Published online Jul 16, 2019. doi: 10.4253/wjge.v11.i7.427
Peer-review started: May 10, 2019
First decision: May 31, 2019
Revised: June 7, 2019
Accepted: June 20, 2019
Article in press: June 21, 2019
Published online: July 16, 2019
Processing time: 72 Days and 11.4 Hours
The current guidelines suggest that patients should undergo endoscopic evaluation of the colonic lumen after an episode of computed tomography (CT) proven acute diverticulitis to rule out malignancy. The usefulness of routine endoscopic evaluation of CT proven diverticulitis remains unknown.
To establish whether routine colonoscopy should be offered to patients after an episode of diverticulitis.
We performed a retrospective study, comparing two groups: a diverticulitis group and a control group. The diverticulitis group consisted of patients undergoing a colonoscopy after an episode of diverticulitis. The control group consisted of asymptomatic patients undergoing a screening sigmoidoscopy. We also performed a systematic review and meta-analysis. We searched electronic data resources to identify all relevant studies. The primary outcome was the number of adenomas found, while the secondary outcomes were the number of cancers and polyps identified, and the adenoma risk.
68 and 1309 patients were included in the diverticulitis and control groups respectively. There was no difference in the risk of adenomas (5.9% vs 7.6%, P = 0.59), non-advanced adenomas (5.9% vs 6.9%, P = 0.75), advanced adenomas (0% vs 0.8%, P = 1), cancer (0% vs 0.15%, P = 1.00), and polyps (16.2% vs 14.2%, P = 0.65) between both groups. Meta-analysis of data from 4 retrospective observational studies, enrolling 4459 patients, showed no difference between the groups in terms of risk of adenomas (RD = -0.05, 95%CI: -0.11, 0.01, P = 0.10), non-advanced adenomas (RD = -0.02, 95%CI: -0.08, 0.04, P = 0.44), advanced adenomas (RD = -0.01, 95%CI: -0.04, 0.02, P = 0.36), cancer (RD = 0.01, 95%CI: -0.01, 0.03, P = 0.32), and polyps (RD = -0.05, 95%CI: -0.12, 0.02, P = 0.18).
Routine colonoscopy may not be appropriate in patients with acute diverticulitis. High quality prospective studies are required for more robust conclusions.
Core tip: The results of this study suggest that patients with computed tomography (CT)-proven acute diverticulitis are not at increased risk of colonic adenomas and neoplastic lesions as indicated by comparable endoscopic findings to general populations undergoing screening endoscopy. This suggests that endoscopic evaluation of colon may not be beneficial in cases with CT-proven acute diverticulitis and could be preserved for selected cases only. Our results are consistent with the best available evidence in the literature. However, the best available evidence is derived from a limited number of retrospective studies with moderate quality. High quality prospective studies are required for definite conclusions.
- Citation: Asaad P, Hajibandeh S, Rahm M, Johnston T, Chowdhury S, Bronder C. Should a colonoscopy be offered routinely to patients with CT proven acute diverticulitis? A retrospective cohort study and meta-analysis of best available evidence. World J Gastrointest Endosc 2019; 11(7): 427-437
- URL: https://www.wjgnet.com/1948-5190/full/v11/i7/427.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i7.427
Diverticulosis is a common colonic condition, which increases in prevalence with age. In the United States, 50% of people over 50 years old, and 75% of people over 80 years old, are affected by this condition[1]. Although most of these patients remain asymptomatic, between 10%–25% of patients with diverticulosis, do develop diverticulitis[2]. That means, up to 12.5% of people over 50 years old, will develop diverticulitis in their lifetime. This represents a significant burden on the healthcare system, and therefore, it is important to have clear and evidence-based protocols to manage this condition.
The Association of Coloproctologists of Great Britain and Ireland (ACPGBI) guidelines, and the American Society of Colon and Rectal Surgeons (ASCRS) guidelines, both stipulate, that patients with a suspected episode of acute diver-ticulitis, should undergo a computed tomography (CT) scan during the acute episode for diagnostic purposes, and an endoscopic evaluation of the colonic lumen after the acute episode, to rule out other pathologies such as malignancy or inflammatory bowel disease[3,4]. The World Society of Emergency Surgery (WSES) published guidelines, suggesting that patients with diverticular abscesses treated conservatively require early colonic evaluation with colonoscopy, however, patients with CT proven uncomplicated diverticulitis do not require follow-up colonoscopy[5]. However, these guidelines are mainly based on expert opinion and low quality evidence[5].
Previously, diverticulitis was mainly a clinical diagnosis, and barium enema was the investigation of choice to assess this[6,7]. With the evolution and ease of access of modern day CT imaging, it has since become the gold standard of investigation for many intra-abdominal conditions, including diverticulitis. It has a high sensitivity and specificity in detecting diverticulitis, as well as its complications[6,7]. On the other hand, colonoscopy by nature is invasive. It is associated with discomfort, particularly in patients with diverticular disease[6]. Patients with diverticular disease also have more difficult endoscopic procedures, and have a higher risk of perforation[8]. Cost-effectiveness of investigating every CT-proven diverticulitis remains unclear[9]. Because of this, several authors, between the years 2011 to 2017 have tried to investigate the usefulness of endoscopy post CT-proven diverticulitis. It is interesting to note, that the vast majority of studies concluded that there was no benefit for endoscopic evaluation post CT-proven diverticulitis, in particular, for those patients with uncomplicated diverticulitis[6,7,10-21]. This is contradictory to the guidelines’ recommendations.
Our objective was to assess the usefulness of endoscopic evaluation of CT proven diverticulitis. To achieve this objective, we conducted a multicentre retrospective cohort to assess the risk of colonic adenoma in patients with CT-proven diverticulitis compared to those in general population undergoing colonoscopy for bowel cancer screening. Furthermore, we conducted a systematic review of the literature and meta-analysis of outcomes to provide the best available comparative evidence on usefulness of endoscopic evaluation of CT proven diverticulitis.
On gaining approval from the clinical governance department unit, we conducted a retrospective cohort study in three centres in the north west of England. The study group included consecutive patients who were admitted to our trust with an episode of acute diverticulitis over a three-year period between January 2014 and December 2016. The control group included all patients who had undergone a one-off screening flexible sigmoidoscopy at the age of fifty-five, as part of the National Bowel Cancer Screening Programme over a fourteen-month period between October 2015 and December 2016.
For the study group, we considered all participants of any age or gender with an episode of CT-proven acute diverticulitis who subsequently underwent endoscopic evaluation of colon. Endoscopic evaluation of interest included either a flexible sigmoidoscopy or a colonoscopy. All patients who did not have CT scan for diagnosis of diverticulitis and those who did not have subsequent endoscopic evaluation were excluded. For the screening group, we considered participants of any age or gender in general population who underwent endoscopic evaluation of colon at the age of fifty-five as part of the National Bowel Screening Programme. Symptomatic patients were excluded.
A data collection proforma was designed for data collection. The proforma included data on participant’s demographics (age and gender), type of endoscopic evaluation (flexible sigmoidoscopy or colonoscopy), endoscopic findings and outcomes [the number of polyps found, the number of adenomas found, the risk of the adenomas (low-risk, intermediate-risk, or high-risk), the number of cancers found, and the final histology]. Data collection was performed by three independent authors. Any discrepancies were resolved by discussion between the authors. An independent fourth author was consulted in the event of disagreement.
We considered the total number of adenomas, non-advanced adenomas, and advanced adenomas as primary outcome measures. The secondary outcomes included low-risk adenomas, intermediate-risk adenomas, high-risk adenomas, invasive cancers, total number of polyps, and hyperplastic polyps.
Advanced adenomas were defined as adenomas that on histology were greater than 1 cm in size, have a villous component, or have high-grade dysplasia. All other adenomas were non-advanced adenomas. Based on endoscopy findings, low-risk adenomas were defined as patients with only one or two small adenomas. Intermediate-risk adenomas were defined as patients with three to four small adenomas or one large adenoma. High-risk adenomas were defined as patients with five or more small adenomas, or three or more adenomas with at least one of them being large. Small adenomas were those that were less than 1 cm in size, while large adenomas were defined as those that were greater 1 cm in size.
Simple descriptive statistics was applied to present demographics, clinical characteristics, and outcome data. Data were summarized with mean ± SD for continuous variables, and frequencies/percentages for categorical variables. Differences between the groups were tested for statistical significance using the independent t-test for continuous variables and the χ2 test or Fisher exact test for categorical variables, as appropriate. All statistical tests were two-tailed and statistical significance was assumed at P < 0.05. Statistical analyses was performed using Minitab 17 (Minitab® 17.1.0).
We performed a systematic review according to an agreed predefined protocol and we were compliant with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement standards[22]. We conducted a search of electronic information sources, including MEDLINE; EMBASE; CINAHL; the Cochrane Central Register of Controlled Trials (CENTRAL); the World Health Organization International Clinical Trials Registry; ClinicalTrials.gov; and ISRCTN Register, and bibliographic reference lists to identify all studies comparing the risk of colonic adenoma and neoplastic lesions in patients with CT-proven diverticulitis compared to those in general population undergoing endoscopic evaluation for bowel cancer screening. Our data extraction spreadsheet included study-related data (first author, year of publication, country of origin of the corresponding author, journal in which the study was published, study design, study size, clinical condition of the study participants), baseline demographic information of the included populations (age, gender), and primary and secondary outcome data (adenomas, non-advanced adenomas, advanced adenomas, polyps, and invasive cancers). The methodological quality and risk of bias of the included studies were assessed using the Newcastle-Ottawa scale (NOS)[23]. Literature search, study selection, data collection, and methodological quality assessment were performed by two independent authors. Any discrepancies were resolved by discussion between the authors. An independent third author was consulted in the event of disagreement. We calculated the risk difference (RD) as the summary measure. Heterogeneity among the studies was assessed using the Cochran Q test (χ2). Random or fixed effects modelling were used as appropriate for analysis; random effects models were used if considerable heterogeneity was found among the studies. The results were reported in a forest plot with 95% confidence intervals (CIs). We used the Review Manager 5.3 software for data synthesis.
A total of 1377 patients were included in this study. Of these, 68 patients were included in the diverticulitis group and 1309 patients were included in the screening group. The mean age of the included patients in the diverticulitis group and screening group were 59.1(95%CI: 55.67- 62.4) and 55.4 (95%CI: 55.1-55.7), respectively. Thirty five out of 68 and 694 out of 1309 were male in the diverticulitis group and screening group, respectively (51.5% vs 53.0%, P = 0.94). Diverticulitis had been confirmed by CT scan in all patients in the diverticulitis group. In terms of endoscopic evaluation of colon, all patients in the diverticulitis group underwent colonoscopy while patients in the screening group underwent flexible sigmoidoscopy. Time from diagnosis of diverticulitis and endoscopic evaluations of the colon ranged from 2 to 12 mo.
The outcome data is summarised in Table 1
| Diverticulitis group | Screening group | P-value | |
| Total number of patients | 68 | 1309 | - |
| Mean age | 59.1(55.67- 62.4) | 55.4 (55.1, 55.7) | < 0.001 |
| Male patients | 35 of 68 (51.5%) | 694 out of 1309 | 0.94 |
| Patients with adenoma | 4 out of 68 (5.9%) | 100 out of 1309 (7.6%) | 0.59 |
| Patients with non-advanced adenoma | 4 out of 68 (5.9%) | 90 out of 1309 (6.9%) | 0.75 |
| Patients with advanced adenoma | 0 out of 68 (0%) | 10 out of 1309 (0.8%) | 1 |
| Patients with low-risk adenoma | 4 out of 68 (5.9%) | 84 out of 1309 (6.4%) | 0.86 |
| Patients with intermediate-risk adenoma | 0 out of 68 (0%) | 12 out of 1309 (0.92%) | 1 |
| Patients with high-risk adenoma | 0 out of 68 (0%) | 4 out of 1309 (0.31%) | 1 |
| Patients with cancers | 0 out of 68 (0%) | 2 out of 1309 (0.15%) | 1 |
| Patients with polyps | 11 out of 68 (16.2%) | 186 out of 1309 (14.2%) | 0.65 |
| Patients with hyperplastic polyps | 6 out of 68 (8.8%) | 60 out of 1309 (4.6%) | 0.11 |
| Patients with unbiopsied polyps | 1 out of 68 (1.5%) | 24 out of 1309 (1.8%) | 0.83 |
Adenomas: In the diverticulitis group, 4 out of 68 patients were found to have adenomas (5.9%), while in the screening group, 100 out of 1309 patients were found to have adenomas (7.6%). There was no significant difference in the total number of adenomas between the two groups (5.9% vs 7.6%, P = 0.59).
Non-advanced adenomas: In the diverticulitis group, 4 out of 68 patients were found to have non-advanced adenomas (5.9%), while in the screening group, 90 out of 1309 patients were found to have non-advanced adenomas (6.9%). There was no significant difference in the total number of non-advanced adenomas between the two groups (5.9% vs 6.9%, P = 0.75).
Advanced adenomas: In the diverticulitis group, 0 out of 68 patients were found to have advanced adenomas (0%), while in the screening group, 10 out of 1309 patients were found to have advanced adenomas (0.8%). There was no significant difference in the total number of advanced adenomas between the two groups (0% vs 0.8%, P = 1).
Low-risk adenoma: In the diverticulitis group, 4 out of 68 patients were found to have low-risk adenoma (5.9%), while in the screening group, 84 out of 1309 patients were found to have low-risk adenoma (6.4%). There was no significant difference in the risk of low-risk adenomas between the two groups (5.9% vs 6.4%, P = 0.86).
Intermediate-risk adenoma: In the diverticulitis group, 0 out of 68 patients were found to have intermediate-risk adenoma (0%), while in the screening group, 12 out of 1309 patients were found to have intermediate-risk adenoma (0.92%). There was no significant difference in the risk of intermediate-risk adenomas between the two groups (0% vs 0.92%, P = 1.00).
High-risk adenoma: In the diverticulitis group, 0 out of 68 patients were found to have high-risk adenoma (0%), while in the screening group, 4 out of 1309 patients were found to have high-risk adenoma (0.31%). There was no significant difference in the risk of high-risk adenomas between the two groups (0% vs 0.31%, P = 1.00).
Cancers: No cancers were found in the 68 patients in the diverticulitis group. In the screening group, 2 out of 1309 patients had cancers (0.15%). There was no significant difference between the two groups in terms of cancers found (0% vs 0.15%, P = 1.00).
Polyps: In the diverticulitis group, 11 out of 68 patients were found to have polyps (16.2%), while in the screening group, 186 out of 1309 patients were found to have polyps (14.2%). There was no significant difference in the total number of polyps between the two groups (16.2% vs 14.2%, P = 0.65).
Hyperplastic polyps: In the diverticulitis group, 6 out of 68 patients were found to have hyperplastic polyps (8.8%), while in the screening group, 60 out of 1309 patients were found to have hyperplastic polyps (4.6%). There was no significant difference between the two groups in terms of hyperplastic polyps found (8.8% vs 4.6%, P = 0.11).
Unbiopsied polyps: In the study group, 1 out of 68 patients had polyps which were not biopsied during the endoscopy (1.5%), while in the control group, 24 out of 1309 patients had small benign looking polyps that were not biopsied during endoscopy (1.8%). There was no significant difference between the two groups in terms of unbiopsied polyps (1.5% vs 1.8%, P = 0.83).
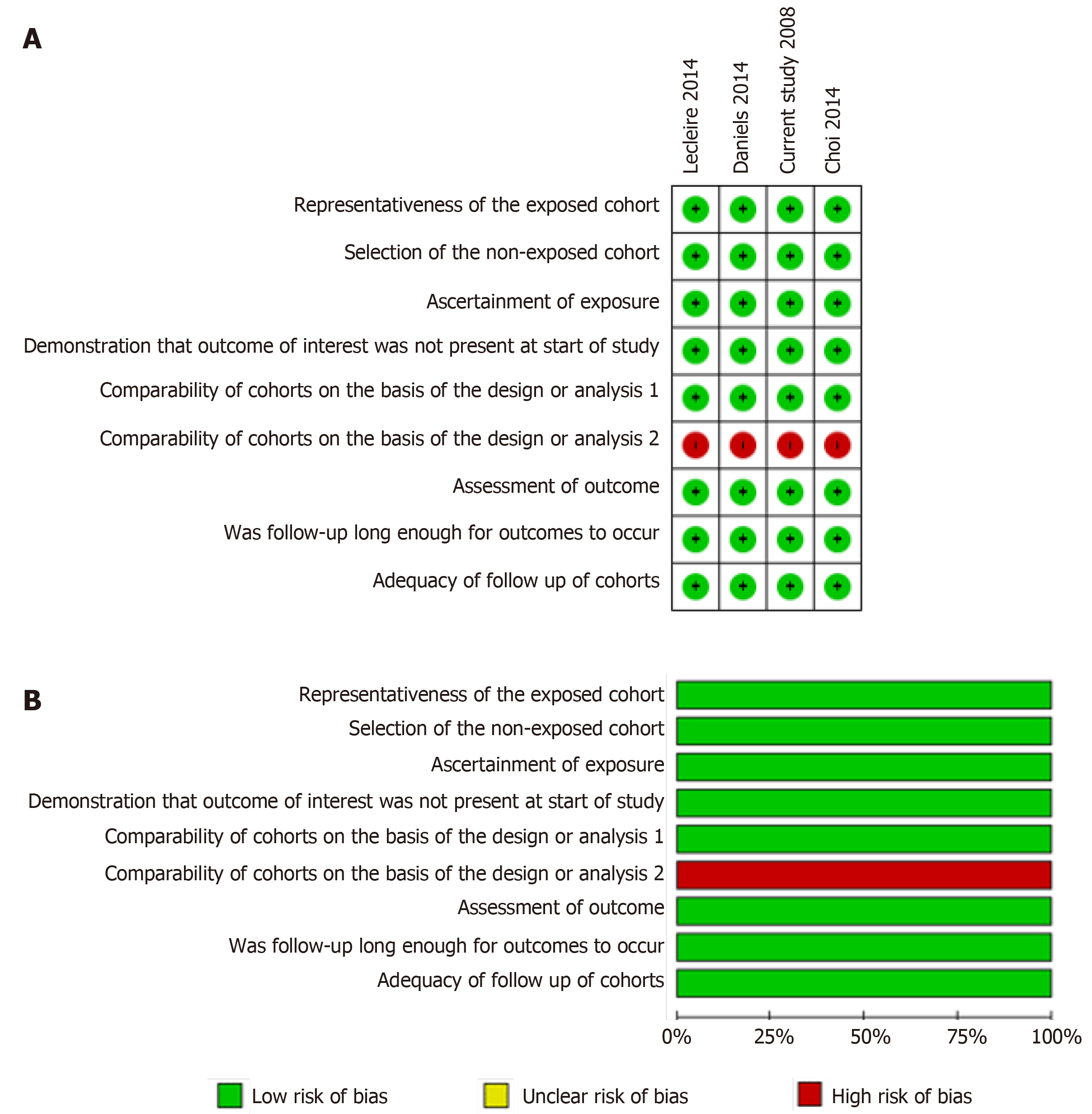
Searches of electronic databases identified 3 retrospective observational studies[16,17,24] enrolling a total of 3082 patients. We included the population of current study (1377 patients) in the meta-analysis increasing the total number of analysed patients to 4459 patients. Overall, 1022 patients were included in the diverticulitis group and 3437 patients were included in the screening group. The patients in the diverticulitis group were older than the screening group (Mean difference: 0.40, 95%CI: 0.11, 0.68, P = 0.006). There was no significant difference between the two groups in terms of gender (OR =C 0.94, 95%CI: 0.81, 1.09, P = 0.41). All patients in the diverticulitis group had CT-proven diverticulitis. In the diverticulitis group, all patients underwent colo-noscopy for endoscopic assessment of the colon, while in the screening group, 2128 patients underwent colonoscopy and 1309 patients underwent flexible sigmoi-doscopy. The baseline characteristics of the included studies and baseline characteristics of the included population are demonstrated in Table 2. The summary and results of methodological quality assessment of the 4 observational studies[16,17,24] are demonstrated graphically in Figure 1.
| Ref. | Year | Country | Journal | Design | Descrip-tion of diverticuli-tis group | Descrip-tion of control group | How diverticuli-tis is diagnosed | Time from diagnosis to endoscopy | Sample size | |
| Diverticuli-tis group | Screening group | |||||||||
| Current study | 2018 | United Kingdom | Not applicable | Retrospec-tive observation-al | Patients undergoing a colonoscopy after medical treatment of CT proven diverticulitis | Individuals from the general population undergoing flexible sigmoidos-copy for screening purposes at age of 55 | Computed tomography | up to 12 mo | 68 | 1309 |
| Daniels et al[16] | 2014 | The Netherlands | Surg Endosc | Retrospec-tive observation-al | Patients undergoing a colonoscopy after medical treatment of CT proven diverticulitis | Individuals from the general population between the age of 50-75 undergoing screening colonoscopy | Computed tomography | up to 6 mo | 401 | 1426 |
| Lecleire et al[17] | 2014 | France | United European Gastroenterol J | Retrospec-tive observation-al | Patients undergoing a colonoscopy after medical treatment of CT proven diverticulitis | Asymptomatic patients undergoing a screening colonoscopy | Computed tomography | up to 6 mo | 404 | 404 |
| Choi et al[24] | 2014 | South Korea | Dig Dis Sci | Retrospec-tive observation-al | Patients undergoing a colonoscopy after medical treatment of CT proven diverticulitis | Healthy individuals undergoing screening colonoscopy | Computed tomography | up to 12 mo | 149 | 298 |
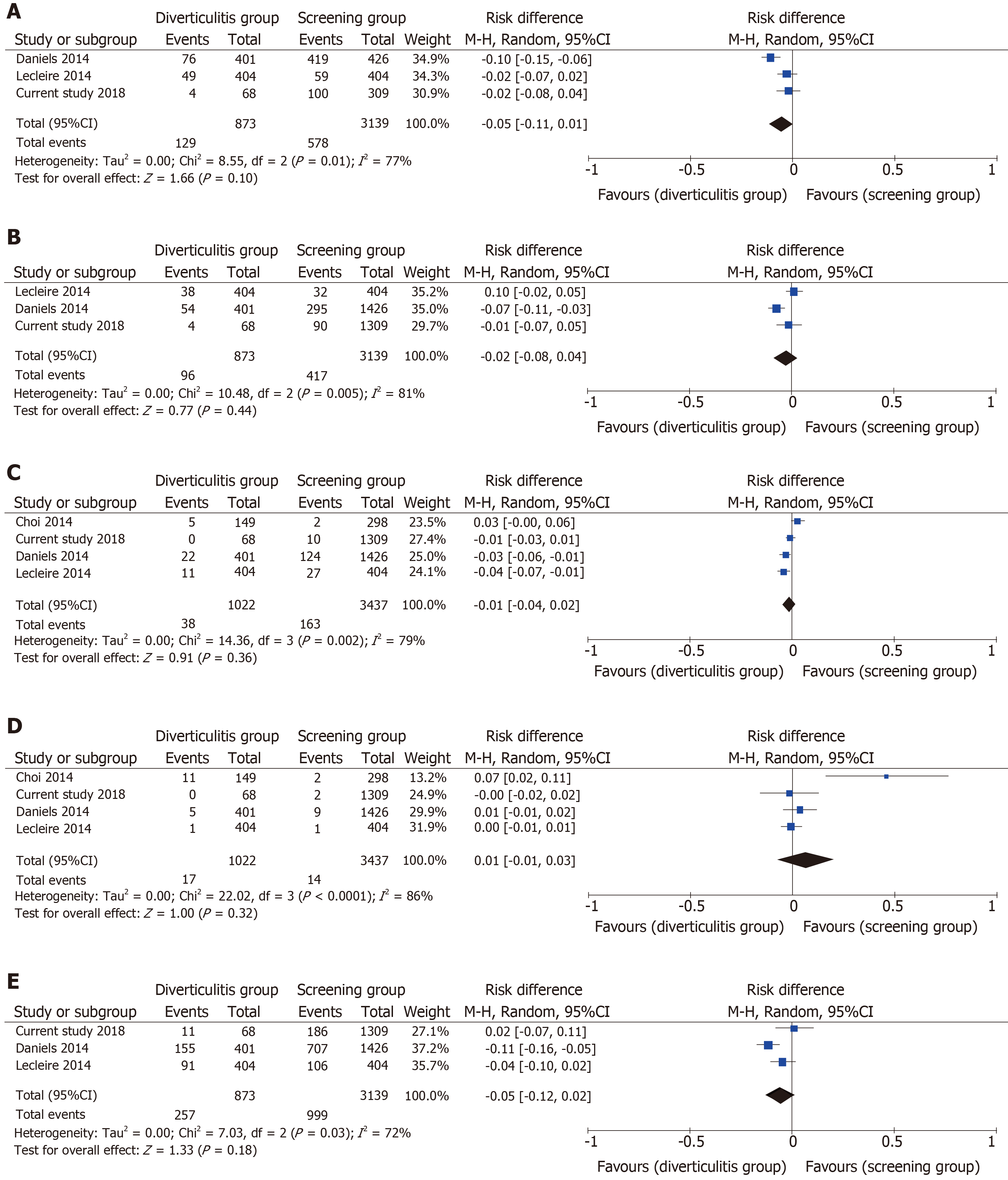
The results of analyses showed that there was no significant difference in the risk of adenomas (RD = -0.05, 95%CI: -0.11, 0.01, P = 0.10), non-advanced adenomas (RD = -0.02, 95%CI: -0.08, 0.04, P = 0.44), advanced adenomas (RD = -0.01, 95%CI: -0.04, 0.02, P = 0.36), cancer (RD = 0.01, 95%CI: -0.01, 0.03, P = 0.32), and polyps (RD = -0.05, 95%CI: -0.12, 0.02, P = 0.18) between the diverticulitis and screening groups (Figure 2). The between study heterogeneity was high for adenomas (I2 = 77%, P = 0.01), high for non-advanced adenomas (I2 = 81%, P = 0.005), high for advanced adenomas I2 = 79%, P = 0.002), high for cancer (I2 = 86%, P < 0.0001), and moderate for polyps (I2 = 72%, P = 0.03) (Figure 2).
We conducted a multicentre retrospective cohort study to assess the risk of colonic adenomas and neoplastic lesions in patients with CT-proven diverticulitis compared to those in general population undergoing endoscopic evaluation for bowel cancer screening. The results of the current study showed that there was no difference in the risk of adenomas, non-advanced adenomas, advanced adenomas, cancer, and polyps between the diverticulitis and screening groups. We also performed a systematic review and meta-analysis of the literature to provide the best available evidence. We identified 4 retrospective observational studies[16,17,24] (including the current study) enrolling a total of 4459 patients. The results of analyses also showed that there is no difference in the risk of adenomas, non-advanced adenomas, advanced adenomas, cancer, and polyps between the diverticulitis and screening groups. The quality of the best available evidence was moderate.
The current ACPGBI and ASCRS guidelines both suggest that patients should undergo endoscopic evaluation of the colonic lumen after an episode of CT proven acute diverticulitis to rule out malignancy[3,4]. However, after reviewing all 1377 patients from our study, and 4459 patients in our meta-analysis, we did not find any evidence that diverticulitis patients had any more adenomas, advanced adenomas, or cancers than the general population. There was therefore seemingly no benefit from this endoscopic evaluation. It therefore follows, that routine endoscopic assessment of patients after an episode of CT proven acute diverticulitis, may be unnecessary.
Colonoscopy has several procedure-related risks such as bleeding or perforation[8]. Reducing the number of colonoscopies would reduce the number of colonoscopy-related complications, and therefore reduce the associated morbidity and mortality. Moreover, colonoscopies on patients with diverticular disease appear to have a higher failure rate, and tend to cause the patient a great deal of discomfort[6]. Furthermore, due to the high number of patients who suffer from diverticulitis, the cost-burden of performing colonoscopies on them post acute episode is significant[9]. Reducing unnecessary colonoscopies on patients with diverticular disease will therefore avoid these issues and reduce excess costs.
It is therefore of the authors’ opinion, that patients should be considered for endoscopy on a case-by-case basis. Only patients who have uncertainty in the diagnosis, or those who have complicated diverticulitis should be offered endoscopic evaluation.
The reported outcomes of the current study should be viewed and interpreted in the context of inherent limitations. In terms of the cohort study, our study had a retrospective design which subject our results to inevitable selection bias. The included patients in the diverticulitis group were older than the patients in the screening group; Moreover, the number of patients in the diverticulitis group was conspicuously smaller than the number of patients in the screening group. All of these, together with the fact that patients in the screening group underwent flexible sigmoidoscopy instead of colonoscopy, might have led to underestimation of the risk of adenomas and neoplastic lesions in the screening group. In terms of the meta-analysis, the best available evidence is derived from a limited number retrospective of studies which are subject to selection bias. The between study heterogeneity was high for almost all outcomes and the quality of the available evidence was moderate. All of these might have affected the robustness of our results.
Our results suggest that patients with CT-proven acute diverticulitis are not at increased risk of colonic adenomas and neoplastic lesions as indicated by comparable endoscopic findings to general populations undergoing screening endoscopy. This suggests that endoscopic evaluation of colon may not be beneficial in cases with CT-proven acute diverticulitis and could be preserved for selected cases only. Our results are consistent with the best available evidence in the literature. However, the best available evidence is derived from a limited number of retrospective studies with moderate quality. High quality prospective studies are required for definite conclusions.
The current guidelines suggest that patients should undergo endoscopic evaluation of the colonic lumen after an episode of computed tomography (CT) proven acute diverticulitis to rule out malignancy. However, with the advancement and evolution of CT scan technology, the necessity for routine colonoscopy post episode of acute diverticulitis has become questionable.
Colonoscopy is invasive and is associated with discomfort, particularly in patients with diverticular disease. Patients with diverticular disease also have more difficult endoscopic procedures, and have a higher risk of perforation. Cost-effectiveness of investigating all patients also remains unclear. For this reason, this project has set out to establish whether routine colonoscopy should be offered to patients after an episode of acute diverticulitis.
The main objective of this research was to establish whether there was any added benefit to offering patients routine colonoscopy after every episode of acute diverticulitis. The significance of demonstrating that colonoscopy may in fact not be required routinely would be two-fold. It would allow for a reduction in number of colonoscopy related complications including discomfort, bleeding and perforation, as well as a significant reduction in overall costs, and financial burden.
We conducted a retrospective cohort study in three centres in the north west of England. The study group included consecutive patients who were admitted to our trust with an episode of acute diverticulitis over a three-year period between January 2014 and December 2016. The control group included all patients who had undergone a one-off screening flexible sigmoidoscopy at the age of fifty-five, as part of the National Bowel Cancer Screening Programme over a fourteen-month period between October 2015 and December 2016. Three independent authors collected the data using a data collection proforma. We considered the total number of adenomas, non-advanced adenomas, and advanced adenomas as primary outcome measures. The secondary outcomes included low-risk adenomas, intermediate-risk adenomas, high-risk adenomas, invasive cancers, total number of polyps, and hyperplastic polyps. We also performed a systematic review according to an agreed predefined protocol and we were compliant with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement standards. We calculated the risk difference (RD) as the summary measure. Heterogeneity among the studies was assessed using the Cochrane Q test (χ2). Random or fixed effects modelling were used as appropriate for analysis; random effects models were used if considerable heterogeneity was found among the studies. The results were reported in a forest plot with 95% confidence intervals (CIs). We used the Review Manager 5.3 software for data synthesis.
Overall, 68 and 1309 patients were included in the diverticulitis and control groups respectively. There was no difference in the risk of adenomas (5.9% vs 7.6%, P = 0.59), non-advanced adenomas (5.9% vs 6.9%, P = 0.75), advanced adenomas (0% vs 0.8%, P = 1), cancer (0% vs 0.15%, P = 1.00), and polyps (16.2% vs 14.2%, P = 0.65) between both groups. Meta-analysis of data from 4 retrospective observational studies, enrolling 4459 patients, showed no difference between the groups in terms of risk of adenomas (RD = -0.05, 95%CI: -0.11, 0.01, P = 0.10), non-advanced adenomas (RD = -0.02, 95%CI: -0.08, 0.04, P = 0.44), advanced adenomas (RD = -0.01, 95%CI: -0.04, 0.02, P = 0.36), cancer (RD = 0.01, 95%CI: -0.01, 0.03, P = 0.32), and polyps (RD = -0.05, 95%CI: -0.12, 0.02, P = 0.18). The results of the current study as well as the meta-analyses showed that there is no difference in the risk of adenomas, non-advanced adenomas, advanced adenomas, cancer, and polyps between the diverticulitis and screening groups. The quality of the best available evidence was moderate. It is therefore of the authors’ opinion, that patients should be considered for endoscopy on a case-by-case basis. Only patients who have uncertainty in the diagnosis, or those who have complicated diverticulitis should be offered endoscopic evaluation. The reported outcomes of the current study should be viewed and interpreted in the context of inherent limitations. In terms of the cohort study, our study had a retrospective design which subject our results to inevitable selection bias. The included patients in the diverticulitis group were older than the patients in the screening group; Moreover, the number of patients in the diverticulitis group was conspicuously smaller than the number of patients in the screening group. All of these, together with the fact that patients in the screening group underwent flexible sigmoidoscopy instead of colonoscopy, might have led to underestimation of the risk of adenomas and neoplastic lesions in the screening group. In terms of the meta-analysis, the best available evidence is derived from a limited number retrospective of studies which are subject to selection bias. The between study heterogeneity was high for almost all outcomes and the quality of the available evidence was moderate. All of these might have affected the robustness of our results.
The results of this study have shown no difference between diverticulitis and control groups in terms of its primary and secondary outcomes. It has therefore demonstrated that it may not be necessary to offer all patients with acute diverticulitis a subsequent colonoscopy. The implications of this in practice, would be a reduction in the number of unnecessary colonoscopies, and therefore a subsequent reduction in associated morbidity and cost.
The best available evidence currently is derived from a limited number of retrospective studies with moderate quality. High quality prospective studies are required for definite conclusions.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang W S-Editor: Ma YJ L-Editor: A E-Editor: Wu YXJ
| 1. | RCS. Commissioning Guide: Colonic Diverticular Disease. 2014. Available from: URL: https://www.acpgbi.org.uk/content/uploads/2017/02/Commissioning-guide-colonic-diverticular-disease-RCS-2014.pdf. Accessed April 26, 2017. |
| 2. | Stollman N, Raskin JB. Diverticular disease of the colon. Lancet. 2004;363:631-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 412] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 3. | Fozard JB, Armitage NC, Schofield JB, Jones OM; Association of Coloproctology of Great Britain and Ireland. ACPGBI position statement on elective resection for diverticulitis. Colorectal Dis. 2011;13 Suppl 3:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, Rafferty JF. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 385] [Article Influence: 35.0] [Reference Citation Analysis (1)] |
| 5. | Sartelli M, Catena F, Ansaloni L, Coccolini F, Griffiths EA, Abu-Zidan FM, Di Saverio S, Ulrych J, Kluger Y, Ben-Ishay O, Moore FA, Ivatury RR, Coimbra R, Peitzman AB, Leppaniemi A, Fraga GP, Maier RV, Chiara O, Kashuk J, Sakakushev B, Weber DG, Latifi R, Biffl W, Bala M, Karamarkovic A, Inaba K, Ordonez CA, Hecker A, Augustin G, Demetrashvili Z, Melo RB, Marwah S, Zachariah SK, Shelat VG, McFarlane M, Rems M, Gomes CA, Faro MP, Júnior GA, Negoi I, Cui Y, Sato N, Vereczkei A, Bellanova G, Birindelli A, Di Carlo I, Kok KY, Gachabayov M, Gkiokas G, Bouliaris K, Çolak E, Isik A, Rios-Cruz D, Soto R, Moore EE. WSES Guidelines for the management of acute left sided colonic diverticulitis in the emergency setting. World J Emerg Surg. 2016;11:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 134] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 6. | Daniels L, Unlü C, de Wijkerslooth TR, Dekker E, Boermeester MA. Routine colonoscopy after left-sided acute uncomplicated diverticulitis: a systematic review. Gastrointest Endosc. 2014;79:378-89; quiz 498-498.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Brar MS, Roxin G, Yaffe PB, Stanger J, MacLean AR, Buie WD. Colonoscopy following nonoperative management of uncomplicated diverticulitis may not be warranted. Dis Colon Rectum. 2013;56:1259-1264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Panteris V, Haringsma J, Kuipers EJ. Colonoscopy perforation rate, mechanisms and outcome: from diagnostic to therapeutic colonoscopy. Endoscopy. 2009;41:941-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 181] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 9. | Disbrow M, Foxx-Orenstein A, Agrwal N. Utility of Colonoscopy to Exclude Underlying Malignant Polyps After Resolution of Uncomplicated Diverticulitis. J Am Osteopath Assoc. 2015;115:720-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Suhardja TS, Norhadi S, Seah EZ, Rodgers-Wilson S. Is early colonoscopy after CT-diagnosed diverticulitis still necessary? Int J Colorectal Dis. 2017;32:485-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Andrade P, Ribeiro A, Ramalho R, Lopes S, Macedo G. Routine Colonoscopy after Acute Uncomplicated Diverticulitis - Challenging a Putative Indication. Dig Surg. 2017;34:197-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (1)] |
| 12. | Walker AS, Bingham JR, Janssen KM, Johnson EK, Maykel JA, Ocampo O, Gonzalez JP, Steele SR. Colonoscopy after Hinchey I and II left-sided diverticulitis: utility or futility? Am J Surg. 2016;212:837-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Horesh N, Saeed Y, Horesh H, Berger Y, Speter C, Pery R, Rosin D, Gutman M, Zmora O. Colonoscopy after the first episode of acute diverticulitis: challenging management paradigms. Tech Coloproctol. 2016;20:383-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Hashimoto R, Matsuda T, Chonan A. Colonoscopy After Computed Tomography-diagnosed Acute Right-sided Diverticulitis May Be Unnecessary. J Clin Gastroenterol. 2016;50:611-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Ou G, Rosenfeld G, Brown J, Chan N, Hong T, Lim H, Bressler B. Colonoscopy after CT-diagnosed acute diverticulitis: Is it really necessary? Can J Surg. 2015;58:226-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Daniels L, Ünlü Ç, de Wijkerslooth TR, Stockmann HB, Kuipers EJ, Boermeester MA, Dekker E. Yield of colonoscopy after recent CT-proven uncomplicated acute diverticulitis: a comparative cohort study. Surg Endosc. 2015;29:2605-2613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Lecleire S, Nahon S, Alatawi A, Antonietti M, Chaput U, Di-Fiore A, Alhameedi R, Marteau P, Ducrotté P, Dray X. Diagnostic impact of routine colonoscopy following acute diverticulitis: A multicenter study in 808 patients and controls. United European Gastroenterol J. 2014;2:301-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | de Vries HS, Boerma D, Timmer R, van Ramshorst B, Dieleman LA, van Westreenen HL. Routine colonoscopy is not required in uncomplicated diverticulitis: a systematic review. Surg Endosc. 2014;28:2039-2047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Sallinen V, Mentula P, Leppäniemi A. Risk of colon cancer after computed tomography-diagnosed acute diverticulitis: is routine colonoscopy necessary? Surg Endosc. 2014;28:961-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Schmilovitz-Weiss H, Yalunin E, Boaz M, Sehayek-Shabbat V, Levin I, Chervinski A, Atar E, Niv Y, Shirin H. Does a colonoscopy after acute diverticulitis affect its management?: a single center experience. J Clin Gastroenterol. 2012;46:317-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Westwood DA, Eglinton TW, Frizelle FA. Routine colonoscopy following acute uncomplicated diverticulitis. Br J Surg. 2011;98:1630-1634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 22. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13215] [Article Influence: 825.9] [Reference Citation Analysis (0)] |
| 23. | Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: http://www.ohri.ca/programs/clinical_epidemiology/nos_manual.pdf. Accessed April 29, 2017. |
| 24. | Choi YH, Koh SJ, Kim JW, Kim BG, Lee KL, Im JP, Kim JS, Jung HC. Do we need colonoscopy following acute diverticulitis detected on computed tomography to exclude colorectal malignancy? Dig Dis Sci. 2014;59:2236-2242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |