Published online Jul 16, 2019. doi: 10.4253/wjge.v11.i7.438
Peer-review started: May 14, 2019
First decision: May 31, 2019
Revised: June 5, 2019
Accepted: June 20, 2019
Article in press: June 21, 2019
Published online: July 16, 2019
Processing time: 69 Days and 8.2 Hours
Rectal Dieulafoy's lesions (DLs) are very rare; however, they can be life threatening when presented with massive hemorrhage.
A 44-year-old female with medical history of chronic renal failure who was on renal replacement therapy presented with lower gastrointestinal hemorrhage. Physical examination revealed signs of hypovolemic shock and massive rectal bleeding. Complete blood count revealed abrupt decrease in hematocrit. After hemodynamic stabilization, an urgent colonoscopy was performed. A rectal DL was diagnosed, and it was successfully treated with two hemoclips. There were no signs of recurrent bleeding at thirty days of follow-up.
Rectal DLs represent an unusual cause of lower gastrointestinal bleeding. Massive hemorrhage can increase the morbidity and mortality of these patients. Endoscopic management continues to be the reference standard in the diagnosis and therapy of these lesions. Thermal, mechanical (hemoclip or band ligation), or combination therapy (adrenaline injection combined with thermal or mechanical therapy) should be considered the first choice for treatment.
Core tip: Rectal Dieulafoy's lesion (DL) represents an unusual cause of lower gastrointestinal bleeding. A 44-year-old female with medical history of chronic renal failure presented massive rectal bleeding. After proper initial management, an urgent colonoscopy was performed. A rectal DL was diagnosed and successfully treated with two hemoclips without recurrence of hemorrhage. Endoscopy is the reference standard for the diagnosis and treatment of these lesions.
- Citation: Pineda-De Paz MR, Rosario-Morel MM, Lopez-Fuentes JG, Waller-Gonzalez LA, Soto-Solis R. Endoscopic management of massive rectal bleeding from a Dieulafoy's lesion: Case report. World J Gastrointest Endosc 2019; 11(7): 438-442
- URL: https://www.wjgnet.com/1948-5190/full/v11/i7/438.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i7.438
Dieulafoy's lesions (DLs) represent less than 5% of all causes of gastrointestinal bleeding. These lesions were initially described as gastric aneurysms by Gallard in 1884, but it was in 1898 when George Dieulafoy, a French surgeon, identified them in three patients as the cause of gastrointestinal bleeding[1]. More than 90% of the lesions are located at the upper gastrointestinal tract and only 2% are found at the rectum[2]. Unlike the proximal lesions, rectal DLs (RDL) usually present hematochezia and/or fresh bleeding. The literature reveals only few case reports of RDL. We report the case of profuse lower gastrointestinal hemorrhage due to a RDL, as well as the proper literature review.
A 44-year-old female patient hospitalized in our institution due to a vascular access infection.
The patient presented profuse rectal bleeding that progressed to hypovolemic shock in four hours.
Her medical comorbidities included chronic kidney disease on replacement therapy and secondary hypertension. Patient denied any toxic habits.
Her surgical history included two cesarean sections, appendectomy, and living-donor kidney transplant followed by acute rejection. Family history was negative for any gastrointestinal disease.
On presentation her vital signs were temperature of 36 °C, pulse of 120 bpm, respiratory rate of 20 rpm, blood pressure of 80/50 mmHg, and oxygen saturation of 92%. On general physical examination she looked pale and dehydrated. Abdominal examination revealed non-distended, soft, non-tender abdomen with normal bowel sounds. Rectal examination revealed bright blood with clots. The cardiovascular, pulmonary and neurological examination was unremarkable.
Complete blood count analysis revealed hemoglobin of 6.7 g/dL, normal platelet count (193000/mm3), partial thromboplastin time of 42 s (RV 25-33), prothrombin time of 20 s (RV 11-15), and international normalized ratio 1.86.
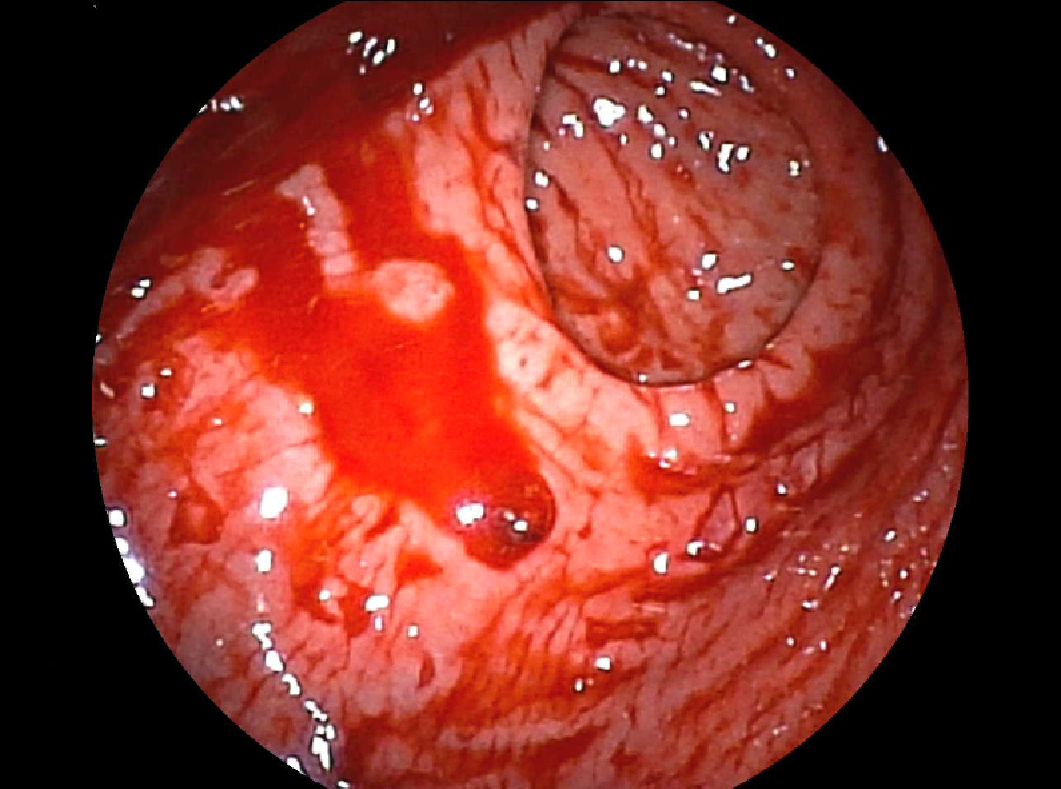
Urgent colonoscopy findings were active bleeding from small bulgy vessel with minimal surrounding erosion and no ulcerative lesions (Figure 1).
The final diagnosis of the presented case was a RDL.
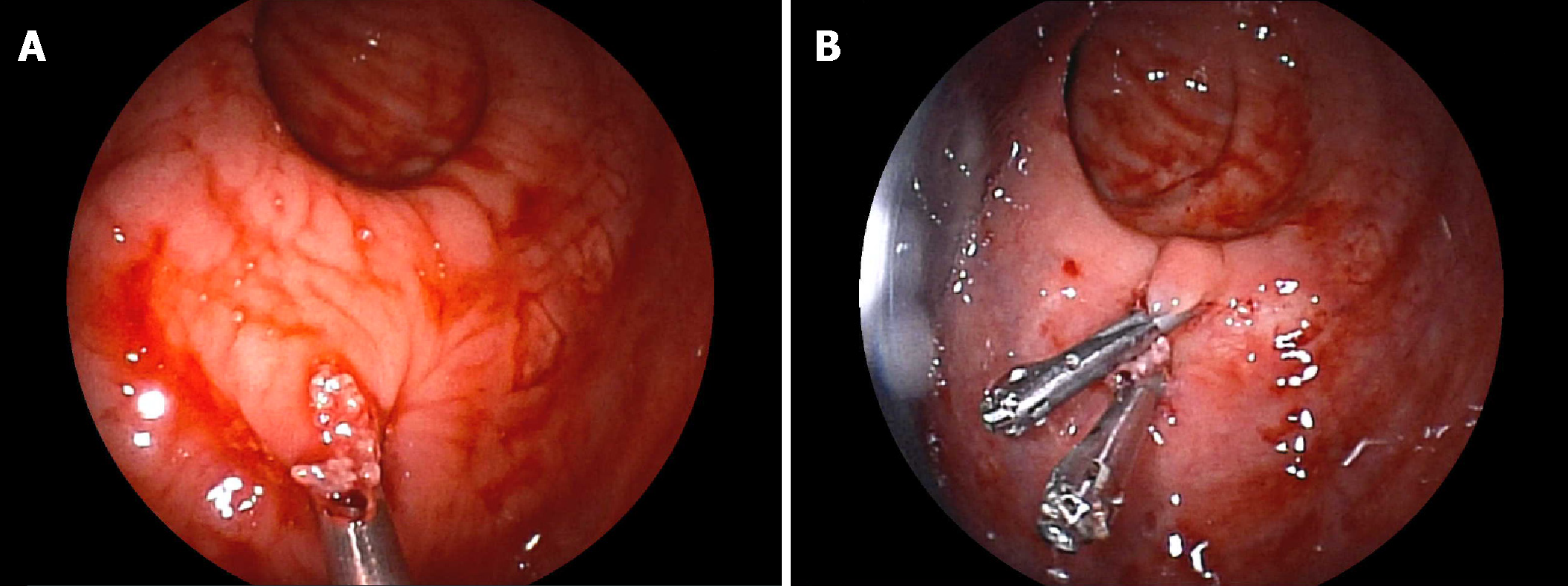
For the management of the hypovolemic shock, proper resuscitation with crystalloids, transfusion of packed red blood cells and vasoactive agents was performed. After hemodynamic stabilization, endoscopic therapy with two hemoclips (Figure 2) was done.
Immediate hemostasis was achieved with endoscopic management, and on the fifth day the patient was discharged. There were no signs of recurrent bleeding at thirty days of follow-up.
DLs represent an unusual cause of non-variceal gastrointestinal bleeding, accounting for less than 5% of all cases. More than 90% of these lesions are located at the esophagus, stomach and duodenum; only 2% are found at the rectum. The most relevant histological findings are aneurysm and inflammation, but a biopsy is not usually necessary[2]. The reference standard for diagnosis is endoscopy. Common findings include a small, usually less than 3 mm, protruding pulsatile lesion surrounded by normal mucosa, with or without active bleeding[3].
Unlike the manifestations described in other parts of the digestive tract, RDL usually present with rectorrhagia or hematoquezia. There are previous case reports of profuse rectal bleeding, but most of them didn't evolve to hypovolemic shock as occurred with our patient. A computed tomography angiography was canceled due to hemodynamic instability in the CT-room. This hemodynamic instability can impact in the morbidity and mortality of these patients[4,5].
If technically feasible, the first line of treatment is endoscopic hemostasis. The European Gastrointestinal Endoscopy Society (ESGE) recommends endoscopic hemostasis for DLs, including: thermal coagulation, mechanical hemostasis (hemoclips or band ligation), or combined therapy (diluted adrenaline injection plus contact thermal or mechanical therapy)[6]. These endoscopic hemostasis techniques are safe and have similar outcomes in observational studies. As in other causes of non-variceal bleeding, there is superiority of combined, thermal and mechanical methods over injection monotherapy[6]. Endoscopic treatment achieves an initial hemostasis rate > 93.6% of cases, with a rebleeding rate of 12.1%, including cases of RDL[7,8]. A prospective study demonstrated superiority of mechanical endoscopic treatment with hemoclips or band ligation versus injection with diluted adrenaline[9]. Regarding to the mechanical therapy, there is no differences in endoscopic band ligation vs hemoclips. A meta-analysis that included 5 studies, compared endoscopic band ligation (75 patients) versus hemoclips (87 patients) for primary hemostasis of DLs; results didn't find any difference for the primary outcome [0.96 (95%CI: 0.88-0.99) vs 0.91 (95%CI: 0.83-0.96), respectively]; there were no differences in rebleeding rates neither [0.06 (95%CI: 0.02-0.15) vs 0.17 (95%CI: 0.10-0.28), respectively][10]. In our patient, there was no rebleeding after the initial effective hemostasis with the place-ment of two hemoclips. Table 1 shows a summary of endoscopic treatment modalities.
| Technique | Initial hemostasis (%) | Rebleeding (%) | Mortality (%) | Adverse events1 (%) |
| Thermal | ||||
| Bipolar EC | 80 | 13.3 | 0 | 0 |
| APC | 100 | 3.4 | NA | 3.4 |
| Injection | ||||
| Epinephrine | 88 | 32.7 | 2.4 | 0 |
| Mechanical | ||||
| Hemoclip | 94.7 | 10.5 | 0.4 | 0.5 |
| EBL | 99.2 | 5.3 | 0 | 0.8 |
| Combined | ||||
| Epinephrine + Hemoclip | 98.2 | 5 | 0 | 0 |
| Epinephrine + EBL | 100 | 0 | 0 | 0 |
Transcatheter angiographic embolization (TAE) should be the next option in cases that can't be treated endoscopically[6,11]. Surgical resection should be reserved for selected cases that can't be treated with endoscopic or angiographic methods[6,12].
Rectal DLs represent a rare cause of lower gastrointestinal bleeding. Massive hemorrhage can increase the morbidity and mortality of these patients. Endoscopic management continues to be the reference standard in the diagnostic and therapeutic approach. Thermal, mechanical (hemoclip or band ligation), or combination therapy (adrenaline injection combined with thermal or mechanical therapy) should be considered the first choice for treatment.
CARE Checklist – 2016 The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Mexico
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Chen CH, Sandhu DS, Vynios D S-Editor: Ma YJ L-Editor:A E-Editor: Wu YXJ
| 1. | Chaer RA, Helton WS. Dieulafoy's disease. J Am Coll Surg. 2003;196:290-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Lara LF, Sreenarasimhaiah J, Jiang Tang S, Alonso BB, Rochey DC. Localization, efficacy of therapy and outcomes of Dieulafoy's lesions of the GI tract-the UT Southwestern GI Bleed Team experience. Gastrointest Endosc. 2008;67:AB87. [DOI] [Full Text] |
| 3. | Lee YT, Walmsley RS, Leong RW, Sung JJ. Dieulafoy's lesion. Gastrointest Endosc. 2003;58:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Tursi A. Rectal Dieulafoy lesion. Clin Res Hepatol Gastroenterol. 2017;41:1-2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Kanth R, Mali P, Roy PK. Outcomes in Dieulafoy's Lesion: A 10-Year Clinical Review. Dig Dis Sci. 2015;60:2097-2103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Gralnek IM, Dumonceau JM, Kuipers EJ, Lanas A, Sanders DS, Kurien M, Rotondano G, Hucl T, Dinis-Ribeiro M, Marmo R, Racz I, Arezzo A, Hoffmann RT, Lesur G, de Franchis R, Aabakken L, Veitch A, Radaelli F, Salgueiro P, Cardoso R, Maia L, Zullo A, Cipolletta L, Hassan C. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:a1-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 494] [Article Influence: 49.4] [Reference Citation Analysis (0)] |
| 7. | Nguyen DC, Jackson CS. The Dieulafoy's Lesion: An Update on Evaluation, Diagnosis, and Management. J Clin Gastroenterol. 2015;49:541-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Park JG, Park JC, Kwon YH, Ahn SY, Jeon SW. Endoscopic Management of Rectal Dieulafoy's Lesion: A Case Series and Optimal Treatment. Clin Endosc. 2014;47:362-366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Chung IK, Kim EJ, Lee MS, Kim HS, Park SH, Lee MH, Kim SJ, Cho MS. Bleeding Dieulafoy's lesions and the choice of endoscopic method: comparing the hemostatic efficacy of mechanical and injection methods. Gastrointest Endosc. 2000;52:721-724. [PubMed] |
| 10. | Barakat M, Hamed A, Shady A, Homsi M, Eskaros S. Endoscopic band ligation versus endoscopic hemoclip placement for Dieulafoy's lesion: a meta-analysis. Eur J Gastroenterol Hepatol. 2018;30:995-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Alshumrani G, Almuaikeel M. Angiographic findings and endovascular embolization in Dieulafoy disease: a case report and literature review. Diagn Interv Radiol. 2006;12:151-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Dogan U, Gomceli I, Koc U, Habibi M, Bulbuller N. Rectal dieulafoy lesions: a rare etiology of chronic lower gastrointestinal bleeding. Case Rep Med. 2014;2014:180230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |