Published online Oct 16, 2023. doi: 10.4253/wjge.v15.i10.629
Peer-review started: July 4, 2023
First decision: August 16, 2023
Revised: August 30, 2023
Accepted: September 7, 2023
Article in press: September 7, 2023
Published online: October 16, 2023
Processing time: 99 Days and 12.8 Hours
Endoscopic sleeve gastroplasty (ESG) is a minimally invasive procedure used in the treatment of obesity, with a complication rate of less than 2% of cases. There have been only two reported cases worldwide of gallbladder injuries as a major complication of ESG.
We present the case of a 34-year-old patient who developed a complication after ESG. The patient experienced epigastric and right hypochondrium pain 12 h after the procedure, and a positive Murphy’s sign was identified on physical exami
Gallbladder plication should be suspected if signs and symptoms consistent with acute cholecystitis occur after ESG.
Core Tip: Only two cases have been reported worldwide of gallbladder plication as a major complication of endoscopic sleeve gastrectomy. We present the case of a 34-year-old patient who experienced right hypochondrium pain after endoscopic sleeve gastrectomy with a positive Murphy’s sign. Laboratory and imaging studies revealed acute cholecystitis findings and a possible gallbladder plication. Diagnostic laparoscopy confirmed plication of the Hartmann’s pouch wall to the stomach. A cholecystectomy was performed with a favorable outcome.
- Citation: Quiroz Guadarrama CD, Saenz Romero LA, Saucedo Moreno EM, Rojano Rodríguez ME. Gallbladder plication as a rare complication of endoscopic sleeve gastroplasty: A case report. World J Gastrointest Endosc 2023; 15(10): 629-633
- URL: https://www.wjgnet.com/1948-5190/full/v15/i10/629.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i10.629
Endoscopic sleeve gastroplasty (ESG) is performed using a suturing device placed at the tip of the endoscope, allowing for full-thickness suturing of the anterior, greater curvature, and posterior walls of the stomach[1-3]. While ESG is generally considered a safe procedure, some minor adverse effects have been observed, such as nausea, vomiting, and mild-to-moderate abdominal pain[4,5]. Only two cases have been reported worldwide of gallbladder plication as a major complication of ESG[6,7]. Due to its extreme rarity, there is no appropriate diagnostic and therapeutic protocol. Therefore, the relevance of this case report lies in identifying relevant clinical data in its presentation to develop a diagnostic strategy and potential treatments.
A 34-year-old female patient with a diagnosis of class I obesity (body mass index 30 kg/m2) was admitted for scheduled ESG as primary treatment for obesity. ESG was performed under balanced general anesthesia, with the patient in the left lateral decubitus position. A suturing device (Apollo EndoSurgery, Austin, TX, United States) was used attached to a dual-channel therapeutic endoscope (Olympus 190; Olympus, Tokyo, Japan). The gastric cavity was insufflated with carbon dioxide, and continuous “U” sutures were placed from the gastric body-antrum junction to the fundus. Four sutures were used, each consisting of eight stitches, creating the anterior, greater curvature, and posterior walls of the stomach. Immediately after the procedure, the patient experienced two episodes of hematemesis and drowsiness.
The patient had a surgical history of two previous cesarean sections and a hysterectomy more than 5 years ago. She also had trauma to both pelvic limbs due to an accident, which required multiple reconstructive surgeries on her left foot. There had no history of bariatric surgery or previous placement of an intragastric balloon.
The patient denied any personal history of illness.
The patient denied any family history of illness.
Immediately after the endoscopic procedure, the abdominal examination revealed a depressible abdomen without signs of peritoneal irritation, with present bowel sounds. Six hours after the procedure, the patient experienced epigastric pain and right hypochondrium pain with an intensity of 4/10 on the visual analog scale (VAS). She was able to tolerate a liquid diet, and her vital signs were stable with a blood pressure of 120/80 mmHg, heart rate of 89 beats per minute, and respiratory rate of 18 breaths per minute. However, 12 h after the procedure, the pain increased to an intensity of 8/10 on the VAS. During the physical examination, the abdomen was soft, and there was deep tenderness on palpation in the epigastrium and right hypochondrium, with a positive Murphy’s sign.
A complete blood count was requested, which showed white blood cell (WBC) count of 17.8 × 103/µL (normal range: 4.5-10.5 × 103/µL), with 91.9% (normal range: 40.0%-63.6%) segmented neutrophils.
An abdominal computed tomography scan was performed, revealing the presence of free fluid in the pelvic cavity at the level of the posterior sac and perihepatic recesses on the right anterior segments. Postsurgical changes in the stomach were also observed, and an image suggestive of a possible suture in the gallbladder wall was noted (Figure 1).
Gallbladder plication following ESG.
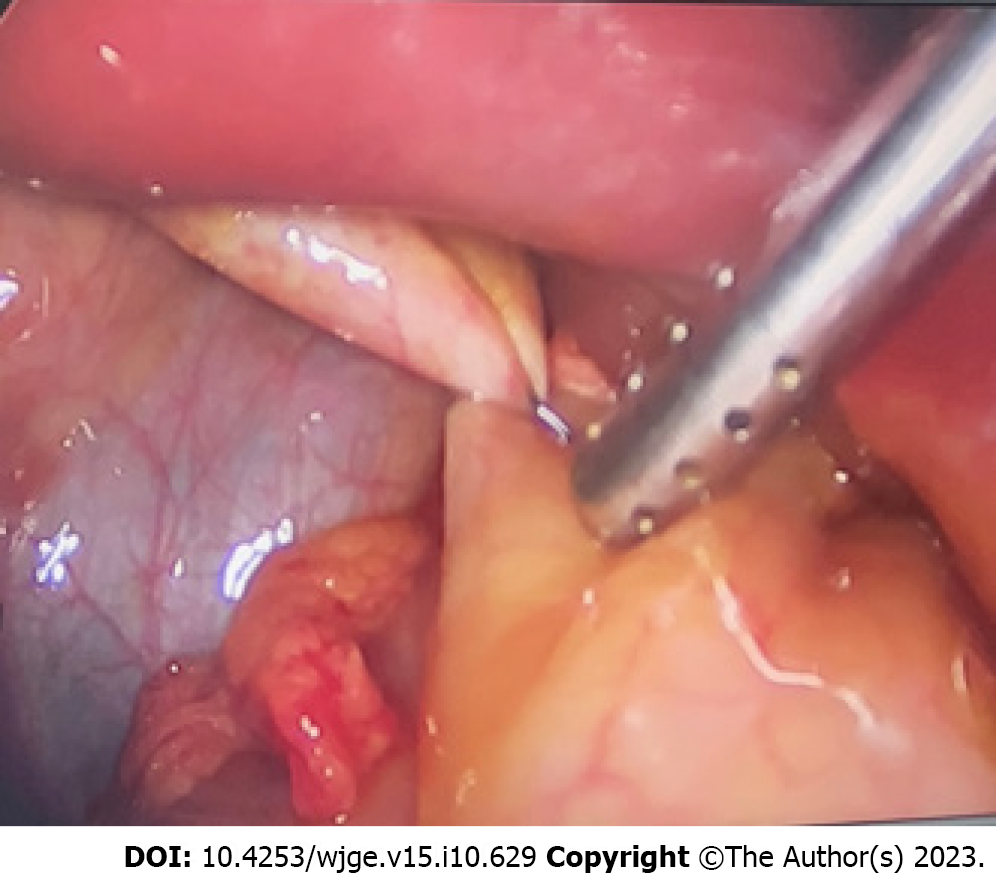
After evaluating the results, a diagnostic laparoscopy with intraoperative panendoscopy was performed. During the procedure, omental adhesions were identified in the gallbladder, a limited amount of free bile fluid was present, and a suture was found folding the gastric wall with the Hartmann’s pouch of the gallbladder (Figure 2). Abdominal cavity lavage was performed with 2 L of 0.9% saline solution, followed by a routine cholecystectomy with a critical view of safety according to Strasberg’s criteria without removing the suture. Intraoperative endoscopy was performed to confirm the absence of leaks into the abdominal cavity. Finally, a closed drainage was placed, and the surgical procedure was concluded.
Prophylactic intravenous ceftriaxone (1 g) was administered. During the first 12 postoperative hours, nonsteroidal anti-inflammatory drugs (intravenous parecoxib 40 mg every 12 h) and intravenous paracetamol (1 g every 8 h) were administered, and the patient continued fasting. At 24 h after surgery, the patient had stable vital signs, abdominal pain with an intensity of 3/10 on the VAS, and no nausea or vomiting with present peristalsis. The drainage output was less than 5 mL of serohematic fluid. Clear liquids were initiated orally 24 h after the surgical procedure, and a follow-up complete blood count was requested, which showed a decrease in WBC count to 13.0 × 103/µL (normal range: 4.5-10.5 × 103/µL). At 72 postoperative hours, the patient advanced to a soft diet with good tolerance, the drainage was removed, and she was discharged to home. During the follow-up visit at 7 d, the patient’s recovery was satisfactory, without pain, tolerating a regular diet, and continuing with post-ESG nutritional management. At 30 d after surgery, the patient had a weight loss of 12 kg without complications.
Obese patients with a high surgical risk or contraindication for abdominal surgery can benefit from minimally invasive endoscopic procedures[1-3,8]. The potential side effects during or after percutaneous endoscopic gastrostomy can be classified as minor or major. According to Alqahtani et al[4], minor symptoms affect 92.2% of patients and may include nausea, vomiting, and mild abdominal pain. Hedjoudje et al[9] conducted a meta-analysis of eight articles and concluded that major adverse events accounted for 2.2% of cases and were primarily related to transmural punctures that can occur during endoscopic suturing. These complications included unresponsive pain or nausea (1.08%), upper gastrointestinal bleeding (0.56%), leakage or perigastric collections (0.48%), pulmonary embolism (0.06%), and pneumoperitoneum (0.06%).
In the published medical literature, there are two cases of biliary tract plication following an ESG[6,7]. In our case, we were able to detect atypical symptoms in the patient’s progression by considering the clinical suspicion and previous knowledge of this complication. Patients who experience epigastric pain radiating to the right hypochondrium and a positive Murphy’s sign after an ESG should be considered as alarm signs.
After a detailed review of this case, several factors that could have contributed to this adverse event were identified. The patient’s position during the procedure was left lateral decubitus, which could have caused the gallbladder to come into contact with the gastric antrum. It is suspected that the suture was initiated closer to the antrum than the gastric body, resulting in the plication of the gallbladder.
It is important to note that there is currently no standardized diagnostic protocol to detect complications following an ESG. However, in cases like the one described in this report where atypical symptoms and elevated leukocyte levels are present, a suggestive computed tomography scan showing biliary tract suture and a high clinical suspicion may be sufficient for a timely diagnosis.
Similarly, there is no standardized therapeutic approach defined for this complication. A surgical approach was chosen for our case upon consideration of the findings from computed tomography (which although inconclusive suggested the presence of free fluid in the abdominal cavity) as well as the possibility of suture in the biliary tract and the patient’s elevated levels of leukocytes. Ultimately, this decision was based on the recommendations of the diagnostic laparoscopy guideline, which indicates its primary application following an initial diagnostic evaluation in patients with unexplained acute abdominal pain (of less than 7 d) or as an alternative to observation in cases of nonspecific abdominal pain[10].
It is important to note that this intervention has been shown to be safe in appropriately selected patients[10]. In this context, we believe that the best treatment option is to perform a diagnostic laparoscopy, which provides diagnostic accuracy and consequently results in earlier diagnoses, shorter hospital stays, and a reduction in morbidity.
In summary, although there are no standardized diagnostic protocols or treatments for biliary tract plication following ESG, we recommend a multidisciplinary approach to diagnosis. Its presence should be suspected based on signs and symptoms consistent with acute cholecystitis, suggestive findings on computed tomography indicating plication or inflammation of the gallbladder, and laboratory results showing leukocytosis. Based on our experience, we recommend that the appropriate treatment includes a diagnostic laparoscopy followed by conventional cholecystectomy.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Mexico
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cesaretti M, Italy; Correia de Sa T, Portugal S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Alqahtani AR, Elahmedi M, Aldarwish A, Abdurabu HY, Alqahtani S. Endoscopic gastroplasty vs laparoscopic sleeve gastrectomy: a noninferiority propensity score-matched comparative study. Gastrointest Endosc. 2022;96:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 39] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 2. | Nduma BN, Mofor KA, Tatang JT, Ekhator C, Ambe S, Fonkem E. Endoscopic Gastric Sleeve: A Review of Literature. Cureus. 2023;15:e36353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Singh S, Hourneaux de Moura DT, Khan A, Bilal M, Ryan MB, Thompson CC. Safety and efficacy of endoscopic sleeve gastroplasty worldwide for treatment of obesity: a systematic review and meta-analysis. Surg Obes Relat Dis. 2020;16:340-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 4. | Alqahtani A, Al-Darwish A, Mahmoud AE, Alqahtani YA, Elahmedi M. Short-term outcomes of endoscopic sleeve gastroplasty in 1000 consecutive patients. Gastrointest Endosc. 2019;89:1132-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 138] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 5. | Matteo MV, Bove V, Pontecorvi V, De Siena M, Ciasca G, Papi M, Giannetti G, Carlino G, Raffaelli M, Costamagna G, Boškoski I. Outcomes of Endoscopic Sleeve Gastroplasty in the Elder Population. Obes Surg. 2022;32:3390-3397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 6. | Lopez-Nava G, Asokkumar R, Ielpo B, Bautista I, Vicente E. Biliary peritonitis after endoscopic sutured gastroplasty for morbid obesity (with video). Gastrointest Endosc. 2019;90:686-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | de Siqueira Neto J, de Moura DTH, Ribeiro IB, Barrichello SA, Harthorn KE, Thompson CC. Gallbladder perforation due to endoscopic sleeve gastroplasty: A case report and review of literature. World J Gastrointest Endosc. 2020;12:111-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Lopez-Nava G, Asokkumar R, Bautista-Castaño I, Laster J, Negi A, Fook-Chong S, Nebreda Duran J, Espinett Coll E, Gebelli JP, Garcia Ruiz de Gordejuela A. Endoscopic sleeve gastroplasty, laparoscopic sleeve gastrectomy, and laparoscopic greater curve plication: do they differ at 2 years? Endoscopy. 2021;53:235-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Hedjoudje A, Abu Dayyeh BK, Cheskin LJ, Adam A, Neto MG, Badurdeen D, Morales JG, Sartoretto A, Nava GL, Vargas E, Sui Z, Fayad L, Farha J, Khashab MA, Kalloo AN, Alqahtani AR, Thompson CC, Kumbhari V. Efficacy and Safety of Endoscopic Sleeve Gastroplasty: A Systematic Review and Meta-Analysis. Clin Gastroenterol Hepatol. 2020;18:1043-1053.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 158] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 10. | Hori Y; SAGES Guidelines Committee. Diagnostic laparoscopy guidelines: This guideline was prepared by the SAGES Guidelines Committee and reviewed and approved by the Board of Governors of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), November 2007. Surg Endosc. 2008;22:1353-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |