Published online Oct 16, 2020. doi: 10.4253/wjge.v12.i10.365
Peer-review started: April 28, 2020
First decision: May 24, 2020
Revised: June 29, 2020
Accepted: September 11, 2020
Article in press: September 11, 2020
Published online: October 16, 2020
Processing time: 168 Days and 16.6 Hours
Bleeding esophageal varices (BEV) is a potentially life-threatening complication in patients with portal hypertension with mortality rates as high as 25% within six weeks of the index variceal bleed. After control of the initial bleeding episode patients should enter a long-term surveillance program with endoscopic intervention combined with non-selective β-blockers to prevent further bleeding and eradicate EV.
To assess the efficacy of endoscopic variceal ligation (EVL) in controlling acute variceal bleeding, preventing variceal recurrence and rebleeding and achieving complete eradication of esophageal varices (EV) in patients who present with BEV.
A prospectively documented single-center database was used to retrospectively identify all patients with BEV who were treated with EVL between 2000 and 2018. Control of acute bleeding, variceal recurrence, rebleeding, eradication and survival were analyzed using Baveno assessment criteria.
One hundred and forty patients (100 men, 40 women; mean age 50 years; range, 21–84 years; Child-Pugh grade A = 32; B = 48; C = 60) underwent 160 emergency and 298 elective EVL interventions during a total of 928 endoscopy sessions. One hundred and fourteen (81%) of the 140 patients had variceal bleeding that was effectively controlled during the index banding procedure and never bled again from EV, while 26 (19%) patients had complicated and refractory variceal bleeding. EVL controlled the acute sentinel variceal bleed during the first endoscopic intervention in 134 of 140 patients (95.7%). Six patients required balloon tamponade for control and 4 other patients rebled in hospital. Overall 5-d endoscopic failure to control variceal bleeding was 7.1% (n = 10) and four patients required a salvage transjugular intrahepatic portosystemic shunt. Index admission mortality was 14.2% (n = 20). EV were completely eradicated in 50 of 111 patients (45%) who survived > 3 mo of whom 31 recurred and 3 rebled. Sixteen (13.3%) of 120 surviving patients subsequently had 21 EV rebleeding episodes and 10 patients bled from other sources after discharge from hospital. Overall rebleeding from all sources after 2 years was 21.7% (n = 26). Sixty-nine (49.3%) of the 140 patients died, mainly due to liver failure (n = 46) during follow-up. Cumulative survival for the 140 patients was 71.4% at 1 year, 65% at 3 years, 60% at 5 years and 52.1% at 10 years.
EVL was highly effective in controlling the sentinel variceal bleed with an overall 5-day failure to control bleeding of 7.1%. Although repeated EVL achieved complete variceal eradication in less than half of patients with BEV, of whom 62% recurred, there was a significant reduction in subsequent rebleeding.
Core Tip: Control of acute bleeding is crucial in patients with portal hypertension and actively bleeding esophageal varices (BEV). The present study demonstrated that endoscopic variceal ligation (EVL) was highly effective in controlling acute variceal bleeding during the first endoscopic intervention in 95.7% of 140 patients with an overall 5-d failure to control bleeding of 7.1%. Although repeated EVL achieved complete variceal eradication in less than half of patients with BEV, of which 62% recurred, there was a significant reduction in subsequent rebleeding. EVL was effective and safe with a low complication rate in treating BEV.
- Citation: Krige J, Jonas E, Kotze U, Kloppers C, Gandhi K, Allam H, Bernon M, Burmeister S, Setshedi M. Defining the advantages and exposing the limitations of endoscopic variceal ligation in controlling acute bleeding and achieving complete variceal eradication. World J Gastrointest Endosc 2020; 12(10): 365-377
- URL: https://www.wjgnet.com/1948-5190/full/v12/i10/365.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i10.365
Bleeding esophageal varices (BEV) is a potentially life-threatening complication in patients with portal hypertension with mortality rates as high as 25% within six weeks of the index variceal bleed[1]. Although endoscopic intervention provides the optimal emergency method to control actively BEV, the risks of bleeding complications remain substantial and as many as 23% of patients have treatment failure within 5-d due to either uncontrolled or early rebleeding[2]. Approximately 60% of survivors rebleed within two years after the initial bleeding episode with a mortality rate of 30%[3]. Secondary prophylaxis of variceal bleeding is thus crucial and there is a general consensus, supported by the American Association for the Study of Liver Diseases (AASLD), the American Society for Gastrointestinal Endoscopy (ASGE) and the British Society of Gastroenterology (BSG) guidelines that following an initial bleeding episode patients should enter a long-term surveillance program with endoscopic intervention combined with non-selective β-blockers to pre-empt further bleeding and eradicate EV[1,3-5].
Endoscopic variceal ligation (EVL) has replaced injection sclerotherapy (IST) as the endoscopic interventional procedure of choice for BEV, supported by randomized controlled trial data that show more rapid eradication of varices with lower rates of recurrent bleeding and fewer endoscopic-related complications[6]. However, few studies have specifically evaluated detailed outcomes in relation to the inherent technical constraints of ligating device design which may influence the effectiveness of EVL in controlling acute variceal bleeding and in particular, achieving complete eradication of varices, a problem conceptually more relevant to endoscopic banding than sclerotherapy. This prospective study, based on a protocol-driven standardized EVL technique from a high-volume academic endoscopy referral center, assessed the efficacy of EVL in controlling acute variceal bleeding, preventing early rebleeding and achieving complete and durable variceal eradication to prevent late recurrent bleeding in a cohort of patients who presented with an index variceal bleeding event.
Consecutive adult patients with endoscopically proven BEV admitted to a specialist surgical gastroenterology unit with a particular interest in portal hypertension in Groote Schuur Hospital, Cape Town between January 2000 and December 2018 were assessed. Patients who had received sclerotherapy or had endoscopic treatment initiated elsewhere were excluded. The outcome of all endoscopic treatments, both emergency and subsequent elective therapy, was analyzed to assess the efficacy of EVL in acute variceal bleeding control and achieving complete and lasting variceal eradication. The study was a monocentric retrospective analysis following STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statements of all patients. After approval from the institutional Human Research and Ethics Committee, the unit database was searched and filtered for adult patients with endoscopically proven BEV who received EVL as the endoscopic method of treatment.
All data were entered prospectively into a bespoke computer programme by a dedicated research and data manager. Data collected included demographic and clinical information, cause of portal hypertension, Child–Pugh score, hematology and liver function tests, liver biopsy, imaging results, endoscopy information, including variceal size, number of bands placed at each session, the interval between and the number of banding sessions. Outcome data included the efficacy of EVL in controlling the acute index bleed, preventing early rebleeding, achieving complete variceal eradication, minimizing late recurrent bleeding and overall survival. Data were analyzed on January 30, 2020.
The primary endpoints of the study were (1) effective endoscopic control of the index variceal bleeding event; and (2) success in achieving complete variceal eradication as defined in the analysis criteria. Secondary endpoints included (1) early rebleeding; (2) variceal recurrence and rebleeding; and (3) overall survival.
Details of the acute bleeding management protocol in our unit have been published previously[7-9]. As soon as the patient was stable, diagnostic endoscopy and EVL were performed[10,11]. Endoscopic banding devices used during the study period included the Saeed Multi-band Ligator (Cook Endoscopy, Winston-Salem, NC, USA), and the Speedband Superview Super 7 Multiple Band Ligator (Boston Scientific Corp., Natick, MA, USA)[11]. Full details of the variceal ligation technique used have been published previously[12-14]. During endoscopy for the sentinel bleed and subsequent bleeds, a band was applied first to the bleeding varix and then proximally in a helical fashion for approximately 10 cm to the remaining varices. In patients in whom bleeding could not be controlled a Sengstaken-Blakemore or Minnesota balloon tube was inserted for immediate tamponade and further endoscopic procedures were performed within 24 h. When endoscopic measures failed transjugular intrahepatic portosystemic shunt (TIPS) was used as rescue treatment.
Patients underwent regular EVL until complete variceal eradication, defined as the absence of varices, was achieved. In a subcategory of patients who had residual varices which were too small or insufficiently pliable to be suctioned into the banding device to allow secure and safe band deployment, complete eradication was not pursued. After the initial EVL session during the index admission to hospital, subsequent variceal ligation procedures were undertaken at two-week intervals as an outpatient until the varices were eradicated or unsuitable for continued ligation. Surveillance endoscopy was performed at 3 and 6 monthly intervals and then annually to identify recurrence or persistent varices and repeat EVL performed whenever technically feasible. All patients were given non-selective β–blockers (NSBB) during follow-up unless specifically contra-indicated.
Baveno criteria were used to define 5-d and 6 wk failure to control bleeding[5]. Additional variceal ligation was undertaken if bleeding was due to residual or recurrent varices. Other sources of bleeding, such as gastric varices, portal hypertensive gastropathy, peptic ulcers or erosive gastritis were included in the definition of rebleeding and treated on their merits.
The Student t-test and χ2 test were used when appropriate and the Kaplan–Meier method was used to estimate the cumulative incidence of re-bleeding and actuarial survival. Multivariate analysis was used to assess risk factors for rebleeding. A P value < 0.05 was considered significant. SAS System Package version 9.2.1 software (SAS Systems International, Cary, NC, USA) was used for statistical analysis. Data were censored at the time of the last clinic or endoscopy visit, TIPS placement or death. Ethical and institutional review board approval (HREC 120/2019) was obtained before study initiation and data analysis.
The 140 patients (100 men, 40 women, median age: 50 years; range: 21-84 years) included 32 Child-Pugh grade A, 48 grade B and 60 grade C patients when assessed on first admission to hospital (Table 1). The underlying diagnoses were alcoholic cirrhosis n = 75 (53.6%), hepatitis B infection n = 13 (9.9%), cryptogenic cirrhosis n = 13 (9.9%), hepatitis and alcohol n = 9 (6.4%), non-alcoholic fatty liver disease n = 8 (5.7%), schistosomiasis n = 7 (5%), and portal vein thrombosis n = 5 (3.6%). The remaining ten patients had autoimmune hepatitis (n = 3), hepatitis C (n = 2), and one each of granulomatous hepatitis, myelofibrosis, Budd-Chiari syndrome, chronic active hepatitis and primary sclerosing cholangitis. The 140 patients received 160 emergency and 298 elective EVL procedures during a total of 928 endoscopy sessions.
| Child-Pughgrade | Number of patients | Survival > 90 d | Numbereradicated | Number of banding proceduresmedian (range) | Months to eradicatemedian (range) | Number recurred |
| A | n = 32 | 32 | 15 | 3 (1-13) | 15 (1-55) | 9 |
| B | n = 48 | 44 | 18 | 2 (1-12) | 4 (1-29) | 12 |
| C | n = 60 | 35 | 17 | 2 (1-5) | 3 (1-47) | 10 |
| Total | n = 140 | 111 | 50 | 2 (1-13) | 5 (1-55) | 13 |
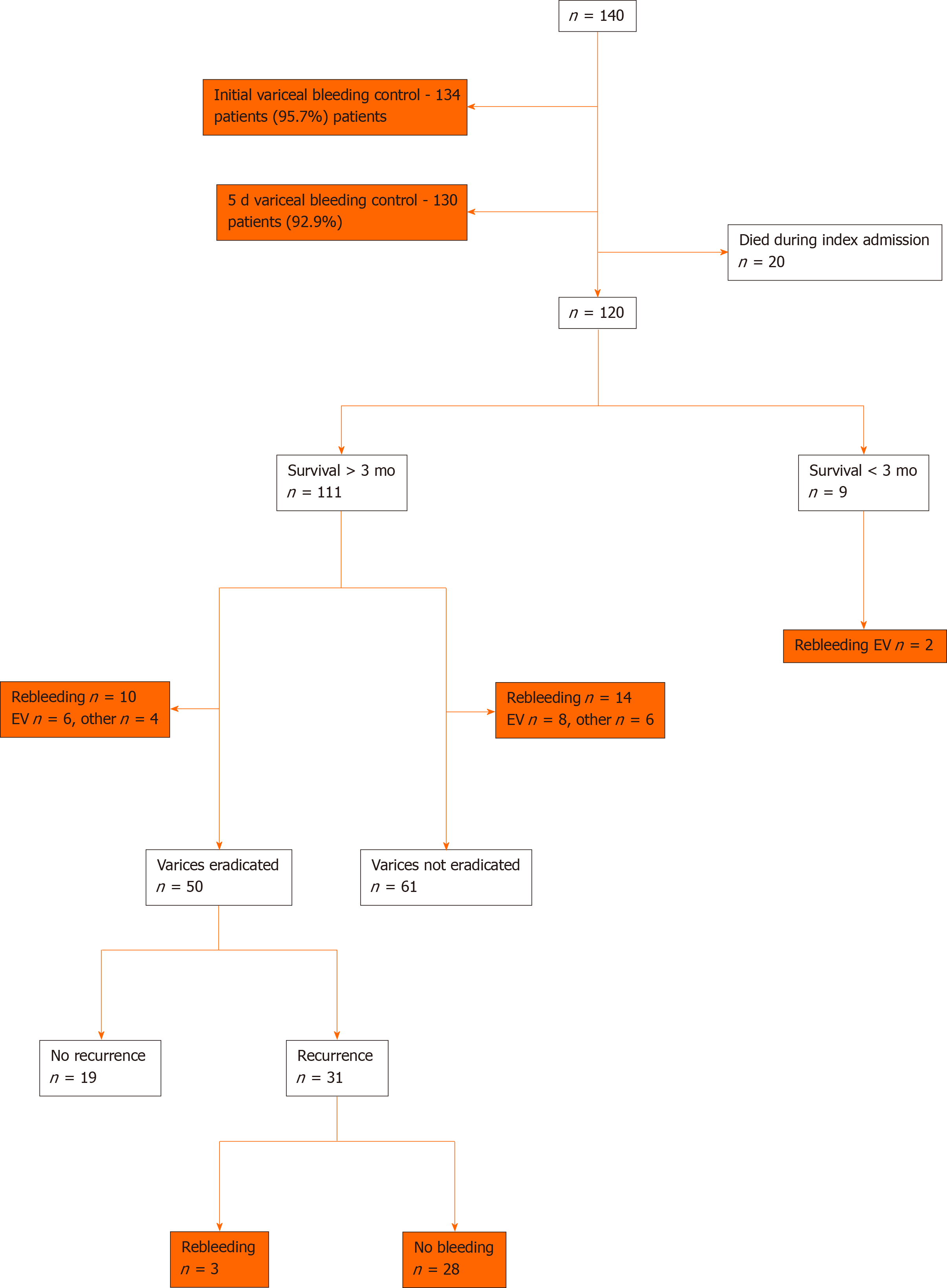
Acute bleeding was successfully controlled by EVL in 134 of 140 patients (95.7%) during the index endoscopic procedure (Figure 1). A balloon tube was used in six patients in whom acute bleeding could not be controlled by EVL, and a further four patients rebled within 5-d, resulting in a cumulative 5-d failure to control bleeding of 7.1% (n = 10; Child-Pugh grade A n = 0, grade B n = 1, grade C n = 9). These ten patients required 11 additional endoscopic banding sessions and four patients with recalcitrant variceal bleeding required a salvage TIPS.
The index in-hospital admission mortality was 14.2% (n = 20) with a median survival of 8 d (range 1-44). Ten patients died of multi-organ failure (MOF) including two of the four patients who had a salvage TIPS. A further seven patients died of progressive liver failure, another as a result of advanced hepatocellular carcinoma and two elderly patients with vasculopathy died of a myocardial infarction. The index admission mortality for the 32 Child-Pugh grade A patients was 0, for the 48 Child-Pugh grade B patients was 2.1% and for the 60 Child-Pugh grade C patients was 31.7% (19 of 60 patients).
Overall, 26 (21.7%) of the 120 surviving patients had 31 recurrent bleeding episodes after discharge from hospital. Two of these patients survived less than 3 mo (Figure 1). Sixteen patients had 21 EV rebleeding episodes which were successfully treated with emergency EVL. The 6-mo EV specific rebleeding incidence was 8.3% (n = 10 patients), at 12 mo was 12.5% (n = 15), at 2 years was 12.5% (n = 15) and beyond 2 years the total cumulative rebleeding rate after initial index control was 13.3% (n = 16). The remaining ten patients had bleeding from other sources which included gastric varices (n = 3), gastric ulcers (n = 4), duodenal ulcer (n = 1), esophagitis (n = 1), and Mallory Weiss tear (n = 1). The 6-mo overall all sources rebleeding incidence was 13.3% (n = 16 patients), at 12 mo was 17.5% (n = 21), at 2 years was 20.8% (n = 25) and beyond 2 years the total cumulative rebleeding rate after initial index control was 21.7% (n = 26, Table 2).
| Overall bleeding from all sources | Bleeding from esophageal varices | |||
| Patients | Bleeding events | Patients | Bleeding events | |
| < 6 mo | 16 (13.3%) | 22 | 10 (8.3%) | 16 |
| 6-12 mo | 21 (17.5%) | 28 | 15 (12.5%) | 20 |
| 1-2 yr | 25 (20.8%) | 30 | 15 (12.5%) | 20 |
| > 2 yr | 26 (21.7%) | 31 | 16 (13.3%) | 21 |
| Overall | 26 (21.7%) | 31 | 16 (13.3%) | 21 |
Eradication was achieved in 50 of 111 patients (45%) who survived longer than 3 mo, after a median of 2 banding procedures (range 1-13), during a median of 6 mo, (range 0.5-55 mo) (Table 1). EV remained eradicated in 19 (Child-Pugh grade A n = 6, grade B n = 6, grade C n = 7) patients with a median follow-up from eradication of 25 mo (range 4-112 mo) (Figure 1). Seven of the 19 patients died after a median survival of 44 mo (range 4-112 mo).
Three of the 31 patients with recurrent EV after eradication presented with variceal rebleeding at 3, 4 and 25 mo, respectively, and were successfully treated with EVL.
The 61 patients whose EV were not eradicated had a total of 224 banding procedures (median 5 banding procedures, range 1-11) during a mean of 25 mo (Figure 1). Twenty three of the 61 patients died (18 due to progressive liver failure, 3 with MOF aggravated by recurrent BEV and 2 due to hepatorenal failure) at a median of 23 mo (range 3-103 mo). The remaining 38 patients were followed up for a median of 6 mo (range 0.5-99 mo). In 41 patients who had at least 4 banding sessions, EV reduced in size to either grade 1 (n = 25) or grade 2 (n = 16) none of whom rebled despite no further EVL. This group in whom EVL was not technically possible was regarded as having “functional eradication” as results were comparable to those with complete eradication.
Esophageal stricture at the banding site was noted in 16 patients during a follow-up endoscopy, none of whom required esophageal dilatation for relief of symptoms and resolved after passage of the endoscope.
During a median follow-up period of 42 mo (range 9-220 mo), 69 (49.3%) of the 140 patients died (mean: 6.7 mo, range 0.03-141.7 mo). Liver failure (n = 46) was the most common cause of death followed by MOF in 14 patients. The cumulative overall survival of all 140 patients by life table analysis was 71.4% at 1 year, 65% at 3 years, 60% at 5 years and 52.1% at 10 years. Overall survival according to Child-Pugh grading is presented in Table 3. No significant specific risk factors for rebleeding were evident on multivariate analysis (Table 4).
| Child-Pugh Grade | Number of patients | 1-yr survival | 3-yr survival | 5-yr survival | 10-yr survival |
| A | n = 32 | 30 (93.7) | 29 (90.6) | 29 (90.6) | 25 (78.1) |
| B | n = 48 | 40 (83.3) | 36(75) | 34 (70.8) | 31 (64.5) |
| C | n = 60 | 30 (50) | 26 (43.3) | 21 (35) | 17 (28.3) |
| Total, n = 140 | No rebleeding, n = 104 | Rebleeding, n = 36 | P value | |
| Age | 0.149 | |||
| 20-39 yr | 36 | 30 | 6 | |
| 40-59 yr | 74 | 50 | 24 | |
| > 60 yr | 30 | 24 | 6 | |
| Gender | 0.112 | |||
| Male | 100 | 78 | 22 | |
| Female | 40 | 26 | 14 | |
| Child-Pugh grade | 0.965 | |||
| A | 32 | 24 | 8 | |
| B | 48 | 35 | 13 | |
| C | 60 | 45 | 15 | |
| Cause of varices | 0.343 | |||
| Alcoholic | 84 | 60 | 24 | |
| Non-Alcoholic | 56 | 44 | 12 |
In this prospective study the efficacy of EVL was evaluated in a large cohort of consecutive portal hypertensive patients treated at a specialist endoscopy referral center using specific and validated endpoints including control of the initial bleeding event and subsequent variceal eradication, rebleeding and recurrence. Acute control of active variceal bleeding was highly successful and hemostasis was achieved in 95.7% of patients with minimal banding morbidity. However, varices were completely eradicated in only 45% of patients who survived more than 3 mo. Furthermore, varices recurred in 62% of patients previously eradicated and 9.7% of these had further variceal bleeding. Overall, 81% of patients in this study had bleeding that was effectively controlled during the index banding procedure and, after repeat banding, never bled again from esophageal varices. However, the remaining 19% of the cohort had refractory and complicated variceal bleeding and required either balloon tamponade during the index endoscopy (4%) or rebled during the initial hospitalization (3%) or rebled subsequently (12%) over the next 24 mo from residual or recurrent esophageal varices. As EVL is now universally regarded as the endoscopic method of choice for treating EV[6] the data in this study are relevant and pertinent to current endoscopic variceal management and emphasize several important and unresolved issues related to the role of EVL in achieving hemostasis in actively bleeding varices and variceal eradication to prevent rebleeding[1-4].
Experts agree that EVL requires a high level of manipulative skill and mature judgement, especially when applying bands during active variceal bleeding[15]. Despite initial scepticism and concerns that EVL would prove less effective than sclerotherapy in achieving control of actively bleeding varices as blood or clot filling the cap during profuse bleeding may obscure vision and limit accurate band deployment, there were very few failures of acute hemostasis in this study. In three small non-randomized studies by El-Saify[16], Saeed[17] and Hou[18], active variceal bleeding control was reported in 100% of patients. Patient numbers in these studies, however, were small and there was no consistency in the definition of duration of control of active bleeding. In an updated analysis of 17 prospective randomized controlled trials (RCTs) comparing EVL with sclerotherapy, bleeding variceal control with EVL ranged from 86% to 100%, and was significantly better than IST in 2[19,20] of 17 RCTs[21-35] (Table 4). However, the reported efficacy of EVL in these RCTs varied widely due to arbitrary and inconsistent definitions of bleeding control[19].
The incidence of variceal rebleeding after EVL in RCTs ranges from 0% to 36% (Table 4). In a meta-analysis[6] of 14 RCTs, the overall rebleeding rate for EVL patients was 21.7% compared to an earlier analysis of RCTs which showed a median rebleeding rate of 32%[36]. However, the calculations and denominators in many papers are not clearly defined and lack adherence to uniform standard definitions of rebleeding including time periods, whether overall or confined to variceal bleeding, or uncontrolled, or during the first admission or during long-term follow-up. In addition, there is non-uniformity among different trials in the definition of recurrent bleeding which may include esophageal, gastric and ectopic varices and non-variceal sources (portal hypertensive gastropathy, treatment-induced or peptic ulcer)[25,26]. In our study we defined these criteria and analyzed the three specific and crucial time periods. The most common source of recurrent bleeding in our patient cohort during the early phase after initiation of endoscopic therapy and before variceal eradication was from patent residual varices which occurred in two-thirds of bleeding episodes, while one-third rebled from other sources.
Current AASLD/ACG guidelines emphasize total eradication of all varices as the desired endpoint of EVL[1]. Similarly, the reported incidence of variceal eradication varies widely, ranging from a high of 95% to a low of 55% in RCTs (Table 5). A plausible explanation is that inconsistent definitions were used and in some reports the definition of variceal eradication included varices too small to be ligated. The wide variation in eradication rates may also be related to different treatment protocols such as different treatment intervals, number of bands applied per session and selective banding of EV in some centers which band only grade 3–4 EV[26,27]. Ultimately, the results of any long-term banding study are influenced by the diligence and regularity of follow-up endoscopy and the meticulousness and reproducibility of the methodology, and the accuracy with which residual variceal size is recorded. There is increasing recognition that two important limitations of long-term EVL are the number of varices that are resistant to complete eradication and the substantial variceal recurrence rate after eradication. Both limitations are influenced by the design and mechanism of ligation. Experienced endoscopists know that EVL becomes increasingly difficult as varices decrease in size[15,37]. Small varices are difficult to ligate effectively for two technical reasons. Grade I and 2 varices do not have sufficient variceal substance to provide purchase and grip for the constricting elastic band. In addition, mucosal fibrosis due to prior banding episodes further limits mucosal pliability and the ability to suck enough tissue into the cap, thus preventing successful band application. Of note are the number of RCTs which report higher variceal recurrence rates in patients undergoing EVL (Table 5).
| Ref. | Year | Number of patients | Number in each group | Control of bleeding | Varices eradicated | Eradication sessions | Rebleeding | Major complications | Variceal recurrence | Survival | ||||||||
| EVL | IST | EVL | IST | EVL | IST | EVL | IST | EVL | IST | EVL | IST | EVL | IST | EVL | IST | |||
| Stiegmann et al[21] | 1992 | 129 | 64 | 65 | 86% | 77% | 55% | 56% | 4 | 5 | 36% | 48% | 2% | 22% | 33% | 50% | 72% | 55% |
| Laine et al[22] | 1993 | 77 | 38 | 39 | 89% | 89% | 59% | 69% | 4.1 | 6.2 | 24% | 31% | 24% | 56% | - | - | 89% | 85% |
| Gimson et al[23] | 1993 | 103 | 54 | 49 | 91% | 92% | 82% | 71% | 3.4 | 4.9 | 30% | 53% | 69% | 65% | - | - | 52% | 18% |
| Lo et al[24] | 1995 | 120 | 61 | 59 | 94% | 80% | 74% | 63% | 3.8 | 6.5 | 11% | 36% | 3.3% | 19% | - | - | 84% | 68% |
| Hou et al[25] | 1995 | 134 | 67 | 67 | 100% | 88% | 87% | 79% | 3.5 | 4.6 | 18% | 33% | 4% | 22% | 48% | 30% | 79% | 84% |
| Sarin et al[26] | 1997 | 95 | 47 | 48 | 86% | 80% | 94% | 94% | 4.1 | 5.2 | 6.4% | 20.8% | 45% | 50% | 28.7% | 7.5% | 93% | 89% |
| Baroncini et al[27] | 1997 | 111 | 57 | 54 | - | - | 93% | 93% | 3.5 | 4.0 | 16% | 19% | 11% | 31% | 30% | 13% | 79% | 78% |
| Avgerinos et al[28] | 1997 | 77 | 37 | 40 | - | - | 95% | 98% | 3.7 | 5.8 | 27% | 48% | 35% | 60% | 31% | 44% | 80% | 79% |
| Lo et al[19] | 1997 | 71 | 37 | 34 | 97% | 76% | - | - | - | - | 17% | 33% | 5% | 29% | - | - | 81% | 65% |
| Siqueira et al[29] | 1998 | 40 | 20 | 20 | - | - | 90% | 100% | 3.1 | 3.7 | 0% | 5% | - | - | 0% | 0% | 100% | 95% |
| De la Pena et al[30] | 1999 | 88 | 42 | 46 | - | - | 79% | 71% | 5.3 | 6.6 | 31% | 50% | 14% | 41% | 47% | 23% | 81% | 78% |
| Masci et al[31] | 1999 | 100 | 50 | 50 | - | - | 88% | 82% | 3.4 | 5.3 | 12% | 42% | 18% | 38% | 32% | 27% | 80% | 78% |
| Fakhry et al[32] | 2000 | 84 | 43 | 41 | 94% | 94% | - | - | 2.8 | 4.8 | 16% | 15% | 2% | 65% | 21% | 20% | 93% | 93% |
| Zargar et al[33] | 2005 | 73 | 37 | 36 | 100% | 83% | 95% | 92% | 3.7 | 7.7 | 3% | 19% | 3% | 22% | 11% | 9% | - | - |
| Villanueva et al[20] | 2006 | 179 | 90 | 89 | 96% | 85% | - | - | - | - | 7% | 12% | 4% | 13% | - | - | 87% | 79% |
| Luz et al[34] | 2011 | 100 | 50 | 50 | 92% | 96% | - | - | - | - | 22% | 14% | - | - | - | - | 77% | 80% |
| Ali et al[35] | 2017 | 124 | 60 | 64 | 100% | 100% | 87% | 80% | - | - | 23% | 28% | 10% | 27% | - | - | 78% | 72% |
The number of endoscopy sessions required to achieve variceal eradication has varied considerably within reported series and between centers (Table 5). A number of studies, including a meta-analysis by Ko et al[18,38-42] indicated that EVL achieved variceal eradication rates between 79% and 100%. While there is some evidence to suggest that the methodology and technique of EVL might affect the number of sessions necessary to achieve obliteration, this alone does not explain the substantial differences found between patients. Furthermore, the reproducibility, method and accuracy with which residual variceal size is recorded is dependent on the degree of insufflation used during endoscopy as prolonged or over-inflation during endoscopy tends to flatten varices which then appear misleadingly small.
A major drawback of EVL is the higher propensity to variceal recurrence when compared to IST in RCTs (Table 5). Although new varices formed following initial eradication in 31 of 50 (62%) patients in our study, this was associated with rebleeding in only 3 (9.7%) patients. Variceal recurrence in other studies ranged between 8% and 48% after banding[18,35,42]. More recent studies have shown recurrence rates of 12% to 36% (mean 25%) using EVL and NSBB[26-28,30]. Interpretation of these results is complicated by the differences in length of follow up, definitions of variceal recurrence, different medications and dosage used and the etiology of portal hypertension. Accumulated evidence suggests that patent para-esophageal and peri-esophageal variceal feeder vessels predispose to variceal recurrence. Data from RCTs show lower recurrence rates after IST, probably because sclerotherapy induces fibrosis and eradication of perforating veins in contrast to band ligation, which does not affect collateral vessels in the deeper esophageal wall layers[18,42].
The current study has several limitations. Firstly, as the study was conducted in a single center academic tertiary referral hospital with experienced on-call endoscopists and staff available around the clock, patient selection and treatment bias may occur as similar advanced interventions may not be available or replicated in smaller hospitals. Secondly, half the patients in the study were Child-Pugh grade C with hepatic decompensation associated with the highest mortality and our results cannot be generalized to all other patient populations. The use of an inclusive “all-cause” definition for rebleeding was applied to minimize bias found in previous definitions which often excluded non-variceal causes of re-bleeding.
The strengths of this study are derived from the implementation of a modern protocol-driven and standardized EVL technique in a specialist endoscopy center. In order to provide the highest possible level of uniformity and to minimize differences in the zero-time entry, only patients who received their initial and subsequent treatment in our unit were included. The study design minimized possible biases that may arise from patient selection, referral practices and local variations in treatment strategies. The use of rebleeding and death as the main outcomes provided robust, consistent and objective end-points in the study. Unlike other studies which included non-consecutive patients, incomplete reporting of inclusion and exclusion criteria and have incomplete follow-up or inclusion of patients at differing disease stages without separate analyses, our study design avoided these pitfalls by excluding non-measurable biases.
In conclusion, this study confirms that EVL provides the optimal endoscopic method both for control of acute bleeding and for the long-term treatment of varices despite the higher tendency for recurrence. Consistent with previous reports, EVL in this study was safe with low procedure-related complication rates. While complete visual eradication of varices is more frequently achievable with IST and has consistently been used as the desired endpoint for endoscopic variceal intervention, this goal is not always attainable in EVL. As alluded to above, the inherent attributes of EVL and IST are dissimilar and complete eradication may not be achievable in all patients undergoing EVL. Overall four-fifths of patients in this study had EV that were easily managed and responded to β-blockers and EVL with no further bleeding after the initial index intervention. However, the remaining one-fifth of patients were complicated and had bleeding that was difficult to control in the short and long-term despite being on combination therapy. We have identified a subgroup of patients with small (Grade 1 and 2) varices where size and mucosal scarring preclude further safe banding. Importantly we have shown that these patients have “stable varices” with no rebleeding or progression which resulted in “functional eradication” despite the presence of residual small visible varices. The results of this study should stimulate further research to optimize robust and objective endpoints for reporting of EVL which are likely to differ from the historical outcomes reported in previous RCTs. The elusive Holy Grail of endoscopic variceal banding remains the attainment of long-term bleed-free survival.
Bleeding esophageal varices (BEV) is a potentially life-threatening complication in patients with portal hypertension with mortality rates as high as 25% within six weeks of the index variceal bleed. Although endoscopic intervention provides the optimal emergency method to control actively BEV, the risks of bleeding complications remain substantial and as many as 23% of patients have treatment failure within 5-d due to either uncontrolled or early rebleeding. Approximately 60% of survivors rebleed within two years after the initial bleeding episode with a mortality rate of 30%. Secondary prophylaxis to prevent further variceal bleeding is thus crucial.
Endoscopic variceal ligation (EVL) has replaced injection sclerotherapy (IST) as the endoscopic interventional procedure of choice for BEV, supported by randomized controlled trial data that show more rapid eradication of varices with lower rates of recurrent bleeding and fewer endoscopic-related complications. However, few studies have specifically evaluated detailed outcomes in relation to the inherent technical constraints of ligating device design which may influence the effectiveness of EVL in controlling acute variceal bleeding and in particular, achieving complete eradication of varices, a problem conceptually more relevant to endoscopic banding than sclerotherapy.
This analysis, based on a protocol-driven standardized EVL technique from a high-volume academic endoscopy referral center, used STROBE guidelines to assess the efficacy of EVL in controlling acute variceal bleeding, preventing early rebleeding and achieving complete and durable variceal eradication to prevent late recurrent bleeding in a cohort of patients who presented with an index variceal bleeding event.
Consecutive adult patients with endoscopically proven BEV between January 2000 and December 2018 were assessed. The outcome of all endoscopic treatments, both emergency and subsequent elective therapy, was analyzed to assess the efficacy of EVL in acute variceal bleeding control and achieving complete and lasting variceal eradication. Data collected included demographic and clinical information, cause of portal hypertension, Child–Pugh score, hematology and liver function tests, liver biopsy, imaging results, endoscopy information, including variceal size, number of bands placed at each session, the interval between and the number of banding sessions. Outcome data included the efficacy of EVL in controlling the acute index bleed, preventing early rebleeding, achieving complete variceal eradication, minimizing late recurrent bleeding and overall survival. The primary endpoints of the study were (1) effective endoscopic control of the index variceal bleeding event and (2) success in achieving complete variceal eradication as defined in the analysis criteria. Secondary endpoints included (1) early rebleeding; (2) variceal recurrence and rebleeding and (3) overall survival.
Acute control of active variceal bleeding in the 140 patients was highly successful and hemostasis was achieved in 95.7% of patients with minimal banding morbidity. However, varices were completely eradicated in only 45% of patients who survived more than 3 months. Furthermore, varices recurred in 62% of patients previously eradicated and 9.7% of these had further variceal bleeding. Overall, 81% of patients in this study had bleeding that was effectively controlled during the index banding procedure and, after repeat banding, never bled again from esophageal varices. However, the remaining 19% of the cohort had refractory and complicated variceal bleeding and required either balloon tamponade during the index endoscopy (4%) or rebled during the initial hospitalization (3%) or rebled subsequently (12%) over the next 24 months from residual or recurrent esophageal varices.
In conclusion, this study confirms that EVL provides the optimal endoscopic method both for control of acute bleeding and for the long-term treatment of varices despite the higher tendency for recurrence. Consistent with previous reports EVL in this study was safe with low procedure-related complication rates. While complete visual eradication of varices is more frequently achievable with IST and has consistently been used as the desired endpoint for endoscopic variceal intervention, this goal is not always attainable in EVL.
In this study we have identified a subgroup of patients with small varices where size and mucosal scarring preclude further safe banding. Importantly we have shown that these patients have “stable varices” with no rebleeding or progression which resulted in “functional eradication” despite the presence of residual small visible varices. The results of this study should stimulate further research to optimize robust and objective endpoints for reporting of EVL which are likely to differ from the historical outcomes reported in previous randomized controlled trials. The elusive Holy Grail of endoscopic variceal banding remains the attainment of long-term bleed-free survival.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Africa
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Kadayifci A, Karagiannakis D S-Editor: Zhang H L-Editor: Webster JR P-Editor: Wang LL
| 1. | Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1441] [Article Influence: 180.1] [Reference Citation Analysis (3)] |
| 2. | Amitrano L, Guardascione MA, Manguso F, Bennato R, Bove A, DeNucci C, Lombardi G, Martino R, Menchise A, Orsini L, Picascia S, Riccio E. The effectiveness of current acute variceal bleed treatments in unselected cirrhotic patients: refining short-term prognosis and risk factors. Am J Gastroenterol. 2012;107:1872-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 133] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 3. | Fortune BE, Garcia-Tsao G, Ciarleglio M, Deng Y, Fallon MB, Sigal S, Chalasani NP, Lim JK, Reuben A, Vargas HE, Abrams G, Lewis MD, Hassanein T, Trotter JF, Sanyal AJ, Beavers KL, Ganger D, Thuluvath PJ, Grace ND, Groszmann RJ; Vapreotide Study Group. Child-Turcotte-Pugh Class is Best at Stratifying Risk in Variceal Hemorrhage: Analysis of a US Multicenter Prospective Study. J Clin Gastroenterol. 2017;51:446-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 4. | Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, Austin A, Ferguson JW, Olliff SP, Hudson M, Christie JM; Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015;64:1680-1704. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 454] [Cited by in RCA: 416] [Article Influence: 41.6] [Reference Citation Analysis (2)] |
| 5. | de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015;63:743-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2011] [Cited by in RCA: 2294] [Article Influence: 229.4] [Reference Citation Analysis (3)] |
| 6. | Dai C, Liu WX, Jiang M, Sun MJ. Endoscopic variceal ligation compared with endoscopic injection sclerotherapy for treatment of esophageal variceal hemorrhage: a meta-analysis. World J Gastroenterol. 2015;21:2534-2541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 96] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (1)] |
| 7. | Krige J, Spence RT, Jonas E, Hoogerboord M, Ellsmere J. A New Recalibrated Four-Category Child-Pugh Score Performs Better than the Original Child-Pugh and MELD Scores in Predicting In-Hospital Mortality in Decompensated Alcoholic Cirrhotic Patients with Acute Variceal Bleeding: a Real-World Cohort Analysis. World J Surg. 2020;44:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Krige JE, Kotze UK, Distiller G, Shaw JM, Bornman PC. Predictive factors for rebleeding and death in alcoholic cirrhotic patients with acute variceal bleeding: a multivariate analysis. World J Surg. 2009;33:2127-2135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Krige JE, Kotze UK, Bornman PC, Shaw JM, Klipin M. Variceal recurrence, rebleeding, and survival after endoscopic injection sclerotherapy in 287 alcoholic cirrhotic patients with bleeding esophageal varices. Ann Surg. 2006;244:764-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Terblanche J, Stiegmann GV, Krige JE, Bornman PC. Long-term management of variceal bleeding: the place of varix injection and ligation. World J Surg. 1994;18:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Tait IS, Krige JE, Terblanche J. Endoscopic band ligation of oesophageal varices. Br J Surg. 1999;86:437-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Krige JEJ, Bornman PC. Endoscopic therapy in the management of esophageal varices: injection sclerotherapy and variceal ligation. In: Blumgart L (ed) Surgery of the Liver, Biliary Tract and Pancreas, 4th Edition, Saunders, Elsevier, Philadelphia. 2007: 1579-1593. [DOI] [Full Text] |
| 13. | Krige JEJ, Botha JF, Bornman PC. Endoscopic variceal ligation for bleeding esophageal varices. Digest Endosc. 1999;11:315-320. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Krige JEJ, Thomson SR. Endoscopic therapy in the management of esophageal varices. In: Fischer. (Ed) Mastery of Surgery, 7th Edition. Lippincott, WilliamsWilkens. Philadelphia. 2019: 1616-1629. |
| 15. | Baron TH, Wong Kee Song LM. Endoscopic variceal band ligation. Am J Gastroenterol. 2009;104:1083-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | El-Saify WM, Mourad FA. Use of the six-shooter ligation device in the management of bleeding esophageal varices: a developing-country experience. Dig Dis Sci. 2005;50:394-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Saeed ZA, Stiegmann GV, Ramirez FC, Reveille RM, Goff JS, Hepps KS, Cole RA. Endoscopic variceal ligation is superior to combined ligation and sclerotherapy for esophageal varices: a multicenter prospective randomized trial. Hepatology. 1997;25:71-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 84] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Hou MC, Lin HC, Lee FY, Chang FY, Lee SD. Recurrence of esophageal varices following endoscopic treatment and its impact on rebleeding: comparison of sclerotherapy and ligation. J Hepatol. 2000;32:202-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Lo GH, Lai KH, Cheng JS, Lin CK, Huang JS, Hsu PI, Chiang HT. Emergency banding ligation versus sclerotherapy for the control of active bleeding from esophageal varices. Hepatology. 1997;25:1101-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 135] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Villanueva C, Piqueras M, Aracil C, Gómez C, López-Balaguer JM, Gonzalez B, Gallego A, Torras X, Soriano G, Sáinz S, Benito S, Balanzó J. A randomized controlled trial comparing ligation and sclerotherapy as emergency endoscopic treatment added to somatostatin in acute variceal bleeding. J Hepatol. 2006;45:560-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 21. | Stiegmann GV, Goff JS, Michaletz-Onody PA, Korula J, Lieberman D, Saeed ZA, Reveille RM, Sun JH, Lowenstein SR. Endoscopic sclerotherapy as compared with endoscopic ligation for bleeding esophageal varices. N Engl J Med. 1992;326:1527-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 504] [Cited by in RCA: 415] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 22. | Laine L, el-Newihi HM, Migikovsky B, Sloane R, Garcia F. Endoscopic ligation compared with sclerotherapy for the treatment of bleeding esophageal varices. Ann Intern Med. 1993;119:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 203] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 23. | Gimson AE, Ramage JK, Panos MZ, Hayllar K, Harrison PM, Williams R, Westaby D. Randomised trial of variceal banding ligation versus injection sclerotherapy for bleeding oesophageal varices. Lancet. 1993;342:391-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 186] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Lo GH, Lai KH, Cheng JS, Hwu JH, Chang CF, Chen SM, Chiang HT. A prospective, randomized trial of sclerotherapy versus ligation in the management of bleeding esophageal varices. Hepatology. 1995;22:466-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 134] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 25. | Hou MC, Lin HC, Kuo BI, Chen CH, Lee FY, Lee SD. Comparison of endoscopic variceal injection sclerotherapy and ligation for the treatment of esophageal variceal hemorrhage: a prospective randomized trial. Hepatology. 1995;21:1517-1522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Sarin SK, Govil A, Jain AK, Guptan RC, Issar SK, Jain M, Murthy NS. Prospective randomized trial of endoscopic sclerotherapy versus variceal band ligation for esophageal varices: influence on gastropathy, gastric varices and variceal recurrence. J Hepatol. 1997;26:826-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 141] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Baroncini D, Milandri GL, Borioni D, Piemontese A, Cennamo V, Billi P, Dal Monte PP, D'Imperio N. A prospective randomized trial of sclerotherapy versus ligation in the elective treatment of bleeding esophageal varices. Endoscopy. 1997;29:235-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 97] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 28. | Avgerinos A, Armonis A, Manolakopoulos S, Poulianos G, Rekoumis G, Sgourou A, Gouma P, Raptis S. Endoscopic sclerotherapy versus variceal ligation in the long-term management of patients with cirrhosis after variceal bleeding. A prospective randomized study. J Hepatol. 1997;26:1034-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Siqueira ES, Rohr MR, Libera ED, Castro RR, Ferrari AP. Band ligation or sclerotherapy as endoscopic treatment for oesophageal varices in schistosomotic patients: results of a randomized study. HPB Surg. 1998;11:27-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | de la Peña J, Rivero M, Sanchez E, Fábrega E, Crespo J, Pons-Romero F. Variceal ligation compared with endoscopic sclerotherapy for variceal hemorrhage: prospective randomized trial. Gastrointest Endosc. 1999;49:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Masci E, Stigliano R, Mariani A, Bertoni G, Baroncini D, Cennamo V, Micheletti G, Casetti T, Tansini P, Buscarini E, Ranzato R, Norberto L. Prospective multicenter randomized trial comparing banding ligation with sclerotherapy of esophageal varices. Hepatogastroenterology. 1999;46:1769-1773. [PubMed] |
| 32. | Zargar SA, Javid G, Khan BA, Shah OJ, Yattoo GN, Shah AH, Gulzar GM, Singh J, Shah NA, Shafi HM. Endoscopic ligation vs. sclerotherapy in adults with extrahepatic portal venous obstruction: a prospective randomized study. Gastrointest Endosc. 2005;61:58-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Fakhry S, Omar M, Gannam M, Syam M, Attia M, Moustafa I, El-Beheiry N, Hunter, S. Endoscopic sclerotherapy versus endoscopic variceal ligation in the management of bleeding esophageal varices: a prospective randomized study in schistosomal hepatic fibrosis. Endosc Arab Edition. 2000;1:39-44. |
| 34. | Luz GO, Maluf-Filho F, Matuguma SE, Hondo FY, Ide E, Melo JM, Cheng S, Sakai P. Comparison between endoscopic sclerotherapy and band ligation for hemostasis of acute variceal bleeding. World J Gastrointest Endosc. 2011;3:95-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 35. | Ali SM, Wu S, Xu H, Liu H, Hao J, Qin C. A Prospective Study of Endoscopic Injection Sclerotherapy and Endoscopic Variceal Ligation in the Treatment of Esophageal Varices. J Laparoendosc Adv Surg Tech A. 2017;27:333-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 36. | Burgener FA, Spataro RF. Early medullary cystic disease: a urographic diagnosis? Radiology. 1979;130:321-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 467] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 37. | Kim DH, Cho E, Jun CH, Son DJ, Lee MJ, Park CH, Cho SB, Park SY, Kim HS, Choi SK, Rew JS. Risk Factors and On-site Rescue Treatments for Endoscopic Variceal Ligation Failure. Korean J Gastroenterol. 2018;7:188-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 38. | Ray G. Long-term outcome of endoscopic variceal band ligation of esophageal varices in patients with chronic liver disease. Indian J Gastroenterol. 2019;38:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Aggeletopoulou I, Konstantakis C, Manolakopoulos S, Triantos C. Role of band ligation for secondary prophylaxis of variceal bleeding. World J Gastroenterol. 2018;24:2902-2914. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 40. | Branch-Elliman W, Perumalswami P, Factor SH, Sled SM, Flamm SL. Rates of recurrent variceal bleeding are low with modern esophageal banding strategies: a retrospective cohort study. Scand J Gastroenterol. 2015;50:1059-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Ko SY, Kim JH, Choe WH, Kwon SY, Lee CH. Pharmacotherapy alone vs endoscopic variceal ligation combination for secondary prevention of oesophageal variceal bleeding: meta-analysis. Liver Int. 2012;32:867-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 42. | Cho H, Nagata N, Shimbo T, Sakurai T, Sekine K, Okubo H, Imbe K, Watanabe K, Mikami S, Yokoi C, Kobayakawa M, Mizokami M, Yanase M, Akiyama J, Uemura N. Recurrence and prognosis of patients emergently hospitalized for acute esophageal variceal bleeding: A long-term cohort study. Hepatol Res. 2016;46:1338-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |