Published online Oct 16, 2020. doi: 10.4253/wjge.v12.i10.404
Peer-review started: May 27, 2020
First decision: September 11, 2020
Revised: September 19, 2020
Accepted: September 25, 2020
Article in press: September 25, 2020
Published online: October 16, 2020
Processing time: 139 Days and 13.7 Hours
Pneumonia caused by severe acute respiratory syndrome coronavirus 2 occasionally becomes severe and requires endotracheal intubation. Endotracheal intubation is usually performed using a laryngoscope; however, the operator needs to be in close proximity to the patient’s face during the procedure, which increases the risk of droplet exposure. Therefore, we simulated fiberoptic endotracheal intubation on a mannequin representing the patient, using an ultrathin flexible gastrointestinal endoscope as an alternative to the bronchoscope, in order to maintain distance from the patient during the procedure. We performed this procedure 10 times and measured the time required; the median procedure time was 6.4 s (interquartile range, 5.7-8.1 s). The advantage of this method is the short procedure time and distance maintained from the patients. The flexible tip-steerable control and length of the gastrointestinal endoscope contributed to shortening the procedure time and maintaining distance from the patients. In addition, this method can handle difficult airways without risk of misplacement of the endotracheal tube. However, it is necessary to consider the risk of aerosol generation associated with this procedure. In the pandemic setting of coronavirus disease 2019, this approach may be useful when a gastrointestinal endoscopist is in charge of endotracheal intubation of patients with coronavirus disease 2019.
Core Tip: Proximity of the operators to the patient is inevitable with conventional endotracheal intubation procedures. In this endotracheal intubation method, the gastrointestinal endoscope is used as an alternative to the bronchoscope. Thus, endotracheal intubation can be performed while keeping a relatively safe distance from the patient, as the gastrointestinal endoscope has a long effective length. Furthermore, the flexible tip-steerable control of the gastrointestinal endoscope enables quick and reliable endotracheal intubation.
- Citation: Masaki S, Yamada C, Kawamoto T. Endotracheal intubation in patients with COVID-19 using an ultrathin flexible gastrointestinal endoscope. World J Gastrointest Endosc 2020; 12(10): 404-407
- URL: https://www.wjgnet.com/1948-5190/full/v12/i10/404.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i10.404
Endotracheal intubation is performed in patients with severe respiratory failure induced by severe acute respiratory syndrome coronavirus 2[1]. These patients are usually intubated using a laryngoscope[2]. Coronavirus disease 2019 (COVID-19) is highly contagious; thus, preventing the propagation of infection requires maintaining a safe distance and avoiding direct exposure to droplets from infected patients[3]. However, it is difficult for healthcare professionals to maintain distance while intubating patients using a laryngoscope because operators need to stand in close proximity to patients’ faces.
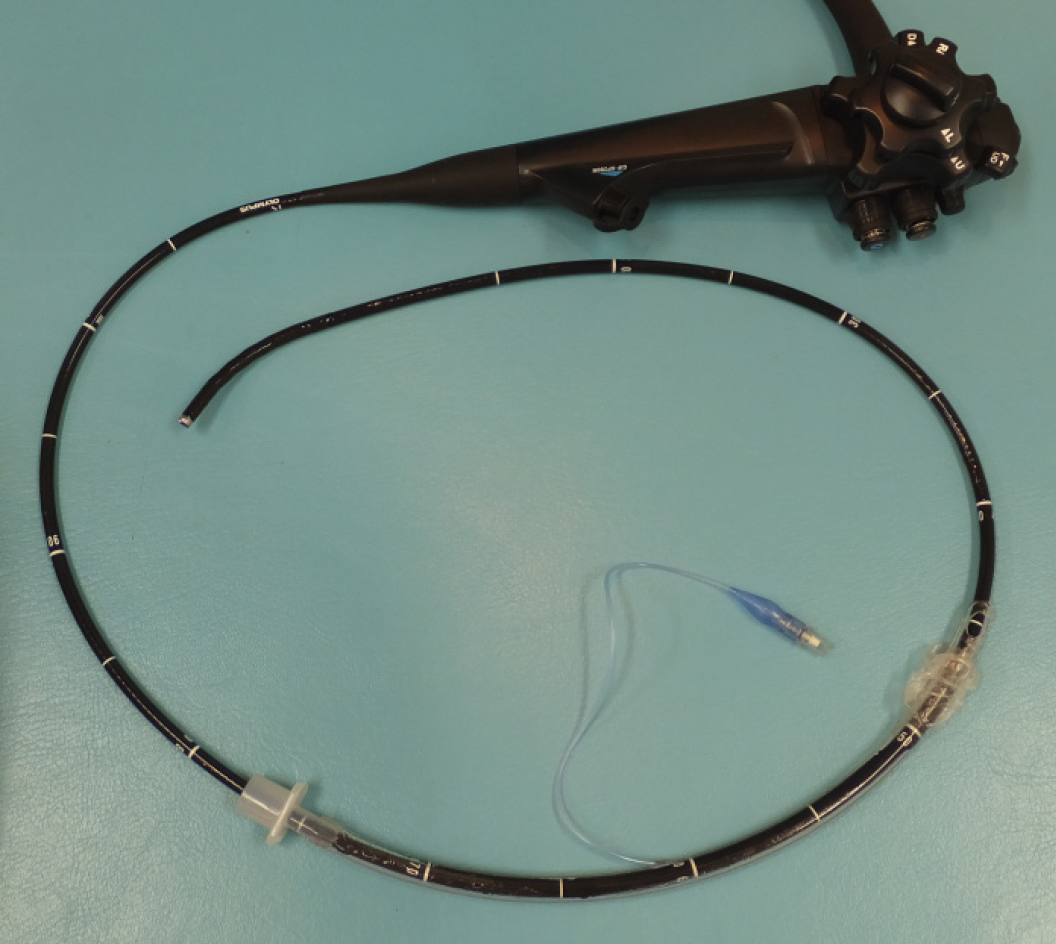
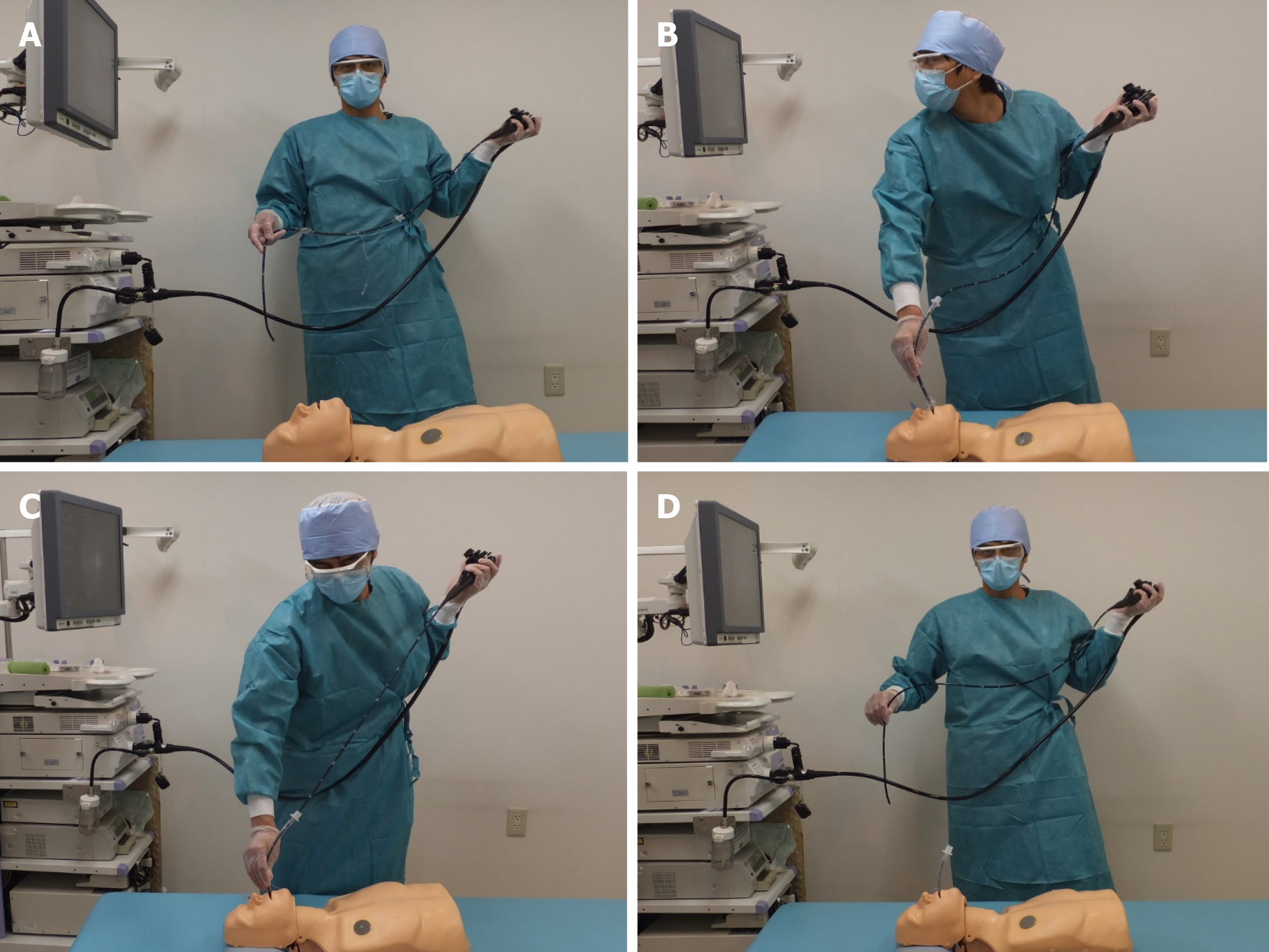
Here, we report the use of an ultrathin flexible gastrointestinal endoscope with a tip outer diameter of 5.0 mm (GIF-XP260N; Olympus, Tokyo, Japan) to perform endotracheal intubation on a mannequin representing the patient. The purpose of this simulation-based study was to evaluate the feasibility and usefulness of using a gastrointestinal endoscope as an alternative to the bronchoscope in endotracheal intubation. This procedure included four steps (Figures 1 and 2) as follows: First, the operator holding an endoscope over which a 7.0 mm endotracheal tube was mounted stood to the left of the supine patient; second, the endoscope was inserted into the trachea; third, we ensured instant insertion of the endotracheal tube into the trachea using the endoscope as a guide; and finally, the endoscope was withdrawn. We repeatedly performed the procedure 10 times and recorded the corresponding time taken for each procedure. The procedure time was defined as the total time elapsed between the insertion of the endoscope into the mouth and the final withdrawal of the endoscope. The median procedure time was 6.4 s (interquartile range, 5.7-8.1 s; Table 1).
| Time (s) | |
| 1st | 10.2 |
| 2nd | 7.9 |
| 3rd | 8.1 |
| 4th | 10.0 |
| 5th | 6.5 |
| 6th | 5.6 |
| 7th | 4.5 |
| 8th | 5.8 |
| 9th | 5.6 |
| 10th | 6.2 |
| Median, 6.4 (interquartile range, 5.7–8.1) |
Bronchoscope-guided endotracheal intubation in patients with COVID-19 has already been reported[4,5]. In our method, an ultrathin gastrointestinal endoscope was used as an alternative to the bronchoscope. This method is advantageous owing to the short procedure time. This can be attributed to the flexible tip-steerable control of the gastrointestinal endoscope because the gastrointestinal endoscope has angulation control knobs for up, down, left, and right movements, whereas the bronchoscope has an angulation control knob only for up and down movements[6]. Hence, the gastrointestinal endoscope may serve as a better alternative to the bronchoscope for endotracheal intubation. This technique will also be useful in patients with difficult airways in order to avoid the risk of misplacement of the endotracheal tube[7]. Furthermore, the effective length of the gastrointestinal endoscope used was 1.1 meters allowing the operator to maintain a relatively safe distance by standing to the left of the patient, minimizing direct exposure to droplets from patients.
However, our method has a few limitations. Conventionally, endotracheal intubation is performed by anesthesiologists familiar with techniques used in intubation[1]. Notably, gastrointestinal endoscopes are not usually available in the emergency room or intensive care unit where endotracheal intubation is often performed. Furthermore, owing to the potential for generating aerosols, it is unlikely that flexible bronchoscope-guided intubation will be the first choice in conscious patients with COVID-19[1,2].
During this COVID-19 pandemic, there may be occasions when a gastrointestinal endoscopist is in charge of endotracheal intubation in patients with confirmed or suspected COVID-19. If the gastrointestinal endoscopist is not familiar with endotracheal intubation using a laryngoscope, the intubation procedure is expected to be time-consuming, thus increasing the risk of direct exposure to droplets from patients. Therefore, endotracheal intubation using this method may be useful in reducing the risk of exposure to severe acute respiratory syndrome coronavirus 2.
Endotracheal intubation using an ultrathin flexible gastrointestinal endoscope is a quick and reliable procedure that can be performed while maintaining distance from the patient. Therefore, this method may be useful in endotracheal intubation in patients with COVID-19.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Friedel D, Rawat K S-Editor: Zhang L L-Editor: A P-Editor: Wang LL
| 1. | Yao W, Wang T, Jiang B, Gao F, Wang L, Zheng H, Xiao W, Yao S, Mei W, Chen X, Luo A, Sun L, Cook T, Behringer E, Huitink JM, Wong DT, Lane-Fall M, McNarry AF, McGuire B, Higgs A, Shah A, Patel A, Zuo M, Ma W, Xue Z, Zhang LM, Li W, Wang Y, Hagberg C, O'Sullivan EP, Fleisher LA, Wei H; collaborators. Emergency tracheal intubation in 202 patients with COVID-19 in Wuhan, China: lessons learnt and international expert recommendations. Br J Anaesth. 2020;125:e28-e37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 229] [Cited by in RCA: 224] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 2. | Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia. 2020;75:785-799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 619] [Cited by in RCA: 618] [Article Influence: 123.6] [Reference Citation Analysis (0)] |
| 3. | Canelli R, Connor CW, Gonzalez M, Nozari A, Ortega R. Barrier Enclosure during Endotracheal Intubation. N Engl J Med. 2020;382:1957-1958. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 400] [Cited by in RCA: 378] [Article Influence: 75.6] [Reference Citation Analysis (0)] |
| 4. | Cai SJ, Wu LL, Chen DF, Li YX, Liu YJ, Fan YQ, Du SH, Huang H, Liu N, Cheng LL, Deng XL, Li SY. [Analysis of bronchoscope-guided tracheal intubation in 12 cases with coronavirus disease 2019 under the personal protective equipment with positive pressure protective hood]. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:332-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 5. | Wu CN, Xia LZ, Li KH, Ma WH, Yu DN, Qu B, Li BX, Cao Y. High-flow nasal-oxygenation-assisted fibreoptic tracheal intubation in critically ill patients with COVID-19 pneumonia: a prospective randomised controlled trial. Br J Anaesth. 2020;125:e166-e168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Garg N, Sindwani G, Suri A, Shamim R, Pandey CK. Flexible gastroendoscope as a rescue device for an anaesthetist. J Clin Anesth. 2018;45:73-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Jamil LH, Bucobo JC, Nakamura M, Kadar A. Flexible Scope Endotracheal Intubation Using a Gastroscope. Am J Gastroenterol. 2017;112:535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |