Published online Jul 16, 2021. doi: 10.4253/wjge.v13.i7.233
Peer-review started: December 18, 2020
First decision: December 31, 2020
Revised: January 14, 2021
Accepted: June 25, 2021
Article in press: June 25, 2021
Published online: July 16, 2021
Processing time: 207 Days and 12 Hours
Red dichromatic imaging (RDI) is a novel image-enhanced endoscopy expected to improve the visibility of the bleeding point. However, it has not been thoroughly investigated.
A 91-year-old man developed a sudden massive hematochezia and underwent emergent colonoscopy. An ulcer with pulsatile bleeding was found on the lower rectum. Due to massive bleeding, the exact location of the bleeding point was not easy to detect with white light imaging (WLI). Upon switching to RDI, the bleeding point appeared in deeper yellow compared to the surrounding blood. Thus, RDI enabled us for easier recognition of the bleeding point, and hemostasis was achieved successfully. Furthermore, we reviewed endoscopic images and evaluated the color difference between the bleeding point and surrounding blood for WLI and RDI. In our case, the color difference of RDI was greater than that of WLI (9. 75 vs 6. 61), and RDI showed a better distinguished bleeding point from the surrounding blood.
RDI may improve visualization of the bleeding point by providing better contrast in color difference relative to surrounding blood.
Core Tip: Red dichromatic imaging (RDI) is a novel image-enhanced endoscopy presumed to improve the visibility of the bleeding point but has not yet been fully explored. We present a case in which RDI effectively identified the bleeding point in an acute hemorrhagic rectal ulcer lesion with an analysis of color difference compared to white light imaging. RDI may enable easier recognition of the bleeding point by enhancing the color contrast of the bleeding point relative to the surrounding blood.
- Citation: Hirai Y, Kayashima A, Nakazato Y, Fujimoto A. Visibility of the bleeding point in acute rectal hemorrhagic ulcer using red dichromatic imaging: A case report. World J Gastrointest Endosc 2021; 13(7): 233-237
- URL: https://www.wjgnet.com/1948-5190/full/v13/i7/233.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i7.233
Endoscopic hemostasis of acute gastrointestinal bleeding is sometimes a challenging task, especially when pulsatile bleeding from the artery impedes clear visibility of the bleeding point. Red dichromatic imaging (RDI) is a new endoscopic technology using three types of wavelength (540 nm, 600 nm and 630 nm) lights[1]. It is integrated as a new function in the latest endoscopic system (EVIS X1, Olympus Co., Tokyo, Japan) from April 2020. An endoscopist can quickly switch from white light imaging (WLI) to RDI, a modality that visualizes blood in yellow, during an endoscopic intervention. Recently, RDI has been found to be effective in the identification of bleeding point in endoscopic hemostasis during endoscopic submucosal dissection or hemorrhage from upper gastrointestinal ulcer[2-5]. In this report, we describe an impressive case in which RDI effectively identified the bleeding point in an acute hemorrhagic rectal ulcer lesion via analysis of the color difference between the bleeding point and surrounding blood.
A 91-year-old man hospitalized with pneumonia was referred to our department due to sudden massive fresh hematochezia on the 13th day of hospitalization.
At admission, a right femoral neck fracture was also found and required bed-rest as a nonoperative treatment.
He had a history of pneumonia and hypertension.
He had smoked 2 packs-per-day of cigarettes for over 30 years but quit 40 years ago and was a social drinker. His family history was unremarkable.
He presented signs of hypovolemic shock with low blood pressure (BP of 79/38 mmHg) and tachycardia (101 bpm). The vital signs were stabilized after a rapid infusion of 1000 mL of lactated Ringer’s solution. His abdominal examination was normal with no tenderness.
His hemoglobin level dropped from 11.5 to 7.2 g/dL.
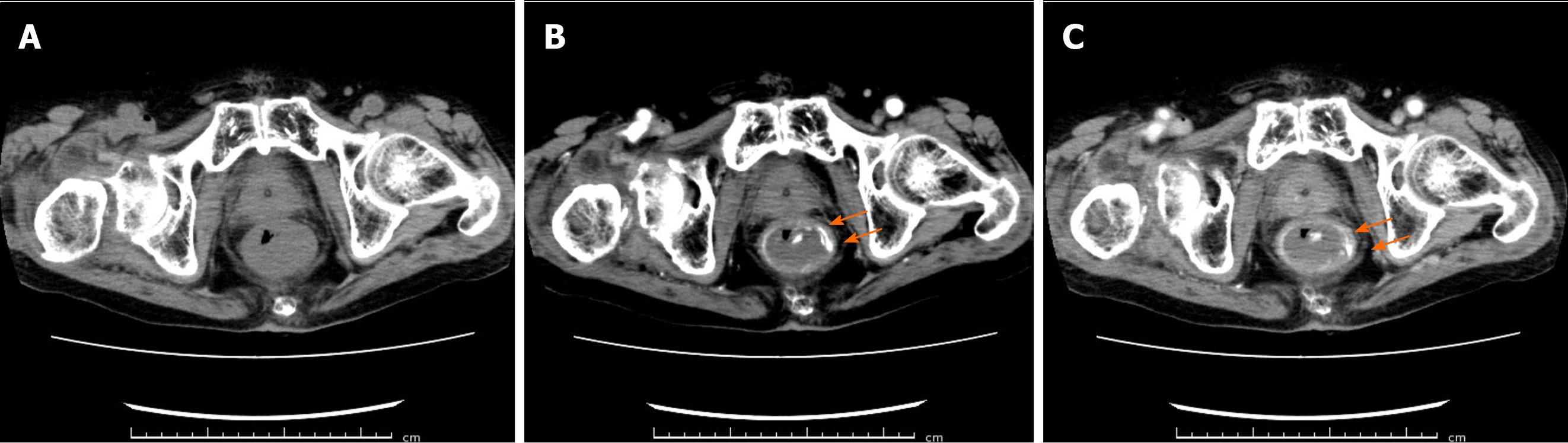
Contrast computed tomography revealed extravasation in the lower rectum (Figure 1). After computed tomography, we promptly performed an emergent colonoscopy using a prototype endoscope (GIF-Y0058; Olympus Co., Tokyo, Japan) instrumented with RDI mode, and an ulcer accompanied with a pulsatile bleeding was found on the lower rectum.
The patient was diagnosed with acute hemorrhagic rectal ulcer, likely caused due to being bed-rest status and constipated.
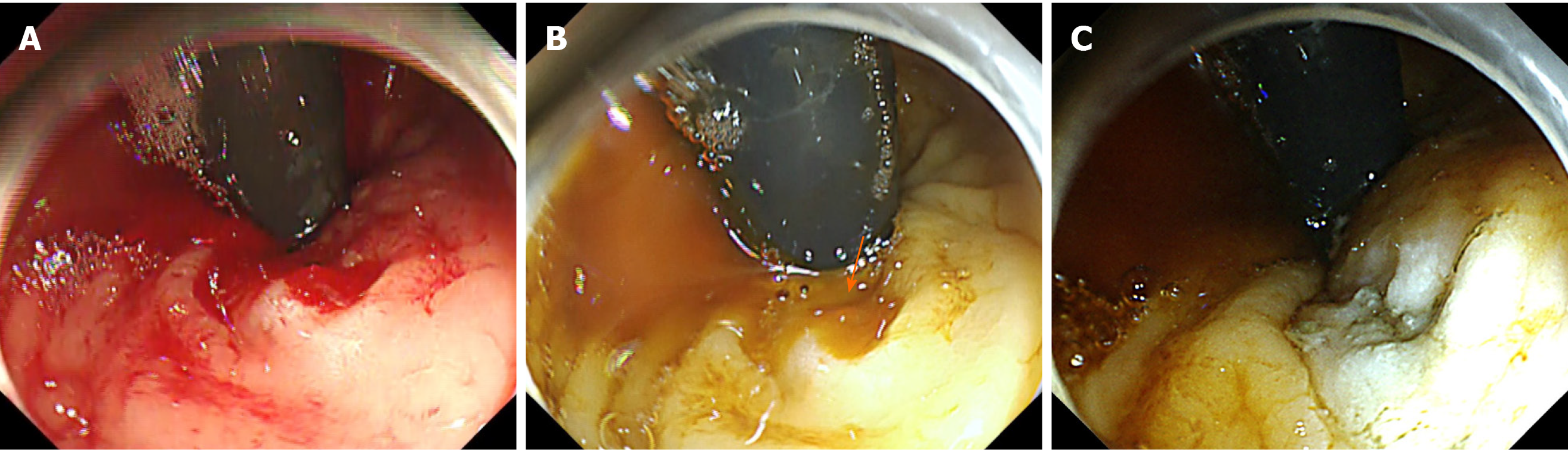
Followed by endoscopic observation, we went on to achieve hemostasis. However, massive bleeding with pooled blood hindered observation of the bleeding point with WLI (Figure 2A). Thereby, we switched to RDI, and the bleeding point was clearly identified as it was displayed in deeper yellow compared to the surrounding blood (Figure 2B). The bleeding vessel was coagulated with hemostatic forceps (Coagrasper; Olympus Co., Tokyo, Japan) in soft coagulation current (effect 5, 50 W) using an electrosurgical system (VIO300D; ERBE, Tübingen, Germany), and hemostasis was obtained successfully (Figure 2C).
After the achievement of endoscopic hemostasis, his anemia improved after receiving 4 units of packed red blood cells. No further bleeding was noted for a month until the patient was discharged to another hospital for rehabilitation.
When attempting endoscopic hemostasis for active bleeding with acute hemorrhagic rectal ulcer using WLI, we often encounter with pooled blood hindering the detection of bleeding points in a similar shade of red. The patient may even need to be repositioned to facilitate the detection of the bleeding point when the bleeding point is located at the gravity side. RDI may overcome this problem as it can enhance the bleeding point in the presence of pooled blood and eventually facilitate the endoscopic hemostasis. The key mechanism of RDI that enables clear visualization of the bleeding point in the presence of pooled blood is the difference in blood concentration and/or blood volume. The narrow-band light of 600 nm wavelength highlights the difference in blood concentration and/or its volume because of the light absorption features of the hemoglobin. The center and circumference of the bleeding point appears in clear contrast because they contain different amounts of hemoglobin and accordingly absorb and reflect differential levels of 600 nm light[6,7]. This means that more light is reflected from the center and less from the circumference. We speculated that this mechanism produces a larger color difference between the bleeding point and surrounding blood, resulting in easier detection of the bleeding point.
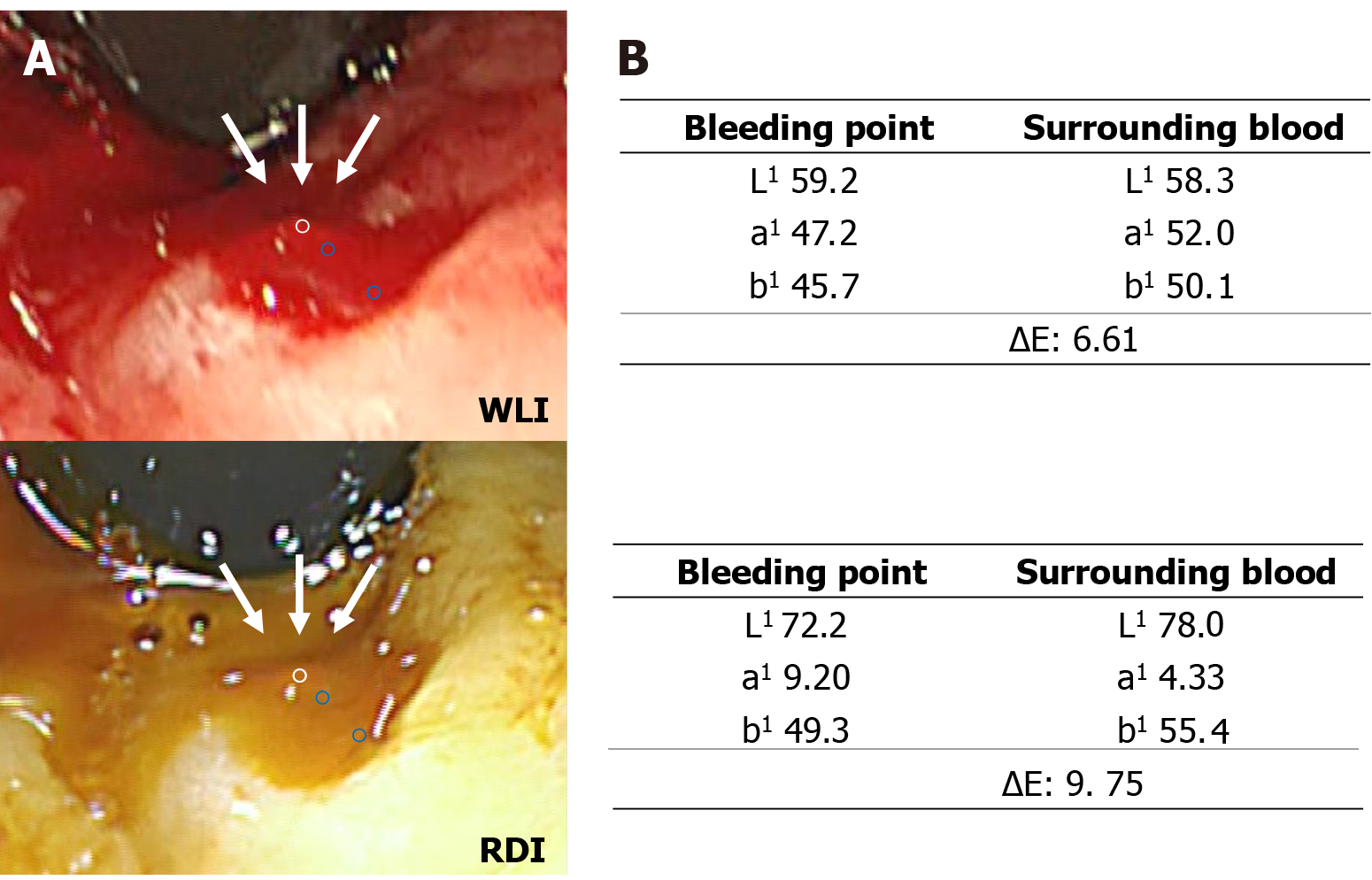
Therefore, we investigated the visibility of the bleeding point by evaluating the color difference between the bleeding point and surrounding blood for WLI and the corresponding RDI images in still pictures of this case. The color difference was evaluated by comparing the color values of regions of interest (ROI) for the bleeding point and surrounding blood using Adobe Photoshop Elements 2020 (Adobe Systems Inc., CA, San Jose, United States). The details for the setting of ROI are shown in Figure 3A. The color values were defined as the median color values in each ROI (24 × 24 pixels) according to the Commission Internationaled’Eclairage L1a1b1 (L1 = black to white; 0 to + 100, a1 = green to red; -128 to + 127, b1 = blue to yellow; -128 to + 127) color space[8]. The color difference was calculated by the following equation: ΔE = √ (ΔL)2 + (Δa)2 + (Δb)2. In the present case, the color difference with WLI and RDI was 6.61 and 9.75, respectively (Figure 3B). Thus, RDI differentiated the bleeding point from surrounding blood better than WLI based on color difference.
This report is the first of its kind to use the color difference as an objective indicator for the investigation of the visibility of bleeding point with RDI. Subsequent to this research, we are now conducting a larger study by comparing the visibility of the bleeding point including the evaluation of the color difference between WLI and RDI for acute gastrointestinal bleeding.
Our case of acute hemorrhagic rectal ulcer demonstrated the usefulness of red dichromatic imaging for achieving endoscopic hemostasis by improving the detection of the bleeding point. Red dichromatic imaging may be useful for recognition of the bleeding point by offering good contrast in color difference relative to surrounding blood.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Montemurro N S-Editor: Zhang L L-Editor: A P-Editor: Wang LL
| 1. | Yahagi N, Fujimoto A, Horii J, Uraoka T, Shimoda M, Takabayashi K, Nisizawa T, Goto O, Ochiai Y, Maehata T, Nakayama A, Kato M, Hosoe N, Naganuma M. Dual red imaging: a novel endoscopic imaging technology visualizing thick blood vessels in the gastrointestinal wall. Endosc Int Open. 2019;7:E1632-E1635. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Tanaka H, Oka S, Tanaka S. Endoscopic hemostasis for spurting duodenal bleeding using dual red imaging. Dig Endosc. 2017;29:816-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Kubosawa Y, Mori H, Fujimoto A. Utility of Dual Red Imaging for Endoscopic Hemostasis of Gastric Ulcer Bleeding. Dig Dis. 2020;38:352-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Yorita N, Oka S, Tanaka S, Kotachi T, Nagasaki N, Hata K, Kuroki K, Masuda K, Kurihara M, Kiso M, Boda T, Ito M, Chayama K. Clinical Usefulness of Dual Red Imaging in Gastric Endoscopic Submucosal Dissection: A Pilot Study. Clin Endosc. 2020;53:54-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Maehata T, Fujimoto A, Uraoka T, Kato M, Horii J, Sasaki M, Kiguchi Y, Akimoto T, Nakayama A, Ochiai Y, Goto O, Nishizawa T, Yahagi N. Efficacy of a new image-enhancement technique for achieving hemostasis in endoscopic submucosal dissection. Gastrointest Endosc. 2020;92:667-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Fujimoto A, Saito Y, Abe S, Hoteya S, Nomura K, Yasuda H, Matsuo Y, Uraoka T, Kuribayashi S, Saito I, Tsuji Y, Maehata T, Ochiai Y, Nishizawa T, Yahagi N. Haemostasis treatment using dual red imaging during endoscopic submucosal dissection: a multicentre, open-label, randomised controlled trial. BMJ Open Gastroenterol. 2019;6:e000275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Miyamoto S, Sugiura R, Abiko S, Hatanaka K, Yamamoto Y, Naruse H, Sakamoto N. Red dichromatic imaging helps in detecting exposed blood vessels in gastric ulcer induced by endoscopic submucosal dissection. Endoscopy. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Kuehni RG. Color-tolerance data and the tentative CIE 1976 L a b formula. J Opt Soc Am. 1976;66:497-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 99] [Article Influence: 2.0] [Reference Citation Analysis (0)] |