Published online Mar 16, 2020. doi: 10.4253/wjge.v12.i3.111
Peer-review started: November 6, 2019
First decision: November 20, 2019
Revised: November 29, 2019
Accepted: December 23, 2019
Article in press: December 23, 2019
Published online: March 16, 2020
Processing time: 127 Days and 2.8 Hours
The healthcare impact of obesity is enormous, and there have been calls for new approaches to containing the epidemic worldwide. Minimally invasive procedures have become more popular, with one of the most widely used being endoscopic sleeve gastroplasty (ESG). Although major adverse events after ESG are rare, some can cause considerable mortality. To our knowledge, there has been no previous report of biliary ascites after ESG.
A 48-year-old female with obesity refractory to lifestyle changes and prior gastric balloon placement underwent uncomplicated ESG and was discharged on the following day. On postoperative day 3, she developed abdominal pain, which led to an emergency department visit the following day. She was readmitted to the hospital, with poor general health status and signs of peritoneal irritation. Computed tomography imaging showed fluid in the abdominal cavity. Laparoscopy revealed biliary ascites and showed that the gallbladder was sutured to the gastric wall. The patient underwent cholecystectomy and lavage of the abdominal cavity and was admitted to the intensive care unit post-operatively. After 7 d of antibiotic therapy and 20 d of hospitalization, she was discharged. Fortunately, 6 mo later, she presented in excellent general condition and with a 20.2% weight loss.
ESG is a safe procedure. However, adverse events can still occur, and precautions should be taken by the endoscopist. In general, patient position, depth of tissue acquisition, location of stitch placement, and endoscopist experience are all important factors to consider to mitigate procedural risk.
Core tip: Despite broader acceptance of endoscopic sleeve gastroplasty for weight loss management, the procedure can still present challenges for endoscopists. Although the inadvertent puncture of organs adjacent to the stomach is a rare occurrence, it can lead to catastrophic outcomes. Early identification of possible unintended events and an assertive approach to case management can be life-saving. Patient selection and optimal technique remain under debate. With broader adoption of endoscopic sleeve gastroplasty worldwide, risk mitigation strategies must be emphasized to optimize procedural safety.
- Citation: de Siqueira Neto J, de Moura DTH, Ribeiro IB, Barrichello SA, Harthorn KE, Thompson CC. Gallbladder perforation due to endoscopic sleeve gastroplasty: A case report and review of literature. World J Gastrointest Endosc 2020; 12(3): 111-118
- URL: https://www.wjgnet.com/1948-5190/full/v12/i3/111.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i3.111
Obesity is a disease of great social and financial impact which can lead to significant health conditions, such as cardiovascular disease, non-alcoholic steatohepatitis, osteoarthritis, obstructive sleep apnea, depression, and gastroesophageal reflux disease[1-3]. In recent years, endoscopic procedures have begun to fill the large gap between medical and surgical treatments aimed at controlling this disease[4,5]. One of the recently developed procedures is endoscopic sleeve gastroplasty (ESG), which is performed with a suturing device coupled to the distal tip of an endoscope enabling placement of full thickness sutures in the gastric wall to alter the form and function of the stomach.
Although ESG is considered to be a safe procedure[6-8], various major and minor adverse events have been described[9]. According to previous studies, the most common symptoms occurring after ESG are nausea, vomiting, and mild-to-moderate abdominal pain[9-11]. Severe adverse events, such as peritoneal fluid collections requiring drainage or surgical intervention, gastrointestinal or intraabdominal hemorrhage requiring intervention or transfusion, or severe abdominal pain are rare, occurring in only 0-2% of reported cases[9-12].
To our knowledge, only one prior case of biliary peritonitis during ESG has been reported[13], however, ascites was not described in this case. Our case of gallbladder perforation and biliary ascites was identified early and appropriately managed leading to a favorable outcome for the patient, similar to the aforementioned case. Given the rapid increase in the number of ESG procedures worldwide, it is imperative to document and educate one another on adverse events to reduce their rate of occurrence and minimize the morbidity associated with the procedure.
A 48-year-old female with obesity and with various comorbidities.
A 48-year-old female with obesity was referred for consideration of ESG. She had a medical history significant for hypertension that was controlled with oral agents. She had no prior history of bariatric surgery. At initial presentation, her weight was 93 kg, with a body mass index of 31.4 kg/m2, despite lifestyle changes and prior placement of a gastric balloon.
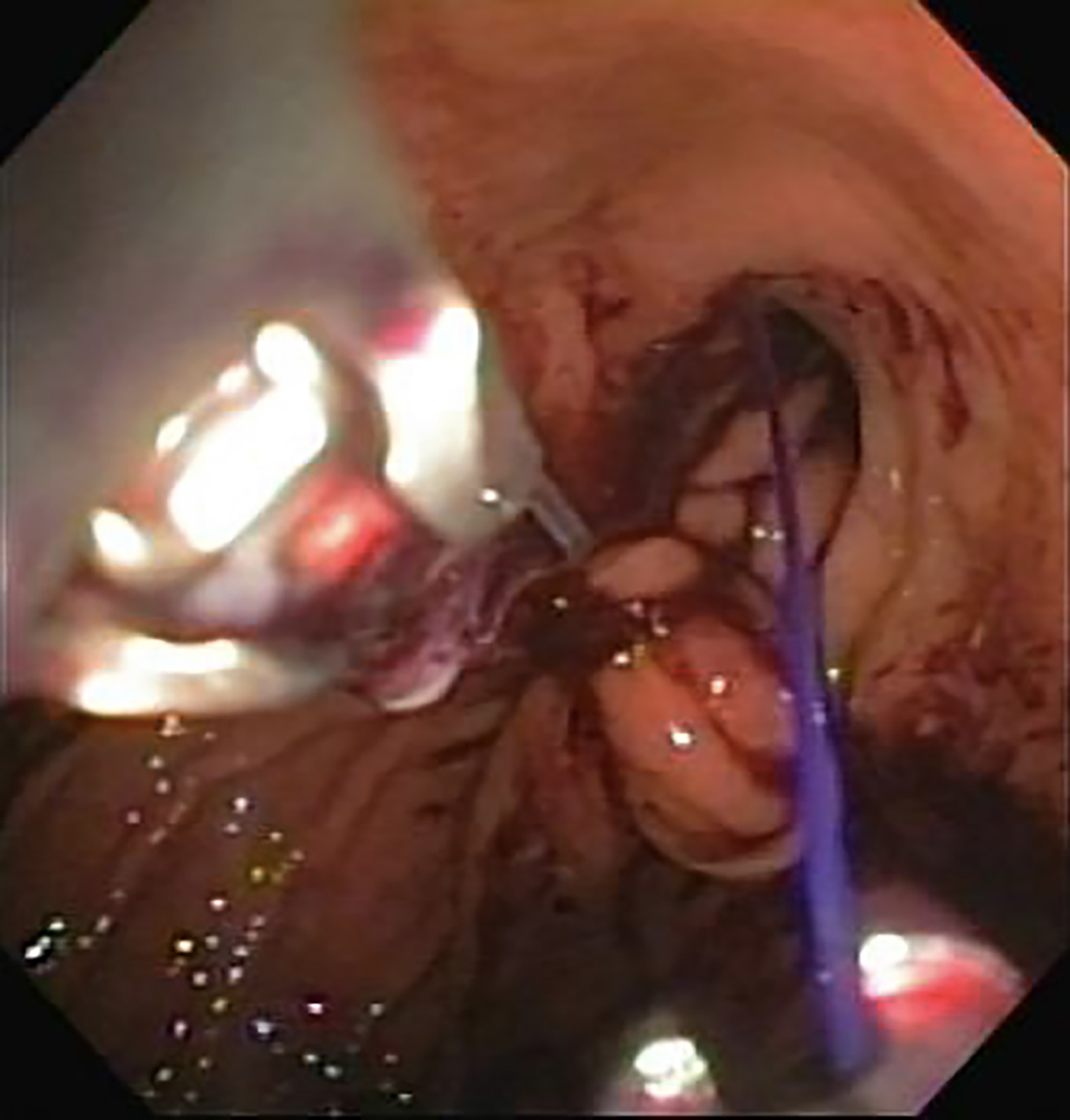
The patient gave written informed consent, after which she underwent ESG at a private hospital (Hospital Meridional, Cariacica, ES, Brazil). This was the first ESG performed at this center. There were no immediate procedural related complications. The procedure was performed under general anesthesia, with an endoscopic suturing system (OverStitch endosuturing device; Apollo Endosurgery, Austin, TX, United States) coupled to a dual-channel endoscope (GIF-2T160; Olympus America, Center Valley, PA, United States). Carbon dioxide insufflation was used. A full thickness U-shaped suture pattern was used by the physician to perform ESG, as previously described[10] (Figure 1). A total of five sutures were used.
In the immediate postoperative period, the patient was treated daily with antiemetics (ondansetron, dimenhydrinate, dexamethasone, and scopolamine), as well as dipyrone and omeprazole. The patient was discharged on post-operative day 1, in good condition and without any complaints, with prescriptions for omeprazole, ondansetron, dipyrone, scopolamine, and codeine phosphate combined with acetaminophen if necessary.
On postoperative day 3, the patient developed abdominal pain which continued to worsen over the next 24 h; thus, she was referred to the emergency department for further evaluation.
Obesity and hypertension.
Physical examination was normal preoperatively. On the fourth postoperative day, the patient had a rigid abdomen with signs of peritoneal irritation.
On the fourth postoperative day and admission to the emergency department, the patient had significant leukocytosis (19800 × 103 leukocytes/µL) and an increased C-reactive protein level (147 mg/L).
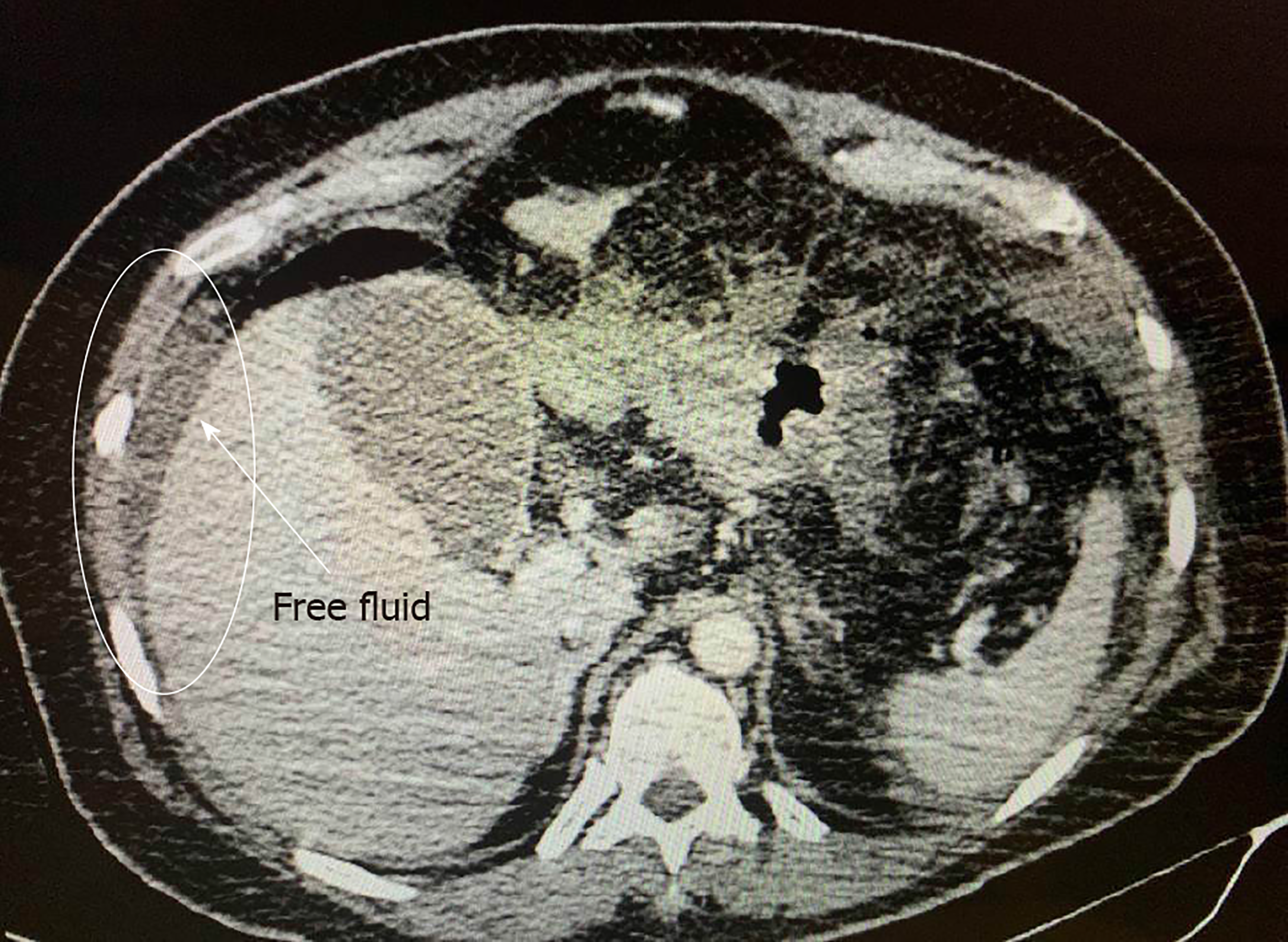
At the emergency entrance, computed tomography imaging revealed free fluid in the peritoneal cavity (Figure 2).
The patient was diagnosed with biliary ascites caused by inadvertent puncture of the gallbladder.
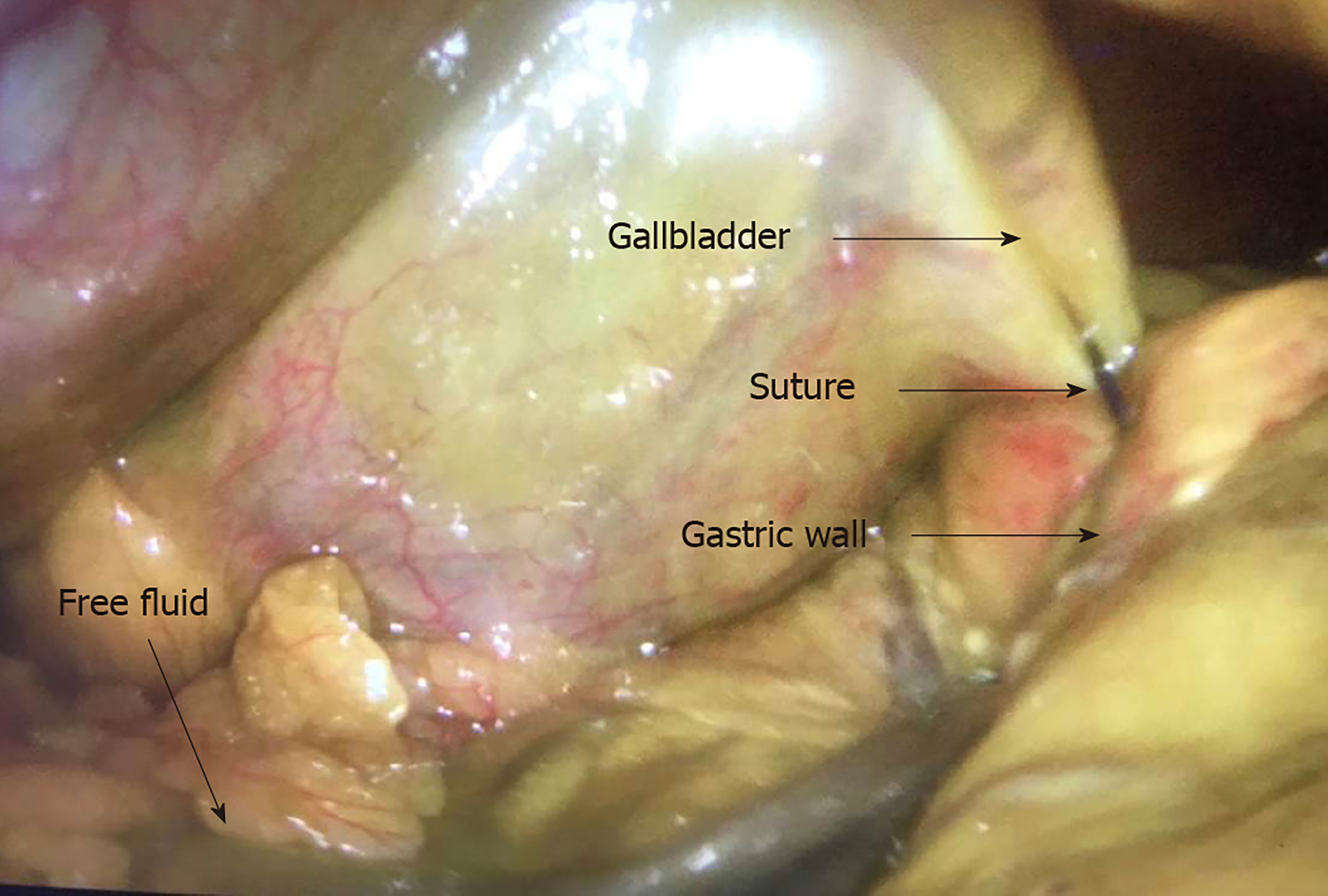
Patient was taken for emergent diagnostic laparoscopy. In addition to the biliary ascites, the stomach appeared to be tubular in shape as expected post-ESG. After significant lavage of the peritoneal cavity, it was noted that the fundus of the gallbladder was transfixed to the stomach (Figure 3). Biliary fluid collections were identified throughout the upper abdomen (Figure 4). Thus, the suture was cut and laparoscopic cholecystectomy was performed. At the conclusion of the case, intraoperative endoscopy with a methylene blue test was performed, finding no evidence of additional complications.
The patient was admitted to the intensive care unit, where she remained for one week, requiring IV antibiotics for septic shock. She did not require further surgical intervention. She ultimately improved from an infectious perspective, and was discharged to home 20 d after her initial admission to the hospital.
At the time of this case report (Table 1), the patient continued to follow in the outpatient clinic, and had no further complications related to the procedure. She had lost 18.7 kg (20.2% of her total body weight) in the first six months after the ESG. She was still undergoing interdisciplinary follow-up with a nutritionist, a psychologist, and a physical therapist.
| Time line | |
| 1 | Patient underwent endoscopic sleeve gastroplasty with no complications |
| 2 | On postoperative day 3, she developed abdominal pain, which led to an emergency department visit on postoperative day |
| 3 | She was readmitted to the hospital, with poor general health status and signs of peritoneal irritation |
| 4 | Computed tomography showed fluid in the abdominal cavity |
| 5 | Laparoscopy revealed biliary ascites and showed that the gallbladder was sutured to the gastric wall |
| 6 | The patient underwent cholecystectomy, together with review and lavage of the abdominal cavity, and was admitted to the intensive care unit |
| 7 | After 7 d of antibiotic therapy and 20 d of hospitalization, she was discharged |
| 8 | Of 6 mo later, she presented excellent general condition and a 20.2% weight loss |
Endoscopic treatment of obesity has begun to rapidly fill the gap between medical and surgical therapies, as endoscopic therapy provides a minimally invasive option, which has greater efficiency than medical interventions and a greater safety profile than open surgical interventions[14-17]. The advent of endoscopic suturing was a major step forward in the minimally invasive treatment of a number of gastrointestinal pathologies[18,19]. The OverStitch Endosuturing device has stood out from other such systems and is currently the only system in widespread use[8]. Since 2001, endoscopic suturing systems have been adapted for the treatment of obesity, as experiments in ex vivo animal models have led to the development of the systems and techniques in use today[20]. In ESG, full thickness sutures are placed throughout the gastric body to bring the anterior wall, greater curvature, and posterior wall of the gastric body all closer together, resulting in a tubular configuration[8], in a manner similar to that achieved with surgical sleeve gastrectomy. The technique has been improving since 2012, when Thompson and Hawes performed the first ESG[11,21]. Since then, Abu Dayyeh et al[22] and Sharaiha et al[23] confirmed the technical feasibility of the procedure, as well as its safety and efficacy for weight reduction.
Minor adverse events, such as nausea, vomiting, and mild-to-moderate abdominal pain are the most common symptoms following ESG. In a study involving 1000 patients whom underwent ESG, Alqahtani et al[10] observed minor adverse events in 92.2% of patients. However, while there were high rates of minor adverse events reported, there were very few major adverse events associated with the procedure[10]. A recently published review article on the topic by Jain et al[24] evaluated nine original articles and confirmed that there was a high incidence of minor adverse events, while similarly demonstrated a low rate of major adverse events, seen only in 2.3% of cases. Of note, there was no incidence of biliary injury or ascites described in this analysis.
Despite an exhaustive search of the literature, we found no reports of death related to the procedure. Readmissions due to upper gastrointestinal hemorrhage requiring endoscopic intervention or administration of blood products occur only occasionally, having a minimal impact on morbidity and length of hospital stay[10,25]. Among the major adverse events occurring after ESG, leaks and peritoneal fluid collections are most common, having been reported in various studies in the literature[7,10,11,25-30]. In most cases, the complication was treated conservatively or by image-guided percutaneous drainage.
On detailed review of this case, there were several factors that may have contributed to this adverse event. There is a learning curve associated with any endoscopic procedure, including ESG, and this case was the very first ESG performed by the endoscopist. Despite this procedure being performed under the supervision of an experienced proctor, this may have contributed. Additionally, the patient was in the “swimmers” position, instead of a more conventional supine, lazy left-lateral position, which may have brought the stomach and gallbladder into closer proximity, thus increasing the risk of gallbladder perforation with a full-thickness gastric suturing technique. And finally, we believe that the suturing was started in close proximity to the lesser curvature of the stomach, which could have also increased the risk of biliary injury.
As described in this case report, biliary ascites after ESG should be considered as a rare but major adverse event of great clinical severity. The treatment team must maintain a high level of diagnostic suspicion in a patient presenting with fever and abdominal pain following ESG. Timely, aggressive therapy must be taken to minimize long term sequelae.
Although rare, gallbladder perforation can occur during ESG, and can have significant clinical consequences. Further studies, focusing on patient positioning, use of anatomic landmarks to guide suture patterns, and learning curve should be performed to further reduce the occurrence of adverse events such as the one described here.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Galloro G, Martini F S-Editor: Yan JP L-Editor: A E-Editor: Liu JH
| 1. | GBD 2015 Obesity Collaborators. Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, Salama JS, Vos T, Abate KH, Abbafati C, Ahmed MB, Al-Aly Z, Alkerwi A, Al-Raddadi R, Amare AT, Amberbir A, Amegah AK, Amini E, Amrock SM, Anjana RM, Ärnlöv J, Asayesh H, Banerjee A, Barac A, Baye E, Bennett DA, Beyene AS, Biadgilign S, Biryukov S, Bjertness E, Boneya DJ, Campos-Nonato I, Carrero JJ, Cecilio P, Cercy K, Ciobanu LG, Cornaby L, Damtew SA, Dandona L, Dandona R, Dharmaratne SD, Duncan BB, Eshrati B, Esteghamati A, Feigin VL, Fernandes JC, Fürst T, Gebrehiwot TT, Gold A, Gona PN, Goto A, Habtewold TD, Hadush KT, Hafezi-Nejad N, Hay SI, Horino M, Islami F, Kamal R, Kasaeian A, Katikireddi SV, Kengne AP, Kesavachandran CN, Khader YS, Khang YH, Khubchandani J, Kim D, Kim YJ, Kinfu Y, Kosen S, Ku T, Defo BK, Kumar GA, Larson HJ, Leinsalu M, Liang X, Lim SS, Liu P, Lopez AD, Lozano R, Majeed A, Malekzadeh R, Malta DC, Mazidi M, McAlinden C, McGarvey ST, Mengistu DT, Mensah GA, Mensink GBM, Mezgebe HB, Mirrakhimov EM, Mueller UO, Noubiap JJ, Obermeyer CM, Ogbo FA, Owolabi MO, Patton GC, Pourmalek F, Qorbani M, Rafay A, Rai RK, Ranabhat CL, Reinig N, Safiri S, Salomon JA, Sanabria JR, Santos IS, Sartorius B, Sawhney M, Schmidhuber J, Schutte AE, Schmidt MI, Sepanlou SG, Shamsizadeh M, Sheikhbahaei S, Shin MJ, Shiri R, Shiue I, Roba HS, Silva DAS, Silverberg JI, Singh JA, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tegegne BS, Terkawi AS, Thakur JS, Tonelli M, Topor-Madry R, Tyrovolas S, Ukwaja KN, Uthman OA, Vaezghasemi M, Vasankari T, Vlassov VV, Vollset SE, Weiderpass E, Werdecker A, Wesana J, Westerman R, Yano Y, Yonemoto N, Yonga G, Zaidi Z, Zenebe ZM, Zipkin B, Murray CJL. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377:13-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5669] [Cited by in RCA: 5068] [Article Influence: 633.5] [Reference Citation Analysis (2)] |
| 2. | Hourneaux De Moura DT, Thompson CC. Endoscopic management of weight regain following Roux-en-Y gastric bypass. Expert Rev Endocrinol Metab. 2019;14:97-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Ribeiro IB, Gestic MA, Utrini MP, Chaim FDM, Chaim EA, Cazzo E. Drain amylase levels may indicate gastrojejunostomy leaks after roux-en-y gastric bypass. Arq Gastroenterol. 2018;55:66-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | de Almeida LS, Bazarbashi AN, de Souza TF, de Moura BFBH, de Moura DTH. Modifying an Intragastric Balloon for the Treatment of Obesity: a Unique Approach. Obes Surg. 2019;29:1445-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | de Moura DTH, de Moura EGH, Neto MG, Thompson CC. To the Editor. Surg Obes Relat Dis. 2019;15:155-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Lopez-Nava G, Galvão MP, Bautista-Castaño I, Fernandez-Corbelle JP, Trell M, Lopez N. Endoscopic sleeve gastroplasty for obesity treatment: two years of experience. Arq Bras Cir Dig. 2017;30:18-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Sartoretto A, Sui Z, Hill C, Dunlap M, Rivera AR, Khashab MA, Kalloo AN, Fayad L, Cheskin LJ, Marinos G, Wilson E, Kumbhari V. Endoscopic Sleeve Gastroplasty (ESG) Is a Reproducible and Effective Endoscopic Bariatric Therapy Suitable for Widespread Clinical Adoption: a Large, International Multicenter Study. Obes Surg. 2018;28:1812-1821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 8. | de Moura DTH, de Moura EGH, Thompson CC. Endoscopic sleeve gastroplasty: From whence we came and where we are going. World J Gastrointest Endosc. 2019;11:322-328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Lopez-Nava G, Sharaiha RZ, Vargas EJ, Bazerbachi F, Manoel GN, Bautista-Castaño I, Acosta A, Topazian MD, Mundi MS, Kumta N, Kahaleh M, Herr AM, Shukla A, Aronne L, Gostout CJ, Abu Dayyeh BK. Endoscopic Sleeve Gastroplasty for Obesity: a Multicenter Study of 248 Patients with 24 Months Follow-Up. Obes Surg. 2017;27:2649-2655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 151] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 10. | Alqahtani A, Al-Darwish A, Mahmoud AE, Alqahtani YA, Elahmedi M. Short-term outcomes of endoscopic sleeve gastroplasty in 1000 consecutive patients. Gastrointest Endosc. 2019;89:1132-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 138] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 11. | Barrichello S, Hourneaux de Moura DT, Hourneaux de Moura EG, Jirapinyo P, Hoff AC, Fittipaldi-Fernandez RJ, Baretta G, Felício Lima JH, Usuy EN, de Almeida LS, Ramos FM, Matz F, Galvão Neto MDP, Thompson CC. Endoscopic sleeve gastroplasty in the management of overweight and obesity: an international multicenter study. Gastrointest Endosc. 2019;90:770-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Kumar N, Sahdala HNP, Shaikh S, Wilson EB, Manoel GN, Zundel N, Thompson CC. Mo1155 Endoscopic Sleeve Gastroplasty for Primary Therapy of Obesity: Initial Human Cases. Gastroenterology. 2014;146:S-571-S-572. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Lopez-Nava G, Asokkumar R, Ielpo B, Bautista I, Vicente E. Biliary peritonitis after endoscopic sutured gastroplasty for morbid obesity (with video). Gastrointest Endosc. 2019;90:686-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Genco A, Cipriano M, Materia A, Bacci V, Maselli R, Musmeci L, Lorenzo M, Basso N. Laparoscopic sleeve gastrectomy versus intragastric balloon: a case-control study. Surg Endosc. 2009;23:1849-1853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Moura D, Oliveira J, De Moura EG, Bernardo W, Galvão Neto M, Campos J, Popov VB, Thompson C. Effectiveness of intragastric balloon for obesity: A systematic review and meta-analysis based on randomized control trials. Surg Obes Relat Dis. 2016;12:420-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 78] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 16. | Baptista A, Hourneaux De Moura DT, Jirapinyo P, Hourneaux De Moura EG, Gelrud A, Kahaleh M, Salinas A, Sabagh LC, Ospina A, Rincones VZ, Doval R, Bandel JW, Thompson CC. Efficacy of the cardiac septal occluder in the treatment of post-bariatric surgery leaks and fistulas. Gastrointest Endosc. 2019;89:671-679.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | de Moura DTH, Ribeiro IB, Funari MP, Baptista A, Thompson CC, de Moura EGH. Novel use of a cardiac septal occluder to treat a chronic recalcitrant bariatric fistula after Roux-en-Y gastric bypass. Endoscopy. 2019;51:E111-E112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Halvax P, Diana M, Nagao Y, Marescaux J, Swanström L. Experimental Evaluation of the Optimal Suture Pattern With a Flexible Endoscopic Suturing System. Surg Innov. 2017;24:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Madruga-Neto AC, Bernardo WM, de Moura DTH, Brunaldi VO, Martins RK, Josino IR, de Moura ETH, de Souza TF, Santo MA, de Moura EGH. The Effectiveness of Endoscopic Gastroplasty for Obesity Treatment According to FDA Thresholds: Systematic Review and Meta-Analysis Based on Randomized Controlled Trials. Obes Surg. 2018;28:2932-2940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Awan AN, Swain CP. Endoscopic vertical band gastroplasty with an endoscopic sewing machine. Gastrointest Endosc. 2002;55:254-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Neto MG, Zundel N, Campos J, Alvarado A, Silva L, Orilaac J, Shaikh S, Gomez E, Wilson E, Thompson CC. ET010 Endoluminal greater curvature plication-A case series. SAGES. Available from: https://www.sages.org/meetings/annual-meeting/abstracts-archive/endoluminal-greater-curvature-plication-a-case-series/. |
| 22. | Abu Dayyeh BK, Rajan E, Gostout CJ. Endoscopic sleeve gastroplasty: a potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc. 2013;78:530-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 190] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 23. | Sharaiha RZ, Kedia P, Kumta N, DeFilippis EM, Gaidhane M, Shukla A, Aronne LJ, Kahaleh M. Initial experience with endoscopic sleeve gastroplasty: technical success and reproducibility in the bariatric population. Endoscopy. 2015;47:164-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 24. | Jain D, Bhandari BS, Arora A, Singhal S. Endoscopic Sleeve Gastroplasty - A New Tool to Manage Obesity. Clin Endosc. 2017;50:552-561. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 25. | Fayad L, Adam A, Schweitzer M, Cheskin LJ, Ajayi T, Dunlap M, Badurdeen DS, Hill C, Paranji N, Lalezari S, Kalloo AN, Khashab MA, Kumbhari V. Endoscopic sleeve gastroplasty versus laparoscopic sleeve gastrectomy: a case-matched study. Gastrointest Endosc. 2019;89:782-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 121] [Article Influence: 20.2] [Reference Citation Analysis (1)] |
| 26. | Abu Dayyeh BK, Acosta A, Camilleri M, Mundi MS, Rajan E, Topazian MD, Gostout CJ. Endoscopic Sleeve Gastroplasty Alters Gastric Physiology and Induces Loss of Body Weight in Obese Individuals. Clin Gastroenterol Hepatol. 2017;15:37-43.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 197] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 27. | Hill C, El Zein M, Agnihotri A, Dunlap M, Chang A, Agrawal A, Barola S, Ngamruengphong S, Chen YI, Kalloo AN, Khashab MA, Kumbhari V. Endoscopic sleeve gastroplasty: the learning curve. Endosc Int Open. 2017;5:E900-E904. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 28. | Saumoy M, Schneider Y, Zhou XK, Shukla A, Kahaleh M, Aronne L, Sharaiha RZ. A single-operator learning curve analysis for the endoscopic sleeve gastroplasty. Gastrointest Endosc. 2018;87:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 74] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 29. | Novikov AA, Afaneh C, Saumoy M, Parra V, Shukla A, Dakin GF, Pomp A, Dawod E, Shah S, Aronne LJ, Sharaiha RZ. Endoscopic Sleeve Gastroplasty, Laparoscopic Sleeve Gastrectomy, and Laparoscopic Band for Weight Loss: How Do They Compare? J Gastrointest Surg. 2018;22:267-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 82] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 30. | Sharaiha RZ, Kumta NA, Saumoy M, Desai AP, Sarkisian AM, Benevenuto A, Tyberg A, Kumar R, Igel L, Verna EC, Schwartz R, Frissora C, Shukla A, Aronne LJ, Kahaleh M. Endoscopic Sleeve Gastroplasty Significantly Reduces Body Mass Index and Metabolic Complications in Obese Patients. Clin Gastroenterol Hepatol. 2017;15:504-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 164] [Article Influence: 20.5] [Reference Citation Analysis (0)] |