Published online Jul 16, 2022. doi: 10.4253/wjge.v14.i7.434
Peer-review started: January 11, 2022
First decision: March 10, 2022
Revised: March 16, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: July 16, 2022
Processing time: 183 Days and 8.8 Hours
Obscure gastrointestinal (GI) bleeding is defined as persistent bleeding despite negative evaluation with both esophagogastroduodenoscopy and colonoscopy and can be secondary to small intestinal pathology. Standard endoscopy as well as push endoscopy can be a challenge in those with altered anatomy given inaccessible areas as well as perforation risk. Single and double balloon enter
To assess the safety and diagnostic efficacy of balloon enteroscopy for obscure GI bleeding in patients with surgically altered anatomy.
A search was conducted through PubMed, MEDLINE, Google Scholar, Scopus, and Embase with the key words “enteroscopy,” “obscure bleeding,” and “altered anatomy,” to identify relevant articles in English with no restricted time frame. A search within the Reference Citation Analysis database was conducted to ensure inclusion of the latest high impact articles. Study types included in the review were prospective and retrospective reviews, case series, and case reports. The reference lists of these papers were also reviewed to find further papers that were applicable. The authors extracted the data from the studies that fit inclusion criteria. Data of interest included type of study, type of procedure, and type of altered anatomy, as well as the number of patients with any diagnostic or therapeutic intervention. Data was also recorded on procedure tolerance and complications. The data was analyzed with descriptive statistics.
Our literature search yielded 14 studies that were included. There were 68 procedures performed with 61 unique patients subjected to these procedures. Forty-four (65%) of the procedures were double balloon, 21 (31%) were single balloon, and 3 (4%) were classified as through the scope balloon assisted. The most common altered anatomy types included Gastric Bypass Roux-en-Y, Pylorus Sparing Whipple, Orthotopic Liver Transplantation with Roux-en-Y, and Gastrojejunostomy Roux-en-Y. The procedures were successfully performed in each patient. There were 5 (7%) procedures that were complicated by perforation. Amongst the available data, the diagnostic yield was 48/59 (81%) and a therapeutic yield of 39/59 (66%). One patient was recommended surgical revision of their altered anatomy following enteroscopy.
Balloon enteroscopy is a useful diagnostic modality in investigating obscure GI bleeding within those with surgically altered anatomy; however, precautions must be taken as this population may have increased perforation risk.
Core Tip: Balloon enteroscopy is often warranted in patients with surgically altered anatomy who suffer from obscure gastrointestinal (GI) bleeding. Data remain limited on the clinical utility of single or double balloon enteroscopy in those with altered anatomy. The primary aim of this systematic review was to assess the diagnostic and therapeutic efficacy of balloon enteroscopy for obscure GI bleeding in patients with surgically altered anatomy. The secondary aim was to investigate the safety of balloon enteroscopy in this patient population.
- Citation: Aryan M, Colvin T, Ahmed AM, Kyanam Kabir Baig KR, Peter S. Role of balloon enteroscopy for obscure gastrointestinal bleeding in those with surgically altered anatomy: A systematic review. World J Gastrointest Endosc 2022; 14(7): 434-442
- URL: https://www.wjgnet.com/1948-5190/full/v14/i7/434.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i7.434
Obscure gastrointestinal (GI) bleeding is defined as persistent bleeding despite negative evaluation with both esophagogastroduodenoscopy and colonoscopy. Most obscure GI bleeding can be secondary to small intestinal pathology and has now become manageable with the introduction of single balloon enteroscopy (SBE) or double balloon enteroscopy (DBE) in 2001[1]. The overall diagnostic utility of DBE has ranged from 59%-90%[2-5]. In patients with surgically altered anatomy, endoscopic procedures may be challenging. Given distortion of native anatomy, areas that may have been accessible with standard endoscopy may be inaccessible or difficult to reach. In such instances, anastomotic areas remain at risk for perforation especially when larger diameter endoscopes are inserted at longer lengths. Deep enteroscopy can also be implemented to access sites unreachable by standard endoscopy[6]. Those with distorted anatomy may require thorough investigation of the upper GI tract in instances such as refractory abdominal pain or obscure GI bleeding. Balloon enteroscopy can be warranted in such cases where standard and push endoscopy are unrevealing.
SBE and DBE have been shown to be effective in patients with surgically altered anatomy in regards to endoscopic retrograde pancreatography (ERCP) and biliary complications. However, there remains limited information regarding management of obscure GI bleeding in patients with surgically altered anatomy. This systematic review aims to assess the overall safety and diagnostic efficacy of balloon enteroscopy for obscure GI bleeding in patients with surgically altered anatomy.
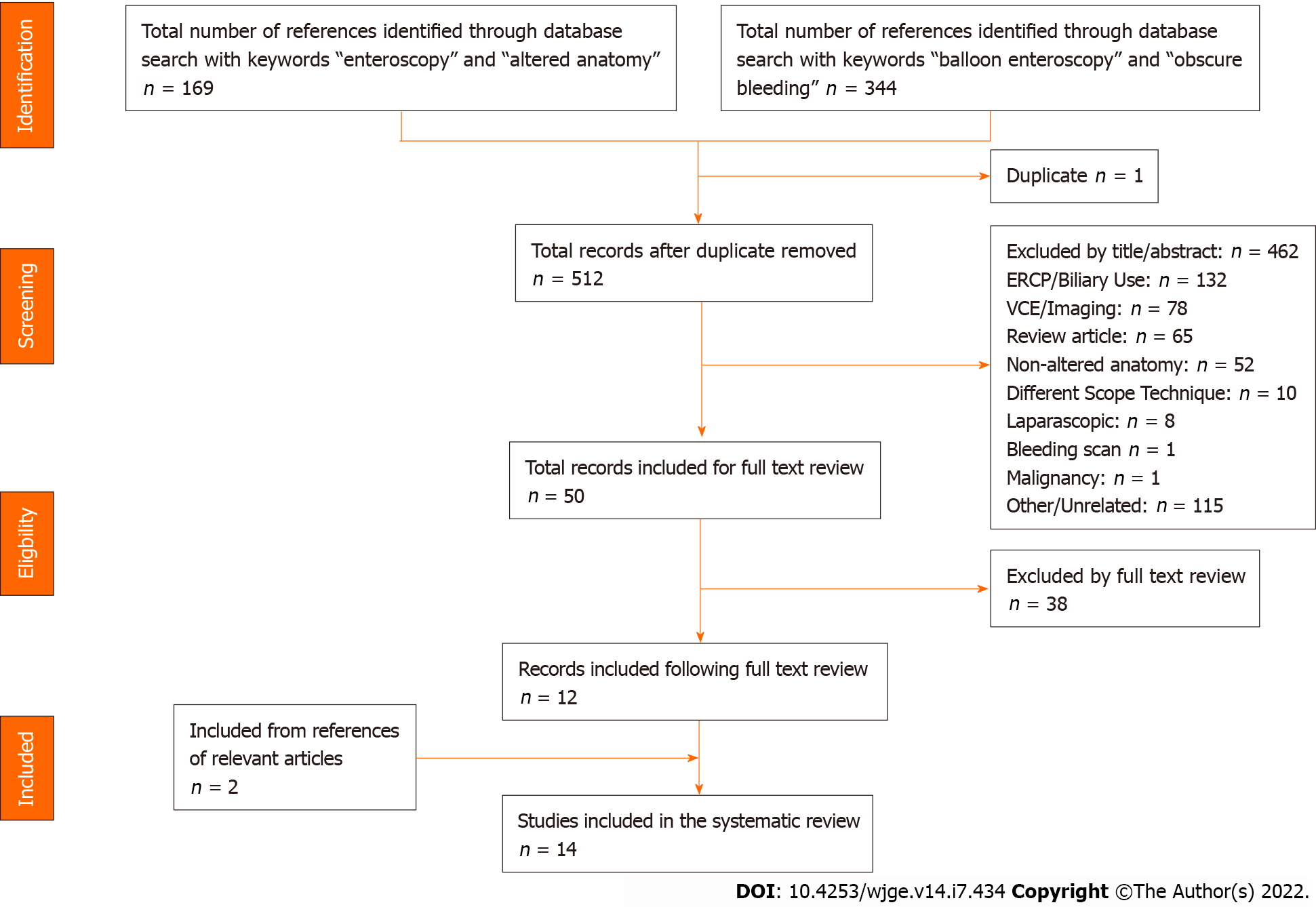
Data for this review was identified and performed by two independent reviewers (MA, TC) with consensus to avoid bias. Discrepancies and the decision over whether to include or exclude a study were resolved by means of discussion with consensus to avoid bias. Searches were done on PubMed, Google Scholar, Scopus, and Embase. All relevant articles were carefully reviewed with a review of each article’s references as well. Terms used for the search included “enteroscopy,” “obscure bleeding,” “gastrointestinal bleeding,” and “altered anatomy.” The literature search was performed in December 2021. Study types included in the review were prospective and retrospective reviews, case series, and case reports. Reference lists from these articles were also reviewed to find pertinent articles. Inclusion criteria for our systematic review included studies that were subjected to peer review and had available text in English. Only studies accessible through the search engines listed above were included in our review. Solitary abstract reports were excluded from our study in addition to any studies performed on animals. Studies that were not subject to peer review or were of pediatric focus (< 18 years) were also excluded from the study. A specific PRISMA flow diagram is included in Figure 1 to summarize our search methods. A further literature search was conducted with the reference citation analysis (RCA) engine, an artificial intelligence technology-based open multidisciplinary citation analysis database (https://www.referencecitationanalysis.com). This database was implemented to ensure the latest high impact articles were included in our study. Following a search of “balloon enteroscopy” within the RCA database no further studies were identified that fit our inclusion criteria.
Data from each study were extracted into an excel file in a systematic fashion. Extracted data included type of study, type of procedure, and type of altered anatomy, as well as the number of patients with any diagnostic findings or therapeutic intervention. Data were also recorded on procedure tolerance and complications. Due to the lack of controlled trials, retrospective and prospective observational studies were also included, as were case reports. We considered all clinical studies or reports that had been published until December 2019. As the current work only involved previously performed studies, approval by the Institutional Review Board or individual patient consent was deemed unnecessary.
Statistical analysis in the form of descriptive statistics was reported from each study. This data was organized and included in a structured table (Table 1).
| Cases (n-patients) | Anatomy | Device | Study type | Yield | Complications | Ref. |
| 17 (12) | 8 GBR, 6 PSW, 2 OLTR, 1 GJR | DBE | Retrospective | 15/17 diagnostic; 14/17 therapeutic | 1/17 perforation | [7] |
| 3 (3) | Not specified | TTS-BAE | Retrospective | 1/3 diagnostic; 1/3 therapeutic | None | [8] |
| 3 (3) | 1 OLTR, 1 Ileal-sigmoid anastomosis, 1 right hemicolectomy with ileostomy | DBE | Retrospective | 3/3 diagnostic; 0/3 therapeutic | 3/3 perforation | [9] |
| 15 (15) | Not specified | SBE | Retrospective | 8/15 diagnostic; 5/15 therapeutic | None | [10] |
| 3 (1) | Most OLTR | DBE | Retrospective | 3/3 diagnostic; 1/3 therapeutic | None | [11] |
| 5 (5) | Not specified | DBE | Retrospective | 5/5 diagnostic; 5/5 therapeutic | None | [12] |
| 9 (9) | Not specified | DBE | Prospective | Does not specify | 1/9 perforation | [13] |
| 3 (3) | 3 GBR | DBE | Prospective | 3/3 diagnostic; 3/3 therapeutic | None | [14] |
| 5 (5) | 2 HJ, 1 PSW, 1 GBR, 1 right hemihepatectomy w/RYHJ | 3 DBE 2 SBE | Case Series | 5/5 diagnostic; 5/5 therapeutic | None | [15] |
| 1 (1) | OLTR | SBE | Case Report | 1/1 diagnostic; 1/1 therapeutic | None | [16] |
| 1 (1) | HJ | SBE | Case Report | 1/1 diagnostic; 1/1 therapeutic | None | [17] |
| 1 (1) | Whipple | DBE | Case Report | 1/1 diagnostic; 1/1 therapeutic | None | [18] |
| 1 (1) | GBR | SBE | Case Report | 1/1 diagnostic; 1/1 therapeutic | None | [19] |
| 1 (1) | OLT | SBE | Case Report | 1/1 diagnostic; 1/1 therapeutic | None | [20] |
Following the search of these databases, 14 studies in total were included in our review. Of these studies, 6 were retrospective studies[7-12], 2 were prospective studies[13,14], 1 was a case series[15], and the remaining 5 were case reports[16-20]. In total, there were 68 procedures performed with 61 unique patients that had undergone these procedures. All patients were above the age 17 years old at the time of procedure. Forty-four (65%) of the procedures were double balloon, 21 (31%) were single balloon, and 3 (4%) were classified as through the scope balloon assisted. There were a variety of altered anatomy types with the most common being Gastric bypass Roux-en-Y (GBR), Pylorus sparing Whipple (PSW), Orthotopic Liver Transplantation with Roux-en-Y (OLTR), and Gastrojejunostomy Roux-en-Y (GJR).
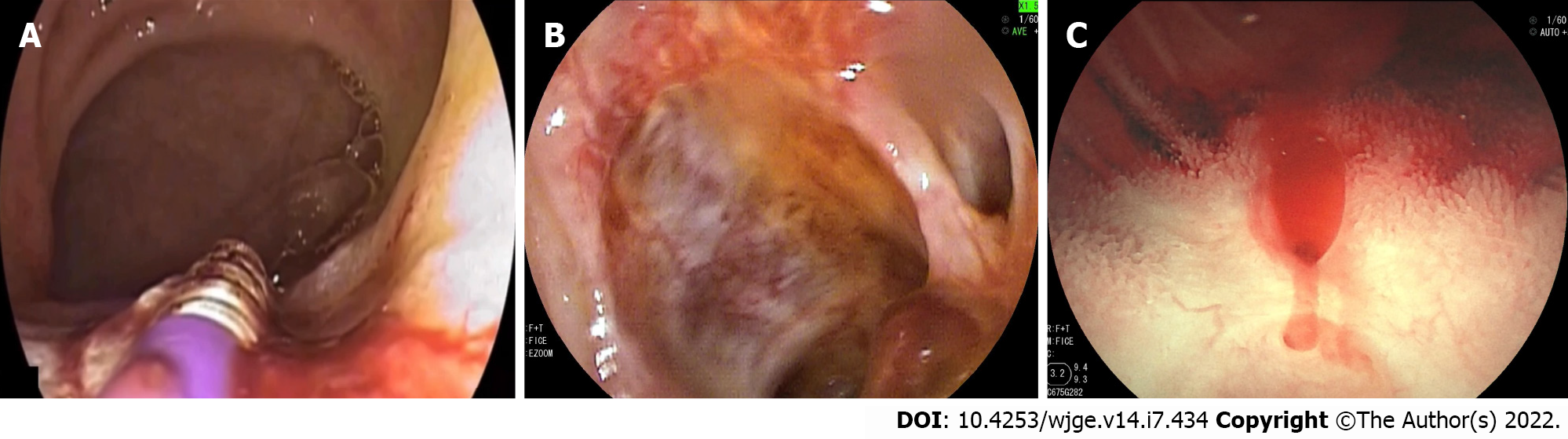
The procedures (SBE vs DBE) were performed in all patients; however, five (7%) procedures were complicated by perforation. There were no reported complications in the remaining 63 (93%) patients. Amongst the 5 reported procedure related perforations, 2 (40%) patients had a Roux-en-Y. The remaining 3 patients consisted of an ileal-sigmoid anastomosis, a right hemicolectomy with ileostomy, and an unspecified altered anatomy type. From the available data in each study, there was an overall diagnostic yield of 48/59 (81%) and a therapeutic yield of 39/59 (66%). Common diagnostic findings included ulcers (Figure 2A), arteriovenous malformations, angioectasia, anastomotic site bleeding (Figure 2B), and other post-surgical bleeding (Figure 2C). Therapeutic interventions consisted of argon plasma coagulation (APC), endoscopic clip placement, epinephrine injection, and N-butyl-2-cyanoacrylate (Histoacryl) injection. There was 1 patient who was recommended surgical revision of their altered anatomy following enteroscopy.
Obscure GI bleeding accounts for 5% of all GI bleeds with the culprit most often being small bowel origin[21]. Balloon enteroscopy has been implemented to assess for obscure GI bleeding and can be performed through different approaches. SBE utilizes an enteroscope (200 cm in length) with an overtube (140 cm in length) and balloon inflation device. DBE on the other hand has the same enteroscope and overtube but consists of two balloons: one at the tip of the enteroscope and the other acting as an anchoring leverage on the distal part of the overtube. These procedures can be performed anterograde (through the mouth) or retrograde (through the anus)[21].
Despite the differences in the devices, the techniques for these procedures are similar. The overtube is backloaded on the enteroscope after which the enteroscope is advanced deeply into the small intestine. Anchoring of the endoscope is secured by the balloon tip on the enteroscope in DBE vs the flexible tip with no balloon assisted anchoring in SBE. The overtube with its deflated balloon is advanced all the way to the distal tip of the enteroscope. Once the overtube has reached the distal end of the enteroscope, a stepwise pattern of inflation and deflation of the single vs double balloon apparatus is used to assist enteroscope transit in visualizing the area of small bowel[21,22].
The SBE model frequently utilized is the Olympus SIF-Q180 with an outer diameter of 13.2 mm, inner diameter of 11 mm, and balloon diameter of 40mm. DBE models are developed by Fujinon and consist of the EN-450T5, EN-450PS/20, and the EC-450BI5 with outer diameter ranging from 12.2-13.2 mm, inner diameter ranging from 10-10.8 mm, and balloon diameter being 40 mm[23].
Obscure GI bleeding has been estimated to account for 5%-10% of all GI bleeding, with increasing number of patients requiring balloon enteroscopy for small bowel evaluation[24]. The diagnostic yield of balloon enteroscopy amongst those without altered anatomy has been reported around 45%-55%[21,25]. Adverse rates are overall low at 3.2% with most common complications including intestinal bleeding, perforation, or post-procedure pancreatitis[26,27]. With the emerging surgical techniques for various GI pathologies, surgically altered GI anatomy remains prevalent. The obesity epidemic in the United States has led to increased referrals to bariatric surgeries. Additionally, the advancements in liver transplant (LT) have led to increasing number of patients receiving LT over the past several years[28]. Given their surgically altered GI anatomy, these patients remain at risk for GI bleeding. Furthermore, the management of these patients may be complicated by surgical anastomotic sites often serving as culprits of obscure GI bleeding[7,17,18]. These patients may require work up leading to SBE or DBE for underlying diagnosis.
Besides a substantial diagnostic yield, therapeutic interventions can be effectively achieved using the enteroscope channel. Balloon enteroscopy allows the endoscopist to safely deploy and advance ablation catheters, injection needles, and mechanical or hemostatic clips. These devices can even be modified to deliver Hemospray®. According to our literature, perforation remains the most frequently reported complication following balloon enteroscopy in those with altered anatomy. Post-surgical small bowel adhesions are prone to tearing during enteroscopy which can lead to perforation. Overall perforation rates in enteroscopy amongst those with both unaltered and altered anatomy from meta-analysis data have been reported to be as low as 0.24%[10,29,30]. Colonoscopy and upper endoscopy on the other hand have perforation rates as low as 0.1%[31]. From the available literature in this review, perforation rates were as high as 7% in those with surgically altered anatomy requiring single or double balloon enteroscopy. Such risk should be considered by clinicians during procedure planning in this patient population. Notably, the presence of post-surgical adhesions and overtube maneuvering through tight bends can be potential factors leading to added complications. The use of fluoroscopy can aid in navigating the enteroscope in challenging situations.
GBR, PSW, OLTR, and GJR were the most reported altered anatomy types observed in our review. The various types of altered anatomy structures may have an impact on the underlying procedure regarding luminal passage and scope maneuvers. No trend was identified regarding an association between diagnostic or therapeutic yield with altered anatomy types. We observed that 20% of the perforations were seen in patients with a Roux-en-Y. Those with altered small bowel anatomy may be more prone to suffer procedure related complications; however, further work is needed to verify these findings.
When compared to previous systematic reviews of balloon assisted ERCP in those with surgically altered anatomy, our study has notable differences. Diagnostic yields have varied between 70%-90% with procedure success rates approaching 62%-93% amongst single or double balloon assisted ERCP[32-34]. These studies depicted overall adverse event rates between 4%-7% with perforations making up a minority of these complications[32-34]. Such variance from our study may stem from the purpose of procedure with balloon enteroscopy for obscure GI bleeding requiring a thorough investigation of the small bowel, whereas balloon assisted ERCP typically focuses on assessment and interventions within the biliary tree. Although both procedures can be technically challenging, underlying maneuvers and interventions can vary. The higher incidence of perforation rate in our study when compared to balloon assisted ERCP may be attributed to aspects related to altered anatomy including procedure time, more extended exploration of the small bowel, presence of underlying adhesions and different targeted therapeutic techniques. Further studies are needed to further characterize these differences.
We recognize that our study has limitations. Foremost, given the small number of relevant published literature on this topic, our review is limited by a small sample size within these 14 reports. The lack of extensive literature that fits our inclusion criteria highlights the need for further studies to continue to assess the role of balloon enteroscopy in surgically altered anatomy patients. Additionally, most of our accessed studies being retrospective in nature as well as inclusion of case reports without controlled studies limit the conclusions taken from our review. Given the limited availability of studies to fit our inclusion criteria, we included case reports which may have skewed our overall results given many having 100% diagnosis rates and 0% complication rates. Furthermore, we were unable to perform analysis based on the procedure approach (retrograde vs anterograde) given reporting variability amongst the studies. The variety of altered anatomy types and the variability in data reporting in each of these studies also places further limits on the generalizability of our findings.
Our systematic review indicates that the data on the clinical utility of balloon enteroscopy in the evaluation of small bowel bleeding remains limited in those with surgically altered anatomy. The compiled data from the available literature demonstrates that balloon enteroscopy represents a clinically useful diagnostic modality in identifying culprit lesions for this subset of patients with diagnostic and therapeutic yields as high as 83% and 64% respectively. However, precautions and appropriate selection of cases must be taken within this patient population with an incidence of perforation as high as 7%.
Obscure gastrointestinal (GI) bleeding is defined as persistent bleeding despite negative evaluation with both esophagogastroduodenoscopy and colonoscopy and is often secondary to small intestinal pathology. This form of GI bleeding has now become manageable with the introduction of single balloon enteroscopy or double balloon enteroscopy. Those with distorted anatomy may require thorough investigation of the upper GI tract during obscure GI bleeding, and balloon enteroscopy may be warranted.
Balloon enteroscopy can be warranted in instances of obscure GI bleeding in those with altered anatomy; however, literature remains limited on the overall diagnostic and therapeutic yields as well as the overall safety of these procedures in this patient population.
The primary aim of this systematic review was to assess the diagnostic and therapeutic efficacy of balloon enteroscopy for obscure GI bleeding in patients with surgically altered anatomy. The secondary aim was to investigate the safety of balloon enteroscopy in this patient population.
We performed an extensive literature search on PubMed, Google Scholar, Scopus, and Embase where relevant articles were carefully reviewed. Terms used for the search included “enteroscopy,” “obscure bleeding,” “gastrointestinal bleeding,” and “altered anatomy.” Further search with the Reference Citation Analysis database was conducted to ensure inclusion of the latest high impact articles. Prospective and retrospective reviews, case series, and case reports were all included. Data from each study that fit our inclusion criteria were extracted into an excel file in a systematic fashion. Statistical analysis in the form of descriptive statistics was reported from each study.
Following our literature search, 14 studies were included in our review. In total, there were 68 procedures performed with 61 unique patients that had undergone these procedures. From the available data in each study, there was an overall diagnostic yield of 48/59 (81%) and a therapeutic yield of 39/59 (66%). Five (7%) procedures were complicated by perforation.
Our systematic review shows that balloon enteroscopy can be implemented in obscure GI bleeding in those with altered anatomy. Diagnostic and therapeutic yields were as high as 83% and 64% respectively. Given the overall perforation of 7%, caution is warranted in such cases. Further literature is needed to expand upon our findings.
Balloon enteroscopy remains a viable option to investigate obscure GI bleeding in those with altered anatomy. Caution is warranted given the reported perforation rates; however, further studies are needed to add to the limited available literature.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gong N, China; Liu LP, China; Nakamura K, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 861] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 2. | Akyuz U, Akyuz F. Diagnostic and Therapeutic Capability of Double-Balloon Enteroscopy in Clinical Practice. Clin Endosc. 2016;49:157-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Saygili F, Saygili SM, Oztas E. Examining the whole bowel, double balloon enteroscopy: Indications, diagnostic yield and complications. World J Gastrointest Endosc. 2015;7:247-252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006;38:42-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 284] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 5. | Wang P, Wang Y, Dong Y, Guo J, Fu H, Li Z, Du Y. Outcomes and safety of double-balloon enteroscopy in small bowel diseases: a single-center experience of 1531 procedures. Surg Endosc. 2021;35:576-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Takano S, Fukasawa M, Shindo H, Takahashi E, Hirose S, Fukasawa Y, Kawakami S, Hayakawa H, Yokomichi H, Kadokura M, Sato T, Enomoto N. Risk factors for perforation during endoscopic retrograde cholangiopancreatography in post-reconstruction intestinal tract. World J Clin Cases. 2019;7:10-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Skinner M, Peter S, Wilcox CM, Mönkemüller K. Diagnostic and therapeutic utility of double-balloon enteroscopy for obscure GI bleeding in patients with surgically altered upper GI anatomy. Gastrointest Endosc. 2014;80:181-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Cai JX, Diehl DL, Kiesslich R, Storm AC, El Zein MH, Tieu AH, Hoffman A, Singh VK, Khashab MA, Okolo PI 3rd, Kumbhari V. A multicenter experience of through-the-scope balloon-assisted enteroscopy in surgically altered gastrointestinal anatomy. Surg Endosc. 2017;31:2753-2762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Gerson LB, Tokar J, Chiorean M, Lo S, Decker GA, Cave D, Bouhaidar D, Mishkin D, Dye C, Haluszka O, Leighton JA, Zfass A, Semrad C. Complications associated with double balloon enteroscopy at nine US centers. Clin Gastroenterol Hepatol. 2009;7:1177-1182, 1182.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 112] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 10. | Kurzynske FC, Romagnuolo J, Brock AS. Success of single-balloon enteroscopy in patients with surgically altered anatomy. Gastrointest Endosc. 2015;82:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Chua TJ, Kaffes AJ. Balloon-assisted enteroscopy in patients with surgically altered anatomy: a liver transplant center experience (with video). Gastrointest Endosc. 2012;76:887-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Shishido T, Oka S, Tanaka S, Imagawa H, Takemura Y, Yoshida S, Chayama K. Outcome of patients who have undergone total enteroscopy for obscure gastrointestinal bleeding. World J Gastroenterol. 2012;18:666-672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Patel MK, Horsley-Silva JL, Gómez V, Stauffer JA, Stark ME, Lukens FJ. Double balloon enteroscopy procedure in patients with surgically altered bowel anatomy: analysis of a large prospectively collected database. J Laparoendosc Adv Surg Tech A. 2013;23:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Cedrón Cheng HG, Chirinos Vega JA. [Single balloon enteroscopy in the management of small bowel pathology. Experience of the Small Bowel Unit - British American Hospital from December 2012 to December 2018]. Rev Gastroenterol Peru. 2019;39:27-37. [PubMed] |
| 15. | Gubler C, Glenck M, Pfammatter T, Bauerfeind P. Successful treatment of anastomotic jejunal varices with N-butyl-2-cyanoacrylate (Histoacryl): single-center experience. Endoscopy. 2012;44:776-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Curcio G, Sciveres M, Mocciaro F, Riva S, Spada M, Tarantino I, Barresi L, Traina M. Out-of-reach obscure bleeding: single-balloon enteroscopy to diagnose and treat varices in hepaticojejunostomy after pediatric liver transplant. Pediatr Transplant. 2012;16:E78-E80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Prachayakul V, Aswakul P, Kachintorn U. Bleeding hepaticojejunostomy anastomotic varices successfully treated with Histoacryl injection, using single-balloon enteroscopy. Endoscopy. 2011;43 Suppl 2 UCTN:E153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Neumann H, Mönkemüller K, Malfertheiner P. Obscure overt GI bleeding secondary to angiodysplasias at the hepaticojejunostomy diagnosed and successfully treated with double-balloon enteroscopy. Gastrointest Endosc. 2008;67:563-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Hakim S, Reddy SRR, Batke M, Polidori G, Cappell MS. Two case reports of acute upper gastrointestinal bleeding from duodenal ulcers after Roux-en-Y gastric bypass surgery: Endoscopic diagnosis and therapy by single balloon or push enteroscopy after missed diagnosis by standard esophagogastroduodenoscopy. World J Gastrointest Endosc. 2017;9:521-528. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Urgesi R, Riccioni ME, Nista EC, Lionetti R, Tisone G, Familiari P, Ricci R, Pelecca G, Angelico M, Costamagna G. Obscure gastrointestinal bleeding as first symptom of eosinophilic jejunitis in a liver transplant recipient: diagnosis and treatment with single balloon enteroscopy. BMJ Case Rep. 2010;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Gerson LB, Fidler JL, Cave DR, Leighton JA. ACG Clinical Guideline: Diagnosis and Management of Small Bowel Bleeding. Am J Gastroenterol. 2015;110:1265-87; quiz 1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 448] [Article Influence: 44.8] [Reference Citation Analysis (1)] |
| 22. | Sanchez‐Yague A. Middle gastrointestinal bleeding. Gastro Emerg. 20:230-238. [DOI] [Full Text] |
| 23. | Koornstra JJ, Fry L, Mönkemüller K. ERCP with the balloon-assisted enteroscopy technique: a systematic review. Dig Dis. 2008;26:324-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | ASGE Technology Committee; Chauhan SS, Manfredi MA, Abu Dayyeh BK, Enestvedt BK, Fujii-Lau LL, Komanduri S, Konda V, Maple JT, Murad FM, Pannala R, Thosani NC, Banerjee S. Enteroscopy. Gastrointest Endosc. 2015;82:975-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 25. | Tanaka S, Mitsui K, Yamada Y, Ehara A, Kobayashi T, Seo T, Tatsuguchi A, Fujimori S, Gudis K, Sakamoto C. Diagnostic yield of double-balloon endoscopy in patients with obscure GI bleeding. Gastrointest Endosc. 2008;68:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 26. | Teshima CW, Kuipers EJ, van Zanten SV, Mensink PB. Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: an updated meta-analysis. J Gastroenterol Hepatol. 2011;26:796-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 208] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 27. | Nakayama S, Tominaga K, Obayashi T, Okamoto J, Minamino H, Ominami M, Fukunaga S, Nagami Y, Sugimori S, Machida H, Okazaki H, Sogawa M, Yamagami H, Tanigawa T, Watanabe K, Watanabe T, Fujiwara Y, Arakawa T. The prevalence of adverse events associated with double-balloon enteroscopy from a single-centre dataset in Japan. Dig Liver Dis. 2014;46:706-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Otani K, Watanabe T, Shimada S, Hosomi S, Nagami Y, Tanaka F, Kamata N, Taira K, Yamagami H, Tanigawa T, Shiba M, Fujiwara Y. Clinical Utility of Capsule Endoscopy and Double-Balloon Enteroscopy in the Management of Obscure Gastrointestinal Bleeding. Digestion. 2018;97:52-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 29. | Xin L, Liao Z, Jiang YP, Li ZS. Indications, detectability, positive findings, total enteroscopy, and complications of diagnostic double-balloon endoscopy: a systematic review of data over the first decade of use. Gastrointest Endosc. 2011;74:563-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 189] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 30. | May A, Nachbar L, Pohl J, Ell C. Endoscopic interventions in the small bowel using double balloon enteroscopy: feasibility and limitations. Am J Gastroenterol. 2007;102:527-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 161] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 31. | Levy I, Gralnek IM. Complications of diagnostic colonoscopy, upper endoscopy, and enteroscopy. Best Pract Res Clin Gastroenterol. 2016;30:705-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 127] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 32. | Inamdar S, Slattery E, Sejpal DV, Miller LS, Pleskow DK, Berzin TM, Trindade AJ. Systematic review and meta-analysis of single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy. Gastrointest Endosc. 2015;82:9-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 33. | Tanisaka Y, Ryozawa S, Mizuide M, Araki R, Fujita A, Ogawa T, Tashima T, Noguchi T, Suzuki M, Katsuda H. Status of single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: Systematic review and meta-analysis on biliary interventions. Dig Endosc. 2021;33:1034-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 34. | Anvari S, Lee Y, Patro N, Soon MS, Doumouras AG, Hong D. Double-balloon enteroscopy for diagnostic and therapeutic ERCP in patients with surgically altered gastrointestinal anatomy: a systematic review and meta-analysis. Surg Endosc. 2021;35:18-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |