Published online Sep 16, 2022. doi: 10.4253/wjge.v14.i9.564
Peer-review started: June 2, 2022
First decision: July 12, 2022
Revised: July 26, 2022
Accepted: September 6, 2022
Article in press: September 6, 2022
Published online: September 16, 2022
Processing time: 104 Days and 3.4 Hours
Choledocholithiasis develops in up to 20% of patients with gall bladder stones. The challenge in diagnosis usually occurs with small stones that may be missed by magnetic resonance cholangiopancreatography (MRCP). Endoscopic ultr
To evaluate the accuracy of EUS in detecting CBD stones missed by MRCP.
Patients with an intermediate likelihood of choledocholithiasis according to ESGE guidelines and those with acute pancreatitis of undetermined cause were incl
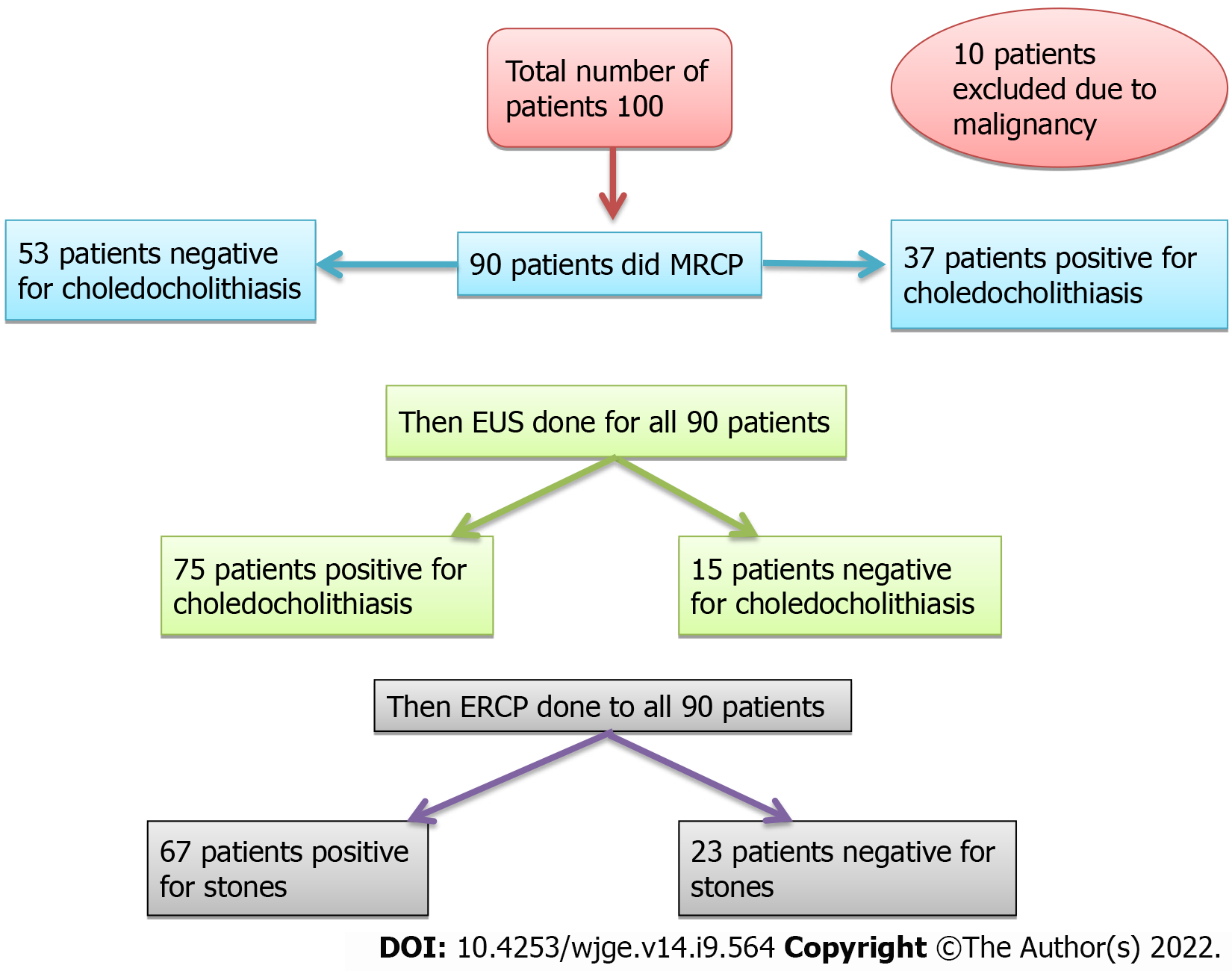
Ninety out of 100 involved patients had choledocholithiasis, while ten patients were excluded as they had pancreatic or gall bladder masses during EUS exam
EUS could be a useful tool in assessing patients with suspected choledocholithiasis especially if combined with MRCP. However, its usefulness depends on its availability and the experience of the local centers.
Core Tip: Still, there is a great challenge in diagnosing suspected cases of choledocholithiasis that could develop in up to 20% of patients with gall bladder stones. Endoscopic ultrasound (EUS) can easily detect small stones that magnetic resonance cholangiopancreatography (MRCP) could miss. EUS still has many diagnostic purposes with high accuracy in detecting common bile duct (CBD) stones missed by MRCP, especially the small ones or those impacted at the distal CBD or the papillary region.
- Citation: Eissa M, Okasha HH, Abbasy M, Khamis AK, Abdellatef A, Rady MA. Role of endoscopic ultrasound in evaluation of patients with missed common bile duct stones. World J Gastrointest Endosc 2022; 14(9): 564-574
- URL: https://www.wjgnet.com/1948-5190/full/v14/i9/564.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i9.564
Choledocholithiasis is considered one of the most important causes of abdominal pain in patients with gall bladder stones. It can occur in 3%-16% of patients with gall stones and can reach up to 21% in patients with gall stone pancreatitis[1,2]. Diagnosis of choledocholithiasis is not always straightforward[3]. Clinical evaluation and biochemical tests are insufficient to establish a firm diagnosis without reliable confirmatory testing, so magnetic resonance cholangiopancreatography (MRCP) is routinely used to clarify the diagnosis after ultrasound results[4]. Endoscopic retrograde cholangiopancreatography (ERCP) is now considered the gold standard for diagnosis; however, its invasive nature and complications such as pancreatitis defer its use in diagnosis as a first option[5].
Since the recommendations by the ASGE and ESGE guidelines for diagnosing patients with an intermediate likelihood of choledocholithiasis by MRCP, endoscopic ultrasound (EUS) is now widely used to assess the presence of choledocholithiasis[6,7]. Despite its overall high accuracy, the role of EUS in the diagnosis of choledocholithiasis has not been firmly established since EUS is relatively invasive compared with MRCP and computed tomography[8].
The cause of biliary obstruction is not always detected by the available non-invasive imaging modalities like MRCP and may be detected later during biliary drainage as small stones, so in our study, we evaluated the usefulness and accuracy of EUS in detecting missed stones by MRCP as a cause of biliary obstruction.
This observational cohort study aimed primarily to evaluate the usefulness and accuracy of EUS in de
This prospective study was conducted on 100 patients recruited from National Liver Institute and Internal Medicine Department, Kasr Al-Ainy Hospital from 2019 to 2021. We included patients with dilated CBD (diameter ranging from 6 to 10 mm), those with unexplained elevated liver enzymes, and those with unexplained causes of acute pancreatitis. All patients with cholangitis were excluded from the study and referred for urgent ERCP drainage. Also, we excluded patients with malignant masses found by EUS and confirmed by histopathology. All included patients were above 18 years of age.
Assessment of our patients was performed by liver function tests, serum amylase, lipase, abdominal ultrasound, MRCP, and EUS. ERCP was conducted on all patients for confirmation of the findings of MRCP and EUS. MRCP was done few days before EUS, then ERCP was done later on. The EUS operator was blind to MRCP examination. We followed up with the patients for 3 mo after the procedures clinically and biochemically.
Results from MRCP and EUS were compared with those from ERCP to calculate the sensitivity and specificity of EUS and MRCP in detecting choledocholithiasis in our patients. Also, the accuracy of both MRCP and EUS in detecting the size and number of stones in CBD was evaluated.
Our institution’s Research Ethical Committee approved the study, and all patients gave their informed written consent before inclusion in the study, according to the ethical guidelines of the 1975 Declaration of Helsinki.
All the patients, after thorough full history taking and clinical examination, were subjected to: (1) EUS examination using a linear Echoendoscope Pentax EG3870UTK (HOYA Corporation, PENTAX Life Care Division, Showanomori Technology Center, Tokyo, Japan) connected to a Hitachi AVIUS machine (Hitachi Medical Systems, Tokyo, Japan). All examinations were performed under deep sedation with IV propofol. For EUS-FNA, we used the Cook 19G and 22G needles (Echotip; Wilson-Cook, Winston Salem, NC). Prophylactic ceftriaxone (1 g) was administrated before the procedure; and (2) ERCP examination that was performed using a side view scope Pentax ED-3490TK (HOYA Corporation, Tokyo, Japan). All examinations were performed under deep sedation with IV propofol. Prophylactic ceftriaxone (1 g) was administrated before the procedure.
Data were fed to the computer and analyzed using IBM SPSS software version 20.0 (Armonk, NY: IBM Corp). Qualitative data are described using numbers and percentages. The Kolmogorov-Smirnov test was used to verify the normality of distribution. Quantitative data are described using range (minimum and maximum), mean, standard deviation, median, and interquartile range. The significance of the obtained results was judged at the 5% level. The chi-square test was applied to compare categorical variables between different groups. The Fisher’s exact test was used for correction for chi-square when more than 20% of the cells had an expected count of less than 5.
After excluding the ten patients with malignancy, the total number of male patients was 47 (52%), and that of female patients was 43 (48%), who were included till the end of the study with a mean age of 52.37 ± 14.64 years (Figure 1). The number of patients who fulfilled the criteria of an intermediate probability of biliary obstruction were 67 (74.4%), while that of patients with unexplained acute pancreatitis was 23 (25.6%). Only seven patients proved to have CBD stones, of whom all were detected by EUS, but only four were detected by MRCP. No other causes of acute pancreatitis as cystic pancreatic lesions, pancreatic divisum, or pancreatic duct stones could be detected by MRCP or EUS. Most patients had elevated liver enzymes (60%) and direct hyperbilirubinemia (81%), as shown in Table 1. Abdominal ultrasound showed that 72.2% of patients had gall bladder stones; meanwhile, only nine had a history of cholecystectomy with a mean CBD diameter of 9.13 ± 2.35 mm (Figure 2).
| n | % | |
| Alanine transaminase, aspartate aminotransferase | Up to 33 U/L | |
| Normal | 36 | 40.0 |
| < 3 fold | 44 | 48.9 |
| ≥ 3 fold | 10 | 11.1 |
| Bilirubin | Up to 1.1 mg/dL | |
| Normal | 17 | 18.9 |
| Yes | 73 | 81.1 |
| < 5 mg/100 mL | 54 | 74.0 |
| ≥ 5 mg/100 mL | 19 | 26.0 |
| Min-Max | 1.40-20.0 | |
| mean ± SD | 3.99 ± 3.30 | |
| Median (IQR) | 3.0 (2.0-5.0) | |
| Alkaline phosphatase | 35-104 U/L | |
| GGT | Up to 40 U/L | |
| Normal | 7 | 7.8 |
| < 3 fold | 24 | 26.7 |
| ≥ 3 fold | 59 | 65.6 |
Choledocholithiasis was detected in 83.3% of patients by EUS, 74.4% by ERCP but only 41.1% by MRCP. EUS detected the number of stones more accurately than MRCP (95% vs 41%, respectively), as shown in Table 2.
| Common bile duct stones detected by endoscopic ultrasound | Patients (n) | % |
| Common bile duct stones detected by endoscopic ultrasound | ||
| No | 15 | 16.7 |
| Yes | 75 | 83.3 |
| Stones (n) | ||
| No stones | 20 | 22.2 |
| 1 | 42 | 46.7 |
| 2 | 12 | 13.3 |
| 3 | 5 | 5.6 |
| 4 | 1 | 1.1 |
| 5 | 1 | 1.1 |
| 6 | 1 | 1.1 |
| Multiple | 8 | 8.9 |
| Size of stones (mm) | ||
| No stones | 20 | 22.2 |
| Gravels (1-2 mm) | 2 | 2.2 |
| 3-5 | 25 | 27.8 |
| > 5 | 43 | 47.8 |
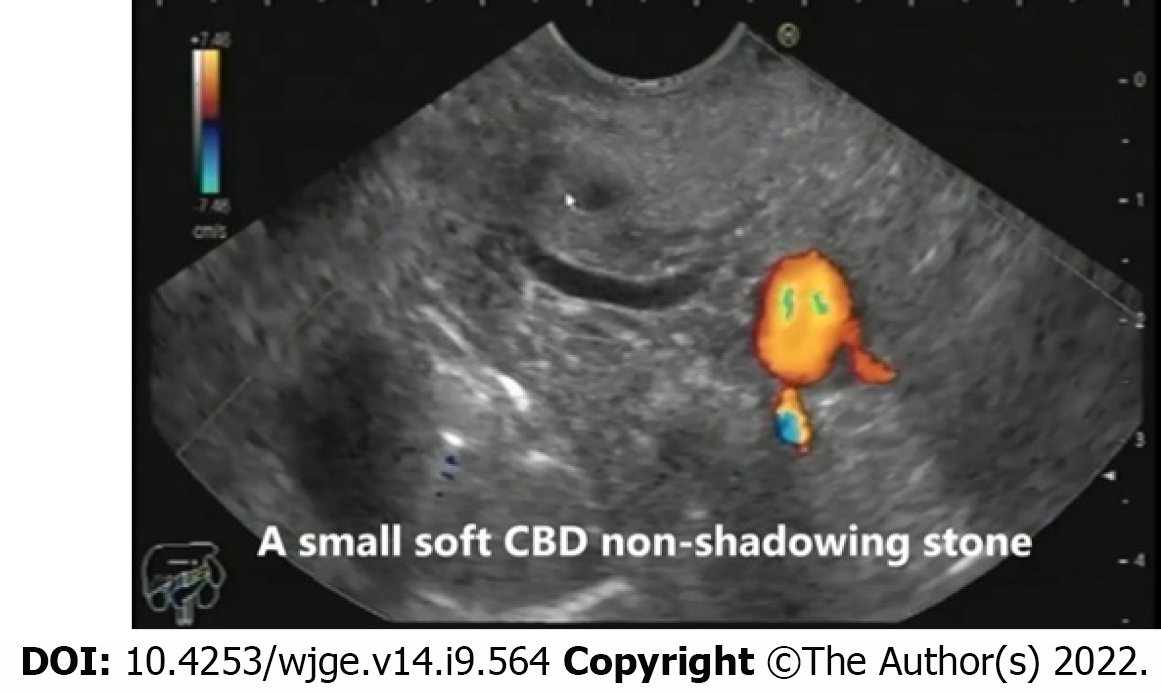
Regarding the size of stones, EUS had a higher accuracy in detecting stones less than 5 mm (25 out of 53 negatives for stones by MRCP), as shown in Table 2.
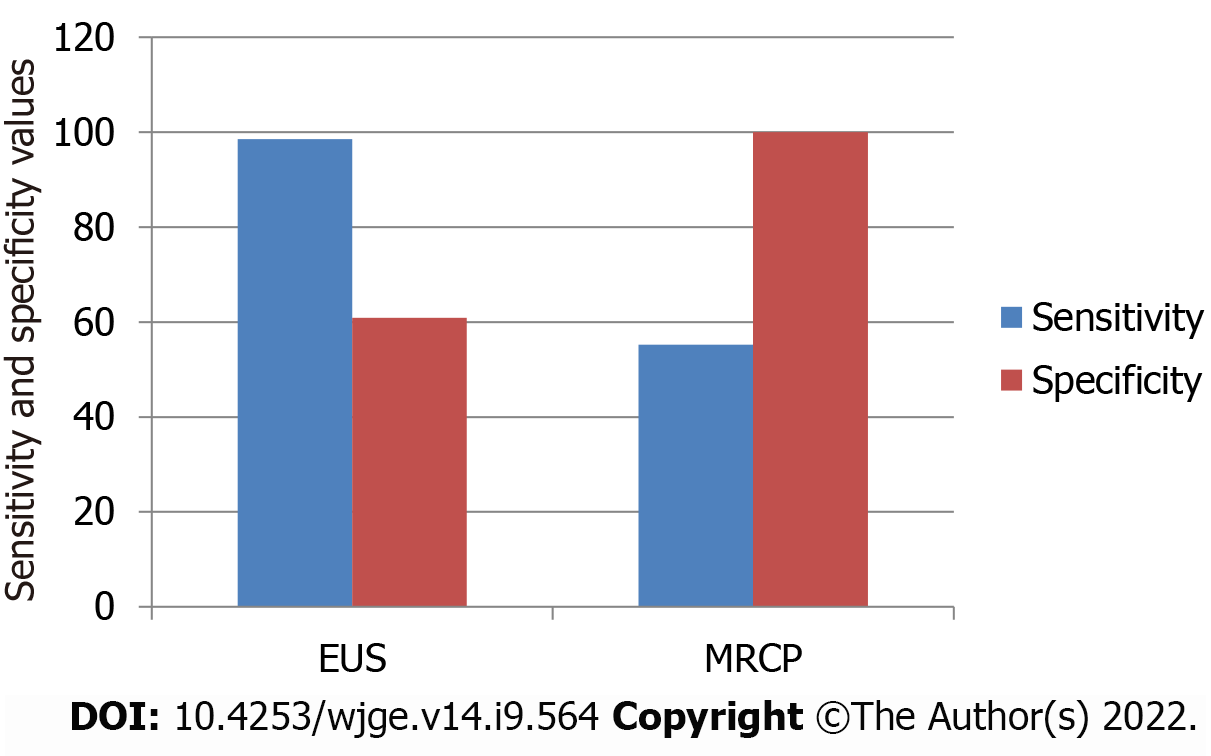
EUS was statistically more accurate than MRCP in detecting stones (P < 0.001), especially in stones less than 5 mm (88.8% vs 66.6%, respectively). The sensitivity of EUS was 98.51%, while that of MRCP was only 55.5%, but the specificity of MRCP was higher than that of EUS (100% vs 60.87%, respectively), as shown in Table 3. The combination of EUS with MRCP showed a sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and overall accuracy of 97.22%, 100%, 100%, 91.67%, and 97.87%, respectively (Table 4).
| Endoscopic retrograde cholangiopancreatography findings | Sensitivity | Specificity | PPV | NPV | Accuracy | ||||
| No (n = 23) | Yes (n = 67) | ||||||||
| CBD stones detected by EUS | n | % | n | % | |||||
| No | 14 | 60.9 | 1 | 1.5 | 98.51 | 60.87 | 88.0 | 93.33 | 88.89 |
| Yes | 9 | 39.1 | 66 | 98.5 | |||||
| FEP value | 43.464 (< 0.001) | ||||||||
| MRCP stones | n | % | n | % | |||||
| No | 23 | 100.0 | 30 | 44.8 | |||||
| Yes | 0 | 0.0 | 37 | 55.2 | 55.22 | 100.0 | 100.0 | 43.40 | 66.67 |
| P value | 21.569 (< 0.001) | ||||||||
| Combined EUSMRCP | ERCP findings | Sensitivity | Specificity | PPV | NPV | Accuracy | |||
| No (n = 11) | Yes (n = 36) | ||||||||
| n | % | n | % | ||||||
| No | 11 | 100.0 | 1 | 2.8 | 97.22 | 100.0 | 100.0 | 91.67 | 97.87 |
| Yes | 0 | 0.0 | 35 | 97.2 | |||||
| FEP value | 41.887 (< 0.001) | ||||||||
Indeed, there are differences in endoscopic skill between endoscopists, so we analyzed the data for expert and non-expert endoscopists (Table 5).
| CBD stones detected by EUS | Total (n = 90) | Non-expert (n = 27) | Expert (n = 63) | ||||||
| n | % | n | % | n | % | ||||
| No | 15 | 16.7 | 11 | 40.7 | 4 | 6.3 | |||
| Yes | 75 | 83.3 | 16 | 59.3 | 59 | 93.7 | |||
| Number | |||||||||
| No. | 20 | 22.2 | 14 | 51.9 | 6 | 9.5 | |||
| 1 | 42 | 46.7 | 8 | 29.6 | 34 | 54.0 | |||
| 2 | 12 | 13.3 | 2 | 7.4 | 10 | 15.9 | |||
| 3 | 5 | 5.6 | 0 | 0.0 | 5 | 7.9 | |||
| 4 | 1 | 1.1 | 0 | 0.0 | 1 | 1.6 | |||
| 5 | 1 | 1.1 | 0 | 0.0 | 1 | 1.6 | |||
| 6 | 1 | 1.1 | 0 | 0.0 | 1 | 1.6 | |||
| Multiple | 8 | 8.9 | 3 | 11.1 | 5 | 7.9 | |||
| Size (mm) | |||||||||
| No. | 22 | 24.4 | 14 | 51.9 | 8 | 12.7 | |||
| ≤ 5 | 25 | 27.8 | 4 | 14.8 | 21 | 33.3 | |||
| > 5 | 43 | 47.8 | 9 | 33.3 | 34 | 54.0 | |||
| Other findings of EUS | |||||||||
| No | 65 | 72.2 | 14 | 51.9 | 51 | 81.0 | |||
| Yes | 25 | 27.8 | 13 | 48.1 | 12 | 19.0 | |||
| ERCP findings | Sensitivity | Specificity | PPV | NPV | Accuracy | ||||
| No | Yes | ||||||||
| n | % | n | % | ||||||
| Total sample (n = 90) | n = 23 | n = 67 | |||||||
| No | 14 | 60.9 | 1 | 1.5 | |||||
| Yes | 9 | 39.1 | 66 | 98.5 | 98.51 | 60.87 | 88.0 | 93.33 | 88.89 |
| FEP value | 43.464 (< 0.001) | ||||||||
| Non-expert (n = 27) | n = 13 | n = 14 | |||||||
| No | 10 | 76.9 | 1 | 7.1 | |||||
| Yes | 3 | 23.1 | 13 | 92.9 | 92.86 | 76.92 | 81.25 | 90.91 | 85.19 |
| FEP value | 13.595 (< 0.001) | ||||||||
| Expert (n = 63) | n = 10 | n = 53 | |||||||
| No | 4 | 40.0 | 0 | 0.0 | |||||
| Yes | 6 | 60.0 | 53 | 100.0 | 100.0 | 40.0 | 89.83 | 100.0 | 90.48 |
| FEP value | 22.637 (< 0.001) | ||||||||
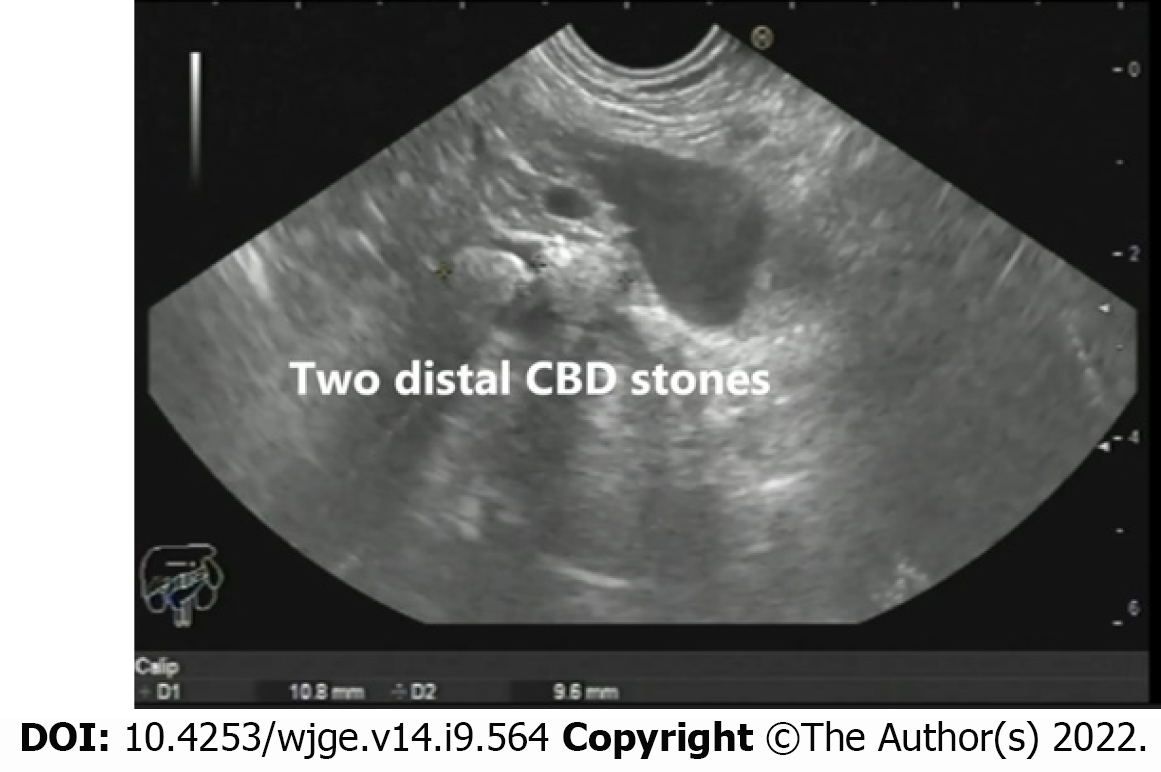
We found ten cases considered false negative by EUS, where six cases had gravels on EUS, three had small non-floating stones less than 5 mm, and one had a stone over the old plastic stent. Figures 3-5 show different forms of detected CBD stones from our patients.
The ten cases with the malignant cause of biliary obstruction were detected by EUS as seven cases with pancreatic head mass, two with gall bladder carcinoma, and one with CBD mass (diagnosed as cholangiocarcinoma by further evaluation with spyglass).
MRCP has been used to detect biliary obstruction in the last decade, but the cause cannot be detected in many patients[5]. The latest ASGE and ESGE guidelines recommend performing MRCP or EUS for evaluating patients with an intermediate probability of choledocholithiasis. However, it does not recommend one modality over the other[6,7]. Since the wide use of EUS, many studies have evaluated its role in detecting the cause of biliary obstruction[8]. EUS has a high accuracy in diagnosing pancreatic diseases and sampling tissues, but its role in diagnosing choledocholithiasis has not been confirmed like in pancreatic diseases[9].
This study evaluated the accuracy of EUS in detecting CBD stones, especially those missed by MRCP in patients with an intermediated probability of CBD stones and recurrent unexplained pancreatitis. Our study included 100 patients, which is considered a large number compared to other studies like Rana et al[10] (40 patients) and Patel et al[11] (78 patients), but a small number compared to Wee et al[12] who included 593 patients but only 35.3% of those patients had MRCP (all our patients had MRCP).
Similar to the previously mentioned studies[10,11], we found no statistically significant variables regarding clinical and laboratory data that could predict the presence of CBD stones on EUS, MRCP, or ERCP.
In the current study, we found that EUS had a higher accuracy in detecting choledocholithiasis than MRCP (88.8% vs 66.6%, respectively) with a higher sensitivity (98% vs 55%, respectively) but lower specificity (60.8% vs 100%, respectively). This lower specificity of EUS might be attributed to the time gap between EUS and ERCP (passed stones), missed gravels during balloon sweeping, and false perception of air as stones in some cases. Many other studies that evaluated the diagnosis of choledocholithiasis by EUS showed variable results regarding sensitivities and specificities. For example, Jagtap et al[13] showed that the sensitivities of both EUS and MRCP were similarly high (92%-98%). Also, Patel et al[11] showed that the sensitivity and specificity of EUS were 93% and 97.3%, respectively, but most included patients had a high probability of choledocholithiasis. Wee et al[12] reported sensitivities from 85% to 100% for EUS and 73% to 99% for MRCP. In a meta-analysis of five head-to-head studies comparing EUS to MRCP for choledocholithiasis, the pooled sensitivity and specificity of EUS were 97% and 90%, respectively, vs 87% and 92% for MRCP, respectively[14].
Also, de Lédinghen et al[15] reported a good sensitivity (100%) but low specificity (62%) for MRCP in diagnosing choledocholithiasis. Meanwhile, Materne et al[16] showed a 91% sensitivity and 94% specificity for MRCP, close to the values for EUS. The study conducted by Scheiman et al[17] reported significantly better results with EUS (sensitivity, 95%; specificity, 80%) than with MRCP (sensitivity, 40%; specificity, 96%) in diagnosing choledocholithiasis.
Another study compared the accuracy of EUS with ERCP in detecting choledocholithiasis and showed that EUS had a sensitivity of 100% and specificity of 94.7%.
One of the reasons for missed stones by MRCP that were detected by EUS was non-floating stones at the papillary region or distal CBD, as this is considered one of the pitfalls in MRCP interpretation, as mentioned by Irie et al[18]. Another reason was the stones with a diameter less than 5 mm (25 cases detected by EUS vs only 10 by MRCP), which suggests the accuracy of EUS in detecting small stones[19]. Also, EUS was superior to MRCP in detecting the number of stones inside the CBD (70 cases by EUS vs only 26 by MRCP), which is contradictory to the study of Aubé et al[20] that found no significant difference between the two modalities (MRCP detected four of six cases while EUS detected five of six cases).
Many studies comparing EUS and MRCP in idiopathic acute pancreatitis have shown that EUS has higher diagnostic yields than MRCP[21]. In this context, EUS should be considered the first choice in diagnosing idiopathic acute pancreatitis[22]. Biliary diseases such as cholelithiasis, choledocholithiasis, microlithiasis, and biliary sludge are the leading cause of idiopathic acute pancreatitis[23].
In our study, cases with unexplained pancreatitis were evaluated by EUS and MRCP, which showed that EUS was more sensitive in detecting stones than MRCP (90% vs 78%, respectively), as only seven patients proved to have CBD stones, of whom all were detected by EUS but only four were detected by MRCP[23]. Meanwhile, no other causes of acute pancreatitis as cystic pancreatic lesions, pancreatic divisum, or pancreatic duct stones could be detected by MRCP or EUS. And this finding is in agreement with Akkuzu et al[24], who reported a sensitivity of EUS and MRCP in evaluating acute pancreatitis of 89.65% and 72.4%, respectively.
Combining EUS with MRCP is very valuable in diagnosis of missed CBD stones than each one alone. In our study, the combination of the two tools raised the sensitivity, specificity, PPV, NPV, and overall accuracy into 97.22, 100, 100, 91.67, and 97.87, respectively.
The main limitation in our study was the financial cost of doing EUS, ERCP, and MRCP for all of the included patients. The second limitation was that we considered ERCP as the gold standard in detecting CBD stones. Although it is an accurate modality for detecting CBD stones, some false-negative cases may occur. Small stones may be missed if the CBD is under- or over-filling with contrast. Minute stones or gravels may be missed during balloon sweeping. Also, in some cases, there was a time gap between ERCP and EUS that might give a chance of passage of small stones out of the CBD that could give false-positive results on EUS.
Our study showed that EUS and MRCP are not equal tools in diagnosing choledocholithiasis in patients with an intermediate probability of choledocholithiasis. EUS is more accurate than MRCP in detecting non-floating stones in the papillary region and small stones, especially those less than 5 mm, and defining the size and number of stones. Furthermore, combining EUS with MRCP proved to be very valuable in accurate diagnosis of patients with an intermediate probability of choledocholithiasis.
EUS could be a good first option for evaluating patients with an intermediate probability of choledocholithiasis when it is available with good experience.
Combining EUS with MRCP is recommended for accurate evaluation of patients with an intermediate probability of choledocholithiasis if both are available.
Choledocholithiasis develops in up to 20% of patients with gall bladder stones. The challenge in diagnosis usually occurs with small stones that may be missed by magnetic resonance cholangiopancreatography (MRCP). Endoscopic ultrasound (EUS) is accurate in detecting common bile duct (CBD) stones missed by MRCP, especially the small ones or those impacted at the distal CBD or the papillary region.
Still, there is a great challenge in diagnosing cases with an intermediate probability of choledocholithiasis that develop in up to 20% of patients with gall bladder stones. EUS can easily detect small stones that MRCP could miss. EUS still has many diagnostic purposes with a high accuracy in detecting CBD stones missed by MRCP, especially the small ones or those impacted at the distal CBD or the papillary region.
To evaluate the accuracy of EUS in detecting CBD stones missed by MRCP.
Patients with an intermediate likelihood of choledocholithiasis according to ESGE guidelines and those with acute pancreatitis of undetermined cause were included. The presence of choledocholithiasis was evaluated by MRCP and EUS, and then results were confirmed by endoscopic retrograde cholangiopancreatography (ERCP). The sensitivity and specificity of EUS and MRCP were compared regarding the presence of stones, the size, and the number of detected stones.
Ninety out of 100 involved patients had choledocholithiasis, while ten patients were excluded as they had pancreatic or gall bladder masses during EUS examination. In choledocholithiasis patients, the mean age was 52.37 ± 14.64 years, and 52.2% were males. Most patients had biliary obstruction (74.4%), while only 23 (25.6%) patients had unexplained pancreatitis. The overall prevalence of choledocholithiasis was 83.3% by EUS, 41.1% by MRCP, and 74.4% by ERCP. Also, the number and size of CBD stones could be detected accurately in 78.2% and 75.6% by EUS and 41.1% and 70.3% by MRCP, respectively. The sensitivity of EUS was higher than that of MRCP (98.51% vs 55.22%), and their predictive value was statistically different (P < 0.001). Combination of both tools raised the sensitivity to 97.22% and specificity to 100%.
EUS could be a useful tool in assessing patients with suspected choledocholithiasis especially if combined with MRCP. However, its usefulness depends on its availability and the experience of the local centers.
EUS could be a good first option for evaluating patients with an intermediate probability of choledocholithiasis when it is available with good experience. Combining EUS with MRCP is recommended for accurate evaluation of patients with an intermediate probability of choledocholithiasis if both are available.
We would like to acknowledge our great hospital, and its workers, nurses, and staff members, for all the support and help in this study and throughout our careers.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Er LM, China; Pelaez-Luna M, Mexico S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones. Gastroenterol Clin North Am. 2010;39:157-169, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 227] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 2. | Collins C, Maguire D, Ireland A, Fitzgerald E, O'Sullivan GC. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg. 2004;239:28-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 319] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 3. | Gurusamy KS, Giljaca V, Takwoingi Y. Ultrasound vs liver function tests for diagnosis of common bile duct stones. Cochrane Database Syst Rev. 2015;2015:CD011548. [RCA] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Schmidt S, Chevallier P, Novellas S, Gelsi E, Vanbiervliet G, Tran A, Schnyder P, Bruneton JN. Choledocholithiasis: repetitive thick-slab single-shot projection magnetic resonance cholangiopancreaticography versus endoscopic ultrasonography. Eur Radiol. 2007;17:241-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Richard F, Boustany M, Britt LD. Accuracy of magnetic resonance cholangiopancreatography for diagnosing stones in the common bile duct in patients with abnormal intraoperative cholangiograms. Am J Surg. 2013;205:371-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 372] [Article Influence: 62.0] [Reference Citation Analysis (0)] |
| 7. | ASGE Standards of Practice Committee; Buxbaum JL, Abbas Fehmi SM, Sultan S, Fishman DS, Qumseya BJ, Cortessis VK, Schilperoort H, Kysh L, Matsuoka L, Yachimski P, Agrawal D, Gurudu SR, Jamil LH, Jue TL, Khashab MA, Law JK, Lee JK, Naveed M, Sawhney MS, Thosani N, Yang J, Wani SB. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019;89:1075-1105.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 327] [Article Influence: 54.5] [Reference Citation Analysis (0)] |
| 8. | Giljaca V, Gurusamy KS, Takwoingi Y. Endoscopic ultrasound vs magnetic resonance cholangiopancreatography for common bile duct stones. Cochrane Database Syst Rev. 2015;2015:CD011549. [RCA] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 9. | Gonzalo-Marin J, Vila JJ, Perez-Miranda M. Role of endoscopic ultrasound in the diagnosis of pancreatic cancer. World J Gastrointest Oncol. 2014;6:360-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 55] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Rana SS, Bhasin DK, Sharma V, Rao C, Gupta R, Singh K. Role of endoscopic ultrasound in evaluation of unexplained common bile duct dilatation on magnetic resonance cholangiopancreatography. Ann Gastroenterol. 2013;26:66-70. [PubMed] |
| 11. | Patel R, Ingle M, Choksi D, Poddar P, Pandey V, Sawant P. Endoscopic Ultrasonography Can Prevent Unnecessary Diagnostic Endoscopic Retrograde Cholangiopancreatography Even in Patients with High Likelihood of Choledocholithiasis and Inconclusive Ultrasonography: Results of a Prospective Study. Clin Endosc. 2017;50:592-597. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Wee D, Izard S, Grimaldi G, Raphael KL, Lee TP, Trindade AJ. EUS assessment for intermediate risk of choledocholithiasis after a negative magnetic resonance cholangiopancreatography. Endosc Ultrasound. 2020;9:337-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Jagtap N, Kumar JK, Chavan R, Basha J, Tandan M, Lakhtakia S, Kalapala R, Nabi Z, Gupta R, Ramchandani M, Talukdar R, Reddy M, Yarlagadda R, Singh J, Memon SF, Venkat Rao G, Reddy DN. EUS versus MRCP to perform ERCP in patients with intermediate likelihood of choledocholithiasis: a randomised controlled trial. Gut. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Meeralam Y, Al-Shammari K, Yaghoobi M. Diagnostic accuracy of EUS compared with MRCP in detecting choledocholithiasis: a meta-analysis of diagnostic test accuracy in head-to-head studies. Gastrointest Endosc. 2017;86:986-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 97] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 15. | de Lédinghen V, Lecesne R, Raymond JM, Gense V, Amouretti M, Drouillard J, Couzigou P, Silvain C. Diagnosis of choledocholithiasis: EUS or magnetic resonance cholangiography? Gastrointest Endosc. 1999;49:26-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 135] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Materne R, Van Beers BE, Gigot JF, Jamart J, Geubel A, Pringot J, Deprez P. Extrahepatic biliary obstruction: magnetic resonance imaging compared with endoscopic ultrasonography. Endoscopy. 2000;32:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 74] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Scheiman JM, Carlos RC, Barnett JL, Elta GH, Nostrant TT, Chey WD, Francis IR, Nandi PS. Can endoscopic ultrasound or magnetic resonance cholangiopancreatography replace ERCP in patients with suspected biliary disease? Am J Gastroenterol. 2001;96:2900-2904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 133] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Irie H, Honda H, Kuroiwa T, Yoshimitsu K, Aibe H, Shinozaki K, Masuda K. Pitfalls in MR cholangiopancreatographic interpretation. Radiographics. 2001;21:23-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Ney MV, Maluf-Filho F, Sakai P, Zilberstein B, Gama-Rodrigues J, Rosa H. Echo-endoscopy versus endoscopic retrograde cholangiography for the diagnosis of choledocholithiasis: the influence of the size of the stone and diameter of the common bile duct. Arq Gastroenterol. 2005;42:239-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Aubé C, Delorme B, Yzet T, Burtin P, Lebigot J, Pessaux P, Gondry-Jouet C, Boyer J, Caron C. MR cholangiopancreatography versus endoscopic sonography in suspected common bile duct lithiasis: a prospective, comparative study. AJR Am J Roentgenol. 2005;184:55-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Ortega AR, Gómez-Rodríguez R, Romero M, Fernández-Zapardiel S, Céspedes Mdel M, Carrobles JM. Prospective comparison of endoscopic ultrasonography and magnetic resonance cholangiopancreatography in the etiological diagnosis of "idiopathic" acute pancreatitis. Pancreas. 2011;40:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Wan J, Ouyang Y, Yu C, Yang X, Xia L, Lu N. Comparison of EUS with MRCP in idiopathic acute pancreatitis: a systematic review and meta-analysis. Gastrointest Endosc. 2018;87:1180-1188.e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 23. | Wilcox CM, Seay T, Kim H, Varadarajulu S. Prospective Endoscopic Ultrasound-Based Approach to the Evaluation of Idiopathic Pancreatitis: Causes, Response to Therapy, and Long-term Outcome. Am J Gastroenterol. 2016;111:1339-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Mustafa Zanyar Akkuzu, Engin Altıntaş, Serkan Yaraş, Osman Özdoğan, Enver Ucbilek, Fehmi Ates, Orhan Sezgin, Ferzan Aydın, Hatice Rızaoğlu Balcı, Yaren Dirik. EUS accuracy against MRCP for detection of pancreaticobiliary lesions. Eastern J Med. 2020;25:535-539. [DOI] [Full Text] |