Published online Feb 16, 2023. doi: 10.4253/wjge.v15.i2.44
Peer-review started: November 16, 2022
First decision: December 11, 2022
Revised: December 23, 2022
Accepted: January 23, 2023
Article in press: January 23, 2023
Published online: February 16, 2023
Processing time: 88 Days and 20.8 Hours
Buried bumper syndrome (BBS) is the situation in which the internal bumper of the gastrostomy tube, due to prolonged compression of the tissues between the external and the internal bumper, migrates from the gastric lumen into the gastric wall or further, into the tract outside the gastric lumen, ending up anywhere between the stomach mucosa and the surface of the skin. This restricts liquid food from entering the stomach, since the internal opening is obstructed by gastric mucosal overgrowth. We performed a comprehensive search of the PubMed li
Core Tip: Buried bumper syndrome is the situation in which the internal bumper of the gastrostomy tube migrates from the gastric lumen into the gastric wall and thus its internal opening is obstructed by gastric mucosal overgrowth. We performed an analysis of the endoscopic techniques described in the literature for releasing the internal bumper to re-establish the functionality of the tube, in an effort to optimize the criteria of choice based on maximum efficacy and safety.
- Citation: Menni A, Tzikos G, Chatziantoniou G, Gionga P, Papavramidis TS, Shrewsbury A, Stavrou G, Kotzampassi K. Buried bumper syndrome: A critical analysis of endoscopic release techniques. World J Gastrointest Endosc 2023; 15(2): 44-55
- URL: https://www.wjgnet.com/1948-5190/full/v15/i2/44.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i2.44
Buried bumper syndrome (BBS) is a rare but serious complication of percutaneous endoscopic gastrostomy (PEG) with one reported incidence of 0.3%-2.4% per PEG-patient per year[1-5], elsewhere raised from 2.0% to 6.7% of PEG placements[6,7]. This complication was first reported for 7 out of 125 PEG placements over a 2-year period in 1988[8], while two years later, in 1990, Klein et al[9] coined the term BBS and successfully treated their cases by pushing the gastrostomy tube into the stomach with a Savary dilator from outside.
The term BBS describes the situation in which the internal bumper of the gastrostomy tube migrates from the gastric lumen into the gastric wall or further, in the tract outside the gastric lumen, ending up anywhere between the stomach mucosa and the surface of the skin. Once the bumper has migrated, the gastrostomy track collapses, with subsequent epithelialization of its inner stoma with gastric mucosa of normal appearance, thus leading either to partial obstruction, leaving a thin fistula towards the stomach lumen, or to complete obstruction[3]. This results in mechanical difficulty or complete failure of feed delivery, rendering the tube useless[10].
BBS is thought to occur because of excessive and prolonged compression of the tissues-stomach plus abdominal wall-sandwiched between the external and internal fixators (bumpers), causing ischemia of the mucosa and subsequent ulceration at the bumper site[5,11], and finally leading to “burying” of the PEG bumper in the gastric wall[12]. A rigid or semi-rigid bumper, such as those made of polyurethane are considered more vulnerable to this pathogenesis[13]-the Sacks-Vine PEG system has been targeted on several occasions, and this is obviously the reason for the high rates of BBS in the bibliography[5,7].
An incompletely buried bumper can usually be easily removed, endoscopically, by using a pair of grasping forceps or a snare from the inside, while simultaneously pushing the tube from the outside. However, the management of a completely buried bumper is more challenging: Several methods have been proposed in case reports of one or two patients or, in some cases, a series of patients, but only some of them have been re-applied by other endoscopists, and none has yet been standardized, as it is likely that different treatment options are better for particular patients[14,15].
In the present analysis, we review all the published endoscopic techniques used over a 30-year period to release the buried internal bumper to re-establish the gastrostomy tube’s functionality (Figure 1).
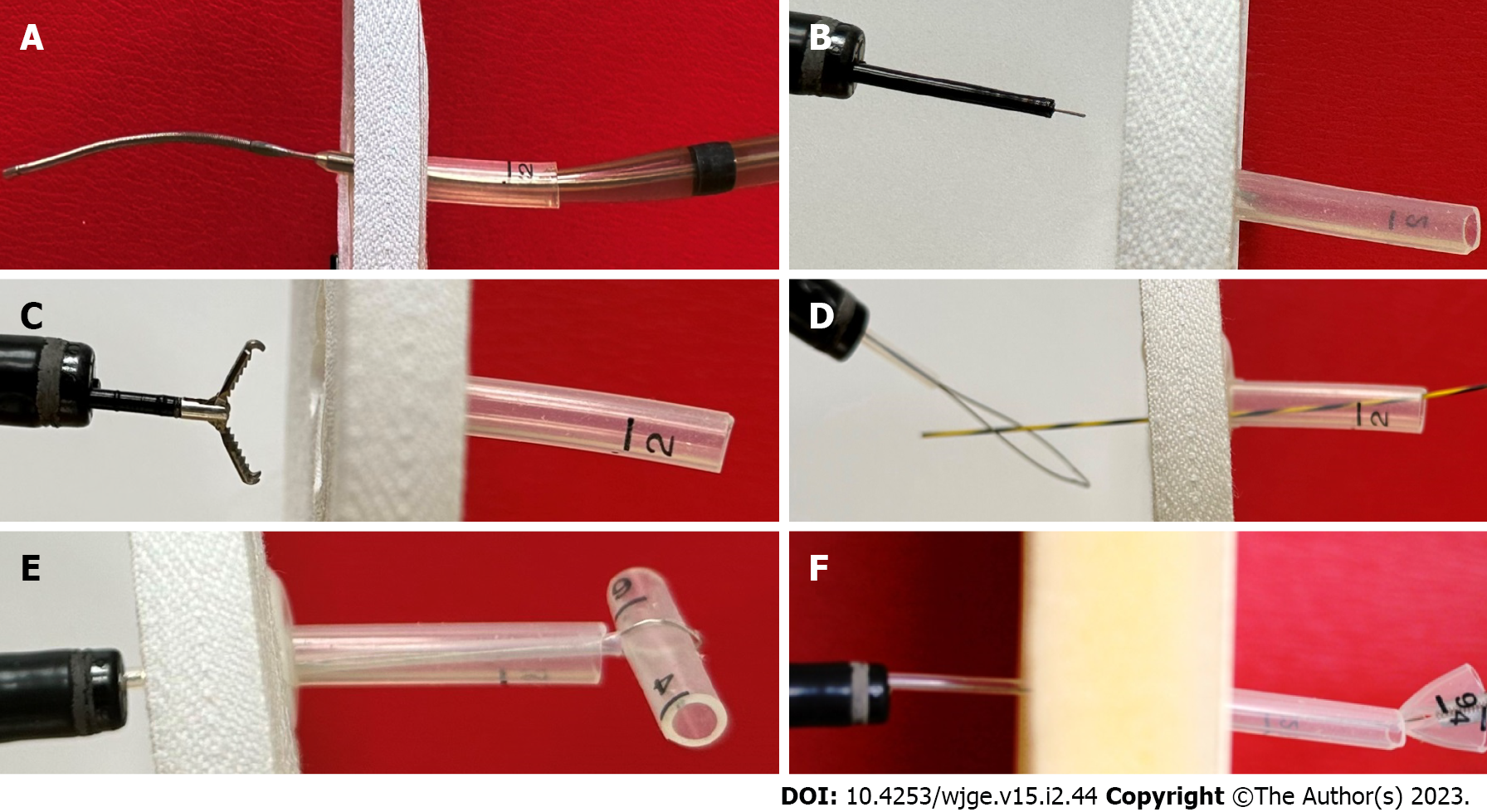
Klein et al[9] were the first to coin the term “buried bumper” syndrome, and the first to describe a simple technique to dislodge the buried bumper from the gastric mucosa. Fortunately for their cases, the continuity of the tube was still not totally obstructed, although the internal bumper was completely covered by the gastric epithelium; thus, passing a guidewire from the outside into the gastrostomy tube which has been cut short previously was the first step. A Savary dilator was then loaded over the guidewire and force was applied perpendicular to the abdominal wall, leading to the release of the internal bumper within the stomach lumen (Figure 2A).
The same technique was also described three years later by Gumaste et al[16], the only difference being that no guidewire was used. They simply shortened the tube externally and introduced a 36F Savary dilator into it, from the outside. The pressure was then applied to successfully dislodge the bumper from the mucosa and release it into the gastric lumen.
Similarly, Binnebösel et al[17], after cutting the external tube to a length of 5 cm, carefully inserted it into the gastric lumen, under endoscopic guidance, a 27-cm long, stainless steel probe with a diameter of 3 mm and a 3 cm tip with a narrowed diameter (2 mm). Slight pressure and gentle manipulation of the PEG tube enabled the bumper to be easily luxated, through the mucosa, into the gastric lumen. A standard polypectomy snare was then passed through the gastroscope to grasp the PEG tube distally to the bumper. Following removal of the probe, the PEG tube was then able to be removed through the mouth along with the gastroscope.
A few years after the first technique description, Ma et al[1] used a needle-knife papillotome to safely release the inner bumper. Unlike the previous technique, “violently” tearing away of the mucosa which had grown, was avoided. Using this pre-cut device, radical incisions into the gastric mucosa, from the center of the dome outwards, were made; the precise direction of the cuts was determined by external manipulation of the tube, to better expose the inner bumper under the mucosa. Final removal was then facilitated by grasping and pulling the bumper towards the gastric lumen with alligator forceps or a snare (Figure 2B and C).
Ma et al[1] applied their technique to a total of 9 BBS cases, in which the buried bumper was from a MIC-type gastrostomy tube.
Frascio et al[18], using the needle-knife technique proposed by Ma et al[1], failed to expose the internal bumper to remove a Sacks-Vine gastrostomy, performed 7 years previously. Then, subsequently, under local anesthesia, with a guidewire in place, two small cutaneous incisions were made, one on each side of the external part of the PEG tube, down to the bumper. The tube and bumper were then removed along the guidewire, without any opening of the peritoneum.
In the same manner, as Ma et al[1], El et al[2] initially inserted a flexible straight Teflon guidewire under endoscopic control from outside, and clamped the PEG tube over the wire, to allow adequate air insufflation of the stomach. Using the guidewire as the central point, cruciform incisions were made on the mucosal “dome” covering the internal bumper by using a needle-knife sphincterotome or an electrosurgical knife. During incisions, the PEG tube was gently pushed internally to allow stretching of the covering mucosa. When the bumper was completely revealed, rat-tooth forceps or a snare-through the gastroscope-was used to withdraw the PEG tube.
This technique was applied in 8 cases.
Boyd et al[19] presented the “push-pull T” technique, citing the advantage of requiring only materials normally readily available in every endoscopic suite. The external part of the gastrostomy tube was first cut short, 3 cm above the skin. An endoscopy was performed, and a polypectomy snare was advanced toward the lumen of the buried bumper to exit via the tube. If the internal lumen opening was covered, a 0.035 soft-tipped guidewire was pushed from the outside and upon entry to the gastric lumen, it was grasped with the snare loaded to the gastroscope. The external end of the guidewire was then pulled manually, dragging out the snare through the gastrostomy tube. When outside, a 2-cm piece of the gastrostomy tube was inserted into the snare loop and securely grasped. The snare was pulled back from inside the gastroscope, to bring the short piece of the tube tight against the end of the external part of the gastrostomy, creating a “T” effect-hence the name of the method. A pair of Kelly clamps were used to secure the T-piece in place, tight against the residual PEG tube. The endoscope, snare, and attached T-piece were then slowly drawn back by the endoscopist, while an assistant pushed the Kelly forceps and the gastrostomy tube into the gastric lumen from outside. Once within the stomach, the Kelly forceps were released and the gastrostomy tube plus the T-piece was removed, along with the gastroscope (Figure 2D-F).
Horbach et al[20] completed this technique by proposing the following: first the use of a Hegar dilator inserted through the external part of the PEG tube to make it protrude into the gastric lumen. If it did not easily protrude, they incised the mucosa radially down to the central dome of the bumper either with a needle papillotome or the tip of a polypectomy snare. Once the gastric opening of the bumper became apparent, a snare was led through it and pushed to the external end of the tube, as previously. However, Horbach et al[20] proposed a 5-cm cut-off piece of the tube, instead of 2 cm, to be grasped by the snare; thus, by pulling the snare back into the stomach it formed an arrow shape, which more easily freed the bumper from the gastric mucosa towards the gastric lumen.
This technique was applied in 18 BBS patients-however, depending on the difficulty of each case, the buried bumper needed up to 5 sessions to be totally revealed.
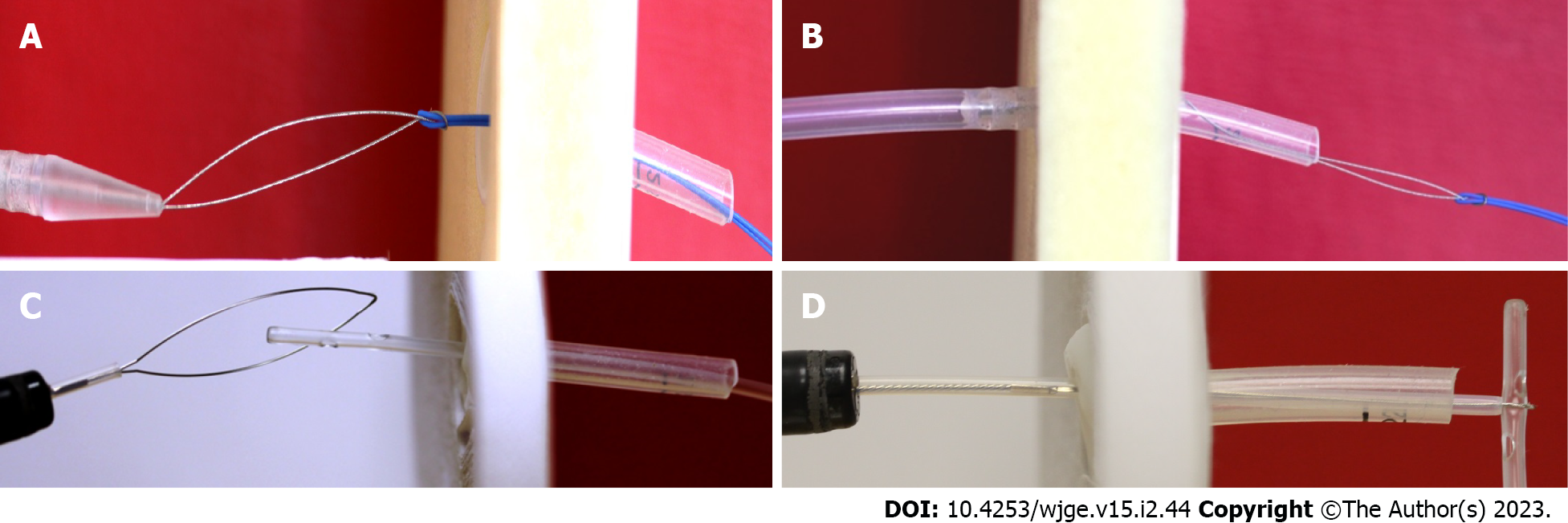
Venu et al[3] described by far the easiest technique for the removal of a gastrostomy with a buried internal bumper. The external part of the gastrostomy tube was cut 3 cm to 4 cm above the skin level. The long needle of a new PEG kit was inserted through the shortened tube stump under endoscopic control and advanced through the buried bumper to protrude into the gastric lumen, exactly as when a new gastrostomy is performed. Once in the lumen, the thread of the PEG kit was advanced through the needle and grasped with a snare introduced through the biopsy channel of the endoscope; the thread, along with the endoscope, was brought out/retrieved through the mouth. The thread was then looped onto the new PEG tube and pulled back through the mouth towards the stomach, by simply gentle traction from its external edge. The sense of slight resistance indicated engagement of the tapered tip of the new PEG tube in the lumen of the buried bumper. The stump of the old tube was then straightened sufficiently to facilitate traction and the stump tube with the buried bumper, followed by the new PEG tube, finally emerged through the abdominal wall. The old PEG was removed and the new one stabilized in the standard fashion (Figure 3A and B).
Similarly, Monib et al[21] used a guidewire passed from outside into the gastric lumen, instead of the needle and thread, to attach it to the distal end of a new PEG tube and continued the procedure as previously described. In order to facilitate the passage of the guidewire towards the gastric cavity they used a simple trick for the identification of the dimple corresponding to the center of the internal bumper: The water jet technique. This technique, initially proposed by Vu[22], involves flushing normal saline into the PEG tube from the outside and looking carefully from the inside-endoscopically. Despite some resistance, a small amount of fluid was finally observed trickling from the dimple.
Leung et al[11] proposed a new technique with two alternative options. Initially, the external part of the gastrostomy tube was shortened to about 5 cm to 7 cm and a ureteric catheter was passed through up to the gastric lumen, identified under endoscopic vision; after which the external part of the gastrostomy tube was securely tied over the ureteric catheter. A polypectomy snare, brought down through the endoscope, was used to grasp the intragastric part of the ureteric catheter. Traction was then applied to the snare, leading to the inversion of the tube and thus dislodging the buried bumper (Figure 3C and D).
Alternatively, the ureteric catheter was not tied to the gastrostomy tube. A polypectomy snare, advanced through the endoscope, was used to grasp the ureteric catheter; simple traction of the catheter from the outside guided the snare out through the shortened gastrostomy tube. The snare was then closed around the tip of the tube and traction applied to, as previously, to pull the gastrostomy tube into the stomach.
This technique was then a slightly modified by Turner et al[23], who replaced the urinary catheters, inserted from outside, with stent-grasping forceps in order to grasp the polypectomy snare advanced through the gastroscope-and bring it out through the short gastrostomy tube. A pair of scissors was used to cut the gastrostomy tube further as closely as possible to the skin surface; the snare then being pushed as far as possible down the tube to enfold the tube. By this method, after traction was applied to the snare, the PEG tube stump was not inverted, as previously, but became “concertinered” and popped through the mucosa.
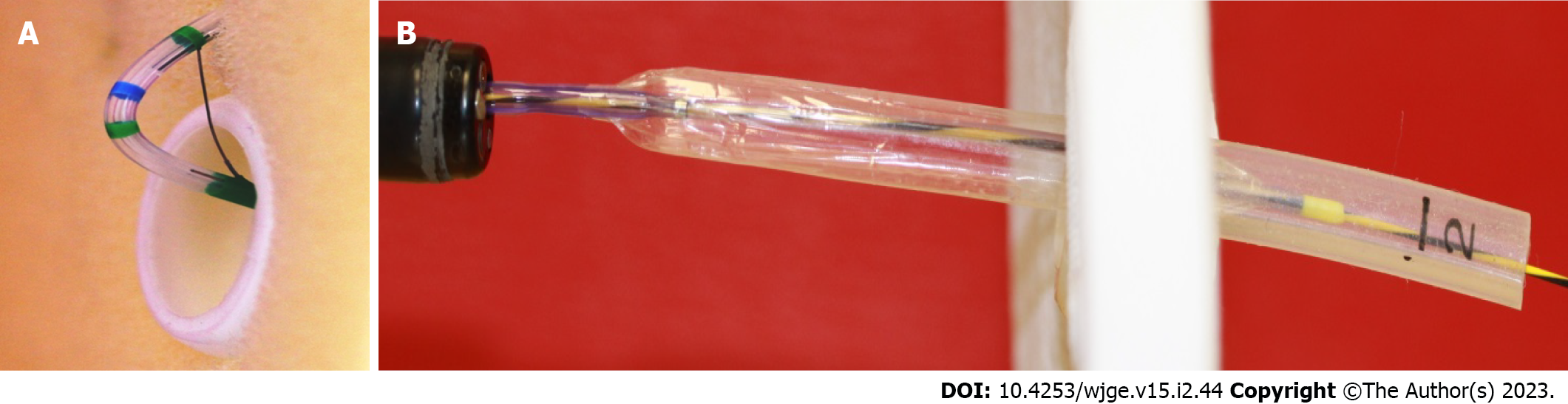
In eight patients Müller-Gerbes et al[24] developed and evaluated another endoscopic technique for buried bumper release. A standard papillotome was inserted from the outside through the shortened PEG tube and over a guidewire into the stomach, under endoscopic control. Then the papillotome was bent and drawn back until its cutting wire was over the mucosa covering the internal bumper. Radical cutting was performed in at least 3 directions, by externally rotating the device over the bumper. After the sufficient release of the bumper, the papillotome was removed and a dilator was inserted in order to push the bumper from outside towards the gastric lumen; from which it was removed as a foreign body (Figure 4A).
Eight years later Müller-Gerbes et al[10], in a comparative study reported their experience in 82 cases, the largest series so far, 35 of which (42.7%) were successfully treated with a wire-guided papillotome.
Cyrany et al[4] modified the technique proposed by Müller-Gerbes et al[24] and applied it to 22 buried bumper cases. After a guidewire was inserted from outside, the overgrowing tissue covering the internal bumper was dissected by a needle-knife papillotome and argon plasma coagulator instead of a standard papillotome; after which, a dilator was passed over the guidewire into the gastrostomy tube to stiffen it and the tube was pushed into the stomach. Finally, the bumper was retrieved with a snare.
Alternatively, in some cases, a cannulotome was inserted into the stomach over the guidewire from outside, through the shortened PEG tube, under endoscopic supervision. The cannulotome was then bent and pulled slightly from the outside, the cutting wire dissecting the overgrowing tissue covering the bumper. Attention was given to the cutting direction: from the center of the buried bumper along the long axis of the tube, the length of the cuts not exceeding the radius of the bumper-three to five cuts usually being sufficient. Additionally, to avoid air leakage around the cannulotome inserted through the PEG tube, the use of a modified part of a dilator was proposed.
The same technique as that of Müller-Gerbes et al[24], slightly modified, was described again in 2014 by Born et al[25], who inserted a conventional Erlangen papillotome, instead of a standard one, over the guidewire into the stomach, and made incisions in all four directions. Then, a 10Fr bougie was advanced from the outside into the tube for stabilization, and all pushed into the stomach.
Based on the Müller-Gerbes et al[24] technique, an endoscopic set, the Flamingo set (Medwork, Höchstadt, Germany), exclusively for radial incision of the granulomatous tissue over a buried bumper, was designed. This set contains the Flamingo device, a papillotomy-like catheter having a U-shape configuration at its end-the cutting wire being 30 cm in length for easy manipulation, a 35-gauge guidewire, and forceps for foreign body removal.
Hindryckx et al[26] were the first to use this commercially available Flamingo set, in 5 cases. The Flamingo device was introduced from the outside, through the shortened PEG tube, into the gastric lumen over a pre-inserted guidewire; it was then flexed by 180 degrees, into an inverted “U”-like the neck of a flamingo bird-to expose the bow-string, sphincterotome-like, cutting wire. Using an ele
At the same time, Costa et al[27] presented a video case, while two years later Costa et al[28] reported a multicenter study comprising 53 cases.
Curcio et al[29] applied the endoscopic technique of endoscopic submucosal dissection (ESD) to un-roof the gastrostomy tube internal bumper. A guidewire was initially inserted through the PEG tube from the outside into the gastric lumen. An 8F feeding tube was then inserted over the guidewire to be used at the central point of the mucosal area to be dissected. Progressive radial endoscopic submucosal dissection was then performed using a water-jet Hybrid-knife T-Type (ERBE, Tübingen, Germany), until the whole bumper was exposed and the endoscopist was able to safely capture it first with rat-tooth forceps and then with a polypectomy snare, for removal through the mouth.
Wolpert et al[30] described a new endoscopic technique in which they mainly replaced the cutting of the overlying bumper mucosa using a Hook knife instead of a needle knife. This is a rotating L-shaped cutting wire designed for hooking tissue and pulling it away from the gastric wall, towards the lumen. They initially used a 15 mm through-the-scope dilation balloon passed externally via the PEG tubing and inflated to dilate the mucosal orifice. A Hook knife was deployed through the gastroscope to incise the gastric mucosa over the buried bumper by hooking the tissue, pulling it towards the lumen and then cutting it using diathermy under direct vision. The balloon dilator was then inflated again into the PEG tube to stiffen it; both the tube and the balloon catheter were clamped together and pushed toward the gastric lumen to force the bumper to exit into the stomach. The PEG was then removed as a foreign body.
Lazaridis et al[12] proposed the use of a 2.5-mm ball-tip, needle-type irrigation knife to dissect the overgrowing gastric mucosa, in order to insert biopsy forceps through the external opening of the PEG tube. This manipulation opened the track for insertion of the sphincterotome over a guidewire, as previously described. After the cuttings were performed, a 6-mm endoscopic balloon dilator was passed through the endoscope, and not from the outside, as proposed by Wolpert et al[30], fully inflated into the PEG tube, and traction was applied-as opposed to previously described pushing from outside into the stomach.
Nakamura et al[31] described buried bumper removal by means of a needle knife for mucosal incision and then an insulation-tipped diathermic knife for submucosal dissection of the bumper-covering mucosa. Upon free movement of the bumper, it was transabdominally removed through the fistula towards the gastric lumen and then through the mouth, along with the gastroscope.
Strock and Weber[32] used a method whereby a guidewire was inserted into the stomach through the lumen of the gastrostomy tube cut to 3 cm. An esophageal balloon dilator was then advanced through the endoscope into the stomach and manipulated into the gastrostomy lumen to meet the guidewire for insertion. Once insertion was achieved, the balloon was fully inflated so that it remained impacted in the tube. Traction of the balloon and the endoscope allowed the extraction of the bumper first and then, more easily, of the remaining gastrostomy catheter into the stomach. Afterward, the PEG catheter was removed from the stomach as a foreign body (Figure 4B).
The same technique was also successfully applied and then published as “a single step” maneuver by Christiaens et al[33], nine years later.
In the pick of “experimentation” with the innovative, most proposed endoscopic modality of surgery through natural orifices, Marks JM and the pioneer in percutaneous endoscopic gastrostomy, Marks et al[34] published a case of the successful rescue of a PEG tube in a neurological severely ill patient whose gastrostomy was inadvertently dislodged 3 d after PEG placement. A Folley catheter inserted immediately to maintain the tract failed to be inserted into the stomach. Thus, under conscious sedation only, with the patient in the intensive care unit, an intragastric abdominal exploration was performed: A standard gastroscope was inserted into the stomach and advanced through the previous gastric opening where the PEG tube had passed into the abdominal cavity. A guidewire was inserted into the peritoneal cavity through the external PEG site, grasped using a snare advanced through the endoscope, and brought back into the stomach and out through the mouth. A standard pull-technique PEG was then successfully inserted.
Six years later, Nennstiel et al[35], in an effort to treat a BBS in a 52-year-old tetraplegic patient, started by using a needle knife papillotome to reveal the PEG lumen; then, in an effort to push the tube from outside into the stomach with a bougie, the gastrostomy was, accidentally, totally dislodged from the gastric wall and fell into the peritoneal cavity. A pediatric gastroscope was then inserted into the stomach and advanced into the peritoneal cavity through the gastric opening in the anterior gastric wall. The PEG tube was grasped and brought back into the stomach and out through the mouth, while a new PEG was advanced through a guidewire inserted from outside into the peritoneal cavity, grasped with biopsy forceps and transferred, similarly, through the stomach out, through the mouth.
In recent years, the NOTES procedures are no longer used in daily practice. These techniques must therefore be kept only as an innovative idea from the past.
The effectiveness of the techniques we have described practically cannot be evaluated, since they comprised improvisation by physicians in order to rescue the embedded internal bumper, in one or more cases, which were then published as a report of a case or a series. The procedure was never or rarely repeated exactly as described and never published again. Usually, with a particular technique as a basis, modifications/variations are applied, either because the endoscopist thinks these changes to be more effective, or because the specific instrument/s are not available, or, finally, because new, modern apparatus is available. The only exception was that of Furlano et al[36], who reported their difficulties in recovering a Freka-PEG-which has a hard, thin disk beneath which is an internal tubular crosspiece, also of hard plastic, not removable with traction from the outside- in a 2.5 year-old boy. They first, in
Overall, it is not fair to compare the techniques with each other for effectiveness-each technique proved to be effective, as long as it had the desired end result for the patient, without apparent complication. The only exception is a comparative study by Müller-Gerbes et al[10]. In a cohort of 82 BBS cases, the largest series published, they compared 35 (42.7%) patients treated with a wire-guided papillotome with 22 (26.8%) treated with a needle-knife, in terms of bleeding. No bleeding was recorded after using the standard papillotome, but bleeding occurred in 7 patients (31.8%) after cutting with a needle-knife papillotome (P < 0.05). Furthermore, ten of the 22 patients (45.5%) treated with the needle knife experienced a serious adverse event and 1 patient finally died (4.5%).
Finally, we have to add a recent, retrospective study derived from 15 Gastroenterology Departments and comprising 53 BBS cases, for whom the commercially available Flamingo device, first tested by Hindryckx et al[26], was used for completely covered internal bumpers[28]. They reported a success rate of 96.4% (53 out of 55 procedures), but also a 12.7% rate (7 cases) of adverse events, all endoscopically managed. Adverse events were: Significant bleeding in 4 patients (7.3%), a small perforation in 2 patients (3.6%), a superficial laceration of the gastroesophageal junction during PEG extraction in 1 patient (1.8%), and sepsis within 48 h from the buried bumper removal, in 2 patients (3.4%).
Mention should also be made of the disadvantages and complications from the application of these techniques, either as reported by the authors themselves, or as assumed in the comments of other authors, usually to support their own point of view and/or to promote their own modified technique as being more effective or safe (Table 1).
| No. | Technique | Cases1 | Advantages | Disadvantages |
| 1 | The “push”[16,17] | Need of readily available endoscopic instruments | Applied to gastrostomy tubes removable only through the mouth | |
| 2 | The “needle-knife”[1,2,18] | 17 | Easier to use through the endoscope, a common instrument | Applied to gastrostomy tubes removable only through the mouth; risk of bleeding/perforation |
| 3 | The “push-pull T”[19,20] | 18 | Need of readily available endoscopic instruments | Applied to gastrostomy tubes removable only through the mouth; need of multiple sessions, traumatic |
| 4 | The “new PEG against the old”[3,21,22] | Simple to be applied | Applied only in gastrostomy tubes able to be removed by traction | |
| 5 | The “snare”[11,23] | Need of readily available endoscopic instruments | Applied to gastrostomy tubes removable only through the mouth | |
| 6 | The “papillotome”[4,24,25] | 112 | The largest series published[24] | Applied to gastrostomy tubes removable only through the mouth; too long/not easily manipulated, lack of rigidity; difficult in handling endoscopic instruments out of the endoscope |
| 7 | The “Flamingo”[26] | 58 | Commercially available | Applied to gastrostomy tubes removable only through the mouth; bleeding/laceration/sepsis; Cost??? |
| 8 | The “ESD devices”[12,29-31] | Easy to handle in experienced hands | Applied to gastrostomy tubes removable only through the mouth; not standard equipment; need of experience in ESD; Cost??? | |
| 9 | The “balloon dilator”[32,33] | Instruments readily available in an endoscopic suite | Applied to gastrostomy tubes removable only through the mouth | |
| 10 | The “NOTES”[34,35] | 2 | Peritoneoscopy through a natural orifice (mouth) | Applied to gastrostomy tubes removable only through the mouth; no longer in clinical practice |
The cutting devices, such as the needle-knife papillotome, came into use as early as 1995 by Ma et al[1], are easier to use than cutting devices inserted from the outside, since they are applied through the endoscope, from the gastric lumen side[2,4], but carry the risk of an unpredictable bleed or perforation of the gastric wall. According to Hindrycks et al[26] the needle knife may fail to un-roof the buried bumper, because of a too-deep ingrowth of the bumper, as occurred in one of their cases. On the other hand, it is a common instrument in every endoscopic suite and can be easily handled by any endoscopist who is able to perform a sphincterotomy.
The standard papillotome, as the instrument proposed initially by Müller-Gerbes et al[24] to cut the mucosal tissue covering the internal bumper, is not designed for this procedure and hence, has less curving potential and less ability to rotate in order to make incisions in a stellate fashion. Moreover, a papillotome, like every other endoscopic apparatus, has a working length of about 200 mm, enough to pass and exit from an endoscope; it is thus too long to be easily manipulated out of the endoscope, as occurs when inserted from the skin side through the lumen of the gastrostomy tube into the stomach. Another disadvantage is the lack of rigidity throughout the 200 mm body, since it is designed to pass through, and therefore be supported by, the working channel of the gastroscope. It may, however, gain when inserted over a guidewire. Despite these difficulties, Müller-Gerbes et al[10] published their experience in 82 BBS cases, 35 of which (42.7%) were successfully treated with a wire-guided papillotome. The same applies to the conventional Erlangen papillotome used, over the guidewire, by Born et al[25] in an effort to modify the Müller-Gerbes technique.
The newest technological devices, such as the ERBE Hybrid-knife and the Olympus Dual-knife, Hook-knife, and insulation-tipped diathermic knife, designed for ESD procedures, are, of course, much safer and easier to handle[12,29,31]; however, these instruments are not among the standard equipment readily available in every endoscopy unit. Additionally, Hindryckx et al[26], reporting the use of the Hybrid-knife and Dual-knife in two BBS cases, revealed that the procedure took more than one hour to successfully complete. Perhaps the rotatable, L-shape Hook-knife may be safer, or simply give a sense of safety, since it is designed for hooking the tissue and pulling it away from the gastric wall towards the lumen and then cutting it using diathermy under direct vision, thus reducing the risk of inadvertent gastric perforation, as may occur when cutting towards the gastric wall[30].
The buried bumper syndrome is mainly attributed to excessive tissue compression-close around the site of tube passage-between the inner and outer bumpers of the gastrostomy. This prolonged pressure causes progressive tissue ischemia and subsequent gastric mucosal ulceration, leading to the lodging of the inner bumper in the gastric mucosa and further on into the gastric or even the abdominal wall tissues. In parallel, the mucosal healing process causes gastric mucosa to grow over the embedded inner bumper to cover the gap, leading to the progressive loss of its viability with regard to feeding delivery. Another mechanism proposed to be involved in the impaction of the internal bumper into the gastric mucosa is the traction of the tube toward the outside by the confused patient or accidentally by the caregiver, with a force insufficient to dislodge the gastrostomy tube totally from the abdominal wall, but to move it outwards sufficiently for it to be impacted somewhere between the mucosa and beneath the skin[13,23,37].
Although nothing can be proven without a double-blind observational study, the first argument is supported by the report of El et al[2], who found a very low incidence (0.9%) of BBS in a total of 879 patients subjected to PEG. They consider the main reason for this low complication rate in their patients to be the existence of a Nutrition Team supporting in- and out-patients, taking special care to “push, pull and rotate the PEG tube frequently in the early post-insertion period”, as the best way to prevent BBS. They additionally took great care to check against the placement of gauze pads underneath the external bumper[15], since this practice carries the risk of slightly pulling the gastrostomy outward, the second scenario of the etiology of BBS is also verified.
In addition to the above, the incidence of BBS appears to be directly related to both the material of the bumper and its design. As early as 1995, both Ma et al[1] and Boyd et al[19] commented that among the published cases of buried bumper syndrome, most occurred among those having the Sacks-Vine feeding tube[8,38]; the propensity of this particular product to “migrate” into the gastric wall being attributed to both the composition and design of the inner bumper[9]. It was constructed from Tecoflex, a hard, medical grade, polyurethane and had a narrow, 2.4 cm long T-piece-design of internal bumper, beneath which lay an internal tubular crosspiece of hard plastic. Both this gastrostomy tube as well as the newest of similar design, were not removable by traction from the outside-all having a hard, thin, circular disk or triangle shaped internal bumper, which was totally inflexible. The design of such internal bumpers involves only a small surface area being in direct contact with the gastric mucosa, which may predispose it to increased local tissue pressure and necrosis, and thus the risk of impaction into the gastric mucosa[5,6,19].
In reinforcement of the above, the incidence of BBS seems to have decreased nowadays. Although the reported incidence of this complication is poorly assessed, coming only from series (larger or smaller) of patients from the same centre, there is a feeling that this frequency has decreased with the passing of the years. This can be attributed to the more sophisticated design of the tubes, and especially of the internal bumper, and of the more tissue-friendly materials, although there are still centres that traditionally stick to the use of gastrostomy catheters requiring endoscopy for their removal; and such catheters are generally harder and more rigid[39].
Whatever the mechanism by which the internal bumper gets buried, the material used, the internal bumper design and the degree of bumper impaction into the gastric wall, every endoscopist should be able to diagnose and treat this condition. The instrumental manipulation for recovering the bumper must be a safe procedure, for both the patient, being per se extremely fragile, as well as for the operator-endoscopist. And such a person cannot be someone who simply knows how to perform a gastrostomy, although, generally speaking, no one has a reasonable degree of experience in dealing with such cases because of their infrequency-0.25% of PEG patients per year-even in reference centres[20]. The use of the needle-knife might lead to complications, mainly gastric perforation, which is a much more serious event in comparison to leaving a gastrostomy buried and inactive[40]. On the other hand, the familiarity of some endoscopists with modern, complex invasive techniques, such as POEM, makes them extremely capable of removing a buried bumper-much more easily than a gastric tumor; so they no longer consider it necessary to publish it as yet another case report.
Coming now to the different techniques previously presented, it is true that in general, we cannot advise which method is the most appropriate, since its success depends on the very specific circumstances of each case, the first criterion being the type of PEG, with respect to the method of removal. When a gastrostomy can be removed by simple traction from outside, the only difficulty is the pushing of the guidewire from outside into the gastric lumen; where upon a new gastrostomy can be passed, either as a replacement tube from outside over the guidewire or as a new one pulled from the mouth. On the other hand, the necessity for endoscopy to remove any apparatus by mouth is what presents the greatest difficulty and which has led to the development of so many alternative techniques. Furthermore, it must be kept in mind that this type of tube is generally made from less flexible material, making the deep impaction of the bumper into the gastric tissue more likely.
The endoscopist should know in advance the exact type of the gastrostomy tube he has to deal with, since the internal bumper configuration will be of importance for the final decision as to the optimal removal strategy. This is why Braden et al[15] used endoscopic ultrasound to successfully localize the internal bumper in 11 patients. Unfortunately, the publications from which the techniques were retrieved are essentially reports of a single case or small case series. And most importantly, the majority of them do not mention the type of gastrostomy involved; only opportunely in some can we make deductions from the photos they provide. It is clearly one thing to try to uncover a dome-shape gastrostomy and quite another to have a Freka-type or formerly Sachs-Vine hard collar which cannot be pulled out.
Finally, the endoscopist should keep in mind that, when the removal of a gastrostomy needs endoscopy, the bumper must be almost completely exposed, and an invasive endoscopy takes time and is definitely burdensome for the patient, if we also take into account the general physical condition, age and underlying diseases; which is why there is always the option to “cut and leave alone”[40].
In conclusion, carefully performed and technically perfect gastrostomies, using high quality materials, in conjunction with post-operative care to avoid excessive pressure of tissues between bumpers will minimize the incidence of BBS. When the BBS case occurs, the ideal procedure has not yet been discovered; thus, the least invasive technique must be applied to solve the problem and subject the already severely ill patient to the least burden possible. In all cases, the success rate, procedure time, and, why not, the cost-effectiveness of the technique to be used should be assessed by the endoscopist in advance.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Altonbary AY, Egypt; Sun Z, China S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Ma MM, Semlacher EA, Fedorak RN, Lalor EA, Duerksen DR, Sherbaniuk RW, Chalpelsky CE, Sadowski DC. The buried gastrostomy bumper syndrome: prevention and endoscopic approaches to removal. Gastrointest Endosc. 1995;41:505-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 56] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | El AZ, Arvanitakis M, Ballarin A, Devière J, Le Moine O, Van Gossum A. Buried bumper syndrome: low incidence and safe endoscopic management. Acta Gastroenterol Belg. 2011;74:312-316. [PubMed] |
| 3. | Venu RP, Brown RD, Pastika BJ, Erikson LW Jr. The buried bumper syndrome: a simple management approach in two patients. Gastrointest Endosc. 2002;56:582-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 4. | Cyrany J, Repak R, Douda T, Fejfar T, Rejchrt S. Cannulotome introduced via a percutaneous endoscopic gastrostomy (PEG) tube--new technique for release of a buried bumper. Endoscopy. 2012;44 Suppl 2:E422-E423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Foutch PG, Woods CA, Talbert GA, Sanowski RA. A critical analysis of the Sacks-Vine gastrostomy tube: a review of 120 consecutive procedures. Am J Gastroenterol. 1988;83:812-815. [PubMed] |
| 6. | Hodges EG, Morano JU, Nowicki MJ. The buried bumper syndrome complicating percutaneous endoscopic gastrostomy in children. J Pediatr Gastroenterol Nutr. 2001;33:326-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Cahill AM, Baskin KM, Kaye RD, Fitz CR, Towbin RB. Transmural migration of gastrostomy tube retention discs. Pediatr Radiol. 2004;34:143-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Gluck MLJ, Drennan F. Retraction of Sacks-Vine gastrostomy tubes into the gastric wall: report of seven cases. Gastrointest Endosc. 1988;34:215. |
| 9. | Klein S, Heare BR, Soloway RD. The "buried bumper syndrome": a complication of percutaneous endoscopic gastrostomy. Am J Gastroenterol. 1990;85:448-451. [PubMed] |
| 10. | Mueller-Gerbes D, Hartmann B, Lima JP, de Lemos Bonotto M, Merbach C, Dormann A, Jakobs R. Comparison of removal techniques in the management of buried bumper syndrome: a retrospective cohort study of 82 patients. Endosc Int Open. 2017;5:E603-E607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 11. | Leung E, Chung L, Hamouda A, Nassar AH. A new endoscopic technique for the buried bumper syndrome. Surg Endosc. 2007;21:1671-1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Lazaridis N, Murino A, Telese A, Koukias N, Despott EJ. A multimodality endoscopic approach for the management of buried bumper syndrome. Endoscopy. 2019;51:E410-E411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol. 2014;20:8505-8524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 325] [Cited by in RCA: 269] [Article Influence: 24.5] [Reference Citation Analysis (10)] |
| 14. | Fujita K, Ozaki M, Obata D, Yoshida M, Kanamitsu K, Nakamura T, Azuma T. Simple and safe replacement technique for a buried percutaneous endoscopic gastrostomy tube using a laparoscopic surgery device. Surg Laparosc Endosc Percutan Tech. 2012;22:546-7; author reply 548. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 15. | Braden B, Brandstaetter M, Caspary WF, Seifert H. Buried bumper syndrome: treatment guided by catheter probe US. Gastrointest Endosc. 2003;57:747-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Gumaste VV, Krachman M, Pottipati A, Dave P. Removal of an embedded PEG bumper. Gastrointest Endosc. 1993;39:598-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Binnebösel M, Klink CD, Otto J, Schumpelick V, Truong S. A safe and simple method for removal and replacement of a percutaneous endoscopic gastrostomy tube after "buried bumper syndrome". Endoscopy. 2010;42 Suppl 2:E17-E18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Frascio F, Giacosa A, Piero P, Sukkar SG, Pugliese V, Munizzi F. Another approach to the buried bumper syndrome. Gastrointest Endosc. 1996;43:263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Boyd JW, DeLegge MH, Shamburek RD, Kirby DF. The buried bumper syndrome: a new technique for safe, endoscopic PEG removal. Gastrointest Endosc. 1995;41:508-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Horbach T, Teske V, Hohenberger W, Siassi M. Endoscopic therapy of the buried bumper syndrome: a clinical algorithm. Surg Endosc. 2007;21:1359-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Monib S, Ritchie A, Hamad A, Elbeshlawy M. Buried Bumper Syndrome: A New Technique of Management. J OD Surgery. 2019;29:2. [DOI] [Full Text] |
| 22. | Vu CK. Buried bumper syndrome: old problem, new tricks. J Gastroenterol Hepatol. 2002;17:1125-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Turner P, Deakin M. Percutaneous endoscopic gastrostomy tube removal and replacement after "buried bumper syndrome": the simple way. Surg Endosc. 2009;23:1914-1917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Müller-Gerbes D, Aymaz S, Dormann AJ. [Management of the buried bumper syndrome: a new minimally invasive technique--the push method]. Z Gastroenterol. 2009;47:1145-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Born P, Winker J, Jung A, Strebel H. Buried bumper--the endoscopic approach. Arab J Gastroenterol. 2014;15:82-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Hindryckx P, Dhooghe B, Wannhoff A. A novel device for the endoscopic management of buried bumper syndrome. Endoscopy. 2019;51:689-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Costa D, Despott EJ, Lazaridis N, Koukias N, Murino A. Minimally invasive endoscopic management of buried bumper syndrome by use of a novel dedicated resection device. VideoGIE. 2019;4:366-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Costa D, Despott EJ, Lazaridis N, Woodward J, Kohout P, Rath T, Scovell L, Gee I, Hindryckx P, Forrest E, Hollywood C, Hearing S, Mohammed I, Coppo C, Koukias N, Cooney R, Sharma H, Zeino Z, Gooding I, Murino A. Multicenter cohort study of patients with buried bumper syndrome treated endoscopically with a novel, dedicated device. Gastrointest Endosc. 2021;93:1325-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Curcio G, Granata A, Ligresti D, Tarantino I, Barresi L, Traina M. Buried bumper syndrome treated with HybridKnife endoscopic submucosal dissection. Gastrointest Endosc. 2014;80:916-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Wolpert LE, Summers DM, Tsang A. Novel endoscopic management of buried bumper syndrome in percutaneous endoscopic gastrostomy: The Olympus HookKnife. World J Gastroenterol. 2017;23:6546-6548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 31. | Nakamura H, Kikuchi S, Ohnuma H, Hirakawa M, Kato J. Total buried bumper syndrome: A case study in transabdominal removal using a technique of endoscopic submucosal dissection. Clin Case Rep. 2019;7:2012-2013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Strock P, Weber J. Buried bumper syndrome: endoscopic management using a balloon dilator. Endoscopy. 2005;37:279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Christiaens P, Bossuyt P, Cuyle PJ, Moons V, Van Olmen A. Buried bumper syndrome: single-step endoscopic management and replacement. Gastrointest Endosc. 2014;80:336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Marks JM, Ponsky JL, Pearl JP, McGee MF. PEG "Rescue": a practical NOTES technique. Surg Endosc. 2007;21:816-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 78] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 35. | Nennstiel S, Schlag C, Meining A. [Therapy of Buried Bumper Syndrome via NOTES - A Case Report]. Z Gastroenterol. 2013;51:744-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Furlano RI, Sidler M, Haack H. The push-pull T technique: an easy and safe procedure in children with the buried bumper syndrome. Nutr Clin Pract. 2008;23:655-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Kurek K, Baniukiewicz A, Świdnicka-Siergiejko A. Buried bumper syndrome: a rare complication of percutaneous endoscopic gastrostomy. Wideochir Inne Tech Maloinwazyjne. 2015;10:504-507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 38. | Lee MP. Impaction of gastrostomy tube in the abdominal wall. J Am Geriatr Soc. 1990;38:956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 39. | Kotzampassi K. "Buried bumper syndrome: It is the time to change the bumper". Parkinsonism Relat Disord. 2022;99:42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 40. | Kejariwal D, Aravinthan A, Bromley D, Miao Y. Buried bumper syndrome: cut and leave it alone! Nutr Clin Pract. 2008;23:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |