Published online Dec 16, 2022. doi: 10.4253/wjge.v14.i12.759
Peer-review started: October 11, 2022
First decision: October 26, 2022
Revised: November 1, 2022
Accepted: November 22, 2022
Article in press: November 22, 2022
Published online: December 16, 2022
Processing time: 63 Days and 16.6 Hours
Current guidelines recommend colonoscopy within 24 h for acute lower gastr
To investigate the effectiveness of early colonoscopy on the length of hospital stay for CDH patients.
We conducted a single-center retrospective cohort study. Patients who underwent colonoscopy within 24 h of presentation (early group) were compared with those who underwent colonoscopy beyond 24 h of presentation (elective group). The primary outcome was the length of hospital stay, and secondary outcomes were the identification of stigmata of recent hemorrhage (SRH), rebleeding, red blood cell transfusion more than 4 units, and interventional radiology and abdominal surgery after colonoscopy.
We identified 574 CDH cases. Patients were divided into the early (n = 328) and elective (n = 226) groups. After propensity score matching, 191 pairs were generated. The length of hospital stay did not significantly differ between the two groups (early group vs elective group; median, 7 vs 8 d; P = 0.10). The early group had a significantly high identification of SRH (risk difference, 11.6%; 95%CI: 2.7 to 20.3; P = 0.02). No significant differences were found in the rebleeding (risk difference, 4.7%; 95%CI: -4.1 to 13.5; P = 0.35), red blood cell transfusion more than 4 units (risk difference, 1.6%; 95%CI: -7.5 to 10.6; P = 0.82), and interventional radiology and abdominal surgery rate after colonoscopy (risk difference, 0.5%; 95%CI: -2.2 to 3.2; P = 1.00).
Early colonoscopy within 24 h, on arrival for CDH, could not improve the length of hospital stay.
Core Tip: Current guidelines recommend colonoscopy within 24 h for acute lower gastrointestinal bleeding; however, the evidence in support for colonic diverticular hemorrhage (CDH) indications remains insufficient. We investigate the effectiveness of early colonoscopy on the length of hospital stay for CDH. The purpose of the study was to compare the length of hospital stay for CDH by dividing patients into two groups: An early group who underwent colonoscopy within 24 h and an elective group who underwent colonoscopy beyond 24 h and analysis was performed using propensity score matching. Early colonoscopy did not improve the length of hospital stay.
- Citation: Ichita C, Shimizu S, Sasaki A, Sumida C, Nishino T, Kimura K. Effectiveness of early colonoscopy in patients with colonic diverticular hemorrhage: A single-center retrospective cohort study. World J Gastrointest Endosc 2022; 14(12): 759-768
- URL: https://www.wjgnet.com/1948-5190/full/v14/i12/759.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i12.759
Among cases of acute lower gastrointestinal bleeding (ALGIB), colonic diverticular hemorrhage (CDH) is the most common, accounting for more than 60% of cases[1,2]. The clinical presentation of diverticular hemorrhage is usually hematochezia without fever or abdominal pain[3], and the diagnosis can be made with computed tomography (CT) findings, but colonoscopy is recommended for a definitive diagnosis[4,5].
Although various studies, including randomized controlled trials (RCTs)[6-9], have shown that current guidelines recommend colonoscopy within 24 h for ALGIB[2,4,5], no clear evidence has been established for CDH alone. The percentage of spontaneous hemostasis for CDH was as high as 60%-90%[2,10-12], while the prevalence of rebleeding was reported to be as high as 13%-48%[13]. Even if the source of bleeding is identified by early colonoscopy, it is unclear whether early colonoscopy reduces hospital stay.
Emergency colonoscopy is often difficult to perform because of colon preparation and personnel availability for the procedure. The purpose of this study was to determine whether early colonoscopy for diverticular hemorrhage improves hospital stay.
This was a single-center, retrospective cohort study.
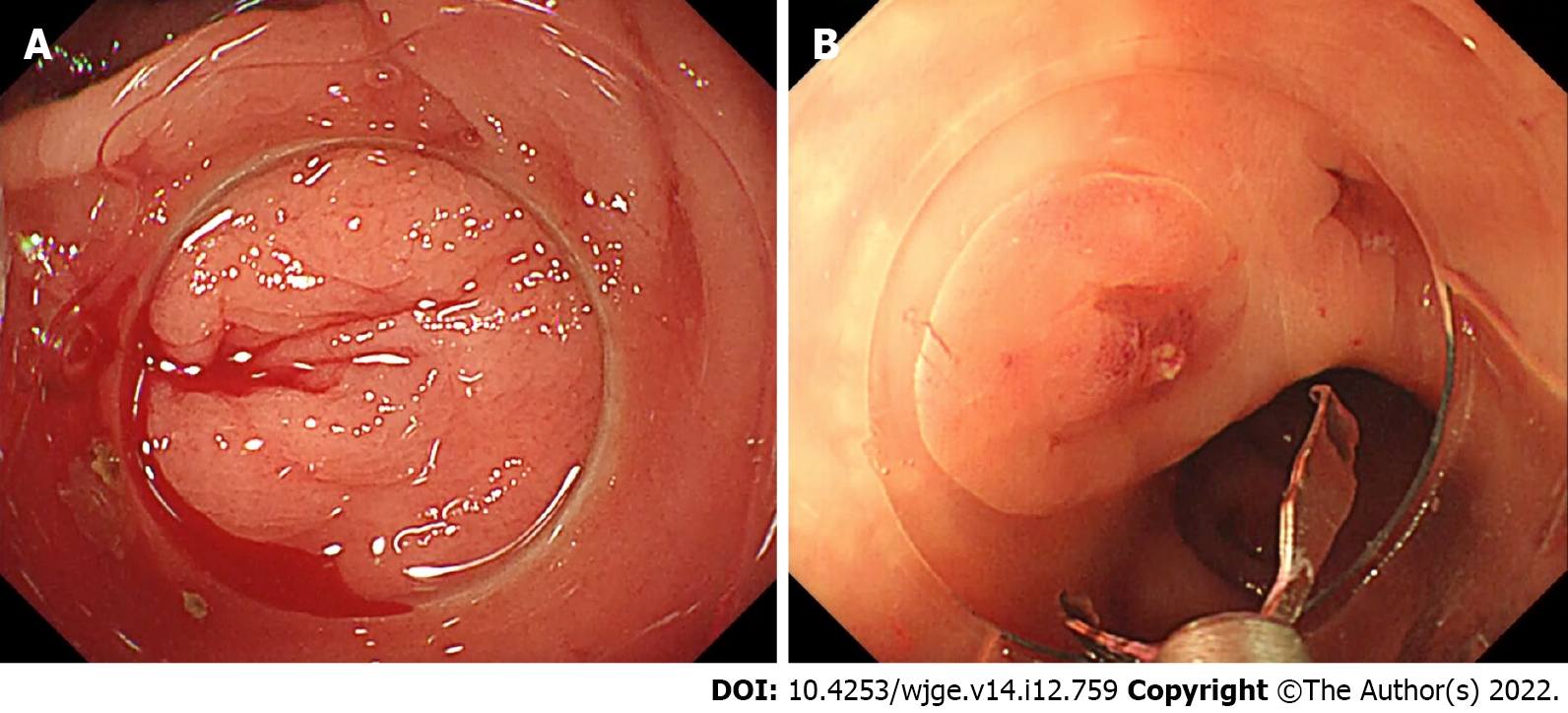
We included patients who presented to Shonan Kamakura General Hospital with hematochezia and underwent colonoscopy with a diagnosis of diverticular hemorrhage over a 5-year period from January 2017 to December 2021. Colonic diverticular hemorrhage was defined as 1) When the stigmata of recent hemorrhage (SRH) were found in the diverticulum[14] (Figures 1 and 2) When the colonoscopic findings ruled out diseases other than CDH.
Patients were divided into early and elective groups. The early group was defined as patients who underwent colonoscopy within 24 h of arrival and the elective group was defined as patients who underwent colonoscopy beyond 24 h of arrival.
Patients who underwent interventional radiology (IVR) or abdominal surgery prior to colonoscopy were excluded. Patients for which variables could not be obtained, such as time from visit to colonoscopy, were also excluded. Patients who presented without hemorrhagic shock but developed hemorrhagic shock during follow-up and were allocated to the early colonoscopy group were excluded because they were allocated to the early colonoscopy group due to deterioration of their condition, which may have disadvantaged the early group.
Variables included age, sex, body mass index, smoking history, Eastern Cooperative Oncology Group performance status (PS) over 3[15], comorbidities (hypertension, diabetes mellites, coronary artery disease, chronic kidney disease, hemodialysis), and the use of medications (antithrombotics and non-steroidal anti-inflammatory drugs, shock vitality at presentation, contrast CT findings, and blood sampling data (hemoglobin under 10 g/dL and platelet under 10000 /μL). Body mass index was categorized as underweight (< 18.5), normal weight (18.5-24.9), overweight (25-29.9), and obese (≥ 30). Smoking history was categorized as current, past, never, or no information. PS was determined by the condition of the patient at the time of the visit. Comorbidities were ascertained from the patient's medical history and medications at the time of presentation, and creatinine over 1.5 mg/dL was defined as chronic kidney disease. Antithrombotics use was defined as the prescription of aspirin, thi
The primary outcome was the length of hospital stay. Secondary outcomes included the identification percentage of SRH[14], rebleeding, red blood cell transfusion more than 4 units, and the IVR and abdominal surgery after colonoscopy. IVR and abdominal surgery were defined as those performed to control diverticular bleeding or to control colonoscopy-related complications. The observation period for the outcome was during hospitalization.
We performed a propensity score matching analysis between the early and elective groups. This method can minimize the effect of selection bias and imbalances in patient backgrounds between the groups[17]. We estimated propensity scores with a logistic regression using early colonoscopy as a dependent variable and all covariates as independent variables. A one-to-one propensity score matching was performed utilizing the nearest neighbor method without replacement. The caliper width was set at 20% of the standard deviation of the propensity scores on the logit scale. Balances in baseline variables using standardized mean differences were also examined and values of < 0.1 were considered balanced[17].
In addition, two analyses were performed as sensitivity analyses. First, we performed an analysis in which the time to exposure was changed. The group with a time from visit to a colonoscopy of fewer than 12 h was defined as the early group (< 12 h), and the group with a time of 12 h or more was defined as the elective group (≥ 12 h). Propensity score matching was used for analysis in the same approach as in the main analysis. Second, we performed a multivariate analysis using the same covariates. We performed multivariable linear regression analyses for the length of hospital stay and performed multivariable logistic regression analyses for the identification of SRH, rebleeding, red blood cell transfusions more than 4 units, and IVR and abdominal surgery after colonoscopy.
Continuous variables are reported using medians and interquartile ranges, and categorical variables are reported using numbers and percentages. Continuous variables were compared using Mann-Whitney U tests and categorical variables were compared using chi-square tests. The risk difference with 95% confidence intervals (CI) was calculated for binary outcomes. We also calculated odds ratios (ORs) and their 95%CIs in the multivariable analysis. The two-sided significance level for all tests was P < 0.05. All analyses were performed using EZR version 1.55[18], a package for R statistical software (https://www.r-project.org/). More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics.
All procedures were performed in accordance with the ethical standards established in the 1964 Declaration of Helsinki and its later amendments. The study was reviewed and approved by the institutional review board of the Future Medical Research Center Ethical Committee (IRB No. TGE01304-024). Due to the observational study based on medical records without using samples taken from the human body, informed consent was obtained from all participants through the opt-out method on our hospital website.
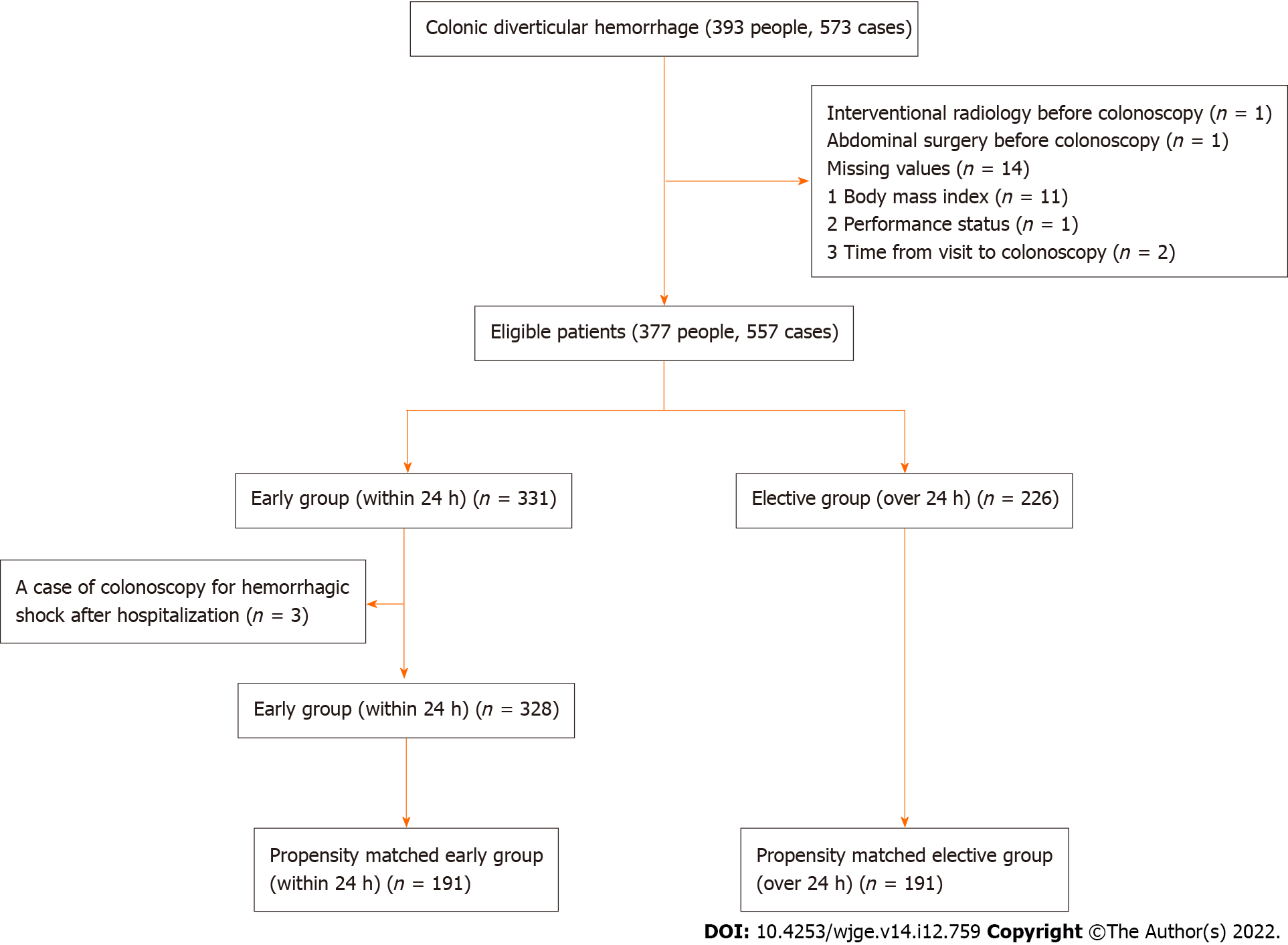
During the study period, 573 CDH cases were identified. After applying the defined exclusion criteria, 557 cases were included in the present study. The patients were divided into the early (n = 328) and elective (n = 226) groups. One-to-one propensity score matching created 191 pairs of patients (Figure 2).
Baseline characteristics of eligible patients before and after propensity score matching are provided in Table 1. Before propensity score matching, sex, smoking history, shock vitals at presentation, and contrast CT findings were unbalanced, especially contrast CT findings were highly unbalanced. After propensity score matching, the baseline characteristics of both groups were nearly balanced.
| Before propensity score matching | After propensity score matching | |||||
| Early group (< 24 h) | Elective group (≥ 24 h) | SMD | Early group (< 24 h) | Elective group (≥ 24 h) | SMD | |
| Variables | n = 328 | n = 226 | n = 191 | n = 191 | ||
| Age, yr, median (IQR) | 79.0 (71.0–84.0) | 79.0 (72.3–84.0) | 0.047 | 78.0 (70.0–84.0) | 79.0 (71.5–84.0) | 0.057 |
| Male, n (%) | 220 (67.1) | 135 (59.7) | 0.153 | 132 (69.1) | 126 (66.0) | 0.067 |
| Body mass index, n (%) | 0.087 | 0.094 | ||||
| < 18.5 | 46 (14.0) | 18 (8.0) | 15 (7.9) | 18 (9.4) | ||
| 18.5-24.9 | 210 (64.0) | 153 (67.7) | 124 (64.9) | 128 (67.0) | ||
| 25-29.9 | 76 (23.2) | 76 (23.2) | 45 (23.6) | 39 (20.4) | ||
| ≥ 30 | 12 (3.7) | 9 (4.0) | 3 (1.6) | 4 (2.1) | ||
| Smoking | 0.162 | 0.075 | ||||
| Current, n (%) | 45 (13.7) | 25 (11.1) | 23 (12.0) | 24 (12.6) | ||
| Past, n (%) | 104 (31.7) | 64 (28.3) | 64 (33.5) | 58 (30.4) | ||
| Never, n (%) | 169 (51.5) | 133 (58.8) | 101 (52.9) | 105 (55.0) | ||
| No information, n (%) | 10 (3.0) | 4 (1.8) | 3 (1.6) | 4 (2.1) | ||
| Performance status ≥ 3, n (%) | 34 (10.4) | 20 (8.8) | 0.051 | 15 (7.9) | 20 (10.5) | 0.091 |
| Comorbidities | ||||||
| Hypertension, n (%) | 210 (64.0) | 152 (67.3) | 0.051 | 124 (64.9) | 122 (63.9) | 0.022 |
| Diabetes mellitus, n (%) | 67 (20.4) | 51 (22.6) | 0.052 | 41 (21.5) | 37 (19.4) | 0.052 |
| Coronary artery disease, n (%) | 92 (28.0) | 67 (29.6) | 0.035 | 63 (33.0) | 57 (29.8) | 0.068 |
| Chronic kidney disease, n (%) | 33 (10.1) | 28 (12.4) | 0.074 | 22 (11.5) | 25 (13.1) | 0.048 |
| Hemodialysis, n (%) | 2 (0.6) | 5 (2.2) | 0.136 | 2 (1.0) | 4 (2.1) | 0.084 |
| Medication | ||||||
| Antithrombotics, n (%) | 123 (37.5) | 80 (35.4) | 0.044 | 79 (41.4) | 68 (35.6) | 0.119 |
| NSAIDs, n (%) | 14 (4.3) | 14 (6.2) | 0.087 | 8 (4.2) | 9 (4.7) | 0.025 |
| Shock vitality at presentation, n (%) | 28 (8.5) | 12 (5.3) | 0.127 | 9 (4.7) | 12 (6.3) | 0.069 |
| Contrast CT findings | 0.811 | 0.027 | ||||
| With an extravascular leak, n (%) | 129 (39.3) | 17 (7.5) | 17 (8.9) | 17 (8.9) | ||
| Without an extravascular leak, n (%) | 159 (48.5) | 170 (75.2) | 138 (72.3) | 140 (73.3) | ||
| Without contrast CT, n (%) | 40 (12.2) | 39 (17.3) | 36 (18.8) | 34 (17.8) | ||
| Blood sampling data | ||||||
| Hemoglobin < 10 g/dL, n (%) | 84 (25.6) | 61 (27.0) | 0.031 | 54 (28.3) | 51 (26.7) | 0.035 |
| Platelet < 10000 /μL, n (%) | 4 (1.2) | 3 (1.3) | 0.01 | 2 (1.0) | 2 (1.0) | < 0.001 |
Table 2 shows outcomes after propensity score matching. Length of hospital stay did not significantly differ between the two groups (early group vs elective group; median, 7 vs 8 d; P = 0.10). Among the secondary outcomes, the identification percentage of SRH was significantly higher in the early group (32.5% in the early group vs 20.9% in the elective group; risk difference, 11.6%; 95%CI: 2.7 to 20.3; P = 0.02). The rebleeding (28.8% vs 24.1%, respectively; risk difference, 4.7%; 95%CI: -4.1 to 13.5; P = 0.35), red blood cell transfusions more than 4 units (29.3% vs 27.7%, respectively; risk difference, 1.6%; 95%CI: -7.5 to 10.6; P = 0.82), and IVR and abdominal surgery after colonoscopy (2.1% vs 1.6%, respectively; risk difference, 0.5%; 95%CI: -2.2 to 3.2; P = 1.00) were not significantly different between the two groups. The results of the sensitivity analysis adopted 12 h as the exposure time, which was similar to those of the main analysis, however, the identification of SRH was different from that of the main analysis, and the superiority of early colonoscopy could not be demonstrated (Table 3). Sensitivity analyses with multivariate analysis showed similar results to the main analysis (Table 4).
| Outcomes | Early group (< 24 h) | Elective group (≥ 24 h) | Difference (95%CI) | P value |
| Primary outcome | ||||
| Length of hospital stay, days, median (IQR) | 7 (7–9) | 8 (7– 9.5) | 0.10 | |
| Secondary outcomes | ||||
| Identification of stigmata of recent hemorrhage (%) | 32.5 (62/191) | 20.9 (40/191) | 11.6 (2.7 to 20.3) | 0.02 |
| Rebleeding (%) | 28.8 (55/191) | 24.1 (46/191) | 4.7 (-4.1 to 13.5) | 0.35 |
| Red blood cell transfusion ≥ 4 units (%) | 29.3 (56/191) | 27.7 (53/191) | 1.6 (-7.5 to 10.6) | 0.82 |
| Interventional radiology and abdominal surgery (%) | 2.1 (4/191) | 1.6 (3/191) | 0.5 (-2.2 to 3.2) | 1.00 |
| Outcomes | Early group (< 12 h) | Elective group (≥ 12 h) | Difference (95%CI) | P value |
| Primary outcome | ||||
| Length of hospital stay, median (IQR) | 7 (6–9) | 8 (7– 9) | 0.09 | |
| Secondary outcomes | ||||
| Identification of stigmata of recent hemorrhage (%) | 40.8 (51/125) | 33.6 (42/125) | 7.2 (-4.7 to 19.1) | 0.30 |
| Rebleeding (%) | 37.6 (47/125) | 25.6 (32/125) | 12.0 (0.6 to 23.4) | 0.06 |
| Red blood cell transfusion ≥ 4 units (%) | 30.4 (38/125) | 28.8 (36/125) | 1.6 (-9.7 to 12.9) | 0.89 |
| Interventional radiology and abdominal surgery (%) | 2.4 (3/125) | 3.2 (4/125) | -0.8 (-4.9 to 3.3) | 0.74 |
| Primary outcome | Coefficient (95%CI) | P value |
| Length of hospital stay | 0.08 (-0.71 to 0.87) | 0.84 |
| Secondary outcomes | Odds ratio (95%CI) | P value |
| Identification of stigmata of recent hemorrhage | 1.76 (1.14–2.70) | 0.01 |
| Rebleeding | 1.21 (0.78–1.86) | 0.39 |
| Red blood cell transfusion ≥ 4 units | 0.91 (0.55–1.50) | 0.71 |
| Interventional radiology and abdominal surgery | 0.93 (0.23–3.78) | 0.92 |
The results of this study showed no significant difference in the length of hospital stay between early colonoscopy within 24 h and elective colonoscopy. Sensitivity analyses also showed similar results, indicating the robustness of the results. In contrast, the identification percentage of SRH, although a sensitivity analysis adopting an exposure time of 12 h did not show any advantage, was significantly higher in the early group. However, early colonoscopy did not indicate significant differences in rebleeding, red blood cell transfusion more than 4 units, and IVR and abdominal surgery after colonoscopy.
The randomized control trial (RCT) investigating the benefit of early colonoscopy, which currently has the most robust evidence, is a multicenter study published in 2020[9]. In this RCT, they found an increased identification percentage of SRH in the early group, but no significant difference in the rebleeding or length of hospital stay. Similar to our study, they were unable to demonstrate the benefit of early colonoscopy within 24 h. Although we did not recognize any RCTs that investigated the usefulness of early colonoscopy for CDH because definitive diagnosis is difficult to make before colonoscopy, we did recognize a large, receipt-based observational study in the United States (n = 20,100)[19]. In this United States study, early colonoscopy within 24 h also increased rebleeding and readmission. Some of the results indicated a disadvantage of early colonoscopy. There may be several reasons for this result. In case of the receipt database study: (1) It was difficult to obtain important information such as imaging information; (2) It did not ensure accurate diagnosis; and (3) It was difficult to obtain information on an hourly scale. In the present study: (1) Although various confounding factors can be compensated for with surrogate markers, confounding factors such as extravascular leakage findings on contrast CT could not be adequately addressed, which was important in this study; and (2) The accuracy of the diagnosis itself is likely to be unclear for diseases for which validation studies are insufficient. In such cases, the diagnosis may be incorrect if factors other than ICD-10 codes are not used appropriately. The Receipt Database Study can provide data on a daily scale, but it is difficult to provide data on an hourly scale. If the procedure was performed on the same day of admission, the range would be from 0 to 47 h, depending on the time at which the patient was admitted to the hospital. Few studies have evaluated the appropriate colonoscopy time for CDH. Although the present study was an observational study conducted at a single institution, the covariates were appropriately selected and adjusted, and robustness was demonstrated in the sensitivity analysis.
A possible reason for a prolonged length of hospital stay despite the identification of the source of bleeding in our study is the high rebleeding. Table 5 shows the hemostatic methods used in endoscopic hemostasis at the time of the main analysis of this study. In this study, the most common method of hemostasis in both the early and elective groups was the zipper clipping method. As shown in Table 6, the rebleeding of the zipper clipping method was considerably higher than that of other hemostatic techniques. In contrast, the direct clipping method and endoscopic band ligation (EBL) method have a significantly lower rebleeding (direct clipping method vs zippier clipping method vs EBL method; 9.3% vs 45.1% vs 10.3%). Especially for the EBL method, its low rebleeding and safety have been reported in recent years[20-24]. The general adoption of these hemostatic methods could improve rebleeding and shorten hospital stays. The number of EBL method cases in this study was inadequate because we adopted the EBL method in 2020. Further studies will be conducted in the future.
| Hemostatic method | Early group (< 24 h) | Elective group (≥ 24 h) | P value |
| Direct clipping method, n (%) | 17/60 (28.3) | 9/40 (22.5) | 0.794 |
| Zipper clipping, method, n (%) | 30/60 (50.0) | 21/40 (52.5) | |
| Endoscopic band ligation method, n (%) | 13/60 (21.7) | 10/40 (25.0) |
| Hemostatic method | Direct clipping method (n = 43) | Zipper clipping method (n = 82) | Endoscopic band ligation method (n = 47) |
| Rebleeding | 4 (9.3) | 37 (45.1) | 5 (10.6) |
There are several limitations associated with our study that should be noted. First, this is a single-center study, and generalizability to outside institutions is insufficient. Second, the localization of diverticula and the frequency of CDH are different among racial groups. It is unclear whether the Asian data can be applied to other races[25-28]. Third, the benefits of colonoscopy for CDH are not only potential in terms of reduced hospital stay associated with the colonoscopic hemostasis, but also an important factor in confirming the diagnosis. It should be noted that this study did not consider the benefits of the diagnostic factor.
Finally, this study focused on the time period from hospital visit to colonoscopy, not from the onset of hematochezia to colonoscopy. Therefore, the time period from the onset of hematochezia to colonoscopy may have differed from the actual time.
In conclusion, our study showed that early colonoscopy within 24 h did not improve the length of hospital stay for CDH. Early colonoscopy may not be necessary for all cases of CDH.
Appropriate timing of colonoscopy for colonic diverticular hemorrhage is not well evidenced.
The motivation for this study is to investigate whether within 24 h is an appropriate timing for colonoscopy for colonic diverticular hemorrhage.
We aimed to compare the length of hospital stay for colonoscopy for colonic diverticular hemorrhage by dividing patients into two groups: early groups (within 24 h) and elective colonoscopy (after 24 h).
A single-center retrospective study over 5 years compared the two groups using propensity score matching.
Early colonoscopy within 24 h did not significantly improve hospital stay.
Early colonoscopy within 24 h for colonic diverticular hemorrhage may not improve length of hospital stay.
Further research is needed to determine which patients really need early colonoscopy.
We would like to express our gratitude to the Gastroenterology Medicine Center, the Emergency Department, and the Surgery Department of Shonan Kamakura General Hospital, who were involved in the patient care.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fusaroli P, Italy; Teramoto-Matsubara OT, Mexico S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Nagata N, Kobayashi K, Yamauchi A, Yamada A, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Kishino T, Ishii N, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Funabiki T, Kinjo Y, Mizuki A, Kiyotoki S, Mikami T, Gushima R, Fujii H, Fuyuno Y, Gunji N, Toya Y, Narimatsu K, Manabe N, Nagaike K, Kinjo T, Sumida Y, Funakoshi S, Kawagishi K, Matsuhashi T, Komaki Y, Miki K, Watanabe K, Fukuzawa M, Itoi T, Uemura N, Kawai T, Kaise M. Identifying Bleeding Etiologies by Endoscopy Affected Outcomes in 10,342 Cases With Hematochezia: CODE BLUE-J Study. Am J Gastroenterol. 2021;116:2222-2234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | ASGE Standards of Practice Committee. Pasha SF, Shergill A, Acosta RD, Chandrasekhara V, Chathadi KV, Early D, Evans JA, Fisher D, Fonkalsrud L, Hwang JH, Khashab MA, Lightdale JR, Muthusamy VR, Saltzman JR, Cash BD. The role of endoscopy in the patient with lower GI bleeding. Gastrointest Endosc. 2014;79:875-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 144] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 3. | Wilkins T, Baird C, Pearson AN, Schade RR. Diverticular bleeding. Am Fam Physician. 2009;80:977-983. [PubMed] |
| 4. | Strate LL, Gralnek IM. ACG Clinical Guideline: Management of Patients With Acute Lower Gastrointestinal Bleeding. Am J Gastroenterol. 2016;111:459-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 300] [Article Influence: 33.3] [Reference Citation Analysis (2)] |
| 5. | Nagata N, Ishii N, Manabe N, Tomizawa K, Urita Y, Funabiki T, Fujimori S, Kaise M. Guidelines for Colonic Diverticular Bleeding and Colonic Diverticulitis: Japan Gastroenterological Association. Digestion. 2019;99 Suppl 1:1-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 130] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 6. | van Rongen I, Thomassen BJW, Perk LE. Early Versus Standard Colonoscopy: A Randomized Controlled Trial in Patients With Acute Lower Gastrointestinal Bleeding: Results of the BLEED Study. J Clin Gastroenterol. 2019;53:591-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Green BT, Rockey DC, Portwood G, Tarnasky PR, Guarisco S, Branch MS, Leung J, Jowell P. Urgent colonoscopy for evaluation and management of acute lower gastrointestinal hemorrhage: a randomized controlled trial. Am J Gastroenterol. 2005;100:2395-2402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 201] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 8. | Laine L, Shah A. Randomized trial of urgent vs. elective colonoscopy in patients hospitalized with lower GI bleeding. Am J Gastroenterol. 2010;105:2636-41; quiz 2642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 140] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 9. | Niikura R, Nagata N, Yamada A, Honda T, Hasatani K, Ishii N, Shiratori Y, Doyama H, Nishida T, Sumiyoshi T, Fujita T, Kiyotoki S, Yada T, Yamamoto K, Shinozaki T, Takata M, Mikami T, Mabe K, Hara K, Fujishiro M, Koike K. Efficacy and Safety of Early vs Elective Colonoscopy for Acute Lower Gastrointestinal Bleeding. Gastroenterology. 2020;158:168-175.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 10. | Tanaka Y, Motomura Y, Akahoshi K, Iwao R, Komori K, Nakama N, Osoegawa T, Itaba S, Kubokawa M, Hisano T, Ihara E, Nakamura K, Takayanagi R. Predictive factors for colonic diverticular rebleeding: a retrospective analysis of the clinical and colonoscopic features of 111 patients. Gut Liver. 2012;6:334-338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Aytac E, Stocchi L, Gorgun E, Ozuner G. Risk of recurrence and long-term outcomes after colonic diverticular bleeding. Int J Colorectal Dis. 2014;29:373-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Poncet G, Heluwaert F, Voirin D, Bonaz B, Faucheron JL. Natural history of acute colonic diverticular bleeding: a prospective study in 133 consecutive patients. Aliment Pharmacol Ther. 2010;32:466-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Segev L, Ozuner G. Natural history of bleeding risk in colonic diverticulosis. Minerva Gastroenterol Dietol. 2017;63:152-157. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Jensen DM, Ohning GV, Kovacs TO, Jutabha R, Ghassemi K, Dulai GS, Machicado GA. Natural history of definitive diverticular hemorrhage based on stigmata of recent hemorrhage and colonoscopic Doppler blood flow monitoring for risk stratification and definitive hemostasis. Gastrointest Endosc. 2016;83:416-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 15. | Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7038] [Cited by in RCA: 7999] [Article Influence: 190.5] [Reference Citation Analysis (0)] |
| 16. | Koch E, Lovett S, Nghiem T, Riggs RA, Rech MA. Shock index in the emergency department: utility and limitations. Open Access Emerg Med. 2019;11:179-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 109] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 17. | Rosenbaum PR, Rubin DB. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39:33-38. [RCA] [DOI] [Full Text] [Cited by in Crossref: 617] [Cited by in RCA: 637] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 18. | Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48:452-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9275] [Cited by in RCA: 13272] [Article Influence: 1106.0] [Reference Citation Analysis (0)] |
| 19. | Nigam N, Patel P, Sengupta N. Outcomes of Early Versus Delayed Colonoscopy in Lower Gastrointestinal Bleeding Using a Hospital Administrative Database. J Clin Gastroenterol. 2018;52:721-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Nagata N, Niikura R, Ishii N, Kaise M, Omata F, Tominaga N, Kitagawa T, Ikeya T, Kobayashi K, Furumoto Y, Narasaka T, Iwata E, Sugimoto M, Itoi T, Uemura N, Kawai T. Cumulative evidence for reducing recurrence of colonic diverticular bleeding using endoscopic clipping vs band ligation: Systematic review and meta-analysis. J Gastroenterol Hepatol. 2021;36:1738-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 21. | Ishii N, Setoyama T, Deshpande GA, Omata F, Matsuda M, Suzuki S, Uemura M, Iizuka Y, Fukuda K, Suzuki K, Fujita Y. Endoscopic band ligation for colonic diverticular hemorrhage. Gastrointest Endosc. 2012;75:382-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 22. | Okamoto T, Nakamura K, Yamamoto K, Yoshimoto T, Takasu A, Shiratori Y, Ikeya T, Okuyama S, Takagi K, Fukuda K. Safety and Effectiveness of Endoscopic Band Ligation for Colonic Diverticular Bleeding in Elderly Patients. Digestion. 2021;102:760-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Nagata N, Ishii N, Kaise M, Shimbo T, Sakurai T, Akiyama J, Uemura N. Long-term recurrent bleeding risk after endoscopic therapy for definitive colonic diverticular bleeding: band ligation versus clipping. Gastrointest Endosc. 2018;88:841-853.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 24. | Kobayashi K, Nagata N, Furumoto Y, Yamauchi A, Yamada A, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Kishino T, Ishii N, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Kaise M; CODE BLUE-J study collaborators. Effectiveness and adverse events of endoscopic clipping vs band ligation for colonic diverticular hemorrhage: a large-scale multicenter cohort study. Endoscopy. 2022;54:735-744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 33] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 25. | Nagata N, Niikura R, Aoki T, Shimbo T, Itoh T, Goda Y, Suda R, Yano H, Akiyama J, Yanase M, Mizokami M, Uemura N. Increase in colonic diverticulosis and diverticular hemorrhage in an aging society: lessons from a 9-year colonoscopic study of 28,192 patients in Japan. Int J Colorectal Dis. 2014;29:379-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 26. | Nagata N, Niikura R, Shimbo T, Kishida Y, Sekine K, Tanaka S, Aoki T, Watanabe K, Akiyama J, Yanase M, Itoh T, Mizokami M, Uemura N. Alcohol and smoking affect risk of uncomplicated colonic diverticulosis in Japan. PLoS One. 2013;8:e81137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 27. | Wheat CL, Strate LL. Trends in Hospitalization for Diverticulitis and Diverticular Bleeding in the United States From 2000 to 2010. Clin Gastroenterol Hepatol. 2016;14:96-103.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 131] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 28. | Peery AF, Keku TO, Martin CF, Eluri S, Runge T, Galanko JA, Sandler RS. Distribution and Characteristics of Colonic Diverticula in a United States Screening Population. Clin Gastroenterol Hepatol. 2016;14:980-985.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 130] [Article Influence: 14.4] [Reference Citation Analysis (0)] |