Published online Mar 16, 2023. doi: 10.4253/wjge.v15.i3.146
Peer-review started: November 21, 2022
First decision: January 2, 2023
Revised: January 15, 2023
Accepted: February 21, 2023
Article in press: February 21, 2023
Published online: March 16, 2023
Processing time: 114 Days and 18.4 Hours
Oesophagogastroduodenoscopy is the gold standard investigation for the upper gastrointestinal (UGI) tract. Orientation during endoscopy is challenging and United Kingdom training focusses on technical competence and procedural safety. The reported location of UGI pathologies is crucial to post-endoscopic planning.
To evaluate endoscopists’ ability to spatially orientate themselves within the UGI tract.
A cross sectional descriptive study elicited, using an anonymised survey, the ability of endoscopists to orientate themselves within the UGI tract. The primary outcome was percentage of correct answers from all surveyed; secondary outcomes were percentage of correct answers from experienced vs novice endoscopists. Pearson’s χ2 test was applied to compare groups.
Of 188 respondents, 86 were experienced endoscopists having completed over 1000 endoscopies. 44.4% of respondents correctly identified the anterior stomach and 47.3% correctly identified the posterior of the second part of the duodenum (D2). Experienced endoscopists were significantly more likely than novice to identify the anterior stomach correctly [61.6% vs 31.3%, X2 (1, n = 188) = 11.10, P = 0.001]. There was no significant difference between the two groups in identifying the posterior of D2.
The majority of endoscopists surveyed were unable to identify key landmarks within the UGI tract. Endoscopic orientation appears to improve with experience yet there are some areas still not well recognised. This has potential considerable impact on post-endoscopic management of patients with posterior duodenal ulcers being more likely to perforate and associated with a higher rebleeding risk. We suggest the development of a consensus statement on endoscopic description.
Core Tip: The majority of endoscopists surveyed were unable to identify key landmarks within the UGI tract. Endoscopic orientation appears to improve with experience yet there are some areas still not well recognised. This has potential considerable impact on post-endoscopic management of patients with posterior duodenal ulcers being more likely to perforate and associated with a higher rebleeding risk. We suggest the development of a consensus statement on endoscopic description.
- Citation: Sivananthan A, Kerry G, Darzi A, Patel K, Patel N. Orientation in upper gastrointestinal endoscopy—the only way is up. World J Gastrointest Endosc 2023; 15(3): 146-152
- URL: https://www.wjgnet.com/1948-5190/full/v15/i3/146.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i3.146
Oesophagogastroduodenoscopy (OGD) is the gold standard investigation for the upper gastrointestinal (UGI) tract allowing direct visualisation, tissue sampling and a widening remit of therapeutic curative procedures for early cancers.
Endoscopy’s role in diagnosing UGI cancer continues to advance, with a better understanding of precursor changes such as Barrett’s and atrophic gastropathy and evolving technologies like image enhanced endoscopy and computer aided detection systems. Despite this 11.3% of UGI cancers are missed by OGD[1]. The role of endoscopy in the management of benign UGI conditions has also improved. There are increasing therapeutic options to intervene endoscopically on complex bleeds, or UGI perforations, with patients who historically would have required surgery now often being managed endoscopically.
There are growing numbers of guidelines and statements to help support approaches to surveillance and management of UGI pathology including a standardised approach to photo-documentation of the UGI tract[2-4]. There are numerous widely accepted protocols on UGI surveillance such as the Seattle protocol for assessing Barrett’s and the Sydney protocol for assessing chronic gastritis[5]. These guidelines require accurate identification of the endoscopic anatomy for appropriate sampling and photo- documentation. However, there is no clear consensus nor accepted statement in understanding orientation or reporting locations within the UGI tract.
Orientation within the UGI tract during endoscopy is challenging due to the complex interaction between the flexibility of the scope, the multiple degrees of freedom of the endoscope tip, use of torque and the predominant focus on the (inverted) displayed image.
Training in the United Kingdom focusses predominantly on technical competence and the safety of the procedure. Lesion detection and identification, reporting and management happen experientially during real-time endoscopy and competency is determined by the individual trainer, with no formal evaluation of these skills in place.
The reported location of UGI pathologies such as ulcers directly impacts post-endoscopy investigation and management. Gastric ulcers located on the greater curve are more commonly malignant, whereas benign gastric ulcers occur predominantly on the lesser curve[6]. Ulceration in the first part of the duodenum (D1) is more likely to lead to perforation if the ulcer is located on the anterior wall and although the overall perforation rate in peptic ulcer disease is relatively low most ulcers that do perforate are anterior D1[7].
The gastroduodenal artery is located directly behind the posterior aspect of the duodenum. Ulcers on the posterior duodenal wall are at risk of eroding into this artery which can result in massive bleeding and as such carry a worse prognosis[8]. Posterior duodenal ulcers are also associated with a higher re-bleeding risk[9,10], and the accurate identification of a posterior duodenal ulcer is important to understand the proximity of the gastroduodenal artery and thus the understanding of endoscopic limits and appropriate targets for interventional radiology or surgery if required.
The RCA, PubMed, Cochrane Library and Embase databases were searched until January 10th 2023 to identify relevant research articles. This revealed limited available data on orientation within the UGI tract. One paper was identified from 1992 showing only a 28% accuracy in endoscopists identifying the posterior duodenal bulb[11].
The authors hypothesise that the combination of the focus of training, the complexities of orientation and the lack of a clear consensus guidance have compromised description of orientation and location in the UGI tract.
The aim of this study is to evaluate endoscopists’ ability to spatially orientate themselves within the UGI tract during endoscopy as manifest in their reporting of locations.
A cross sectional descriptive survey study design was used. The study was approved by the Imperial College London institutional review board. A questionnaire was developed by the authors using anonymised endoscopy pictures taken by the author (Sivananthan A) (with consent for publication given by the patients).
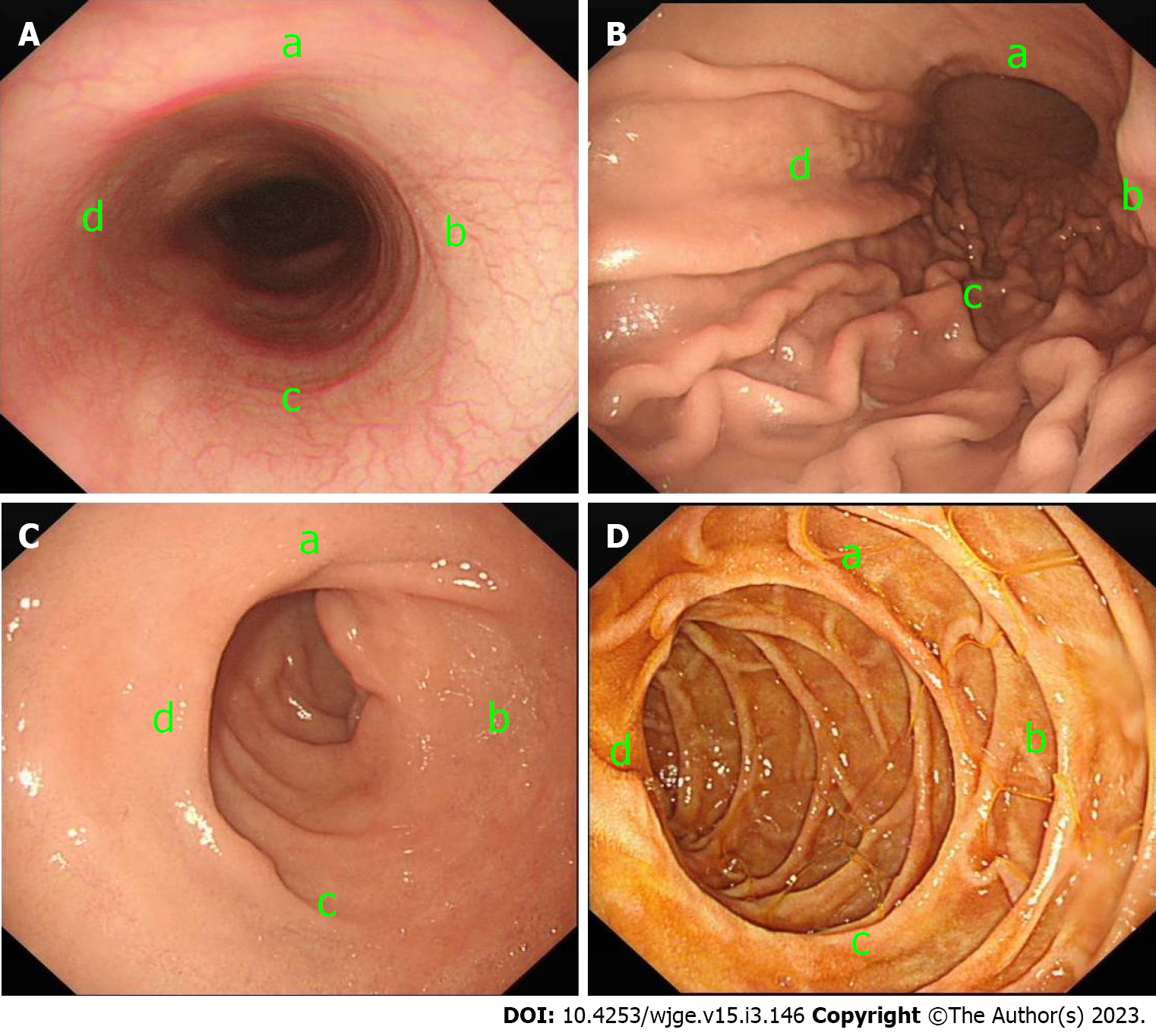
Anonymised endoscopic pictures of the gastro-oesophageal junction, gastric body and the first two parts of the duodenum were used. Images were annotated in each of the four quadrants of the image (Figure 1) to give four options. The patient position (left lateral decubitus) was specified. Orientation of the quadrants in the images and corresponding correct responses were determined in a two-stage process, initially proposed by Sivananthan A/Kerry G and agreed by Patel N/Patel K in the context of the available literature[3-5,12-15]. The questionnaire was developed in QualtricsTM (Provo, UT, United States). Demographics including specialty and endoscopic experience were also collected.
The primary outcome was the percentage of correct answers amongst all surveyed. Secondary outcomes were the percentage of correct answers from experienced vs novice endoscopists.
The survey was distributed through existing national endoscopic research networks including the “digital gastroenterology training network” and opportunistically to endoscopists at the British Society of Gastroenterology Annual Meeting. Inclusion criteria was any experience performing OGDs in adult patients. There were no exclusion criteria. Clinical role of the endoscopists were asked including consultant (equivalent to attendee), registrar (gastroenterology specialist trainee), senior house office (early-stage medical training) and nurse endoscopists (specialist nurses trained to independently perform endoscopy).
Results were collected anonymously using the Qualtrics software and exported to Microsoft Excel for basic statistical analysis. Experienced endoscopists were classified as those who had performed more than 1000 OGDs. Novice endoscopist were classified as those who has completed 1000 or less OGDs. Percentages were used to analyse the discrete data for all subjects. Pearson’s χ2 test was applied to compare the two groups using a p value below 5% to denote significance.
There were 188 respondents to the survey (Table 1). Of these: 74 respondents were consultants, 91 were registrars and 23 were nurse endoscopists. Most were physicians (184) and four were surgeons. There were 163 independent accredited endoscopists and 25 training endoscopists. There were 86 experienced endoscopists having completed more than 1000 endoscopies with 102 novice endoscopists completing 1000 or fewer endoscopies.
| Percentage (number) | |
| Grade | |
| Consultant | 39.4% (74) |
| Registrar | 48.4% (91) |
| Nurse endoscopist | 12.2% (23) |
| Speciality | |
| Medicine | 97.9% (184) |
| Surgery | 21.% (4) |
| Accreditation | |
| Independent | 86.7% (163) |
| Not Independent | 13.3% (25) |
| Experience | |
| Experienced (> 1000) | 45.7% (86) |
| Novice (≤ 1000) | 54.3% (102) |
44.4% of all respondents identified the anterior oesophagus correctly (Table 2). 48.4% of all respondents were able to identify the anterior stomach correctly. 43.1% of all respondents were able to identify the anterior of the first part of the duodenum correctly. 47.3% correctly identified the posterior of the second part of the duodenum.
| All (188) | |
| Anterior oesophagus | 32.4% (61) |
| Anterior stomach | 48.4% (91) |
| Anterior D1 | 43.1% (81) |
| Posterior D2 | 47.3% (89) |
Experienced endoscopists were significantly more likely than novice endoscopists to identify the anterior oesophagus (44.2% vs 22.5%, χ2(1, n = 188) = 9.97, P = 0.002), the anterior stomach than novice endoscopists (61.6% vs 31.3%, χ2(1, n = 188) = 11.10, P = 0.001) and the first part of the duodenum than novice endoscopists (51.2% vs 36.3%, χ2(1, n = 188) = 4.22, P = 0.040) (Table 3).
| Experienced (86) | Novice (102) | P value | |
| Anterior oesophagus | 44.2% (38) | 22.5% (23) | 0.002 |
| Anterior stomach | 61.6% (53) | 31.3% (38) | 0.001 |
| Anterior D1 | 51.2% (44) | 36.3% (37) | 0.040 |
| Posterior D2 | 41.9% (36) | 52% (53) | 0.167 |
There was no significant difference between experienced endoscopists and novice endoscopists in identifying the posterior of the second part of the duodenum (41.9% vs 52.0%, χ2(1, n = 188) = 1.91, P = 0.167).
This study demonstrates that the majority of endoscopists surveyed were unable to accurately identify key landmarks within the UGI tract. This is in keeping with previous work showing the majority of endoscopists being unable to identify the posterior duodenal bulb in 1992.
Although there is no clear evidence that accuracy of orientation and landmark identification during endoscopy has a direct impact on patient outcomes there are logical reasons to think that this would be the case.
Consensus statements on photo-documentation, including those from the British Society of Gastroenterology, European Society of Gastrointestinal Endoscopy, American Gastroenterological Association, American Society of Gastrointestinal Endoscopy and the World Congress of Gastroenterology are reliant on endoscopists correctly identifying key UGI landmarks[2,15]. Based on our findings there is doubt that many respondents are accurately recognising the position of anatomical landmarks and pathology which may have an impact on accurate photo-documenting and thus by inference inspecting all of the anatomical areas suggested.
Accurate anatomical identification of duodenal ulcer location may allow appropriate planning for further management and risk stratification but only a minority of respondents were able to differentiate the anterior and posterior duodenum. Gastrostomy feeding tubes placed endoscopically are accessed via the anterior stomach but the majority of endoscopists were also unable to accurately identify this.
With the increasing role of the multi-disciplinary team, reports are commonly interpreted by non-endoscopists and accurate reporting of lesion location would presumably advantage other specialists when considering management or correlating with radiological findings.
Although there is now wider availability of access to photo-documentation from previous endoscopies, the accurate reporting of the location of lesions may also offer medicolegal support in providing clear evidence that a lesion is new. This is especially relevant in the context of the high reported rate of UGI cancers missed at endoscopy[1].
Experienced endoscopists were significantly more likely to respond correctly in all but the question related to the second part of the duodenum. This suggests that experienced endoscopists more reliably orientate themselves correctly within the UGI tract and posits that understanding of orientation is gained experientially. Although, the correct recognition of posterior D2 by experienced vs novice endoscopists was not statistically significant, which suggests that experience is not the only factor impacting accurate endoscopic orientation.
The focus on the inverted on-screen image may lead to discrepancies in reported locations, often reports are written with lesions documented with respect to their position on a clock face. However, this does not always correlate with the anatomical orientation. For example, left of the screen, when looking at the gastro-oesophageal junction, does not necessarily correlate to the anatomical left of the patient as the orientation of the screen is dependent on both patient position and steering of the endoscope. Orientation based on landmarks provides an objective assessment of location. The inaccuracy of the responses may be due to selecting the responses corresponding to the location on the image itself (i.e., left of the image) rather than based on the anatomical landmarks.
There were limitations to this study including the use of still images which is not akin to real time endoscopic views which may improve orientation. The sample was of British endoscopists and is therefore not generalisable to other countries with different approaches to training and certification.
This study has signalled that orientation within the upper GI tract by endoscopists is generally inaccurate. This study has signalled that orientation within the upper GI tract by endoscopists is generally inaccurate. This may be due to a lack of a consensus statement and confusion between describing orientation on a screen vs anatomical orientation. Endoscopic orientation does appear to improve with experience. Accurate orientation may have beneficial impact on patient outcomes with respect to interventional procedures including rescoping after an UGI bleed and informed arterial embolisation. We suggest the development of a consensus statement on description endoscopically within the GI tract. This would require further controlled research in live endoscopy to allow generalisability to real time endoscopic orientation., but this would require further study with assessment during live endoscopy.
Orientation within the upper gastrointestinal (UGI) tract is challenging due to the flexible nature of the endoscope. There is limited data assessing endoscopist's ability to orient themselves to UGI landmarks.
The ability to accurately identify landmarks is important to allow accurate reporting of UGI lesions and location. Accurate reporting can be important in further therapy and prognostication in UGI bleeds.
To evaluate endoscopists’ ability to spatially orientate themselves within the UGI tract.
A cross sectional descriptive study elicited, using an anonymised survey, the ability of endoscopists to orientate themselves within the UGI tract.
The majority of endoscopists surveyed were unable to identify key landmarks within the UGI tract. Experienced endoscopists were significantly more likely to identify landmarks in the oesophagus, stomach and duodenal bulb than novice endoscopists.
Endoscopic orientation appears to improve with experience yet there are some areas still not well recognised. This has potential considerable impact on post-endoscopic management of patients with posterior duodenal ulcers being more likely to perforate and associated with a higher rebleeding risk.
We suggest the development of a consensus statement on endoscopic description.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Spain; Costache RS, Romania; Ko J, South Korea S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Menon S, Trudgill N. How commonly is upper gastrointestinal cancer missed at endoscopy? Endosc Int Open. 2014;2:E46-E50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 230] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 2. | Beg S, Ragunath K, Wyman A, Banks M, Trudgill N, Pritchard DM, Riley S, Anderson J, Griffiths H, Bhandari P, Kaye P, Veitch A. Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut. 2017;66:1886-1899. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 243] [Cited by in RCA: 224] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 3. | Emura F, Gomez-Esquivel R, Rodriguez-Reyes C, Benias P, Preciado J, Wallace M, Giraldo-Cadavid L. Endoscopic identification of endoluminal esophageal landmarks for radial and longitudinal orientation and lesion location. World J Gastroenterol. 2019;25:498-508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Emura F, Sharma P, Arantes V, Cerisoli C, Parra-Blanco A, Sumiyama K, Araya R, Sobrino S, Chiu P, Matsuda K, Gonzalez R, Fujishiro M, Tajiri H. Principles and practice to facilitate complete photodocumentation of the upper gastrointestinal tract: World Endoscopy Organization position statement. Dig Endosc. 2020;32:168-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (2)] |
| 5. | Banks M, Graham D, Jansen M, Gotoda T, Coda S, di Pietro M, Uedo N, Bhandari P, Pritchard DM, Kuipers EJ, Rodriguez-Justo M, Novelli MR, Ragunath K, Shepherd N, Dinis-Ribeiro M. British Society of Gastroenterology guidelines on the diagnosis and management of patients at risk of gastric adenocarcinoma. Gut. 2019;68:1545-1575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 425] [Cited by in RCA: 409] [Article Influence: 68.2] [Reference Citation Analysis (1)] |
| 6. | Silk AD, Blomquist OA, Schindler R. Ulcer of the greater gastric curvature. J Am Med Assoc. 1953;152:305-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 7. | Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg. 2010;27:161-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 145] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 8. | Hennessy E. Perforated Peptic Ulcer: Mortality and Morbidity in 603 Cases. Aust N Z J Surg. 1972;38:243-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Mille M, Engelhardt T, Stier A. Bleeding Duodenal Ulcer: Strategies in High-Risk Ulcers. Visc Med. 2021;37:52-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Elmunzer BJ, Young SD, Inadomi JM, Schoenfeld P, Laine L. Systematic review of the predictors of recurrent hemorrhage after endoscopic hemostatic therapy for bleeding peptic ulcers. Am J Gastroenterol. 2008;103:2625-32; quiz 2633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 11. | Straker RJ, Bienvenu JC, Nord HJ. Endoscopic orientation within the duodenal bulb. Endoscopy. 1992;24:266-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Salmon PR, Brown P, Htut T, Read AE. Endoscopic examination of the duodenal bulb: clinical evaluation of forward- and side-viewing fibreoptic systems in 200 cases. Gut. 1972;13:170-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Januszewicz W, Kaminski MF. Quality indicators in diagnostic upper gastrointestinal endoscopy. Therap Adv Gastroenterol. 2020;13:1756284820916693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 14. | Canard JM, Létard JC, Lennon AM. Diagnostic upper endoscopy. Gastrointestinal Endoscopy in Practice. 2011;84-100. [DOI] [Full Text] |
| 15. | Lee SH, Park YK, Cho SM, Kang JK, Lee DJ. Technical skills and training of upper gastrointestinal endoscopy for new beginners. World J Gastroenterol. 2015;21:759-785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (11)] |