Published online Oct 16, 2022. doi: 10.4253/wjge.v14.i10.608
Peer-review started: April 6, 2022
First decision: May 31, 2022
Revised: July 3, 2022
Accepted: September 6, 2022
Article in press: September 6, 2022
Published online: October 16, 2022
Processing time: 188 Days and 16.7 Hours
Peroral endoscopic myotomy is an increasingly used less invasive modality to treat esophageal dysmotility. Recently, triangular tip knife with integrated water jet function has been introduced to mitigate multiple instrument exchanges.
To compare traditional triangular tip knife and water jet knife in terms of pro
We conducted a systemic review and meta-analysis with two authors indepen
We included 7 studies involving 558 patients. Triangular knife and water jet knife were similar in odds of procedural success with ratio of 4.78 (95%CI = 0.22-102.47) and odds of clinical success with ratio of 0.93 (95%CI = 0.29-2.97), respectively. Water jet knife had fewer instrument exchanges compared to triangular knife (2.21, 95%CI = 1.98-2.45 vs 11.9, 95%CI = 11.15-12.70) and usage of coagulation forceps (1.75, 95%CI = 1.52-1.97 vs 2.63, 95%CI = 2.37-2.89). Adverse events were higher in triangular knife group (OR: 2.30, 95%CI = 1.35-3.95).
Peroral endoscopic myotomy using water jet knife is comparable in terms of pro
Core Tip: Peroral endoscopic myotomy (POEM) has gained traction due to its novel technique of preserving the mucosal layer while working in the submucosa and minimizing risk of leakage of contents into the mediastinum. It hails comparable efficacy and safety data to the standard surgical therapy of laparoscopic Heller myotomy in short term follow up studies. The major steps of POEM are similar among centers, including small mucosal incision, submucosal tunneling, myotomy, and mucosal closure. Within these individual steps, many tools and variations exist to achieve the result. Recently, an innovative water-jet integrated triangular tip knife (WJ) has been devised in order to improve procedural time with less instrument changes, as well as minimize adverse events. There have been several studies comparing the conventional triangular tip knife and WJ and suggesting that WJ can achieve similar clinical and procedural success rate, but with lower adverse effects, instrument changes, and intra-procedural coagulation devices. This is the first meta-analysis to compare the two instruments.
- Citation: Belopolsky Y, Puli SR. Water-jet vs traditional triangular tip knife in peroral endoscopic myotomy for esophageal dysmotility: A systemic review and meta-analysis. World J Gastrointest Endosc 2022; 14(10): 608-615
- URL: https://www.wjgnet.com/1948-5190/full/v14/i10/608.htm
- DOI: https://dx.doi.org/10.4253/wjge.v14.i10.608
Idiopathic achalasia is classified as an esophageal motility disorder thought to be related to loss of in
More recently, peroral endoscopic myotomy (POEM) has gained traction due to its novel technique of preserving the mucosal layer while working in the submucosa and minimizing risk of leakage of contents into the mediastinum. It hails comparable efficacy and safety data to the standard surgical therapy of laparoscopic Heller myotomy in short term follow up studies[3,4]. The first endoscopic myotomy was described in 1980 by three Venezuelan gastroenterologists, and later the technique refined with a submucosal tunnel based on two USA publications in 2007 performed on pigs[5-7]. POEM as we know it today, was initially performed on 17 achalasia patients by Inoue et al[8] in a groundbreaking study in 2010.
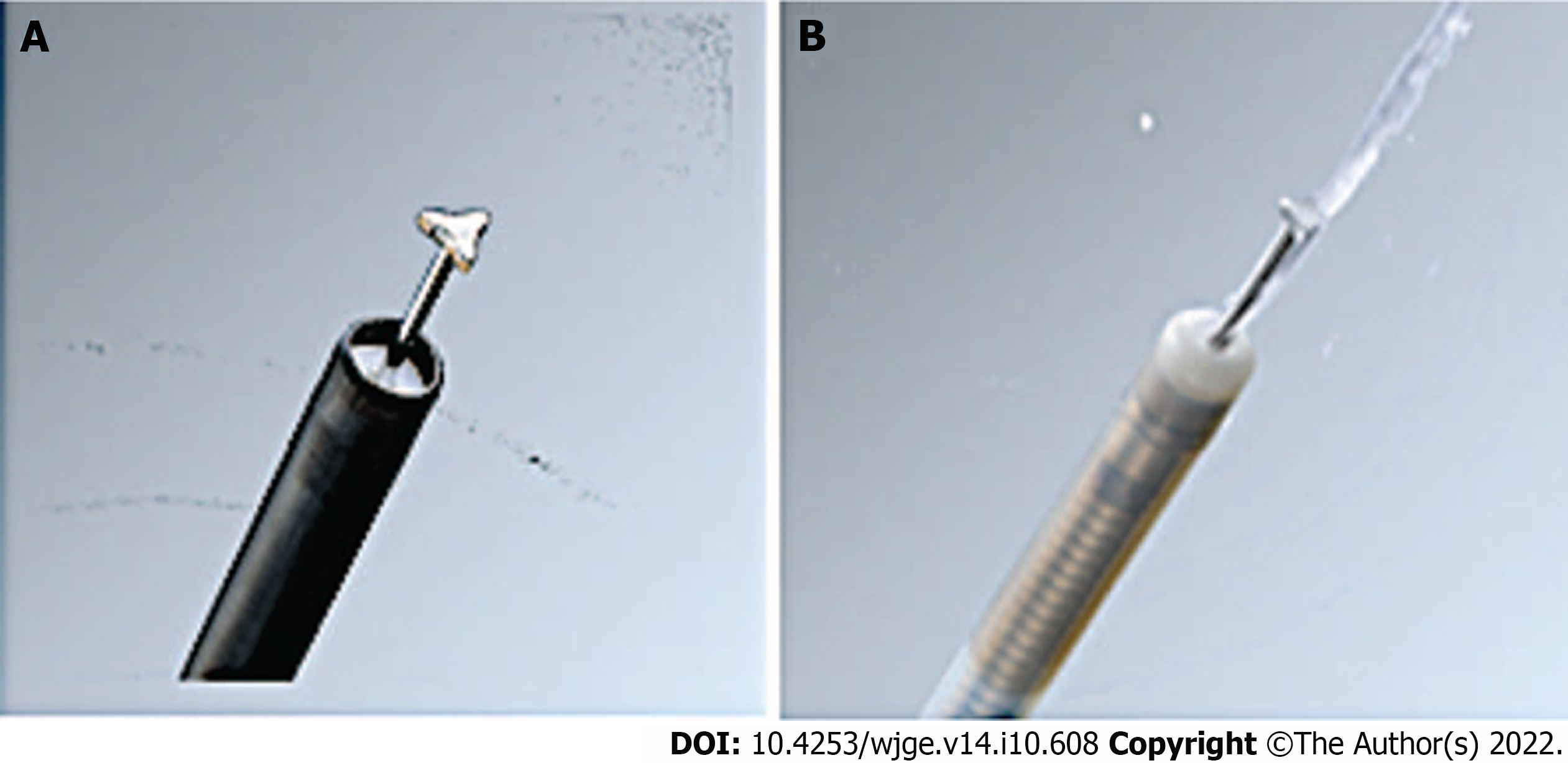
The major steps of POEM are similar among centers, including small mucosal incision, submucosal tunneling, myotomy, and mucosal closure. Within these individual steps, many tools and variations exist to achieve the result. Traditionally, the knife that has been used is a conventional triangular tip knife (TT), which is an electrosurgical knife that has a conductive triangle tip for cutting mucosa. Cutting mucosa can be performed in any direction without rotating the knife, making it suitable for marking, incision, and dissection. Recently, an innovative water-jet integrated triangular tip knife (WJ) has been devised in order to improve procedural time with less instrument changes, as well as minimize adverse events. It comprises a thinner and more compact tip as well as jet function to allow saline injection after cutting without the need to switch devices (Figures 1 and 2). There have been several studies comparing the conventional triangular TT and WJ and suggesting that WJ can achieve similar clinical and procedural success rate, but with lower adverse effects, instrument changes, and intra-procedural coagulation devices[9].
Current literature lacks high-quality evidence to compare clinical outcomes of WJ and TT knives in POEM used for esophageal dysmotility disorders. The purpose of our systemic review and meta-analysis is to compare WJ and TT in terms of procedural and clinical success, and determine whether fewer adverse events and instrument changes could be achieved with the decreased procedural duration.
Studies using triangular tip knife with integrated water jet as the instrument for peroral endoscopic myotomy were selected. Inclusion criteria included both adults and children with an indication of esophageal motility disorders for POEM treatment. Each study used POEM for achalasia, while 1 study did include other indications of diffuse esophageal spasm, nutcracker esophagus, and non-relaxing lower esophageal sphincter. Studies included patients that had been treated with prior therapies before POEM, of which majority were pneumatic balloon dilation.
Studies were systemically searched independently by two investigators (Belopolsky Y and Puli SR) in Pubmed, Cochrane, and EMBASE. The search was performed from inception to May 2021. The search terms used were “peroral endoscopic myotomy” and “knife”. Each abstract and title were screened for eligibility. All references at the end of each selected article were explored manually to retrieve additional studies. Any differences among investigators were resolved by mutual agreement. The interobserver variability was 1. The quality of evidence was evaluated using the Grading of Recommendations Assessment, Development and Evaluation methodology[10]. The agreement between reviewers for the collected data gave a Cohen κ value of 1.0.
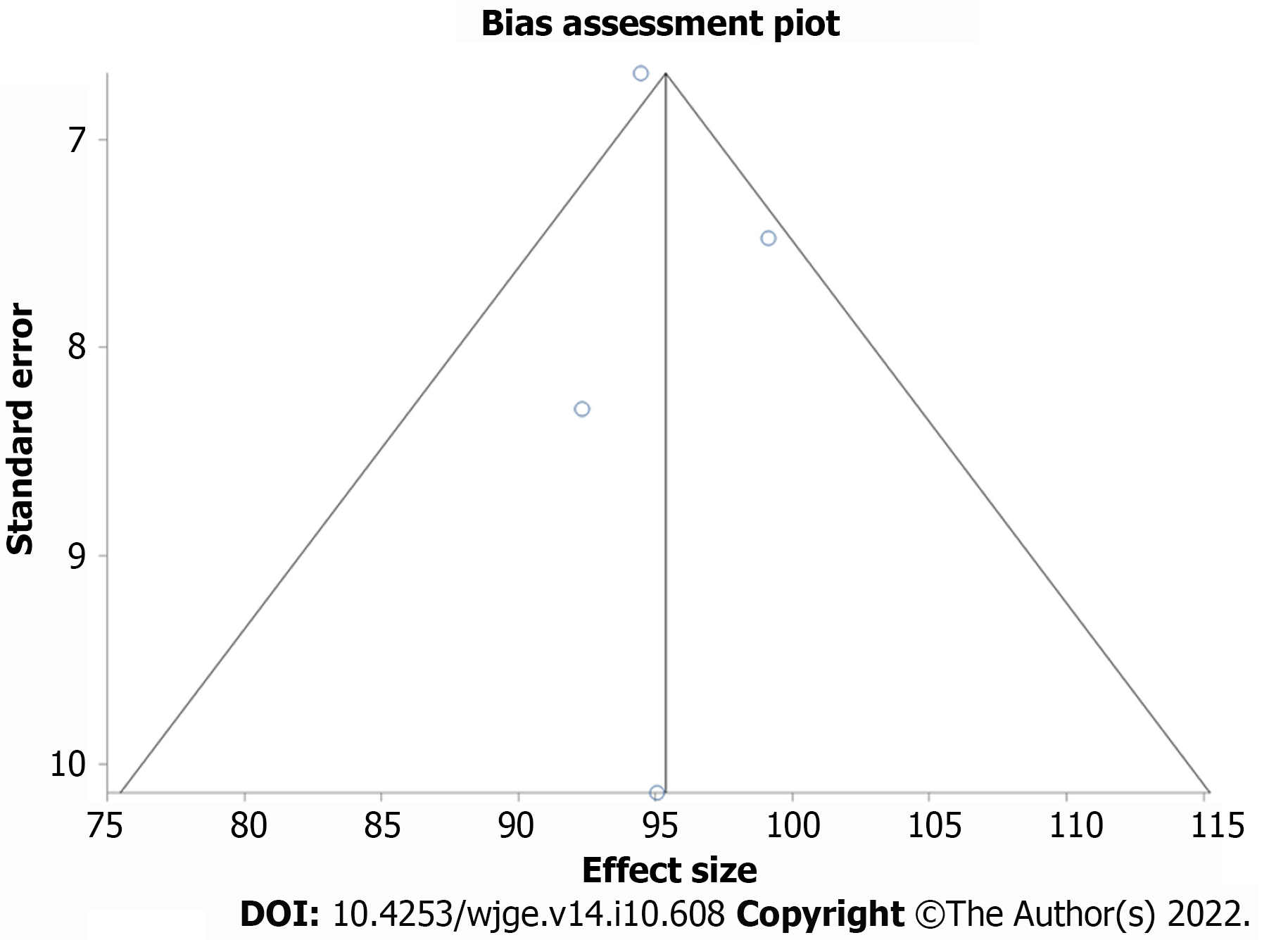
This meta-analysis was performed by calculating weighted pooled effect i.e., weighted pooled effect of patients with procedural success. First the individual study weighted pooled effect of procedural success was transformed into a quantity using Freeman-Tukey variant of the arcsine square root transformed proportion. The pooled proportion is calculated as the back-transform of the weighted mean of the transformed proportions, using inverse arcsine variance weights for the Mantel-Haenszel Method (fixed effects model) and DerSimonian-Laird Method (random effects model)[11,12]. Random effect model was used for meta-analysis in case of heterogeneity being statistically significant otherwise fixed effect models were applied. Forest plots were drawn to show the point estimates in each study in relation to the summary pooled estimate. The width of the point estimates in the Forest plots indicates the assigned weight to that study. In addition, odds ratio was used to represent dichotomous outcomes with a 95% confidence interval (CI), where a p value of <0.05 was considered statistically significant. The heterogeneity among studies was tested using I2 and Cochran’s Q test based upon inverse variance weights[13]. I2 of 0% to 39% was considered as non-significant heterogeneity, 40% to 75% as moderate heterogeneity, and 76% to 100% as considerable heterogeneity. If P value is > 0.10, it rejects the null hypothesis that the studies are heterogeneous. The effect of publication and selection bias on the summary estimates was tested by both Harbord-Egger bias indicator and Begg-Mazumdar bias indicator[14]. Also, funnel plots were constructed to evaluate potential publication bias using the standard error and diagnostic odds ratio[15,16].
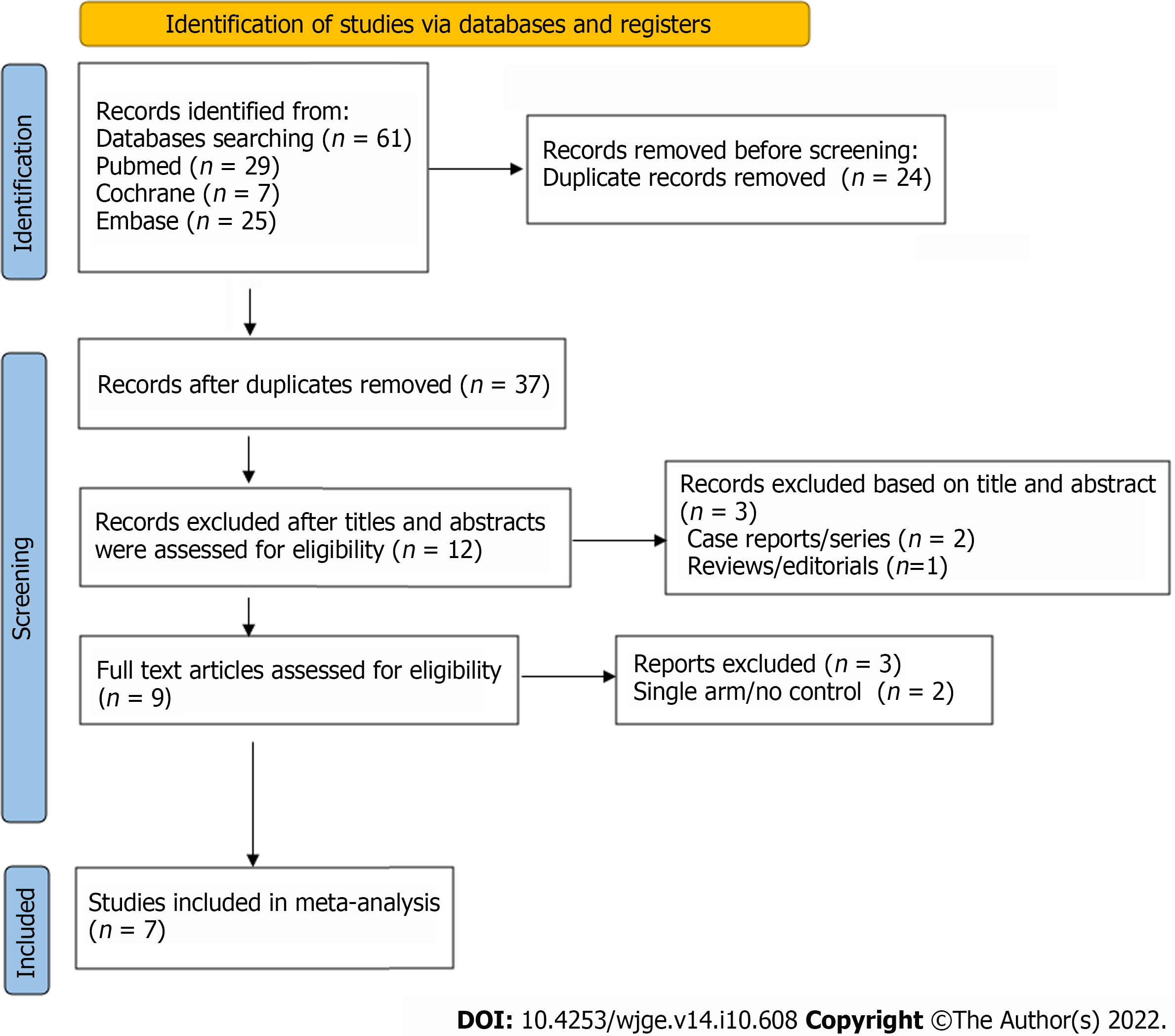
A total of 61 studies were retrieved by our search strategy. We reviewed these and excluded 52 studies based on titles and abstracts and reviewed full texts of remaining 9 studies. Finally, 7 studies met our inclusion and exclusion criteria[9,17-21]. This consisted of 2 randomised controlled trial (RCT) and 5 retrospective single center cohorts published between 2012 and 2021. Five studies were published full text articles while two studies were available as abstract poster presentations. Figure 1 shows the PRISMA flow chart to illustrate how final studies were selected. All pooled estimates were calculated using fixed and random effects models. The pooled effects estimated by both models were similar. All the pooled estimates given below are from the fixed effect model. Heterogeneity was assessed with I-squared, and publication bias with Egger’s test.
A total of 558 patients were included in this meta-analysis. The mean age of patients’ was 42.82 years (SD = 7.86) in the TT group and 37.03 years (SD = 12.29) in the WJ group, of which 59.57% were male in TT vs 52.51% in WJ group.
This review analyzed the various outcomes including procedural success, clinical successes defined as < 3 Eckardt score post-POEM, procedure duration, number of instrument exchanges, and usage of coagulation forceps. Most, but not all studies, included information on every variable that was analyzed. The studies that included information on the specific variable were included in the final analysis of that variable.
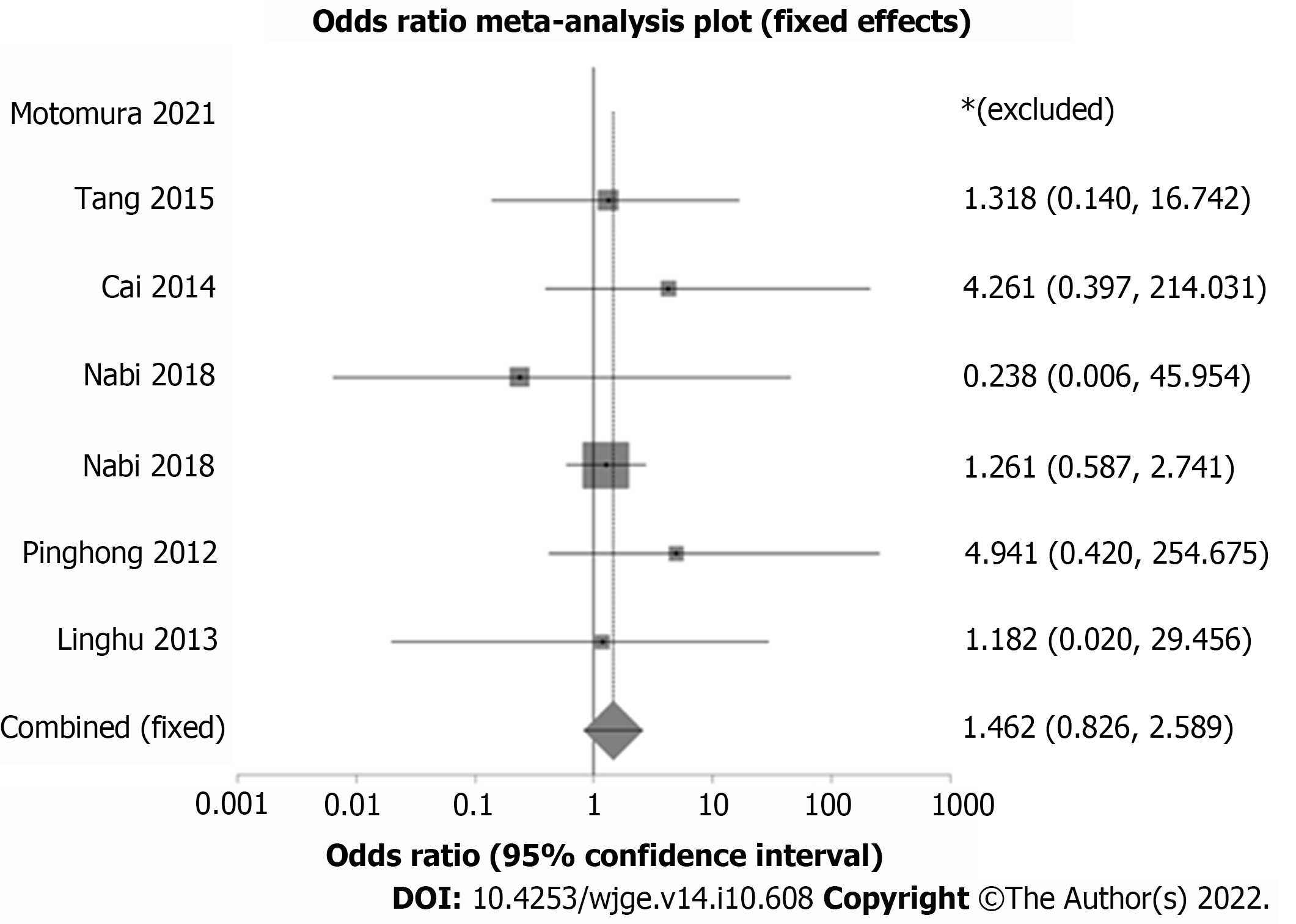
Analysis showed weighted odds of technical success for POEM in TT group compared to WJ group to be 4.78 (95%CI = 0.22-102.47). In terms of clinical success, the standard accepted definition is a score of three or below in Eckardt score. The TT group had weighted odds of clinical success compared to WJ of 0.93 (95%CI = 0.29-2.97) (Figure 3). Publication bias calculated using Begg-Mazumdar gave Kendall’s tau b value of -0.33 (P = 0.33). Heterogeneity calculated using I2was 0 indicating no significant heterogeneity among studies.
Analysis of procedural duration for WJ had a weighted mean duration of 31.63 min (95%CI = 29.44-33.82) as compared to TT with weighted mean duration of 50.45 min (95%CI = 47.35-53.55). Regarding instrument changes, analysis showed a weighted number of instrument changes for TT of 11.92 times (95%CI = 11.15-12.70) vs WJ with weighted number of instrument changes of 2.21 times (95%CI = 1.98-2.45). The usage of coagulation forceps analysis showed for WJ the weighted usage of coagulation forceps to be 2.63 times, (95%CI = 2.37-2.89) vs TT with weighted usage of coagulation forceps to be of 1.75 times (95%CI = 1.52-1.97).
Adverse events
The overall adverse events of TT compared to WJ had a pooled OR of 2.34 (95%CI = 1.34-4.23) (Figure 4). When evaluating the adverse event of subcutaneous emphysema, TT had a pooled OR of 1.46 (95%CI = 0.83-2.59) compared to WJ.
We performed a systemic review and meta-analysis of studies that compared conventionally used triangular tip knife and a knife using new integrated water-jet technology, in terms of several peri- and post-procedural outcomes. There was comparable procedural as well as clinical success, defined as post-operative Eckardt score of 3 or lower.
By pooling data across studies, our meta-analysis showed that WJ had statistically decreased procedural time of 32 min as compared to the TT of 50 min. For the endoscopist, that could theoretically increase procedural productivity. In addition, our analysis showed that both instrument exchanges and usage of coagulation forceps were decreased in the WJ group when compared to the TT group. Likely this can partially explain the shorter procedural duration, as well as indicate less intra-procedural bleeding with the less use of coagulation instruments.
The frequently reported adverse events of POEM include pneumomediastinum, mucosal perforations, pneumothorax, mucosal perforations, and subcutaneous emphysema[22]. In our meta-analysis, statistically adverse events were less likely to happen in the WJ group compared to the TT group. However, when examining one adverse event commented on in each study of subcutaneous emphysema, this was comparable among both groups as the confidence interval crossed one. Thus while overall adverse events were lower, it is difficult to discern which, if any, WJ could have lower risk of provoking.
Our study is the first in the literature to assess TT and WJ knives in POEM procedures for esophageal dysmotility disorders and analyze their effectiveness for the procedure. There are several strengths to our review. First, we included studies of WJ compared to standard TT technique, including 2 RCT. This allowed a more valuable comparison of procedural outcomes. Second, we conducted a systemic literature review with well-defined inclusion criteria, as well as careful exclusion of redundant studies with detailed extraction of data. Third, we separated studies that did not evaluate esophageal dysmotility disorders specifically, due to variable intra-procedural techniques that could have skewed the data.
While this study has included the most recent randomized controlled trials, these are few in our current available literature. Second, our conclusions apply to achalasia primarily, and did not include other indications for POEM other than those related to esophageal motility disorders. Finally, blinding of endoscopists was not possible and thus performance bias could have played a factor as well as inability to assess each performing endoscopist’s skill level.
Water jet triangular tip knife has decreased procedural duration, number of instruments used, and usage of coagulation forceps over the conventional triangular tip knife. As such, this modality represents an attractive option for POEM. Our review represents the first review of the literature regarding water jet triangular tip knife in the management of esophageal dysmotility disorders using POEM. Collectively, the data supports using water jet triangular tip knife as a primary modality in terms of safety for the patient with less adverse events, with comparable technical and clinical success to the conventional triangular tip knife.
This study is the first metanalysis to discover the differences between two main modalities for performing peroral endoscopic myotomy.
This study allows us to continue progressing in terms of instruments as it leads to continued success, but quicker and less adverse outcomes.
To compare two knives, conventional triangular tip as well as water jet integrated triangular tip knives.
Clinical trials were examined and put together into metaanalysis.
This shows that water jet knife is comparable in terms of success to conventional traditional triangular knife with fewer adverse events and faster time.
This study proposes new availability in instruments to the field of endoscopic myotomy.
This allows future research to examine additional instruments and how to continue to further clinical success with better outcomes as well as ease for the endoscopist.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Okasha H, Egypt; Toyoshima O, Japan S-Editor: Wang LL L-Editor: A P-Editor: Cai YX
| 1. | Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol. 2005;100:1404-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 255] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 2. | Pandolfino JE, Gawron AJ. Achalasia: a systematic review. JAMA. 2015;313:1841-1852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 296] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 3. | von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J, Fuchs KH, Rösch T. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012;107:411-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 250] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 4. | Swanström LL, Rieder E, Dunst CM. A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg. 2011;213:751-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 111] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 5. | Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26:8-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 101] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 360] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 7. | Sumiyama K, Gostout CJ, Rajan E, Bakken TA, Knipschield MA. Transesophageal mediastinoscopy by submucosal endoscopy with mucosal flap safety valve technique. Gastrointest Endosc. 2007;65:679-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 114] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 8. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1230] [Article Influence: 82.0] [Reference Citation Analysis (1)] |
| 9. | Nabi Z, Ramchandani M, Chavan R, Tandan M, Kalapala R, Darisetty S, Reddy DN. Peroral Endoscopic Myotomy in Children: First Experience With a New Triangular Knife. J Pediatr Gastroenterol Nutr. 2018;66:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Brozek JL, Akl EA, Alonso-Coello P, Lang D, Jaeschke R, Williams JW, Phillips B, Lelgemann M, Lethaby A, Bousquet J, Guyatt GH, Schünemann HJ; GRADE Working Group. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64:669-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 383] [Cited by in RCA: 582] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 11. | Deeks JJ. Systematic reviews in health care: Systematic reviews of evaluations of diagnostic and screening tests. BMJ. 2001;323:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 822] [Cited by in RCA: 896] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 12. | DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26739] [Cited by in RCA: 30365] [Article Influence: 778.6] [Reference Citation Analysis (0)] |
| 13. | Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25:3443-3457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1463] [Cited by in RCA: 1701] [Article Influence: 89.5] [Reference Citation Analysis (0)] |
| 14. | Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323:101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1519] [Cited by in RCA: 1565] [Article Influence: 65.2] [Reference Citation Analysis (0)] |
| 15. | Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2183] [Cited by in RCA: 2630] [Article Influence: 109.6] [Reference Citation Analysis (0)] |
| 16. | Tran QN, Urayama S, Meyers FJ. Endoscopic ultrasound-guided celiac plexus neurolysis for pancreatic cancer pain: a single-institution experience and review of the literature. J Support Oncol. 2006;4:460-462. [PubMed] |
| 17. | Motomura D, Hew S, Bechara R. Novel triangle tip-jet knife increases efficiency in peroral endoscopic myotomy for achalasia. JGH Open. 2021;5:1142-1147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 18. | Nabi Z, Ramchandani M, Chavan R, Kalapala R, Darisetty S, Reddy DN. Outcome of peroral endoscopic myotomy in achalasia cardia: Experience with a new triangular knife. Saudi J Gastroenterol. 2018;24:18-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Cai MY, Zhou PH, Yao LQ, Xu MD, Zhong YS, Li QL, Chen WF, Hu JW, Cui Z, Zhu BQ. Peroral endoscopic myotomy for idiopathic achalasia: randomized comparison of water-jet assisted vs conventional dissection technique. Surg Endosc. 2014;28:1158-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 20. | Tang X, Gong W, Deng Z, Zhou J, Ren Y, Zhang Q, Chen Z, Jiang B. Comparison of conventional vs Hybrid knife peroral endoscopic myotomy methods for esophageal achalasia: a case-control study. Scand J Gastroenterol. 2016;51:494-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Martinek J, Svecova H, Vackova Z, Dolezel R, Ngo O, Krajciova J, Kieslichova E, Janousek R, Pazdro A, Harustiak T, Zdrhova L, Loudova P, Stirand P, Spicak J. Per-oral endoscopic myotomy (POEM): mid-term efficacy and safety. Surg Endosc. 2018;32:1293-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 22. | Cappell MS, Stavropoulos SN, Friedel D. Updated Systematic Review of Achalasia, with a Focus on POEM Therapy. Dig Dis Sci. 2020;65:38-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |