Published online Jun 16, 2021. doi: 10.4253/wjge.v13.i6.184
Peer-review started: January 18, 2021
First decision: May 5, 2021
Revised: May 17, 2021
Accepted: May 25, 2021
Article in press: May 25, 2021
Published online: June 16, 2021
Processing time: 143 Days and 8.1 Hours
The occurrence of splenic rupture is extremely rare during an upper gastro-intestinal endoscopy. Although infrequent, splenic rupture is a known complication secondary to colonoscopy. However, occurrence of splenic rupture after peroral endoscopic myotomy (POEM) has never been reported to date.
We describe a case of a splenic rupture following a POEM for recurrent achalasia in a patient who previously had a Heller myotomy. Splenic rupture remains very uncommon after an upper gastro-intestinal endoscopic procedure. The most plausible cause for this rare splenic injury appears to be the stretching of the gastro-splenic ligament during the endoscopy. A previous surgery may be a risk factor contributing to this complication.
The possibility for the occurrence of specific complications, such as splenic rupture, does exist even with the development of advanced endoscopic procedures, as presented in the present case after POEM.
Core Tip: Splenic rupture is extremely rare but may occur during an upper gastro-intestinal endoscopy. Occurrence of splenic rupture after peroral endoscopic myotomy (POEM) has never been reported to date. The first reported case of splenic rupture following a POEM is presented. This very unusual but severe complication will probably occur again as this procedure will continue to be developed and implemented. Physicians must be aware that splenic rupture can happen after POEM.
- Citation: Maniere T, Aboudan C, Deslauriers N, Pichette M, Bergeron E. First splenic rupture following an endoscopic esophageal myotomy: A case report. World J Gastrointest Endosc 2021; 13(6): 184-188
- URL: https://www.wjgnet.com/1948-5190/full/v13/i6/184.htm
- DOI: https://dx.doi.org/10.4253/wjge.v13.i6.184
Peroral endoscopic myotomy (POEM) is now considered as an effective therapy for achalasia, at least as efficient as laparoscopic Heller myotomy[1]. Only in about 7.5% of the cases with POEM, adverse events were reported, which were minor in the majority of the cases[2]. To our knowledge, there have been no reports of splenic rupture during or after POEM.
The occurrence of splenic rupture is quite rare during an upper gastro-intestinal endoscopy. Majority of the cases occurred after endoscopic retrograde cholangiopancreatography[3]. Splenic rupture is however a known complication after colonoscopy, with approximately 1 case out of 100000 procedures[4].
Only two cases of splenic rupture after gastroscopy[5,6], and three cases following esophageal endoscopic procedures[7-9] have been reported in the literature since the advent of flexible endoscopes. However, there has been no report of splenic rupture after endoscopic myotomy for achalasia of the esophagus.
We present here for the first time, a patient with recurrent achalasia, who underwent an endoscopic myotomy and developed a splenic rupture, secondary to this procedure.
Three days after POEM, a patient suddenly developed severe diffuse abdominal pain and nausea.
The patient was admitted electively to undergo POEM for recurrent achalasia.
The patient was diagnosed with achalasia and underwent a laparoscopic Heller myotomy with posterior Toupet fundoplication in 2004. He had no history of hepatic or hematologic disease. After one year of improvement, the patient complained of a relapse of achalasia symptoms with significant worsening in the late 2019. He complained about recurrent dysphagia, significant weight loss of 8 kg in 1 year, and repeated food impaction, which needed endoscopic clearance. Food stasis was found with dilated esophagus and resistance at the gastro-esophageal junction (GEJ) without any stricture. A barium meal demonstrated barium stasis and dilated esophagus caused by a large concentric narrowing at the GEJ. Manometry confirmed a recurrence of type 2 achalasia, with ineffective swallowing, incomplete relaxation of the lower esophageal sphincter and pan-pressurization. Computed tomography and magnetic resonance imaging in 2020 for staging workup of prostatic cancer revealed normal size spleen without vascular abnormality or signs of portal hypertension.
Based on the clinical presentation and manometry results we decided to perform a POEM. The procedure was performed under general anesthesia, using carbon dioxide insufflator, in November 2020. A 14 cm long submucosal tunnel that ended 3 cm below the GEJ was made with a triangle type knife using spray coagulation. A selective posterior myotomy was performed involving the circular inner layer using electric endocut. However, a significant bleeding at the GEJ was noted, requiring hemostasis with a hemostatic forceps. The hemostasis maneuvers were efficient but caused a deeper muscle dehiscence. At the end of the procedure, the incision was closed with 6 endoscopic clips, and the iatrogenic pneumoperitoneum was decompressed. The procedure lasted 40 min. The patient was hospitalized for 24 h. Soft diet was resumed the next day, and the patient was discharged. His hemoglobin level was 129 g/L (Normal: 134-170 g/L).
The patient is a 66-year-old man with a history of hypertension, and alcoholism with the consumption of 3 drinks per day. He had a prostatic adenocarcinoma that was treated with curie therapy in 2020. Family history was irrelevant.
Upon admission, the patient had left upper abdominal pain without defense or rebound tenderness. His vital signs were stable with blood pressure of 100/64 mmHg, HR of 76, and temperature of 37.0 °C.
The blood tests revealed low hemoglobin level at 69 g/L (Normal: 134-170 g/L). Liver function tests and coagulation parameters were within the normal limits.
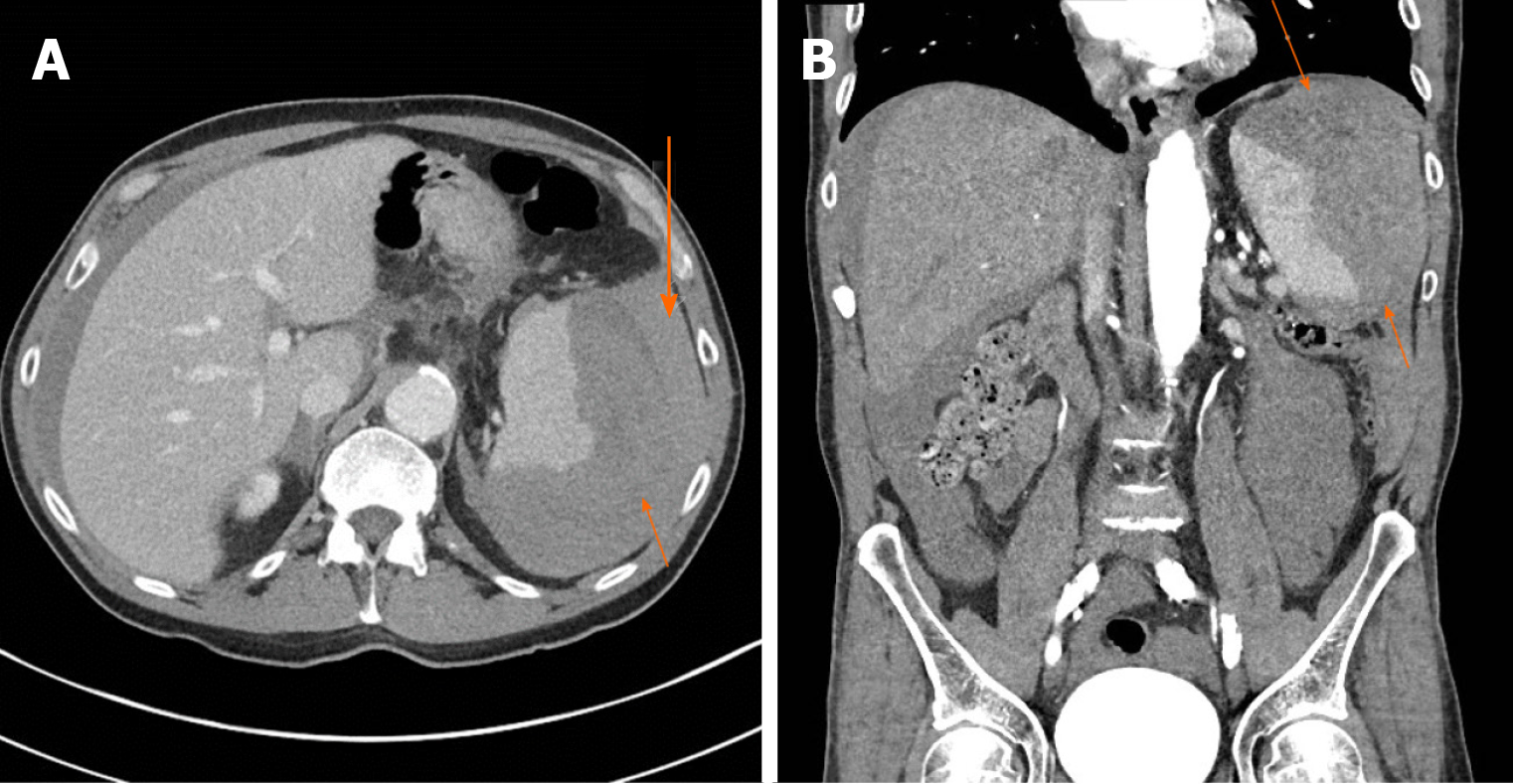
The enhanced abdominal computed tomography demonstrated a subcapsular hematoma in the spleen, measuring a maximum diameter of 12 cm and perpendicular diameter of 6 cm, with no active bleeding, and moderate hemoperitoneum but no pneumoperitoneum (Figure 1). There was still no sign of cirrhosis or portal hypertension.
Splenic rupture after POEM for recurrent achalasia.
Considering the hemodynamic stability of the patient, supportive treatment was initiated with volume repletion and transfusion of two units of red blood cells. Close observation for 48 h confirmed his hematoma to be stable.
After a 48-h observation period, the patient was discharged from the hospital and his hemoglobin was 109 g/L (Normal: 134-170 g/L). The patient was contacted two, four and eight weeks after discharge. His evolution was uneventful. He was also eating normally.
Since its development, POEM is considered as an efficient procedure in the treatment of achalasia[1]. It has also evolved as a therapeutic modality in cases of achalasia recurrence after a surgical approach[10].
POEM appears to have a lower morbidity than the surgical approach[1]. Various complications have been reported with POEM including mucosal injuries, esophageal leak, bleeding or submucosal hematoma, chest pain or empyema. The most frequently reported complications are related to insufflation (capnoperitoneum, capnothorax and capnomediastinum), but these are usually minor[2]. A recent multicentric study reported the global and severe adverse events to be 7.5% and 0.5%, respectively[2]. Reported cases of hemorrhage were limited to esophagus or stomach[2]. To our knowledge, no cases of splenic injury have been reported to date in the literature.
Although splenic rupture is very rare, it is a known complication after colonoscopy[4]. It occurs secondary to the traction that is exerted on the splenocolic ligament either upon advancing or retrieving the colonoscope, leading to capsular lacerations and avulsions.
Cases of splenic rupture have been reported secondary to endoscopic retrograde cholangiography[3]. Splenic injury occurring during this procedure is most likely due to looping of the endoscope and scope-related direct traction or shear forces on the greater curvature of the stomach, short gastric vessels, and splenic capsule[3].
However, this phenomenon of splenic injury is rare during flexible gastroscopy. Such a case was previously described in a patient with a gastric ulcer[6] and also in another patient with a tumor at the esophagogastric junction[5]. In both these cases, endoscopic exams were reported to be easy and no technical factor could evidently explain the splenic injury[5,6].
The precise underlying causes for splenic injury after gastroscopy remain unknown. Bowing of the endoscope along the greater curvature of the stomach can cause avulsion of the gastrosplenic ligament and/or short gastric vessels[3,6]. Some propose that the splenic injury can be caused by insufflation as well as the excessive retching experienced during the procedure, which could result in stretching of the peri-gastric ligaments[5]. In the present case, the procedure was carried out under general anesthesia, and the patient did not have significant nausea or vomiting after surgery. Moreover, no gastric pushing with the endoscope during the intervention was necessary and, despite the relatively long-time procedure, carbon dioxide insufflation significantly prevented distension. While all the other reported cases of splenic rupture following an upper endoscopy splenic rupture occurred immediately after the procedure[3,5-9], the latency for the onset of symptoms may share some similarity to the delayed splenic rupture that occurs after colonoscopy[4,11] or trauma[12].
Three cases of splenic laceration have previously been described after esophageal procedures and manipulation. A case of splenic injury was reported after placing a feeding tube through an extrinsic, probably neoplastic, stenosis of the middle esophagus using a 5.2 mm-gastroscope[9]. A second case of a splenic rupture was described after bougienage through a neoplastic stenosis at the GEJ[8]. Finally, a third case of splenic rupture occurred in a patient with a tortuous esophagus, narrowing of the esophageal sphincter, and enormous, almost completely intrathoracic stomach[7]. When performing a POEM, some force exerted at the GEJ, while forming submucosal tunnel at the tight distal esophagus, due to the hypertonicity of the inferior esophageal sphincter, could possibly contribute to splenic injury. However, this could not have been the cause in our case as we did not experience any unusual or specific difficulty during the procedure. Nevertheless, manipulation at the GEJ seems to be a constant adjunct to the mechanism of splenic injury[7-9].
A previous Heller myotomy along with a posterior partial anti-reflux procedure (Toupet) was carried out more than fifteen years ago in our patient. Earlier scarring around the GEJ and fundus might have inadvertently contributed to the splenic injury in this case. Not all the short gastric vessels could be divided during the previous fundoplication, and thus could be overstretched and became susceptible to bleeding. The exact mechanism that contributed to the splenic rupture is yet to be elucidated. Previous surgery is identified as a known risk factor of splenic rupture after colonoscopy[4]. However, these cases of splenic rupture after upper gastro-intestinal procedures in patients with previous surgery[3] are anecdotal, similar to the present case, and no conclusion can be drawn about antecedent surgery as a significant contributing factor.
In the last ten years, POEM stands-out as the eventual treatment of choice of esophageal achalasia[1]. Thousands of cases have been reported and audited[2]. Cases of repeated POEM, after either endoscopic or surgical procedures, have been reported and evaluated[10]. Not even a single case of splenic rupture has been reported, reflecting the safety of POEM but this adverse event deserves consideration when more procedures will be done in the future by this approach.
This is the first reported case of splenic rupture after POEM. This very unusual but severe complication will probably occur again as this procedure will continue to be developed and implemented. Physicians must be aware that splenic rupture can happen after POEM and pay specific attention in patients with previous Heller myotomy.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Canada
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gurala D, Visaggi P S-Editor: Fan JR L-Editor: A P-Editor: Wang LL
| 1. | Werner YB, Hakanson B, Martinek J, Repici A, von Rahden BHA, Bredenoord AJ, Bisschops R, Messmann H, Vollberg MC, Noder T, Kersten JF, Mann O, Izbicki J, Pazdro A, Fumagalli U, Rosati R, Germer CT, Schijven MP, Emmermann A, von Renteln D, Fockens P, Boeckxstaens G, Rösch T. Endoscopic or Surgical Myotomy in Patients with Idiopathic Achalasia. N Engl J Med. 2019;381:2219-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 344] [Article Influence: 57.3] [Reference Citation Analysis (1)] |
| 2. | Haito-Chavez Y, Inoue H, Beard KW, Draganov PV, Ujiki M, Rahden BHA, Desai PN, Pioche M, Hayee B, Haji A, Saxena P, Reavis K, Onimaru M, Balassone V, Nakamura J, Hata Y, Yang D, Pannu D, Abbas A, Perbtani YB, Patel LY, Filser J, Roman S, Rivory J, Mion F, Ponchon T, Perretta S, Wong V, Maselli R, Ngamruengphong S, Chen YI, Bukhari M, Hajiyeva G, Ismail A, Pieratti R, Kumbhari V, Galdos-Cardenas G, Repici A, Khashab MA. Comprehensive Analysis of Adverse Events Associated With Per Oral Endoscopic Myotomy in 1826 Patients: An International Multicenter Study. Am J Gastroenterol. 2017;112:1267-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 144] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 3. | Lee R, Huelsen A, Saad N, Hodgkinson P, Hourigan LF. Splenic Injury Following Endoscopic Retrograde Cholangiopancreatography: A Case Report and Literature Review. Case Rep Gastroenterol. 2017;11:241-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Jehangir A, Poudel DR, Masand-Rai A, Donato A. A systematic review of splenic injuries during colonoscopies: Evolving trends in presentation and management. Int J Surg. 2016;33 Pt A:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Estevez-Boullosa P, Alonso-Aguirre PA, Couto-Worner I, Blanco-Rodriguez M, de Llano-Monelos P, Sanchez-Gonzalez F. Splenic rupture following a diagnostic upper endoscopy. World J Gastrointest Endosc. 2010;2:235-236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Eter A, Belliveau R. A Very Rare Cause of Splenic Injury: Splenic Hematoma Following a Diagnostic Upper Endoscopy (Esophagogastroduodenoscopy) and Biopsy of Gastric Ulcer. J Clin Med Res. 2020;12:269-271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Jabr F, Skeik N. Spleen rupture complicating upper endoscopy. Endoscopy. 2012;44 Suppl 2 UCTN:E206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Goertz RS, Raithel M, Strobel D, Wehler M, Janka R, Wein A, Maennlein G, Hahn EG, Boxberger F. Splenic rupture as a complication of endoscopic esophageal bouginage. Endoscopy. 2009;41 Suppl 2:E228-E229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Cardoso MF, Alexandrino G, Carvalho R. Splenic Rupture following Transnasal Endoscopy. GE Port J Gastroenterol. 2019;26:300-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Fernandez-Ananin S, Fernández AF, Balagué C, Sacoto D, Targarona EM. What to do when Heller's myotomy fails? J Minim Access Surg. 2018;14:177-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Nimmons W, Getto LP. Delayed presentation of splenic rupture after colonoscopy. Am J Emerg Med 2020; 38: 1043.e5-1043. e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Harmon L, Bilow R, Shanmuganathan K, Lauerman M, Todd SR, Cardenas J, Haugen CE, Albrecht R, Pittman S, Cohen M, Kaups K, Dirks R, Burlew CC, Fox CJ, Con J, Inaba K, Harrison PB, Berg GM, Waller CJ, Kallies KJ, Kozar RA. Delayed splenic hemorrhage: Myth or mystery? Am J Surg. 2019;218:579-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |