Published online Oct 16, 2020. doi: 10.4253/wjge.v12.i10.355
Peer-review started: May 6, 2020
First decision: May 15, 2020
Revised: May 18, 2020
Accepted: August 16, 2020
Article in press: August 16, 2020
Published online: October 16, 2020
Processing time: 161 Days and 3.9 Hours
Although endoscopic ultrasound (EUS) is now widely available and has an established role in adults, the utility of EUS and EUS-guided fine needle aspiration (EUS-FNA) in pediatrics is insufficiently described compared to adults and is supported by only a few studies.
To report the experience of a single tertiary center in the use of EUS and EUS-FNA in a pediatric population and to further assess its safety, feasibility, and clinical impact on management.
A retrospective study of 13 children (aged 18 years or younger) identified from our medical database was conducted. A retrospective review of demographic data, procedure indications, EUS findings, and the clinical impact of EUS on the subsequent management of these patients was performed.
During the 4-year study period, a total of 13 (1.7%) pediatric EUS examinations out of 749 EUS procedures were performed in our unit. The mean age of these 8 females and 5 males was 15.6 years (range: 6-18). Six of the 13 EUS examinations were pancreatobiliary (46.1%), followed by mediastinal 2/13 (15.4%), peri-gastric 2/13 (15.4%), abdominal lymphadenopathy 1/13 (7.7%), tracheal 1/13 (7.7%) and rectal 1/13 (7.7%). Overall, EUS-FNA was performed in 7 patients (53.8%) with a diagnostic yield of 100%. The EUS results had a significant impact on clinical care in 10/13 (77%) cases. No complications occurred in these patients during or after any of the procedures.
EUS and EUS-FNA in the pediatric population are safe, feasible, and have a significant clinical impact on the subsequent management; thus avoiding invasive and unnecessary procedures.
Core Tip: Although endoscopic ultrasound (EUS) is now widely available and has an established role in adults, the utility of EUS and EUS-guided fine needle aspiration in pediatrics is insufficiently described compared to adults and is supported by only a few studies. More effort is required to increase the awareness of EUS among pediatric gastroenterologists which may have a clinical impact on the subsequent management and minimize unnecessary procedures in children.
- Citation: Altonbary AY, Hakim H, Elkashef W. Role of endoscopic ultrasound in pediatric patients: A single tertiary center experience and review of the literature. World J Gastrointest Endosc 2020; 12(10): 355-364
- URL: https://www.wjgnet.com/1948-5190/full/v12/i10/355.htm
- DOI: https://dx.doi.org/10.4253/wjge.v12.i10.355
Since the introduction of endoscopic ultrasound (EUS) in 1980, the diagnostic and therapeutic indications, in addition to the scope design, have rapidly grown. The role of EUS in gastrointestinal and pancreatobiliary disorders in adults is well established[1]. EUS, magnetic resonance cholangiopancreatography, and computed tomography (CT) have been considered in many studies to be minimally or non-invasive tools that can be used in the assessment of pancreatobiliary disorders avoiding invasive and unnecessary procedures[2,3].
Although EUS is now widely available and has an established role in adults, the utility of EUS and EUS-guided fine needle aspiration (EUS-FNA) in pediatrics is insufficiently described compared to adults and is supported by only a few studies[3-12]. This could be attributed to many factors including: Low incidence of gastrointestinal tumors and pancreatobiliary disorders in pediatric patients, a lacking of awareness among pediatric gastroenterologists and the absence of dedicated pediatric endosonographers. Certainly, these few pediatric EUS procedures do not allow pediatric endoscopists to gain and maintain competency in EUS and most EUS procedures in pediatrics are performed by adult endoscopists[7,8]. Therefore, more effort is required to increase the awareness of EUS among pediatric gastroenterologists, as it may have a clinical impact on the subsequent management and minimize unnecessary procedures in children[10].
The aim of this study is to report the experience of a single tertiary center in the use of EUS and EUS-FNA in a pediatric population and to assess its safety, feasibility, and clinical impact on subsequent patient management.
All EUS procedures performed between January 2016 and January 2020 at the Endoscopy Unit of Mansoura Specialized Medical Hospital, Mansoura University, Egypt, were reviewed. Patients aged 18 years or younger were identified from our medical database. A retrospective review of demographic data, procedure indications, EUS findings, and the clinical impact of EUS on subsequent management of the patients was conducted.
The inclusion criteria were as follows: Patients who required EUS and EUS-guided tissue acquisition after imaging studies [abdominal ultrasound (US), CT, or magnetic resonance imaging], that shows either mediastinal, pancreatic, or intra-abdominal solid or cystic lesions (size > 1 cm) or patients who required pancreatic EUS to exclude pancreatic insulinoma after negative imaging studies. The exclusion criteria were as follows: Patients or parents who refused participation in the study, patients with a contraindication to interventional endoscopy; such as patients who were unfit for anesthesia or patients with coagulation disorders. Our ethical committee approved the study protocol and written consent was obtained from all patients or parents before the procedure.
This retrospective study was conducted to assess the safety, feasibility, and clinical impact of EUS and EUS-FNA in a pediatric population. All procedures were performed under intravenous propofol sedation. All EUS examinations were carried out by two experienced endosonographers using a Pentax linear Echoendoscope EG3870UTK (PENTAX Medical, Tokyo, Japan) connected to a Hitachi Avius ultrasound system (Hitachi Medical Systems, Tokyo, Japan).
Technique: Examination of the pancreatic head, Ampulla of Vater, biliary tract, gallbladder, and portal regions was performed from the second part of the duodenum and duodenal bulb; the pancreatic body and tail, left suprarenal gland and the liver were visualized from the stomach; the mediastinum and trachea were examined from the esophagus. For rectal EUS, the scope was advanced to the sigmoid colon, and examination of the rectosigmoid junction, rectum and anal canal was performed after filling the lumen with water during slow withdrawal of the scope.
EUS-FNA was performed using either a 19 or 22 gauge FNA needle (Cook Medical, Bloomington, IN, USA). Color Doppler was used to identify the best position for puncture avoiding interposing blood vessels between the target lesion and the needle. After the solid lesions were penetrated by the needle under EUS guidance, the needle was moved to and fro 10-12 times in different directions while the stylet was slowly removed (slow pull technique). After each pass, tissue material was divided into two parts: The first part was smeared onto slides and fixed with 95% alcohol and the second part was placed in a formalin tube and labelled. Two needle passes were performed for solid lesions to increase the diagnostic yield. EUS elastography was used to differentiate the nature of solid lesions and to target the hardest area of the lesion during sampling. One pass was carried out for cystic lesions with near total aspiration of the fluid content to decrease the risk of infection. Prophylactic intravenous antibiotics were given before aspiration of cystic lesions. All samples were sent to the Pathology Department for evaluation.
Cytopathological examination: All slides were stained with hematoxylin and eosin and all tissue samples fixed in formalin were placed in paraffin and stained with hematoxylin and eosin for evaluation of the presence of a histologic core. Immunohistochemical markers were used when needed. All prepared slides and tissue samples were examined by experienced cytopathologists.
Study outcomes: The patient’s medical records were revised for standard data which included patient demographics, initial diagnosis, previous abdominal US, CT, or magnetic resonance imaging, EUS indications, EUS findings, impact of EUS on the patient’s clinical care, and adverse events during and for 2 h after the procedure.
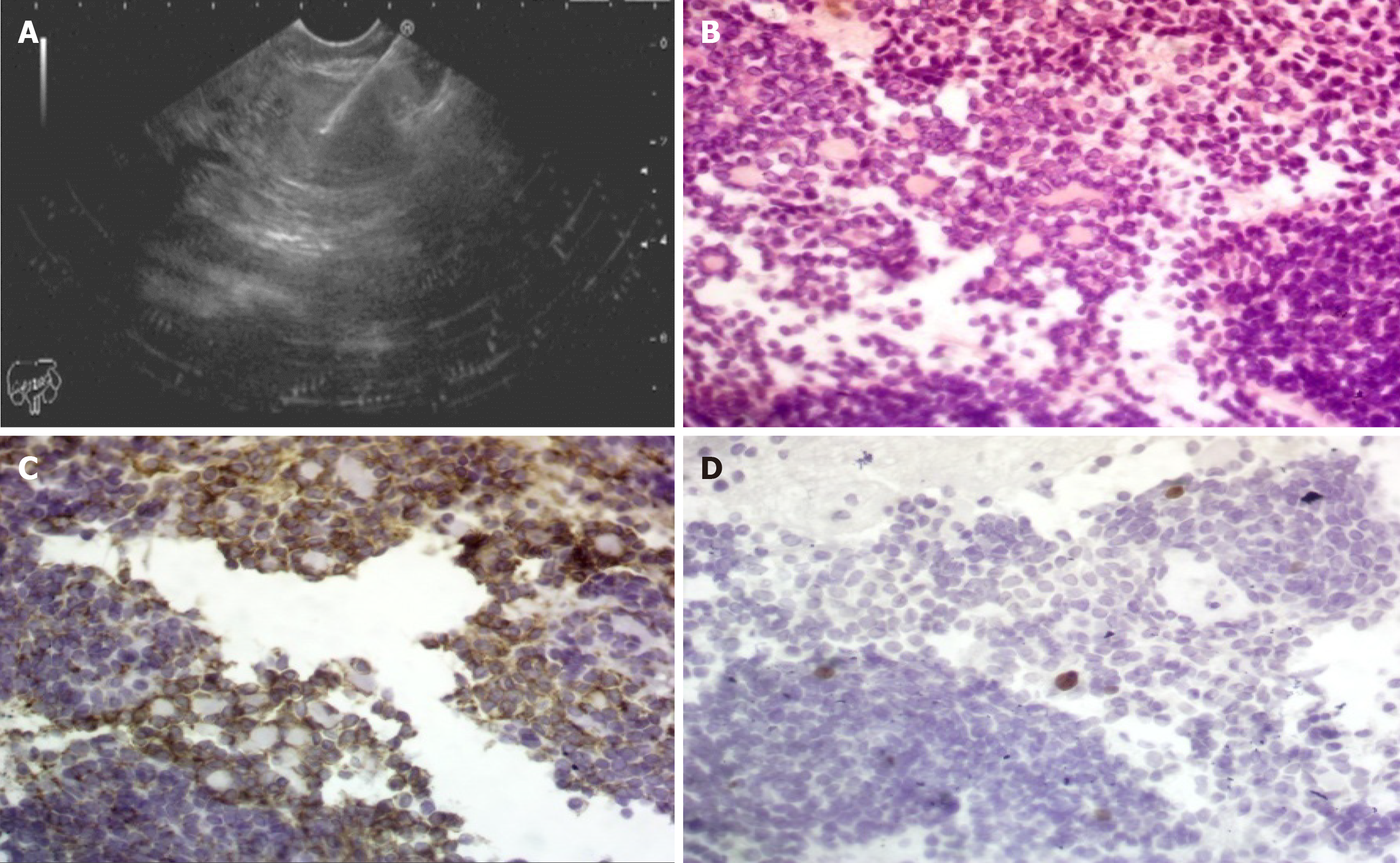
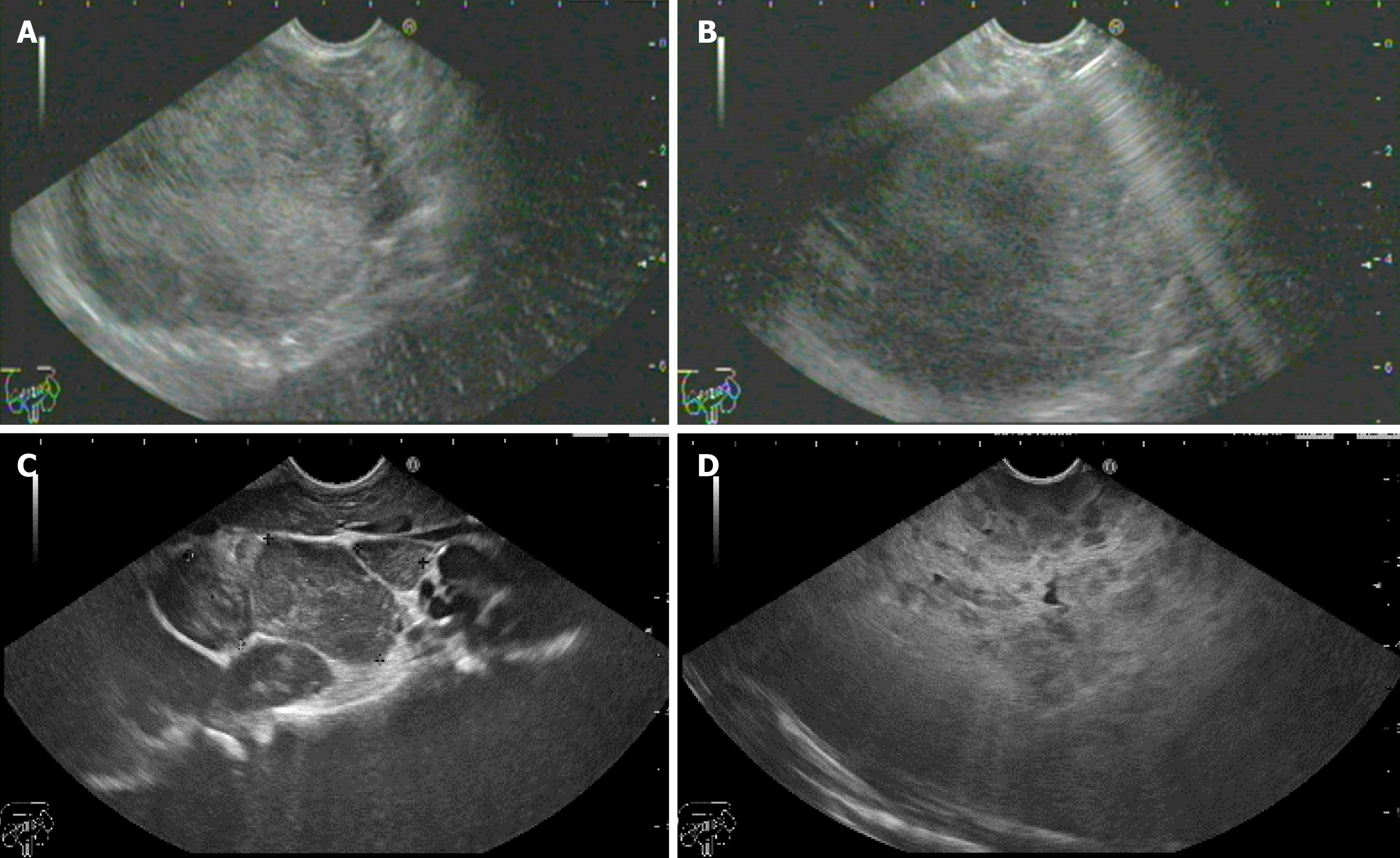
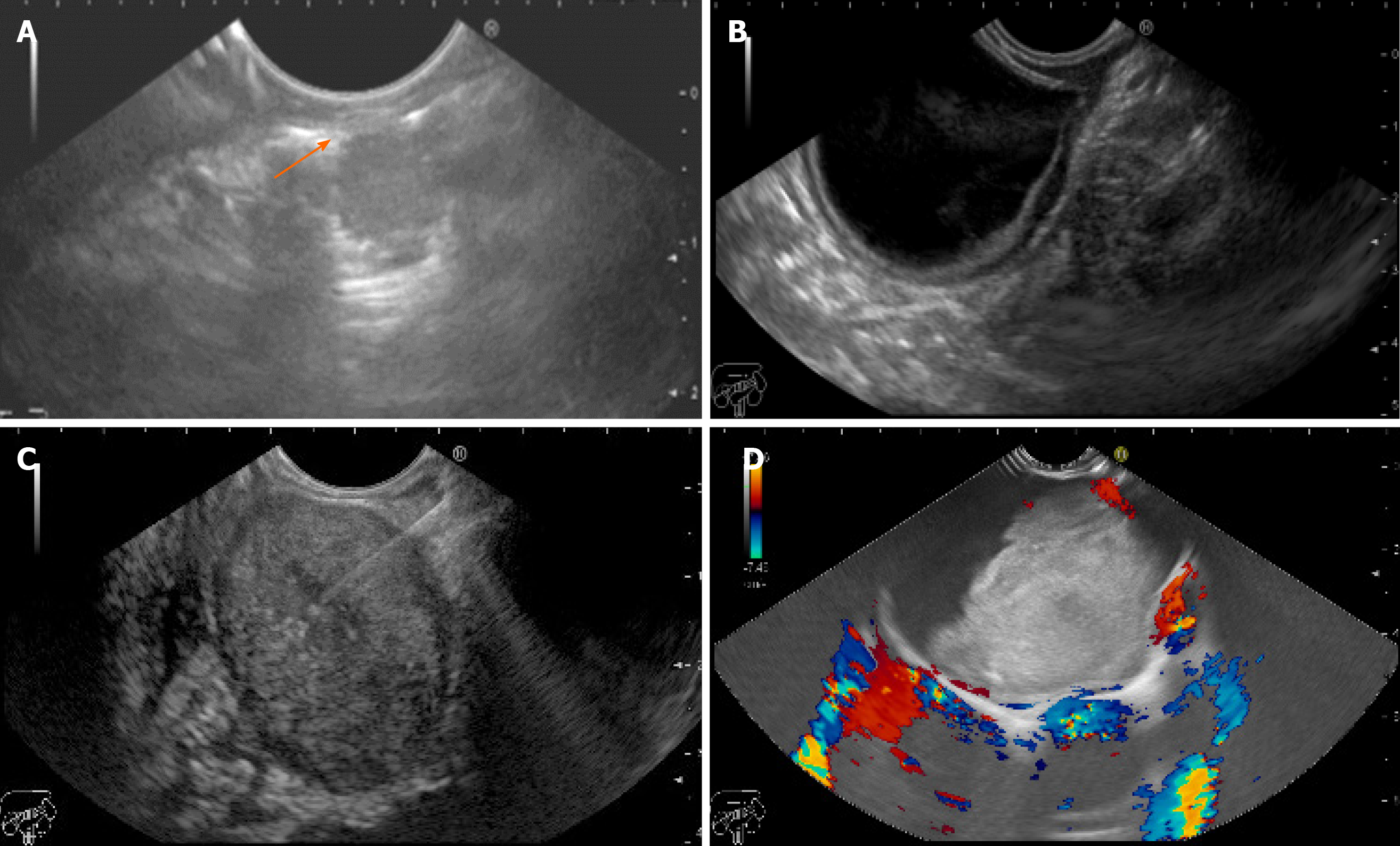
During the 4-year study period, a total of 13 (1.7%) pediatric EUS examinations out of 749 EUS procedures were performed in our unit. The mean age of the 8 females and 5 males was 15.6 years (range: 6-18). The procedures performed included 12 (92.3%) upper EUS and 1 (7.7%) lower EUS. Six of the EUS examinations were pancreatobiliary (46.1%), followed by mediastinal 2/13 (15.4%), peri-gastric 2/13 (15.4%), abdominal lymphadenopathy 1/13 (7.7%), tracheal 1/13 (7.7%) and rectal 1/13 (7.7%) (Table 1). Overall, EUS-FNA was performed in 7 patients (53.8%); using a 19G in 4 patients and a 22G needle in 3 patients with a diagnostic yield of 100%. In cystic lesions or lesions with a cystic component [solid pseudopapillary neoplasm (SPN)], a 19G needle was used. In solid lesions, a 22G needle was used with a median of 2 passes except for a rectal gastrointestinal stromal tumor (GIST) where a 19G needle was used to obtain sufficient tissue. No complications occurred during or after any of the procedures, which were all technically successful. Details of the indications, EUS findings (Figures 1-3), EUS-FNA, diagnosis and treatment are shown in (Table 2).
| Children | n = 13 |
| Females/males | 8/5 |
| Age (median) | 15.6 yr |
| Age (range) | 6-18 yr |
| Indications for EUS (n) | 13 |
| Upper | |
| Thoracic | |
| Tracheal mass | 1 |
| Mediastinal mass | 2 |
| Abdominal | |
| Pancreatic head mass | 1 |
| Retroperitoneal mass | 1 |
| Ampullary mass | 1 |
| Abdominal lymphadenopathy | 1 |
| Peri-gastric mass | 2 |
| Suspected insulinoma | 3 |
| Lower | |
| Rectal subepithelial lesion | 1 |
| EUS-FNA (n) | 7 |
| Solid | 5 |
| Cystic | 2 |
| Adverse events (n) | 0 |
| N | Age | Sex | Indication | EUS findings | EUS-FNA | Diagnosis | Treatment |
| 1 | 17 | F | Tracheal mass assessment before surgery | Hypoechoic tracheal mass measuring 13 mm × 9.5 mm separable from esophageal wall | Nil | Tracheal fibroma | Surgery |
| 2 | 15 | F | Pancreatic head mass | Isoechoic pancreatic head mass with hypoechoic rim about 30 mm × 25 mm separable from all vessels | 22G | Well differentiated NET | Surgery |
| 3 | 12 | F | Retroperitoneal mass | Isoechoic mass with small cystic areas about 60 mm × 60 mm compressing the SMA | 19G | SPN | Surgery |
| 4 | 15 | F | Ampullary mass | Ampullary cyst 35 mm × 30 mm with double wall and clear content | Nil | Duplication cyst | Endoscopic deroofing |
| 5 | 15 | F | Peri-gastric mass | Extraluminal cyst arising from the muscularis propria of antral wall with double wall about 40 mm × 35 mm | Nil | Duplication cyst | Follow up |
| 6 | 18 | M | Peri-gastric mass | Hypoechoic ill-defined peri-gastric collection with hyperechoic calcified areas | 19G | Postpancreatitis collection | Resolved with antibiotics |
| 7 | 17 | M | Rectal SEL | Exophytic rectal mass about 33 mm × 21 mm mostly arising from the muscularis propria with intact submucosa and mucosa | 19G | GIST | Surgery |
| 8 | 18 | M | Mediastinal mass | Large subcarinal cyst 10 cm × 7.6 cm compressing the right atrium and trachea with organized blood inside | 19G | Bronchogenic cyst | Full aspiration by EUS with no recurrence |
| 9 | 18 | F | Mediastinal mass | Multiple hypoechoic subcarinal, para-aortic and celiac lymph nodes, largest about 22 mm | 22G | Lymphoma | Chemotherapy |
| 10 | 18 | M | Abdominal lymphadenopathy | Multiple hypoechoic lymph nodes at portahepatis, para-aortic, and aorto-caval regions, largest about 55 mm × 34 mm. Splenomegaly with multiple focal lesions | 22G | Lymphoma | Chemotherapy |
| 11 | 18 | F | Suspected insulinoma | Normal pancreas with no detected lesions | Nil | Nil | Nil |
| 12 | 6 | M | Suspected insulinoma | Normal pancreas with no detected lesions | Nil | Nil | Nil |
| 13 | 17 | F | Suspected insulinoma | Normal pancreas with no detected lesions | Nil | Nil | Nil |
EUS had a significant impact on clinical care in 10/13 (77%) cases. In these cases, surgical treatment was carried out after accurate staging by EUS or a definitive diagnosis was reached by EUS-FNA in 4 cases (tracheal fibroma, pancreatic neuroendocrine tumor (NET), SPN, and rectal GIST). Chemotherapy was administered in 2 cases (lymphoma), endoscopic treatment was performed in 2 cases (deroofing of ampullary duplication cyst and aspiration of mediastinal bronchogenic cyst), and follow-up in 2 cases (gastric duplication cyst and peri-gastric postpancreatitis collection which resolved with antibiotics). In 3 cases with suspected insulinoma, EUS did not achieve a definitive diagnosis or therapy; as no pancreatic masses were detected.
The role of EUS in the adult population is wellestablished. However, it has not been adequately assessed in the pediatric population with gastrointestinal and pancreaticobiliary disorders. EUS in the pediatric population is most commonly performed for assessment of pancreatic solid/cystic lesions, pancreatitis (recurrent acute, chronic), suspected choledocholithiasis, subepithelial lesions such as duplication cysts and pancreatic rest, and benign/malignant lymphadenopathy. With the gradually increasing number of EUS indications in children, it is likely to gain more acceptance for the pediatric population[13].
The feasibility of EUS in pediatric patients was provided by the ASGE Technology Committee status evaluation report[14]. Based on the size of the echoendoscope, standard adult radial echoendoscopes (diameter: 12.7-14.2 mm) and linear echoendoscopes (diameter: 12.1-14.6 mm) can be used with caution in pediatric patients weighing more than 15 kg, given their relatively rigid distal tip. Throughthe scope miniprobes (frequency: 12-30 MHz) may be used safely in patients weighing less than 15 kg through the standard gastroscopes with a 2.8 mm working channel[14].
Herein, we report the experience of a single tertiary center in the use of EUS and EUS-FNA in a pediatric population and compare the findings to the most relevant studies in the literature assessing the role of EUS in children (Table 3). A total of 12 studies[3-12,15,16] were published between 1998 and 2019 including 524 patients and 584 EUS procedures. The age of the enrolled patients ranged between 0.5 and 21 years. Examination of the pancreatobiliary system was the main indication for EUS; which was performed in 396 (67.8%) cases. EUS-FNA was performed in 92 (15.7%) cases achieving a diagnosis in 81 cases with an overall diagnostic accuracy of 88% (7 cases in our study with a diagnostic accuracy of 100%). Therapeutic EUS was performed in 16 cases (7 pancreatic pseudocyst drainage, 7 celiac plexus block, 1 EUS-guided transgastric biliary drainage[4,6-8,15,16] and 1 mediastinal bronchogenic cyst aspiration in our study). The incidence rate of EUS-related complications ranged between 1.96% and 7.1%; which was reported in only 4 studies[3,4,6,16]. Complications included mild pancreatitis after FNA of solid pancreatic lesions, fever and bleeding after EUS-guided cystogastrostomy and anesthesia-related complications (hypoxia due to airway obstruction and laryngospasm). No complications occurred in any of the patients in our study during or after the procedures. With regard to the echoendoscopes, EUS procedures were performed with different echoendoscopes including radial, linear and recently the slim echoendoscope provided by Pentax (insertion tube of 10.8 mm, biopsy channel 2.8 mm; Pentax EG-3270UK, Pentax Hamburg, Germany) which can be used safely in children younger than 10 years. In our study, all EUS procedures were performed with the standard linear echoendoscope safely without any complications.
| Ref. | Patients, n | EUS, n | Time frame (yr) | Age range (yr) | Pancreatobiliary indications | Other indications | EUS-FNA |
| Roseau et al[9], 1998 | 18 | 23 | 7 | 4-16 | 8 | 15 | 0 |
| Varadarajulu et al[10], 2005 | 14 | 15 | 3 | 5-17 | 15 | 0 | 3 |
| Cohen et al[5], 2008 | 32 | 32 | 6 | 1.5-18 | 19 | 13 | 7 |
| Bjerring et al[11], 2008 | 18 | 18 | 16 | 0.5-15 | 11 | 7 | 0 |
| Attila et al[8], 2009 | 38 | 40 | 7 | 3-17 | 25 | 15 | 12 |
| Al-Rashdan et al[7], 2010 | 56 | 58 | 8 | 4-18 | 42 | 15 | 15 |
| Rosen et al[12], 2010 | 25 | 42 | 5 | NA | 0 | 42 | 0 |
| Scheers et al[4], 2015 | 48 | 52 | 14 | 2-17 | 52 | 0 | 12 |
| Gordon et al[6], 2016 | 43 | 51 | 6 | 4-18 | 34 | 17 | 13 |
| Mahajan et al[3], 2016 | 121 | 125 | 8 | 3-18 | 118 | 7 | 7 |
| Fugazza et al[15], 2017 | 40 | 47 | 6 | 3-18 | 28 | 19 | 3 |
| Raina et al[16], 2017 | 58 | 68 | 5 | 6-21 | 38 | 20 | 13 |
| Current study | 13 | 13 | 4 | 6-18 | 6 | 7 | 7 |
| Total | 524 | 584 | 3-16 | 0.5-21 | 396 | 177 | 92 |
Similar to previous studies, most of our EUS examinations were pancreatobiliary 6/13 (46.1%); mainly for solid pancreatic lesions or suspected insulinomas. EUS-FNA was performed in 7 patients and a definite diagnosis was achieved in all patients allowing them to undergo appropriate management (patients with pancreatic NET, SPN, and rectal GIST underwent surgery, those with mediastinal and abdominal lymphomas started chemotherapy, peri-gastric postpancreatitis collection resolved with antibiotics, and a mediastinal bronchogenic cyst was completely aspirated). A commonly reported therapeutic indication for EUS in pediatrics is the drainage of pancreatic fluid collections[4,15,16]. In the present study, the child who presented with a large mediastinal bronchogenic cyst (10 cm × 7.6 cm) underwent successful EUS-guided aspiration of the cyst content with no recurrence within 6 mo after aspiration. In the 3 cases with suspected insulinomas, one patient subsequently underwent surgical intervention and was diagnosed with nesidioblastosis and 2 patients underwent further evaluation.
In this study, integration of EUS into the management plan had a significant impact on the clinical care in 77% of cases. This was comparable to the study by Varadarajulu et al[10], who reported that EUS had a significant impact on the clinical care of 13 out of 14 patients (93%) with pancreaticobiliary disorders. Similarly, Raina et al[16] reported a significant impact on clinical care in 88% of cases and AlRashdan et al[7] reported a different diagnosis achieved by EUS in 86% of cases. These data suggest that EUS when performed by expert endosonographers is safe, feasible, and has a significant impact on the clinical care of pediatric patients.
Many factors affect the choice of sedation during pediatric EUS procedures including: The expected duration of the procedure, the expected level of patient cooperation particularly during EUS-FNA, the American Standards Association classification of the patient, and the personal preference of the patients and parents, as well as the endoscopists[8]. In our study, all procedures were performed under intravenous propofol sedation. However, the available data in the literature are insufficient to make recommendations about the safety, adequacy, and cost of general anesthesia vs intravenously administered moderate sedation for EUS in pediatric patients.
The present study has some limitations. First, the number of patients included in the study was relatively small; with infants and younger children not well represented, limiting the ability to generalize results to all age groups. Second, it was a single tertiary center experience with retrospective data analysis, with possible selection and recall bias. Finally, the rarity of the performed therapeutic EUS procedures does not allow definite conclusions.
EUS and EUS-FNA in the pediatric population are safe, feasible, and have a significant clinical impact on subsequent management; thus avoiding more invasive and additional unnecessary procedures. EUS utilization in pediatrics although rare, is expected to increase in the future. Dedicated EUS programs in high volume tertiary centers can ensure that the correct indications are followed, with a high impact on patient management and safety of procedures in the pediatric population.
Although endoscopic ultrasound (EUS) is now widely available and has an established role in adults, the utility of EUS and EUS-guided fine needle aspiration (EUS-FNA) in pediatrics is insufficiently described compared to adults and is only supported by a few studies.
More effort is necessary to increase the awareness of EUS among pediatric gastroenterologists, as it may have a clinical impact on the subsequent management and minimize unnecessary procedures in children.
The aim of this study was to report the experience of a single tertiary center in the use of EUS and EUS-FNA in a pediatric population and to further assess its safety, feasibility, and clinical impact on the subsequent management.
This was a retrospective study. The patient’s medical records were reviewed for standard data which included patient demographics, initial diagnosis, previous abdominal ultrasound, computed tomography, or magnetic resonance imaging, EUS indications, EUS findings, impact of EUS on the patient’s clinical care, and adverse events.
During the 4-year study period, a total of 13 (1.7%) pediatric EUS examinations out of 749 EUS procedures were performed in our unit. The mean age of the 8 females and 5 males was 15.6 years (range: 6-18). Most of EUS examinations were pancreatobiliary. Overall, EUS-FNA was performed in 7 patients (53.8%) with a diagnostic yield of 100%. EUS had a significant impact on clinical care in 10/13 (77%) cases. No complications occurred in our patients during or after any of the procedures.
EUS and EUS-FNA in the pediatric population are safe, feasible, and have a significant clinical impact on subsequent management; thus avoiding more invasive and additional unnecessary procedures.
EUS utilization in pediatrics although rare, is expected to increase in the future. Dedicated EUS programs in high volume tertiary centers can ensure that the correct indications are followed, with a high impact on patient management and safety of procedures in the pediatric population.
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Society for Gastrointestinal Endoscopy, No. 176293.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ashida R, Faias S, Lai JP, Sugimoto M S-Editor: Zhang L L-Editor: Webster JR P-Editor: Wang LL
| 1. | LeBlanc JK, DeWitt J, Sherman S. Endoscopic ultrasound: how does it aid the surgeon? Adv Surg. 2007;41:17-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Kieling CO, Hallal C, Spessato CO, Ribeiro LM, Breyer H, Goldani HA, Maguilnik I. Changing pattern of indications of endoscopic retrograde cholangiopancreatography in children and adolescents: a twelve-year experience. World J Pediatr. 2015;11:154-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Mahajan R, Simon EG, Chacko A, Reddy DV, Kalyan PR, Joseph AJ, Dutta AK, Chowdhury SD, Kurien RT. Endoscopic ultrasonography in pediatric patients--Experience from a tertiary care center in India. Indian J Gastroenterol. 2016;35:14-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Scheers I, Ergun M, Aouattah T, Piessevaux H, Borbath I, Stephenne X, De Magnée C, Reding R, Sokal E, Veyckemans F, Weynand B, Deprez PH. Diagnostic and Therapeutic Roles of Endoscopic Ultrasound in Pediatric Pancreaticobiliary Disorders. J Pediatr Gastroenterol Nutr. 2015;61:238-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Cohen S, Kalinin M, Yaron A, Givony S, Reif S, Santo E. Endoscopic ultrasonography in pediatric patients with gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2008;46:551-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Gordon K, Conway J, Evans J, Petty J, Fortunato JE, Mishra G. EUS and EUS-Guided Interventions Alter Clinical Management in Children with Digestive Diseases. J Pediatr Gastroenterol Nutr. 2016;63:242-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Al-Rashdan A, LeBlanc J, Sherman S, McHenry L, DeWitt J, Al-Haddad M. Role of endoscopic ultrasound for evaluating gastrointestinal tract disorders in pediatrics: a tertiary care center experience. J Pediatr Gastroenterol Nutr. 2010;51:718-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Attila T, Adler DG, Hilden K, Faigel DO. EUS in pediatric patients. Gastrointest Endosc. 2009;70:892-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Roseau G, Palazzo L, Dumontier I, Mougenot JF, Chaussade S, Navarro J, Couturier D. Endoscopic ultrasonography in the evaluation of pediatric digestive diseases: preliminary results. Endoscopy. 1998;30:477-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Varadarajulu S, Wilcox CM, Eloubeidi MA. Impact of EUS in the evaluation of pancreaticobiliary disorders in children. Gastrointest Endosc. 2005;62:239-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Bjerring OS, Durup J, Qvist N, Mortensen MB. Impact of upper gastrointestinal endoscopic ultrasound in children. J Pediatr Gastroenterol Nutr. 2008;47:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Rosen MJ, Moulton DE, Koyama T, Morgan WM, Morrow SE, Herline AJ, Muldoon RL, Wise PE, Polk DB, Schwartz DA. Endoscopic ultrasound to guide the combined medical and surgical management of pediatric perianal Crohn's disease. Inflamm Bowel Dis. 2010;16:461-468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Singh RR, Choudhary NS, Puri R. Role of endoscopic ultrasound in pediatric gastrointestinal diseases. J Dig Endosc. 2016;7:104-109. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | ASGE Technology Committee, Barth BA, Banerjee S, Bhat YM, Desilets DJ, Gottlieb KT, Maple JT, Pfau PR, Pleskow DK, Siddiqui UD, Tokar JL, Wang A, Song LM, Rodriguez SA. Equipment for pediatric endoscopy. Gastrointest Endosc. 2012;76:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Fugazza A, Bizzarri B, Gaiani F, Manfredi M, Ghiselli A, Crafa P, Carra MC, de'Angelis N, de'Angelis GL. The role of endoscopic ultrasound in children with Pancreatobiliary and gastrointestinal disorders: a single center series and review of the literature. BMC Pediatr. 2017;17:203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Raina A, Conrad MA, Sahn B, Sedarat A, Ginsberg GG, Ahmad NA, Chandrasekhara V, Mamula P, Kochman ML. Endoscopic ultrasound with or without fine-needle aspiration has a meaningful impact on clinical care in the pediatric population. Endosc Ultrasound. 2017;6:195-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |