the Baylor College of Medicine Institutional Review Board. Patients who underwent endoscopic resection of appendiceal orifice polyps ≥ 1 cm from 2015 to 2022 at a tertiary referral endoscopy center in the United States were enrolled. The main outcomes of this study included en bloc resection, R0 resection, post resection adverse events, and polyp recurrence.
A total of 19 patients were identified. Most patients were female (53%) and Caucasian (95%). The mean age was 63.3 ± 10.8 years, and the average body mass index was 28.8 ± 6.4. The mean polyp size was 25.5 ± 14.2 mm. 74% of polyps were localized to the appendix (at or inside the appendiceal orifice) and the remaining extended into the cecum. 68% of polyps occupied ≥ 50% of the appendiceal orifice circumference. The mean procedure duration was 61.6 ± 37.9 minutes. Polyps were resected via endoscopic mucosal resection, endoscopic submucosal dissection, and hybrid procedures in 5, 6, and 8 patients, respectively. Final pathology was remarkable for tubular adenoma (n = 10) [one with high grade dysplasia], sessile serrated adenoma (n = 7), and tubulovillous adenoma (n = 2) [two with high grade dysplasia]. En bloc resection was achieved in 84% with an 88% R0 resection rate. Despite the large polyp sizes and challenging procedures, 89% (n = 17) of patients were discharged on the same day as their procedure. Two patients were admitted for post-procedure observation for conservative pain management. Eight patients underwent repeat colonoscopy without evidence of residual or recurrent adenomatous polyps.
Our study highlights how endoscopic mucosal resection, endoscopic submucosal dissection, and hybrid procedures are all appropriate techniques with minimal adverse effects, further validating the utility of endoscopic procedures in the management of large appendiceal polyps.
Core Tip: In this study, we evaluated endoscopic mucosal resection, endoscopic submucosal dissection, and hybrid procedures for the resection of large appendiceal polyps. Compared to previously published studies, we noticed a higher en bloc resection rate and R0 resection rate in our study, despite a larger polyp size. Our data supported these procedures as safe and efficacious for the management of large polyps in a challenging location such as the appendiceal orifice, with minimal to no adverse events.
- Citation: Patel AP, Khalaf MA, Riojas-Barrett M, Keihanian T, Othman MO. Expanding endoscopic boundaries: Endoscopic resection of large appendiceal orifice polyps with endoscopic mucosal resection and endoscopic submucosal dissection. World J Gastrointest Endosc 2023; 15(5): 386-396
- URL: https://www.wjgnet.com/1948-5190/full/v15/i5/386.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i5.386
Appendiceal orifice polyps are usually found during autopsy or surgery, with an estimated prevalence of 0.08%[1]. According to the Size, Morphology, Site, Access scoring system that has been proposed to determine the complexity of polypectomy, appendiceal polyps are often classified as “high risk polyps”[2]. Traditionally, despite being visualized by colonoscopy, many of these polyps are referred for surgical resection[3].
Although removal of minute appendiceal orifice polyps is feasible, larger lesions are harder to remove and require advanced endoscopic resection techniques. More recently, many expert endoscopists have considered endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), or full thickness resection (FTR) for the removal of complex appendiceal orifice polyps. Multiple studies have highlighted the predominance of EMR over ESD for the management of appendiceal polyps[4,5]. The anatomic configuration of the appendix makes it difficult to perform ESD for appendiceal polyps. Challenges include limited room for scope maneuverability, higher risk of perforation, limited available devices for appropriate closure post-ESD due to polyp location, and higher risk of appendicitis after complete resection. Because of these challenges and limited expertise in colonic resection with ESD in the Western population, ESD has not been the preferred method of resection for large appendiceal polyps.
With evolving advances in the field of endoscopic resection, removing complex appendiceal polyps has become the preferred approach. However, there is still limited published data examining advanced resection techniques for appendiceal polyps. Data on outcomes of endoscopic resection of large appendiceal orifice polyps is especially lacking in the Western population. Thus, the aim of this study is to evaluate the efficacy and safety of EMR and ESD for the management of appendiceal orifice polyps at a tertiary referral center in the United States.
This was a retrospective observational study conducted to assess the feasibility and safety of EMR and ESD for large appendiceal orifice polyps. This project was approved by the Baylor College of Medicine Institutional Review Board.
Patients who underwent endoscopic resection of appendiceal orifice polyps ≥ 1 cm by EMR or ESD from 2015 to 2022 at Baylor St. Luke’s Medical Center were qualified for initial enrollment. Inclusion criteria included adult patients (ages 18 years and older) and polyp size ≥ 1 cm. Exclusion criteria included pediatric patients (less than 18 years of age), patients with polyps < 1 cm, and patients with a history of a prior appendiceal orifice polypectomy.
The decision to define large appendiceal polyps as ≥ 1 cm was based on the following. Multiple prior studies that evaluated endoscopic resection had average appendiceal polyp sizes around 1 cm[4-6]. Additionally, two other studies had average polyp sizes around 1.5 cm[7,8]. Furthermore, one of these prior studies showed that the odds of polyp recurrence can potentially increase by 3.2 times in polyps ≥ 1 cm with conventional polyp removal techniques[4], so we wanted to specifically evaluate outcomes in this population.
All procedures were performed by one advanced endoscopist experienced in endoscopic resection techniques. All procedures were performed using Pentax EC38-i10L adult colonoscopes (Pentax America, Montvale, NJ, United States). The technique of performing EMR or ESD has been described elsewhere[9]. In brief, EMR was performed using an assisted lifting technique with saline mixed with methylene blue. ESD was performed using a dual knife (Olympus America, Center Valley, PA, United States) or Orise Knife (Boston Scientific, Marlborough, MA, United States). The decision to perform EMR or ESD was based on the endoscopist’s discretion, depending on lesion size and time allotted to perform the procedure. In certain occasions, hybrid EMR/ESD technique was used to expedite the procedure or to facilitate resection when ESD was not feasible. The hybrid EMR/ESD technique involves a circumferential incision of the lesion margins by dual knife, followed by snare resection of the lesion in one or multiple pieces. Post-EMR and ESD defects were routinely closed using Instinct or Instinct plus clip (Cook Medical, Winston Salem, NC, United States). Stabilization devices such as Dilumen (Lumendi, Westport, CT, United States) or Pathfinder (Neptune Medical, Burlingame, CA, United States) were selectively used in some procedures where significant looping or scope instability hindered the performance of endoscopic resection. Patients were scheduled for a follow up colonoscopy in 6 mo to 1 year.
EMR was considered for the resection of pedunculated or sessile appendiceal polyps that were smaller than 1.5 cm, did not extend into the appendiceal orifice, and were easily liftable after injecting solution. ESD and hybrid EMR/ESD were considered for polyps that extended into the appendiceal orifice, flat polyps, polyps with underlying scar and previous manipulation, or polyps that did not adequately lift after injecting solution. The overall goal was to achieve en bloc resection.
Outcome data included en bloc resection, R0 resection rate, hospitalizations, post-procedure adverse events, and polyp recurrence on follow up colonoscopy. Demographic variables [age, sex, race, body mass index (BMI)] and clinical history were collected retrospectively by chart review. Endoscopic appearance of polyps, including size, appearance, location (including degree of lateral spreading), Paris Classification, and lesion fibrosis were collected as well. Endoscopic procedure variables included procedure duration (including clip-closure time), technique, type of ESD knife, use of traction and stabilization methods, number of clips used for closure, need for hemostasis, adverse events, and recurrence rates.
En bloc resection was defined as resection of the entire polyp in one piece. R0 (complete) resection was defined as en bloc resection with negative horizontal and vertical margins. Curative resection was defined as histological complete resection with no risk of lymph node metastasis by histological examination of the resected specimen, according to the Japanese Society for Cancer of the Colon and Rectum guideline criteria[10]. Patients with piecemeal or R1 resection were considered to not have achieved curative resection.
Procedure time was defined as the time from introduction of the colonoscope into the rectum until withdrawal of the colonoscope. Postoperative bleeding was defined as immediate and long-term bleeding (defined as up to 2 wk after the procedure) from the polypectomy site that resulted in rectal bleeding or melena. Perforation was defined as transmural injury of the bowel wall resulting in free air in the abdomen. Appendicitis was defined as inflammation of the appendix at any time period after polypectomy.
Descriptive statistics were performed using means and standard deviations (SD) for continuous variables, and frequency and percentages for categorical variables. Analysis of variance was used to evaluate continuous variables, where appropriate. A P value of less than 0.05 was considered statistically significant. All analyses were performed using built-in Microsoft Excel 2019 software packages. The statistical review of the study was performed by a biomedical statistician.
A total of 19 patients with appendiceal polyps were identified (Table 1). Most patients were female (53%) and Caucasian (95%). The mean age was 63.3 ± 10.8 (SD) years, and the average BMI was 28.8 ± 6.4. Patients were categorized as having an American Society of Anesthesiology score of II and III in 43% (n = 10) and 47% (n = 9) of cases, respectively.
| Total patients (n = 19) | |
| Age, yr (mean ± SD) | 63.3 ± 10.8 |
| BMI, kg/m2(mean ± SD) | 28.9 ± 6.4 |
| Sex | |
| Male | 9 (47) |
| Female | 10 (53) |
| Race | |
| Caucasian | 18 (95) |
| African American | 1 (5) |
| Comorbidities | |
| Family history of colon cancer | 0 (0) |
| Smoking history | 9 (47) |
| Alcohol use | 12 (63) |
| COPD | 2 (11) |
| CAD | 2 (11) |
| ESRD | 0 (0) |
| Prior appendectomy | 2 (11) |
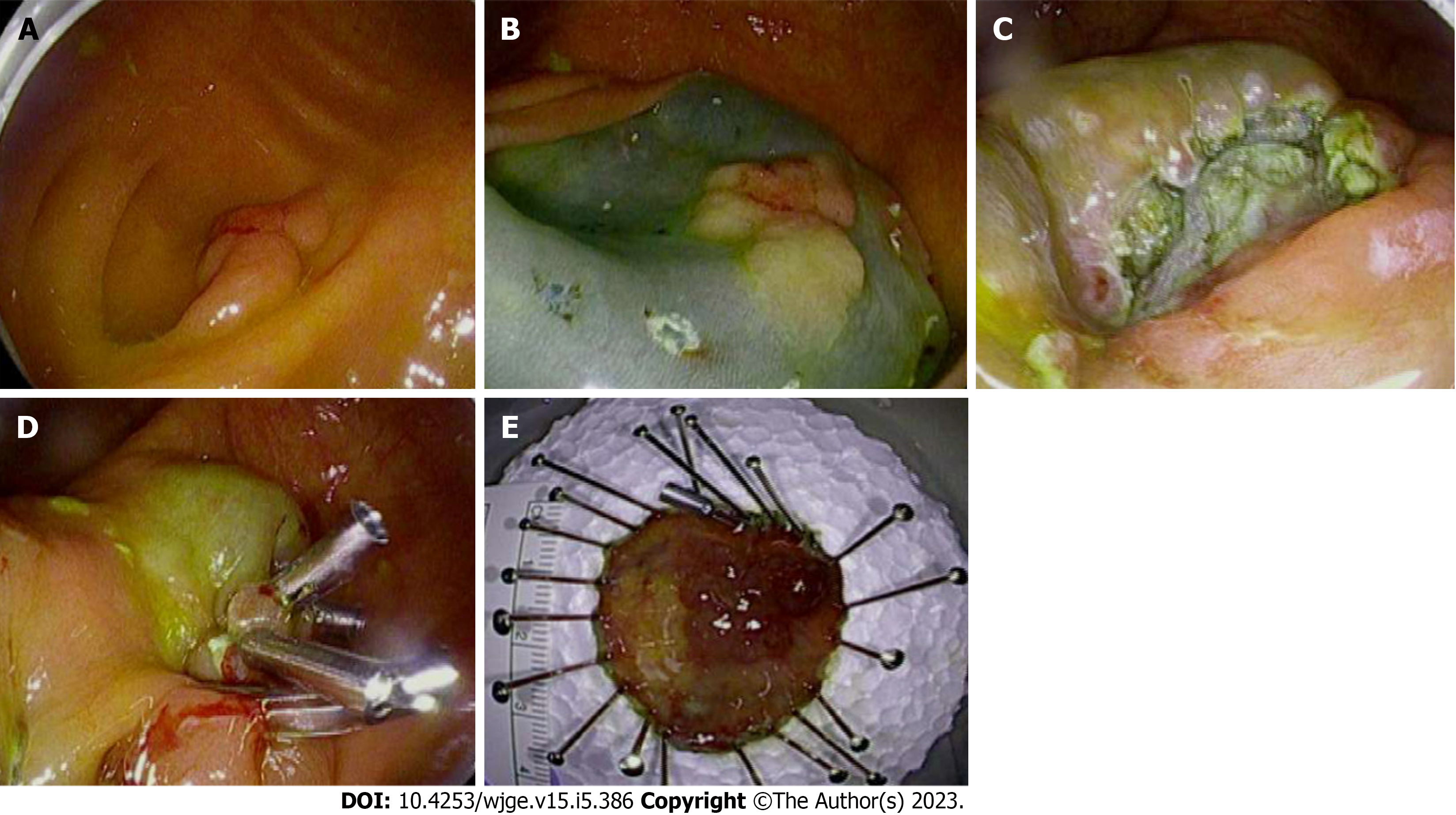
The mean appendiceal polyp size was 25.5 ± 14.2 mm (min: 10 mm - max: 60 mm) (Table 2). 74% of polyps were localized to the appendix (at or inside the appendiceal orifice) and the remaining extended into the cecum. 68% of polyps occupied ≥ 50% of the appendiceal orifice circumference. Two polyps (11%) covered the entire appendiceal orifice, while five polyps (26%) covered 75%-80% of the appendiceal orifice. Figure 1 demonstrates ESD of a 30mm polyp. Twelve polyps were classified as Is under the Paris classification (protruding and pedunculated). Final pathology was remarkable for tubular adenoma (n = 10) (one with high grade dysplasia), sessile serrated adenoma (n = 7), and tubulovillous adenoma (n = 2) (two with high grade dysplasia). Two polyps that were removed by hybrid EMR/ESD were noted to have submucosal fibrosis.
| Total | EMR | ESD | Hybrid EMR/ESD | P value | |
| Total patients (n) | 19 | 5 | 6 | 8 | |
| Polyp Appearance (mean ± SD) | |||||
| Size (mm) | 25.5 ± 14.2 | 26.0 ± 13.4 | 25.0 ± 18.4 | 25.6 ± 13.2 | 0.99 |
| Localized to appendix (at or inside the appendiceal orifice) | 14 (74) | 3 (60) | 6 (100) | 5 (63) | |
| 50% or more involvement of the appendiceal orifice | 13 (68) | 3 (60) | 5 (83) | 5 (63) | |
| Granular, lateral-spreading | 5 (26) | 0 (0) | 2 (33) | 3 (30) | |
| Flat, lateral-spreading | 1 (5) | 0 (0) | 0 (0) | 1 (13) | |
| Not lateral-spreading | 13 (68) | 5 (100) | 4 (67) | 4 (50) | |
| Paris classification: Is | 12 (63) | 3 (60) | 2 (33) | 7 (88) | |
| Lesion fibrosis | 2 (11) | 0 (0) | 0 (0) | 2 (25) | |
| Procedure (mean ± SD) | |||||
| Duration of Procedure (min) | 61.6 ± 37.9 | 43.8 ± 31.5 | 71.0 ± 54.4 | 65.8 ± 26.1 | 0.48 |
| Procedures needing clips | 18 (95) | 4 (80) | 6 (100) | 8 (100) | |
| Number of clips used | 3.9 ± 1.6 | 2.8 ± 0.5 | 3.5 ± 2.2 | 5.0 ± 1.2 | 0.02 |
| Additional resection of non-appendiceal polyps | 4 (21) | 2 (40) | 0 (0) | 2 (25) | |
| ESD knife used (DualKnife/Orise ProKnife) | N/A | N/A | 4/2 (67/33) | 7/1 (88/12) | |
| Traction method used | 3 (21) | 0 (0) | 1 (16.7) | 2 (25) | |
| Stabilization (Dilumen or Pathfinder) | 10 (53) | 1 (20) | 4 (67) | 5 (63) | |
| Hemostasis needed (with Cograsper) | 3 (16) | 0 (0) | 2 (33) | 1 (13) | |
| Outcome (mean ± SD) | |||||
| Admission for post-procedure observation | 2 (11) | 0 (0) | 1 (17) | 1 (13) | |
| Duration of Admission (d) | 2.5 ± 2.1 | 0 ± 0 | 4.0 ± 0 | 1.0 ± 0 | |
| Post-Procedure Pain | 1 (5) | 0 (0) | 1 (17) | 0 (0) | |
| Adenoma on pathology report | 19 (100) | 5 (100) | 6 (100) | 8 (100) | |
| Submucosal/Perineural/Lymphovascular Invasion | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| R0 rate for en bloc resection | 14 (88)a | 4 (80) | 6 (100) | 4 (80)a | 0.56 |
| Curative resection rate | 14 (74) | 4 (80) | 6 (100) | 4 (50) | 0.11 |
| En Bloc resection rate | 16 (84) | 5 (100) | 6 (100) | 5 (63) | 0.09 |
| Repeat colonoscopy done | 8 (57)b | 0 (0) | 2 (67)b | 6 (75) |
Polyps were removed via hybrid EMR/ESD, ESD and EMR techniques in 8, 6 and 5 patients, respectively. The mean procedure duration was 61.6 ± 37.9 min. Ten procedures (53%) required a stabilization device over the colonoscope (Dilumen or Pathfinder). This occurred mainly in ESD or hybrid EMR/ESD procedures (n = 9). In order to facilitate dissection, traction was performed in two procedures with a Dilumen double balloon platform and one procedure with a rubber-band clip. A 1.5 mm DualKnife was used in 4 patients who underwent ESD and 7 patients who underwent hybrid EMR/ESD. The remaining polyps were removed using a 2 mm Orise ProKnife. Post-polypectomy defects were closed in all cases, except in one patient with a 20 mm polyp that was removed via EMR. An average of 3.9 ± 1.6 clips were used for defect closure.
The overall en bloc resection rate was 84%. The en bloc resection rate was 100% for the EMR and ESD groups, and 63% for the hybrid EMR/ESD group. The overall R0 resection rate for en bloc resected polyps was 88%. R0 resection rates for the EMR group, ESD group, and hybrid EMR/ESD group were 80%, 100% and 80%, respectively. The overall curative resection rate was 74%. Curative resection rates were 80% for the EMR group, 100% for the ESD group, and 50% for the hybrid EMR/ESD group.
No major adverse events, such as bleeding or perforation, were observed. Despite the large polyp sizes and challenging procedures, 89% (n = 17) of patients were discharged on the same day as their procedure. Two patients were admitted post-procedure for conservative pain control, for one and four days, respectively. One patient developed delayed appendicitis and required appendectomy four months after hybrid EMR/ESD polyp resection.
Eight patients (57%) had a repeat colonoscopy, with 2 from the ESD group and 6 from the hybrid EMR/ESD group. The average length of follow up was 365 ± 281 d. There was no evidence of polyp recurrence in any of the patients with available follow up colonoscopy.
There was no statistically significant difference in tumor size amongst the EMR, ESD, and hybrid EMR/ESD groups (P value = 0.99). Although the average time for ESD and hybrid procedures were slightly higher in comparison to EMR, no statistically significant difference was observed (P value = 0.48). The average procedure time (P value = 0.76) and polyp size (P value = 0.94) were not significantly different if stabilization with overtube was used. The en bloc resection rate (P value = 0.09), R0 resection rate (P value = 0.56), and curative resection rate (P value = 0.11) did not significantly differ between the three groups (Table 2).
In this single center study, we observed an 84% en bloc resection rate and 88% R0 rate for en bloc resection of large appendiceal orifice polyps. When compared against each other, EMR, ESD, and hybrid EMR/ESD procedures all revealed similar efficacy without significant differences in procedure time, R0 resection rate, en bloc resection rate, or adverse effects.
There has been an increasing interest in natural orifice transluminal endoscopic surgery (NOTES) for removal of complex polyps, due to advances in third space endoscopy. It is associated with less post-procedural morbidity and adverse events, is cost effective, and leads to a decreased length of hospital stay[11-19].
There are a limited number of published literatures addressing the efficacy of advanced endoscopic resection for appendiceal polyps. Furthermore, many of the existing studies involve smaller appendiceal polyps when compared to our study. In a retrospective study by Hassab et al[4], 28 patients with appendiceal polyps underwent removal with EMR or ESD technique, with a median polyp size of 10 mm. Song et al[5] in their study of 131 patients (median polyp size 10mm), utilized piecemeal EMR as the most common method of resection (57.3%), followed by EMR (23.3%) and ESD (3.8%). In this study, en bloc resection was only achieved in 68.7% with a reported 90% R0 resection rate. Underwater EMR yielded en bloc resection in only 59% of 27 patients with appendiceal polyps (average polyp size 15 mm), in another study by Binmoeller et al[8]. In comparison to the published literature, our study observed higher en bloc and R0 resection rates, despite a larger average polyp size. There are two studies focusing on the role of ESD in the management of appendiceal polyps. In one Japanese study of 76 polyps (median size 35.5 mm) in the cecum adjacent to the appendix (only 29 located at the orifice), en bloc resection and R0 resection were achieved in 94.7% and 92.1% of the patients, respectively[20]. In another Japanese study of 27 appendiceal orifice polyps (mean size 31.8 mm), en bloc resection and R0 resection were achieved in 77.8% and 70.4% of patients, respectively[21].
In order to improve en bloc resection of challenging appendiceal polyps, there are two published studies demonstrating the utility of FTR. In a single center study of seven patients with appendiceal polyps that underwent polypectomy via FTR (polyp size min: 5 mm - max: 20 mm), en bloc resection and R0 resection rates were 100% and 85.7%, respectively[7]. In another multicenter study of 66 polyps (mean polyp size 14.5 ± 6.2 mm), en bloc resection was achieved in 80% with a reported R0 resection rate of 93%[6].
En bloc resection of appendiceal polyps can vary from 59% to 100%, depending on the polyp size and resection method as discussed earlier. In our cohort, 74% of polyps were resected via ESD or hybrid EMR/ESD, despite our larger average polyp size (median 20 mm, min: 10 mm - max: 60 mm). Comparatively, we observed a higher en bloc resection rate (84%) and R0 rate for en bloc resection (88%). Furthermore, our procedure times compared similarly to the aforementioned studies.
As ESD technique yields en bloc resection, it has been associated with lower recurrence rates in comparison to conventional EMR techniques[22]. The recurrence rate after appendiceal polyp resection has been varied in the literature, depending on the removal method. The reported incidence of recurrence ranges from 10% with underwater EMR to 15.6% when conventional polyp removal techniques have been applied[4,5,8]. The odds of polyp recurrence can potentially increase by 3.2 times in polyps ≥ 10 mm with conventional polyp removal techniques[4]. In our study, due to a higher proportion of en bloc polyp removal via ESD and hybrid EMR/ESD, we observed no polyp recurrence in our eight patients with available follow up colonoscopy.
Adverse events such as bleeding or perforation after appendiceal polypectomy have been reported in up to 14.5% of patients that underwent EMR or ESD[5,20]. Although appendiceal polyp sizes ≥ 20 mm have been described as a risk factor for developing adverse events[5], no major adverse events such as bleeding or perforation were observed in our study, despite our larger average polyp size. This may have been a result of operator experience, as all procedures were performed by a single operative with enhanced experience in performing third space endoscopy.
One of the unique adverse events after endoscopic resection of appendiceal and peri-appendiceal polyps is appendicitis, as a result of post-polypectomy edema and cautery effect adjacent to the appendiceal orifice. Appendicitis has been reported in up to 17% of cases in the literature, although the majority of cases occurred < 10 d after endoscopy and all cases occurred < 1 mo after endoscopy[6,23,24]. Only one patient in our cohort developed appendicitis requiring laparoscopic appendectomy, although the event occurred four months after hybrid EMR/ESD, suggesting that her appendicitis was not related to her polypectomy. In our study, clipping was attempted in all cases, except for one case where a polyp with Paris classification Ip was not invading the appendiceal orifice. This patient did not develop appendicitis or require appendectomy. Nevertheless, clipping should still be attempted to prevent postoperative appendicitis. In our study, despite larger polyps and challenging polyp locations, same day discharge was achieved in 89.5% of patients.
Advanced polypectomy of appendiceal polyps with ESD or hybrid EMR/ESD seems to be a safe and effective method for the management of large polyps at a challenging location such as the appendiceal orifice, with minimal to no adverse events. However, resection of appendiceal polyps via advanced endoscopic techniques requires a certain expertise due to the difficult location and anatomical configuration of the appendix. One of the main challenges encountered during polyp resection within the right side of the colon, and in particular at the appendiceal orifice, is maintaining scope stability. Ismail et al[9] have previously described the utility of the DiLumen platform for scope stability and expedited resection in challenging polyp locations. In our cohort, scope stabilization with the Dilumen platform or Pathfinder overtube was utilized in half of the cases (52.6%) to assist with stability and facilitate dissection, especially in ESD or hybrid EMR/ESD. Utilization of these devices provided adequate visualization of the dissection plane and made ESD resection easier, without any significant difference in procedure time (P value = 0.76). Another technique to consider when removing appendiceal polyps would be applying traction in order to relocate the polyp in various orientations, to assist with dissection and the plane of view[25,26]. In our study, traction with Dilumen and rubber-band traction resulted in expedited dissection as well as polyp resection in a safe manner.
After evaluating our study and prior evidence, we suggest that EMR is safe for pedunculated appendiceal polyps not extending into the orifice, smaller than 15 mm, and easily liftable after injecting solution. For polyps that extend into appendiceal orifice, flat polyps, polyps with underlying scar and previous manipulation, and polyps not adequately lifting, ESD and hybrid EMR/ESD should be chosen. The overall goal should be to achieve en bloc resection.
For evaluation of polyps that may require surgical intervention, the Japanese Gastroenterological Endoscopy Society guidelines for ESD and EMR can be utilized[27]. Criteria for surgery may include polyps that meet deep invasion guidelines or have increased concern for malignancy. We suggest that appendiceal orifice polyps that are larger than 2 cm should be evaluated on a case to case basis in a multi-disciplinary team for consideration of surgical or endoscopic resection. This decision may vary by institution, depending on the availability of expertise in complex endoscopic resection. Furthermore, patient comorbidities must be considered when pursuing surgical intervention.
Narrow band imaging (NBI), white light endoscopy, and chromoendoscopy are also strategies that can be considered to aid in the detection of high-risk polyps that may harbor advanced neoplasia and require surgical resection rather than endoscopic intervention[28]. Based on the NBI International Colorectal Endoscopic Classification (NICE) criteria, type 2 Lesions can be addressed with endoscopic resection, while type 3 Lesions should be referred for surgical resection[29].
There are many strengths to our study, including an in-depth evaluation of innovative endoscopic procedures for the resection of large appendiceal polyps ≥ 1 cm. Furthermore, we assessed EMR, ESD, and hybrid procedures, identifying the efficacy and safety of these procedures in the management of large appendiceal orifice polyps. This study has certain limitations as well. This is a single center retrospective study with a non-randomized controlled trial design and a limited number of patients, which may limit its generalizability to a larger population. All procedures were performed by a single operative with enhanced experience in performing third space endoscopy. Furthermore, follow up colonoscopy information is missing in some patients that were due for repeat colonoscopy, due to the retrospective nature of the study and lack of patient follow up despite multiple attempts. Although no major adverse events were noted in our study and the removal of complex appendiceal polyps appears to be safe, larger prospective trials are needed to efficiently demonstrate the utility and safety of advanced endoscopic polyp resection techniques in the challenging appendiceal orifice location, in the hands of experienced and naïve endoscopists.
In conclusion, although appendiceal polyps are frequently referred for surgical resection, endoscopic techniques including EMR and ESD are efficacious and safe methods for large polyp removal. The results of our study are comparative to the previous published studies, with higher en bloc resection and R0 resection rates in our study despite a larger average polyp size.
Appendiceal orifice polyps are often referred for surgical resection. More recently, endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) have been considered by expert advanced endoscopists for the removal of complex appendiceal polyps.
However, there is still limited published data investigating EMR and ESD for appendiceal polyps in the Western population.
The main objective of this study is to evaluate the safety and efficacy of EMR and ESD for the management of complex appendiceal orifice polyps.
This was a retrospective observation study involving adult patients who underwent endoscopic resection of appendiceal orifice polyps ≥ 1 cm by EMR, ESD, or hybrid EMR/ESD from 2015 to 2022 at Baylor St. Luke’s Medical Center. All procedures were performed by one advanced endoscopist experienced in endoscopic resection. Data collection included demographic information, polyp characteristics, procedure details, and procedure outcomes. The main outcomes of interest were en bloc resection rate, R0 resection rate, and adverse events.
A total of 19 patients were identified, with a mean polyp size of 25.5 ± 14.2 mm. The overall en bloc resection rate was 84%, with an R0 resection rate of 88% and no significant difference in between EMR, ESD, and hybrid EMR/ESD. 89% of patients were discharged on the same day as their procedure, with only two patients admitted conservatively post-procedure for pain management. Despite our larger overall polyp size, we observed high en bloc and R0 resection rates for EMR, ESD, and hybrid EMR/ESD procedures without any significant adverse effects.
In conclusion, EMR and ESD are efficacious and safe techniques for large appendiceal orifice polyp removal.
Future large, prospective trials can be conducted to demonstrate the safety and utility of EMR and ESD for the resection of complex appendiceal polyps. These studies can also incorporate both experienced and naïve endoscopists across multiple centers in the United States.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Association for the Study of Liver Diseases, No. 263777; American Association for the Study of Liver Diseases, No. 66811.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Osera S, Japan; Viswanath YK, United Kingdom; Zhang J, China S-Editor: Liu JH L-Editor: A P-Editor: Cai YX
| 1. | Author commentary on Abdulbaqi Al-Toma et al. Endoscopy. 2022;54:v37. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Gupta S, Miskovic D, Bhandari P, Dolwani S, McKaig B, Pullan R, Rembacken B, Rutter MD, Riley S, Valori R, Vance ME, Faiz OD, Saunders BP, Thomas-Gibson S. The ‘SMSA’ Scoring System for Determining the Complexity of a Polyp. Gut. 2011;60:A129-A129. [DOI] [Full Text] |
| 3. | Tholoor S, Tsagkournis O, Basford P, Bhandari P. Managing difficult polyps: techniques and pitfalls. Ann Gastroenterol. 2013;26:114-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Hassab TH, Church JM. Appendix orifice polyps: a study of 691 lesions at a single institution. Int J Colorectal Dis. 2019;34:711-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Song EM, Yang HJ, Lee HJ, Lee HS, Cha JM, Kim HG, Jung Y, Moon CM, Kim BC, Byeon JS. Endoscopic Resection of Cecal Polyps Involving the Appendiceal Orifice: A KASID Multicenter Study. Dig Dis Sci. 2017;62:3138-3148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Ichkhanian Y, Barawi M, Seoud T, Thakkar S, Kothari TH, Halabi ME, Ullah A, Edris W, Aepli P, Kowalski T, Shinn B, Shariaha RZ, Mahadev S, Mosko JD, Andrisani G, Di Matteo FM, Albrecht H, Giap AQ, Tang SJ, Naga YM, van Geenen E, Friedland S, Tharian B, Irani S, Ross AS, Jamil LH, Lew D, Nett AS, Farha J, Runge TM, Jovani M, Khashab MA. Endoscopic full-thickness resection of polyps involving the appendiceal orifice: a multicenter international experience. Endoscopy. 2022;54:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Bronzwaer MES, Bastiaansen BAJ, Koens L, Dekker E, Fockens P. Endoscopic full-thickness resection of polyps involving the appendiceal orifice: a prospective observational case study. Endosc Int Open. 2018;6:E1112-E1119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Binmoeller KF, Hamerski CM, Shah JN, Bhat YM, Kane SD. Underwater EMR of adenomas of the appendiceal orifice (with video). Gastrointest Endosc. 2016;83:638-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Ismail MS, Bahdi F, Mercado MO, Habazi R, Alexander A, Prabhu S, John S, Kovvali C, Othman MO. ESD with double-balloon endoluminal intervention platform versus standard ESD for management of colon polyps. Endosc Int Open. 2020;8:E1273-E1279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K; Japanese Society for Cancer of the Colon and Rectum. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1024] [Cited by in RCA: 1311] [Article Influence: 262.2] [Reference Citation Analysis (1)] |
| 11. | Arulampalam T, Patterson-Brown S, Morris AJ, Parker MC. Consensus statement: natural orifice transluminal endoscopic surgery. Ann R Coll Surg Engl. 2009;91:456-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Liu BR, Ullah S, Ye L, Liu D, Mao X. Endoscopic transcecal appendectomy: a novel option for the treatment of appendiceal polyps. VideoGIE. 2019;4:271-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Wallace MB. Take NOTES (Natural Orifice Transluminal Endoscopic Surgery). Gastroenterology. 2006;131:11-12. [DOI] [Full Text] |
| 14. | Whiteford MH, Swanstrom LL. Emerging technologies including robotics and natural orifice transluminal endoscopic surgery (NOTES) colorectal surgery. J Surg Oncol. 2007;96:678-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Abdalla S, Meillat H, Fillol C, Zuber K, Manceau G, Dubray V, Beyer-Berjot L, Lefevre JH, Selvy M, Benoist S, Micelli Lupinacci R. Ileocecal Valve Sparing Resection for the Treatment of Benign Cecal Polyps Unsuitable for Polypectomy. JSLS. 2021;25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Fung TLD, Chan PT, Lee HM, Kwok KH. Case-Matched Analysis Comparing Endoscopic Submucosal Dissection and Surgical Removal of Difficult Colorectal Polyps. J Laparoendosc Adv Surg Tech A. 2018;28:1188-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Gamaleldin M, Benlice C, Delaney CP, Steele S, Gorgun E. Management of the colorectal polyp referred for resection: A case-matched comparison of advanced endoscopic surgery and laparoscopic colectomy. Surgery. 2018;163:522-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Keswani RN, Law R, Ciolino JD, Lo AA, Gluskin AB, Bentrem DJ, Komanduri S, Pacheco JA, Grande D, Thompson WK. Adverse events after surgery for nonmalignant colon polyps are common and associated with increased length of stay and costs. Gastrointest Endosc. 2016;84:296-303.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Yeh JH, Tseng CH, Huang RY, Lin CW, Lee CT, Hsiao PJ, Wu TC, Kuo LT, Wang WL. Long-term Outcomes of Primary Endoscopic Resection vs Surgery for T1 Colorectal Cancer: A Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol. 2020;18:2813-2823.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (1)] |
| 20. | Jacob H, Toyonaga T, Ohara Y, Tsubouchi E, Takihara H, Baba S, Yoshizaki T, Kawara F, Tanaka S, Ishida T, Hoshi N, Morita Y, Umegaki E, Azuma T. Endoscopic submucosal dissection of cecal lesions in proximity to the appendiceal orifice. Endoscopy. 2016;48:829-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 21. | Hotta K, Osera S, Shinoki K, Imai K, Ito S, Yamaguchi Y, Kishida Y, Takada K, Ono H. Feasibility of endoscopic submucosal dissection for cecal tumors involving the ileocecal valve or appendiceal orifice. J Gastroenterol Hepatol. 2022;37:1517-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Reference Citation Analysis (0)] |
| 22. | Rotermund C, Djinbachian R, Taghiakbari M, Enderle MD, Eickhoff A, von Renteln D. Recurrence rates after endoscopic resection of large colorectal polyps: A systematic review and meta-analysis. World J Gastroenterol. 2022;28:4007-4018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (2)] |
| 23. | Schmidbaur S, Wannhoff A, Walter B, Meier B, Schäfer C, Meining A, Caca K. Risk of appendicitis after endoscopic full-thickness resection of lesions involving the appendiceal orifice: a retrospective analysis. Endoscopy. 2021;53:424-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 24. | Falt P, Zapletalová J, Urban O. Endoscopic full-thickness resection versus endoscopic submucosal dissection in the treatment of colonic neoplastic lesions ≤ 30 mm-a single-center experience. Surg Endosc. 2022;36:2062-2069. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Kantsevoy SV, Thuluvath AJ, Raina A, Thuluvath PJ. Endoscopic en bloc removal of appendiceal polyp facilitated by traction. VideoGIE. 2019;4:136-139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Tamari H, Oka S, Ninomiya Y, Tanaka S, Chayama K. Use of a new traction device to expose the base of a pedunculated appendiceal polyp. VideoGIE. 2021;6:38-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 27. | Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Saitoh Y, Tsuruta O, Sugihara KI, Igarashi M, Toyonaga T, Ajioka Y, Kusunoki M, Koike K, Fujimoto K, Tajiri H. Japan Gastroenterological Endoscopy Society guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2020;32:219-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 272] [Article Influence: 54.4] [Reference Citation Analysis (0)] |
| 28. | Singh R, Owen V, Shonde A, Kaye P, Hawkey C, Ragunath K. White light endoscopy, narrow band imaging and chromoendoscopy with magnification in diagnosing colorectal neoplasia. World J Gastrointest Endosc. 2009;1:45-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Patrun J, Okreša L, Iveković H, Rustemović N. Diagnostic Accuracy of NICE Classification System for Optical Recognition of Predictive Morphology of Colorectal Polyps. Gastroenterol Res Pract. 2018;2018:7531368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |