Published online Jun 16, 2020. doi: 10.4253/wjge.v12.i6.193
Peer-review started: March 3, 2020
First decision: April 22, 2020
Revised: April 25, 2020
Accepted: May 16, 2020
Article in press: May 16, 2020
Published online: June 16, 2020
Processing time: 104 Days and 13.1 Hours
Endoscopic full-thickness resection of adenomas or subepithelial tumors is a novel and promising endoscopic technique. There have been several recent studies of full-thickness resection device (FTRD) use in the colon, but data regarding its use and efficacy in the duodenum are still limited.
A 64-year-old female underwent resection of a recurrent adenoma of 7 mm in size in the duodenum after FTRD use for an adenoma eight months prior. The biopsies revealed a low-grade adenoma. The adenoma was removed using the gastroduodenal FTRD, and the pathology results revealed clear margins. Except for minor bleeding that was treated by argon plasma coagulation, no further complications occurred.
Repeat use of the FTRD appears to be a safe and efficacious approach for the treatment of recurrent duodenal lesions. Further prospective studies are needed to investigate the long-term safety and utility of repeat FTRD use after Endoscopic full-thickness resection.
Core tip: Endoscopic full-thickness resection using the full-thickness resection device (FTRD) is a promising technique for resection of adenomas but has not been extensively investigated in duodenal adenomas. We present a case of a recurrent duodenal adenoma after previous full-thickness resection with successful use of repeat FTRD.
- Citation: Gericke M, Mende M, Schlichting U, Niedobitek G, Faiss S. Repeat full-thickness resection device use for recurrent duodenal adenoma: A case report. World J Gastrointest Endosc 2020; 12(6): 193-197
- URL: https://www.wjgnet.com/1948-5190/full/v12/i6/193.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i6.193
Adenomas in the duodenum can develop spontaneously or are associated hereditary syndromes. Approximately 5% of adenomas in the duodenum transform into carcinomas; therefore, resection should be performed[1]. Compared to endoscopic resection, a surgical approach has disadvantages owing to its higher morbidity[2]. However, endoscopic resection harbours a significant risk of complications such as perforation or bleeding[3-7]. Endoscopic full-thickness resection (EFTR) using the full-thickness resection device (FTRD) (Ovesco Endoscopy AG, Tübingen, Germany) has shown safety and efficacy in colorectal lesions[8-10]. The technical success and safety of EFTR in the duodenum have been shown in previous studies[11-14]. The new gastroduodenal FTRD (Ovesco Endoscopy AG, Tübingen, Germany) was recently approved by the Communauté Européenne for EFTR of gastroduodenal lesions.
A 64-year-old Caucasian female was admitted to our department for planned resection of a re-recurrent adenoma with the non-lifting sign in the pars horizontalis of the duodenum. Endoscopic mucosal resection (EMR) of a duodenal adenoma was performed in 2014. A recurrent adenoma was R0 resected eight months prior to admission with the colonic FTRD without any complications. There was no personal or family history of gastrointestinal cancer.
Physical examination was unremarkable and revealed a comfortable lady without any abdominal tenderness on examination. Complete blood count, complete metabolic panel and prothrombin time/international normalised ratio was all within normal limits. An esophagogastroduodenoscopy (EGD) was performed which revealed a normal esophagus and stomach. A recurrent adenoma with a non-lifting sign (7 mm) was found in the pars horizontalis of the duodenum and was biopsied.
Pathologic examination revealed a recurrent adenoma in the duodenum with low-grade dysplasia.
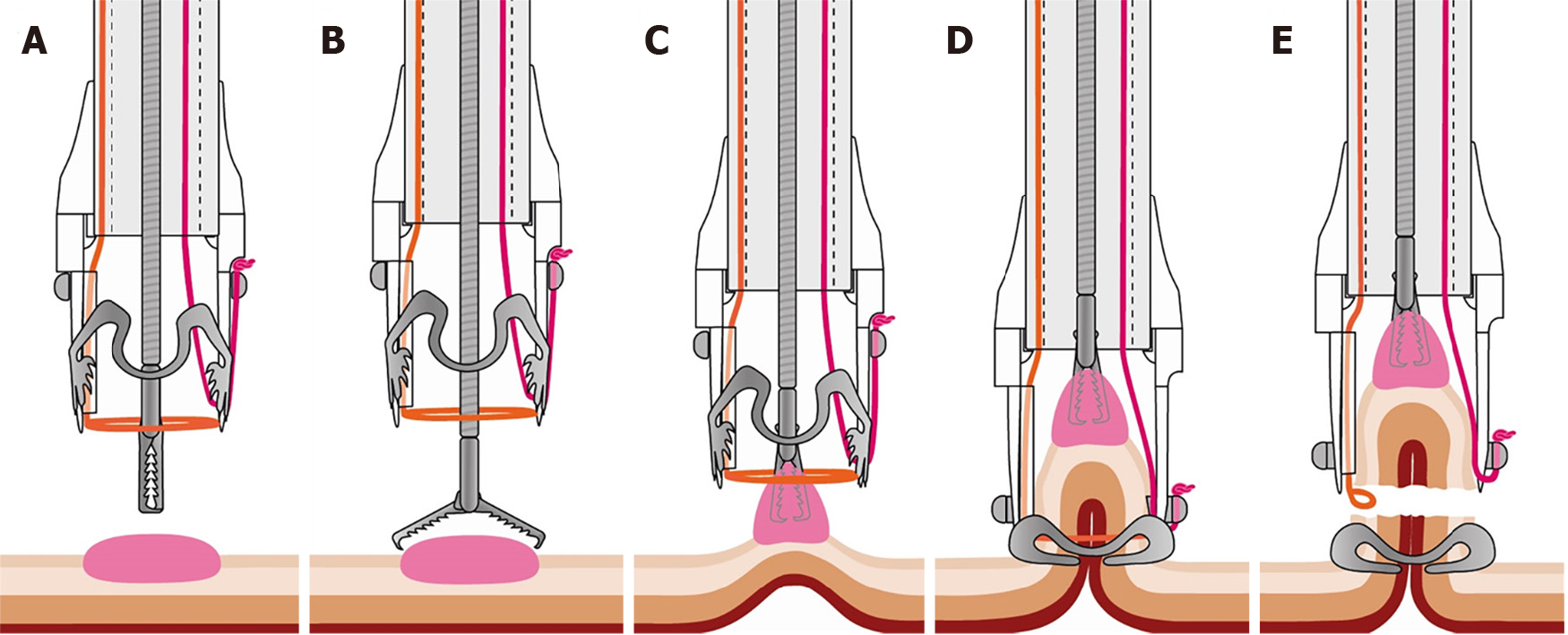
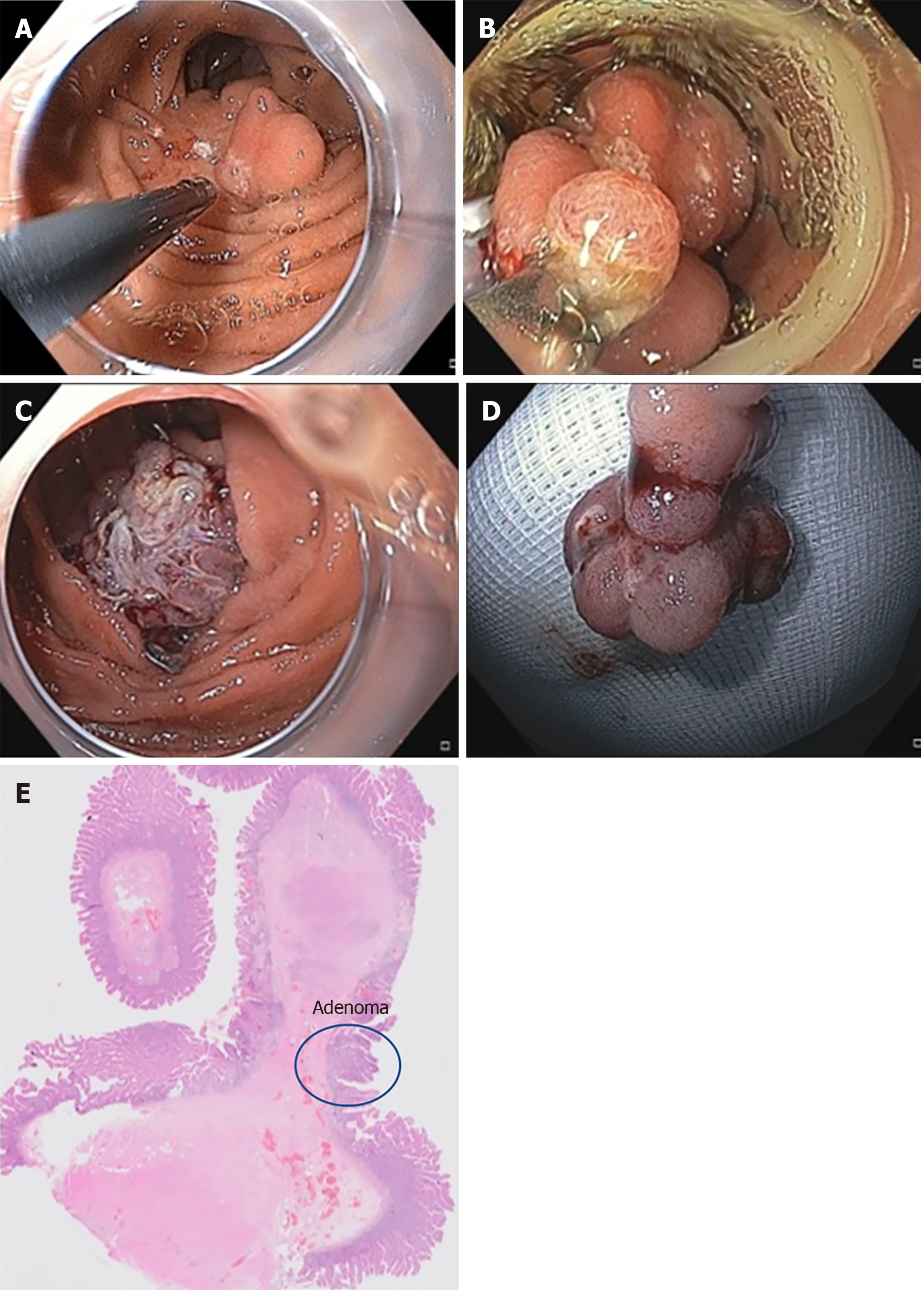
Before resection, the margins of the adenoma were marked with argon plasma coagulation (APC) with a standard gastroscope. Then, we switched to the gastroduodenal FTRD. Passage through the upper esophageal sphincter and pylorus was possible without balloon dilatation. The grasping forceps were advanced through the working channel. The lesion was pulled into the cap to incorporate a double, full-thickness layer of the duodenal wall. An over-the-scope clip (OTSC) was then deployed, and the tissue above the clip was immediately resected with the snare. The resected adenoma was retrieved (Figures 1 and 2). The procedure was performed under sedation with propofol. A control EGD, one day later, showed a correctly placed OTSC. Minor contact bleeding was treated by APC and there was no sign of perforation. The patient was discharged after three days without further complications.
Pathologic examination revealed a full-thickness, complete (R0) resection of a 7 mm low-grade dysplasia. There was no evidence of malignancy. A follow-up EGD four months later revealed that the OTSC was in place. Multiple biopsies did not show evidence of recurrent adenoma cells.
Endoscopic resection of adenomas or subepithelial tumors in the duodenum is more difficult than resection of such lesions in the colon. The risk of bleeding and perforation is higher due to the thinner duodenal wall and its retroperitoneal fixation[3-7]. However, endoscopic resection of duodenal lesions has a lower morbidity than a surgical approach, which often leads to extensive resections[2]. With conventional EMR as the current standard technique, complete resection rates are up to 96%[5]. The risk of periprocedural bleeding is up to 25%, with the risk of delayed bleeding being up to 12%[3,4]. Perforation rates are low, between 0.6%-5%[3,5]. EMR of adenomas with non-lifting signs or subepithelial tumors seems to be very challenging or impossible. Endoscopic submucosal dissection (ESD) in the duodenum has a high risk of perforation up to 35%; for this reason, duodenal ESD is not recommended[5,15].
EFTR is another reasonable technique for resection of non-lifting adenomas or submucosal tumors. FTRD in the colorectum has proven efficacy and safety[8-10]. EFTR in the duodenum with the FTRD has shown promising results in previous studies in patients with “difficult” adenomas (such as adenomas with non-lifting signs) or subepithelial tumors[11,12,14]. Minor bleeding occurred in approximately 20% of patients, whilst no major bleeding or perforation was detected. At our institution, a control gastroscopy is performed one day after FTRD in the upper gastrointestinal tract to exclude major bleedings or perforations. Bauder et al[12] reported an R0 resection rate of 53.8% in duodenal adenomas, with higher “clinical” success rates in control endoscopies.
In this case, we have shown successful repeat FTRD use for a recurrent adenoma after EFTR in the duodenum. Due to the risks of conventional endoscopic techniques and the disadvantage of the lack of a histological work-up when using APC, we opted to use the FTRD. Since the recurrence rates of duodenal adenomas are low, it remains unclear why there was recurrence after EFTR with proven R0 resection[6]. One possible explanation is the release of a metastatic seed of adenomatous tissue during the prior FTRD procedure.
We report a successful recurrent EFTR of a duodenal adenoma using the gastroduodenal FTRD. The gastroduodenal FTRD has an outer diameter of 19.5 mm, 1.5 mm thinner than the colonic FTRD. A guide wire and balloon for dilatation were integrated. A limitation of the FTRD in the upper gastrointestinal tract is the possible need for balloon dilation of the upper esophageal sphincter and pylorus to allow passage of the device, which can be challenging. The FTRD should not be used for lesions in the ampullary duodenum due to the risk of clipping of the common bile duct accidently. We advise localizing the papilla before EFTR and observing a safety distance of a minimum of 20 mm.
To our experience, elective removal of the OTSC is not mandatory unless complications such as obstruction of the duodenal lumen, clipping of extraluminal tissues, ulceration of the surrounding area or patient discomfort occur. Due to the limited number of patients treated with the FTRD in the duodenum, the incidence of complications cannot be evaluated properly.
The gastroduodenal FTRD is a promising new device that makes it possible to resect “difficult” lesions not suitable for EMR and thus avoids surgery even if prior EFTR is performed. Prospective studies are needed to investigate the safety and efficacy of the FTRD in the duodenum.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Casadesus D, Cui J, Viswanath YKS S-Editor: Wang J L-Editor: A E-Editor: Li X
| 1. | Okada K, Fujisaki J, Kasuga A, Omae M, Kubota M, Hirasawa T, Ishiyama A, Inamori M, Chino A, Yamamoto Y, Tsuchida T, Nakajima A, Hoshino E, Igarashi M. Sporadic nonampullary duodenal adenoma in the natural history of duodenal cancer: a study of follow-up surveillance. Am J Gastroenterol. 2011;106:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 121] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 2. | Perez A, Saltzman JR, Carr-Locke DL, Brooks DC, Osteen RT, Zinner MJ, Ashley SW, Whang EE. Benign nonampullary duodenal neoplasms. J Gastrointest Surg. 2003;7:536-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Aschmoneit-Messer I, Richl J, Pohl J, Ell C, May A. Prospective study of acute complication rates and associated risk factors in endoscopic therapy for duodenal adenomas. Surg Endosc. 2015;29:1823-1830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Nonaka S, Oda I, Tada K, Mori G, Sato Y, Abe S, Suzuki H, Yoshinaga S, Nakajima T, Matsuda T, Taniguchi H, Saito Y, Maetani I. Clinical outcome of endoscopic resection for nonampullary duodenal tumors. Endoscopy. 2015;47:129-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Yamasaki Y, Uedo N, Takeuchi Y, Ishihara R, Okada H, Iishi H. Current Status of Endoscopic Resection for Superficial Nonampullary Duodenal Epithelial Tumors. Digestion. 2018;97:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Valli PV, Mertens JC, Sonnenberg A, Bauerfeind P. Nonampullary Duodenal Adenomas Rarely Recur after Complete Endoscopic Resection: A Swiss Experience Including a Literature Review. Digestion. 2017;96:149-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Lim CH, Cho YS. Nonampullary duodenal adenoma: Current understanding of its diagnosis, pathogenesis, and clinical management. World J Gastroenterol. 2016;22:853-861. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Schmidt A, Beyna T, Schumacher B, Meining A, Richter-Schrag HJ, Messmann H, Neuhaus H, Albers D, Birk M, Thimme R, Probst A, Faehndrich M, Frieling T, Goetz M, Riecken B, Caca K. Colonoscopic full-thickness resection using an over-the-scope device: a prospective multicentre study in various indications. Gut. 2018;67:1280-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 205] [Article Influence: 29.3] [Reference Citation Analysis (2)] |
| 9. | Valli PV, Mertens J, Bauerfeind P. Safe and successful resection of difficult GI lesions using a novel single-step full-thickness resection device (FTRD®). Surg Endosc. 2018;32:289-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 10. | Aepli P, Criblez D, Baumeler S, Borovicka J, Frei R. Endoscopic full thickness resection (EFTR) of colorectal neoplasms with the Full Thickness Resection Device (FTRD): Clinical experience from two tertiary referral centers in Switzerland. United European Gastroenterol J. 2018;6:463-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 11. | Schmidt A, Meier B, Cahyadi O, Caca K. Duodenal endoscopic full-thickness resection (with video). Gastrointest Endosc. 2015;82:728-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | Bauder M, Schmidt A, Caca K. Endoscopic full-thickness resection of duodenal lesions-a retrospective analysis of 20 FTRD cases. United European Gastroenterol J. 2018;6:1015-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 13. | Kappelle WFW, Backes Y, Valk GD, Moons LMG, Vleggaar FP. Endoscopic full-thickness resection of gastric and duodenal subepithelial lesions using a new, flat-based over-the-scope clip. Surg Endosc. 2018;32:2839-2846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 14. | Andrisani G, Di Matteo FM. Endoscopic full-thickness resection of duodenal lesions (with video). Surg Endosc. 2020;34:1876-1881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Yamamoto H, Miura Y. Duodenal ESD: conquering difficulties. Gastrointest Endosc Clin N Am. 2014;24:235-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |