Published online Mar 16, 2019. doi: 10.4253/wjge.v11.i3.174
Peer-review started: February 11, 2019
First decision: February 26, 2019
Revised: March 8, 2019
Accepted: March 11, 2019
Article in press: March 11, 2019
Published online: March 16, 2019
Processing time: 43 Days and 2.7 Hours
Foreign body ingestion encompasses both foreign object ingestion (FOI) and esophageal food impaction (EFI) and represents a common and clinically significant scenario among patients of all ages. The immediate risk to the patient ranges from negligible to life-threatening, depending on the ingested substance, its location, patient fitness, and time to appropriate therapy. This article reviews the FOI and EFI literature and highlights important considerations and implications for pediatric and adult patients as well as their providers. Where published literature is insufficient to provide evidence-based guidance, expert opinion is included to supplement the content of this comprehensive review.
Core tip: Foreign body ingestion encompasses both foreign object ingestion (FOI) and esophageal food impaction (EFI) and represents a common and clinically significant scenario among patients of all ages. This article reviews the FOI and EFI literature and highlights important considerations and implications for pediatric and adult patients as well as their providers.
- Citation: Fung BM, Sweetser S, Wong Kee Song LM, Tabibian JH. Foreign object ingestion and esophageal food impaction: An update and review on endoscopic management. World J Gastrointest Endosc 2019; 11(3): 174-192
- URL: https://www.wjgnet.com/1948-5190/full/v11/i3/174.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i3.174
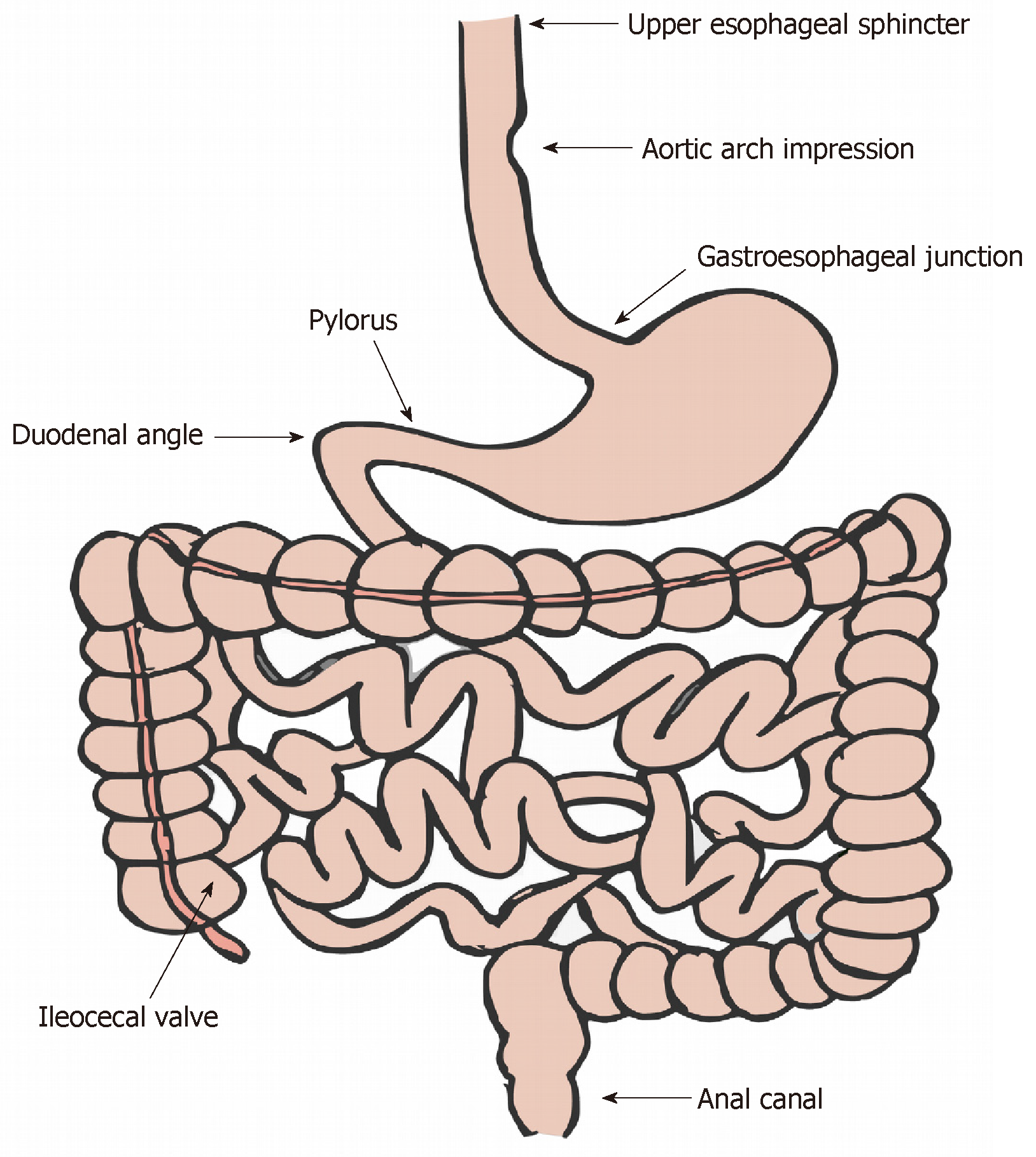
Foreign body ingestion is a common and potentially life-threatening clinical problem with an estimated annual incidence of 120000 cases in the United States alone[1]. The majority of these cases occur in children as a result of curiosity and accidental ingestion, with peak incidence occurring between the ages of 6 mo and 3 years[2]. In adults, groups at higher risk include those with severe psychiatric disorders, mental retardation, acute intoxication, or seeking secondary gain (e.g., incarcerated individuals seeking transfer out of prison to a medical facility)[3-5]. Although the majority of ingested foreign bodies will traverse the gastrointestinal (GI) tract uneventfully, 10-20% will require intervention, most often endoscopic, to mitigate complications such as impaction, ulceration, perforation, and potentially death[6-9]. These complications preferentially occur at areas of physiologic or pathologic sharp angulation or narrowing (Figure 1) and appear to be more common and associated with relatively higher morbidity in intentional as compared to accidental ingestion[3,10-12].
Foreign body ingestion can be classified into two main groups: true foreign object ingestion (FOI) and esophageal food impaction (EFI). These groups encompass a wide variety of potentially ingested substrates, making every case a new potential challenge for even highly experienced gastroenterologists. Furthermore, there is considerable geographic variation in the epidemiology of FOI, both in terms of the ingested substrate as well as the patient demographic. For example, in the United States, food (meat) impaction is the most common FOI in adults[13,14], and eosinophilic esophagitis has become recognized as an increasingly common underlying diagnosis (Table 1)[14-16]. In contrast, bones (primarily fish) represent the most common foreign body ingestions in Spain[17], Iran[18], Nigeria[19], Ethiopia[20], India[21], and China[22,23]. These patterns are different, however, among pediatric patients (where FOI, e.g., coin ingestion, is more common)[2,24-27] and elderly patients (where dental prosthesis ingestion is more common) both in the United States as well as globally[22]. Given the heterogeneity in types of foreign bodies (Table 2) and in demographic characteristics, clinical presentation can vary between cases, as can the array and likelihood of complications. Accordingly, management requires careful diagnosis, recognition of the potential risks, and planning for appropriate intervention.
| Eosinophilic esophagitis |
| Schatzki’s ring |
| Peptic stricture |
| Radiation-induced stricture |
| Esophageal carcinoma |
| Zenker’s diverticulum |
| Non-Zenker’s esophageal diverticulum |
| Post-surgical (e.g., fundoplication) |
| Achalasia |
| Other spastic dysmotility |
| Size |
| Length (≤ 5 vs > 5 cm) Width (≤ 2 vs > 2 cm) |
| Surface consistency |
| Sharp/pointed vs blunt |
| Smooth vs rough/traumatic |
| Material |
| Food (boneless vs with bone) |
| Battery |
| Magnet |
| Packaged drugs |
| Chemical/physical characteristics |
| Radiodensity |
| Metallic vs non-metallic |
| Chemical reactivity/inertness |
As GI endoscopy has become the method of choice for the management of most FOIs and EFIs, it is critically important for gastroenterologists to understand the role and timing of endoscopic intervention as well as the tools for proper therapy in order to avoid complications and mitigate potential morbidity. Therefore, this review will summarize available evidence that should be considered when managing FOI and EFI and provide diagnostic and therapeutic algorithms for clinicians involved in the care of these patients. Where evidence is limited, we suggest pragmatic approaches based on current data, clinical experience, and expert opinion.
History and physical examination: In most adults and older children, FOI and EFI are often recognized at the time of the incident, and the history, including the material swallowed and location of discomfort, can be obtained from the patient. In younger children and the psychiatrically (or otherwise mentally) impaired, diagnosis often becomes more challenging, especially when an episode is unwitnessed. Importantly, the site of discomfort or other symptomatology (if present) often does not reliably predict the location of pathology, especially when occurring below the cricopharyngeus[28]; for example, distal esophageal impaction related to an underlying peptic stricture may be referred to the throat region.
The presentation of FOI depends greatly on the nature of the ingested material, anatomical factors (e.g., prior surgery), and the time that has elapsed from initial ingestion. Presenting symptoms may include choking, refusing to eat, vomiting, abdominal pain, respiratory distress (particularly in pediatric patients with proximal esophageal FOI or EFI), or blood-tinged saliva, among others[29-32]. Thus, a careful history (e.g., regarding the ingested material, prior history of dysphagia/similar episodes, the use of removable dental hardware, and prior GI surgeries) obtained from the patient and/or witnesses is essential and may provide critical diagnostic clues.
With regard to EFI, the classic presentation consists of acute onset substernal chest pain/discomfort and difficulty swallowing while eating boneless (typically roasted or pulled) pork, beef, or poultry due to a sensation that food is “getting stuck”. In some cases, the presentation may be more insidious, and often times patients frequently will not present until several hours after symptom onset, hoping that symptoms will resolve spontaneously with time. In addition to chest pain and dysphagia, other commonly reported symptoms include foreign body sensation, odynophagia, sialorrhea, and a need to spit up secretions. When obtaining a history, it is important to inquire about the content of recent meals and assess whether the ingesta was boneless or if it may have contained bones, as this could change the management approach and the spectrum of potential sequelae.
The physical examination in patients with suspected FOI or EFI should involve evaluating for evidence of luminal obstruction and other complications, especially perforation (which may manifest, for example, with cervical swelling and/or crepitus in the case of oropharyngeal/proximal esophageal perforation, or with fever and peritonitis in the case of intestinal perforation).
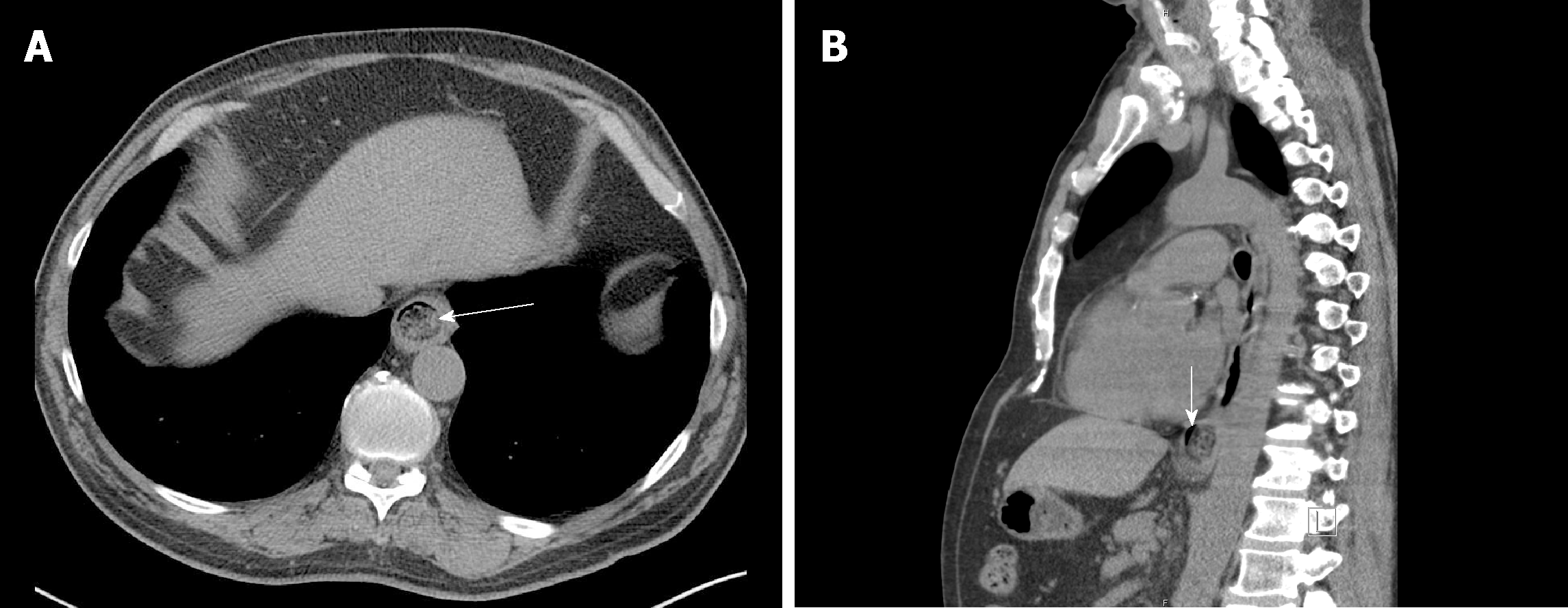
Imaging and localization: Assessment of the anatomic location is of central importance in the clinical management of FOI and EFI. Imaging studies can provide valuable information on the location as well as the morphology and nature (e.g., size and sharpness, composition, and number of objects) of the foreign body. Fortunately, most FOIs are composed of radiopaque material and can be identified on projectional X-rays (e.g., posterior-anterior and lateral images) of the neck, chest, or abdomen. However, objects such as thin bones, plastic, glass, and wood may not be readily seen. X-rays can also provide useful information regarding possible aspiration and free mediastinal or peritoneal air[33]. Contrast administration should generally be avoided given the risk and potential complications of contrast aspiration[6]; moreover, contrast coating of the foreign body and esophageal mucosa can compromise subsequent endoscopy[29,34]. Computed tomography (CT) scanning may be useful (Figure 2)[35-38], particularly if complications are suspected[9], and its sensitivity and accuracy can be improved with three-dimensional reconstruction[39]. Handheld metal detectors can be useful in metallic FOI, particularly in pediatric patients, as well as in the detection of certain radiolucent metallic foreign bodies like aluminum[40-44]. Additional details regarding initial noninvasive diagnostic as well as elimination follow-up imaging have been discussed in recent radiology society clinical guidelines[45].
In the setting of a negative radiographic evaluation but suspected foreign body ingestion and persistent esophageal symptoms, endoscopic intervention is warranted[29,46]. In addition, patients with suspected non-bony EFI without complications (e.g., no evidence of perforation or respiratory distress) can proceed to endoscopic evaluation without obtaining radiographs[6,9].
Airway management: Initial management of patients with FOI and EFI includes assessment of ventilatory status and airway protection. Most adult cases of FOI and EFI may be managed with moderate sedation. In the presence of wheezing, stridor, or dyspnea, however, emergent endotracheal intubation may be indicated. Similarly, endotracheal intubation is appropriate for facilitating airway protection in patients who are unable to manage their secretions (e.g., due to very proximal EFI) and are thus at high aspiration risk[9]. Endotracheal intubation may likewise be indicated for patients with FOI or EFI that is difficult to remove and in cases with multiple objects requiring removal. An overtube may be used to provide additional airway protection, and these are discussed in a forthcoming section[9]. Notably, pediatric GI endoscopy often requires general endotracheal anesthesia, in part due to the fact that smaller and more compliant airways have a higher risk of airway obstruction during endoscopy[46].
Timing and urgency of intervention: Once FOI or EFI is diagnosed, the provider must decide whether intervention is necessary, and if so, how urgently intervention is required. The need for and timing of an intervention for FOI and EFI are dependent on multiple factors; these include patient age and clinical condition, the location and characteristics of the ingested material (Table 2), time since ingestion, and the technical capabilities of the endoscopist and facility[47]. Based on these factors and the perceived risks of aspiration, obstruction, perforation, and other potential complications, as well as the likelihood of procedural success, the timing and nature of endoscopic intervention is determined. As stated previously, patients unable to effectively manage their secretions (e.g., due to complete esophageal obstruction from EFI) or with sharp or disk battery FOI require emergent endoscopic intervention (preferably within 2 h, and at the latest within 6 h)[9]. Other scenarios (e.g., asymptomatic blunt foreign object in the esophagus or incompletely obstructing EFI) need not be managed emergently but should undergo endoscopic intervention within 24 h as delay beyond this time interval decreases the likelihood of successful removal and increases the risk of complications, including but not limited to perforation[48-50]. In cases of FOI where the object has made it past the esophagus, most patients who are clinically stable, in no acute distress, and without signs of GI obstruction will not require urgent endoscopy as the ingested object will often pass spontaneously[3,6,51]. For such patients, conservative outpatient management is reasonable[9,52,53], although endoscopic removal may also be appropriate depending on the circumstance (e.g., disk and cylindrical batteries in the stomach that have not progressed in 48 h), especially given the high success rate and low risk of adverse events in the majority of cases[6,22,54,55]. If endoscopy is foregone, patients may resume a regular diet but should monitor their stool for passage of the ingested object. In the absence of symptoms, weekly imaging (e.g., X-rays, depending on the type of FOI) should be obtained to follow the progression of small blunt objects that have not yet passed in order to ensure their passage. Specific clinical circumstances are discussed in forthcoming sections.
When to avoid endoscopic intervention: As mentioned above, endoscopy can be foregone in cases where patients are asymptomatic and spontaneous passage is believed to be likely. Special note should be made of the importance of avoiding endoscopic intervention in cases of internal concealment of illicit drugs (i.e., “body packers” or “drug mules”). Here, multiple packets of contraband are typically swallowed and pose a risk for obstruction or rupture. Endoscopic removal should generally not be attempted because of the high risk of rupturing a packet, which can lead to fatal drug overdose. Therefore, these patients should be managed conservatively with close monitoring, serial imaging, and assessments for potential toxicity; surgical intervention may be indicated should removal become necessary[8].
Endoscopes: Most FOIs and EFIs are best treated with flexible endoscopes[6,56]. This approach has a high success rate, is generally safer than rigid endoscopy[57], and can be performed with moderate sedation in a majority of cases. However, in some instances, rigid esophagoscopy may be preferable, e.g., for proximal FOIs and EFIs impacted at the level of the upper esophageal sphincter or hypopharynx (i.e., above the cricoid cartilage)[17,54,57-59]. Standard or therapeutic endoscopes are preferable, but small-caliber endoscopes may be used (e.g., if a transnasal approach is deemed necessary or if the patient is unfit for sedation)[60]. However, based on randomized controlled trial (RCT) data, cases of small-caliber endoscope failures can frequently be successfully treated with a standard endoscope, whereas the converse does not appear to be true[61]. Recently, single- and double-balloon enteroscopes are being used in the management of FOIs which are beyond the reach of conventional endoscopes; this is discussed further below[62-65].
Retrieval devices and accessories: A variety of devices and accessories have been described in the published literature for management of FOI and EFI, including but not limited to rat-tooth and alligator forceps, polypectomy snares, multi-prong graspers, Dormia baskets, Roth retrieval nets, Foley catheters, and variceal ligator caps[66-68]. More recently, the use of balloon dilators[69] and sutures[70] has also been described, as has the use of other accessories[71]. The choice of retrieval device depends largely on the type of FOI or EFI and endoscopist experience and preference[72-74]. Foley catheter techniques have also been described and may be more cost-effective in certain pediatric care scenarios (e.g., coin ingestion)[75,76] but are not often used in the adult population. A recent RCT showed that use of a soft, clear cap at the end of the endoscope may provide an advantage by improving visibility and shortening the procedure time[77]. Regardless of the technique and devices/accessories used, ex-vivo practice using the planned retrieval equipment and an object similar to the ingested foreign object can help determine the suitability of the proposed therapeutic approach.
Overtubes: Use of an overtube during the management of FOI and EFI: (1) provides airway protection during retrieval and (2) allows for multiple passes of the endoscope during retrieval, and iii) shields the esophageal mucosa from injury when removing sharp or pointed objects[78,79]. When the object is distal to the esophagus, a longer overtube that extends across the esophagogastric junction can provide additional protection and is often recommended[9]. Overtubes are less commonly used in pediatric patients, as there may be increased risk of esophageal injury and retching associated with overtube insertion. However, newer, softer overtubes may be considered in larger children and adolescents[80].
An alternative to an overtube in cases of sharp or pointed object retrieval is the use of a latex protector hood, which is placed over and affixed to the tip of the endoscope. The bell portion of the protector hood remains inverted during insertion of the endoscope and then flips back to its original shape during withdrawal as it crosses a region of narrowing (e.g., the lower esophageal sphincter)[8,81,82].
Pharmacologic agents: Glucagon has long been employed in the management of EFI and is in fact one of the only interventions to have been studied in the setting of an RCT[83]. The proposed mechanism of action of glucagon in facilitating resolution of EFI involves its spasmolytic activity. Although the aforementioned RCT failed to show therapeutic effects, the study had several notable limitations. For example, it did not specifically investigate whether glucagon could facilitate endoscopic therapy (by facilitating engagement of the impacted bolus via decreasing esophageal spasms), but rather assessed whether it would increase the rate of spontaneous passage. Based on one prospective (non-randomized) study[84], anecdotal experience, and various retrospective series[71,85,86], treatment with glucagon is generally reasonable in the management of patients with EFI[6,29], realizing though that it will be effective in only some patients[9,87]. With respect to dose, esophageal tone appears to reach a nadir at 0.5 mg (based on the results of the only published study of its kind)[88]; however, these data were obtained in normal healthy controls and based on pressure measurements at the lower esophageal sphincter and therefore cannot necessarily be extrapolated to individuals with EFI in a more proximal portion of the esophagus. As a result, and based on its safety and potential usefulness as demonstrated in a prospective (nonrandomized) trial[89], most practitioners advocate for the administration of glucagon 1.0 mg intravenously in cases of EFI prior to endoscopic intervention[6]. If there is no apparent improvement in symptoms and no adverse effects, a repeat dose (within 15-30 min) in an attempt to further relax the esophagus is reasonable, particularly for non-meat EFI, although high quality evidence to support this practice is currently lacking[86].
Effervescent agents such as cola or other carbonated drinks have long been used alone or in combination with other pharmacologic agents (e.g., glucagon)[90-93]. The evidence supporting their use includes a single prospective study[84] and several case series and reports; the collective results suggest that effervescent agents may help to achieve spontaneous resolution of EFI and are associated with little risk in patients capable of protecting their airway. Therefore, the administration of an effervescent is reasonable in select patients (e.g., who do not appear to have severe impaction), but as with other pharmacologic therapies, should not delay endoscopic intervention[93].
The use of various other agents has been described in the management of EFI but is not routinely recommended for this indication[6,94]. Hyoscine butylbromide (i.e., butylscopolamine), a peripherally acting antimuscarinic, anticholinergic agent, is believed to exert potentially therapeutic effects through its spasmolytic activity (similar to glucagon); its use is supported by very limited published data, none of which are prospective[95-97]. Benzodiazepines have also been employed in patients with EFI[83,98,99]. However, the evidence for their use is sparse, and the literature suggests that they are no more effective than placebo[83]; moreover, there is concern that benzodiazepines may impair a patients alertness and thus airway protection. Lastly, use of proteolytic enzymes (e.g., papain) has been described, but this should be avoided due to numerous associated risks, including esophageal erosion and perforation[8,29,100].
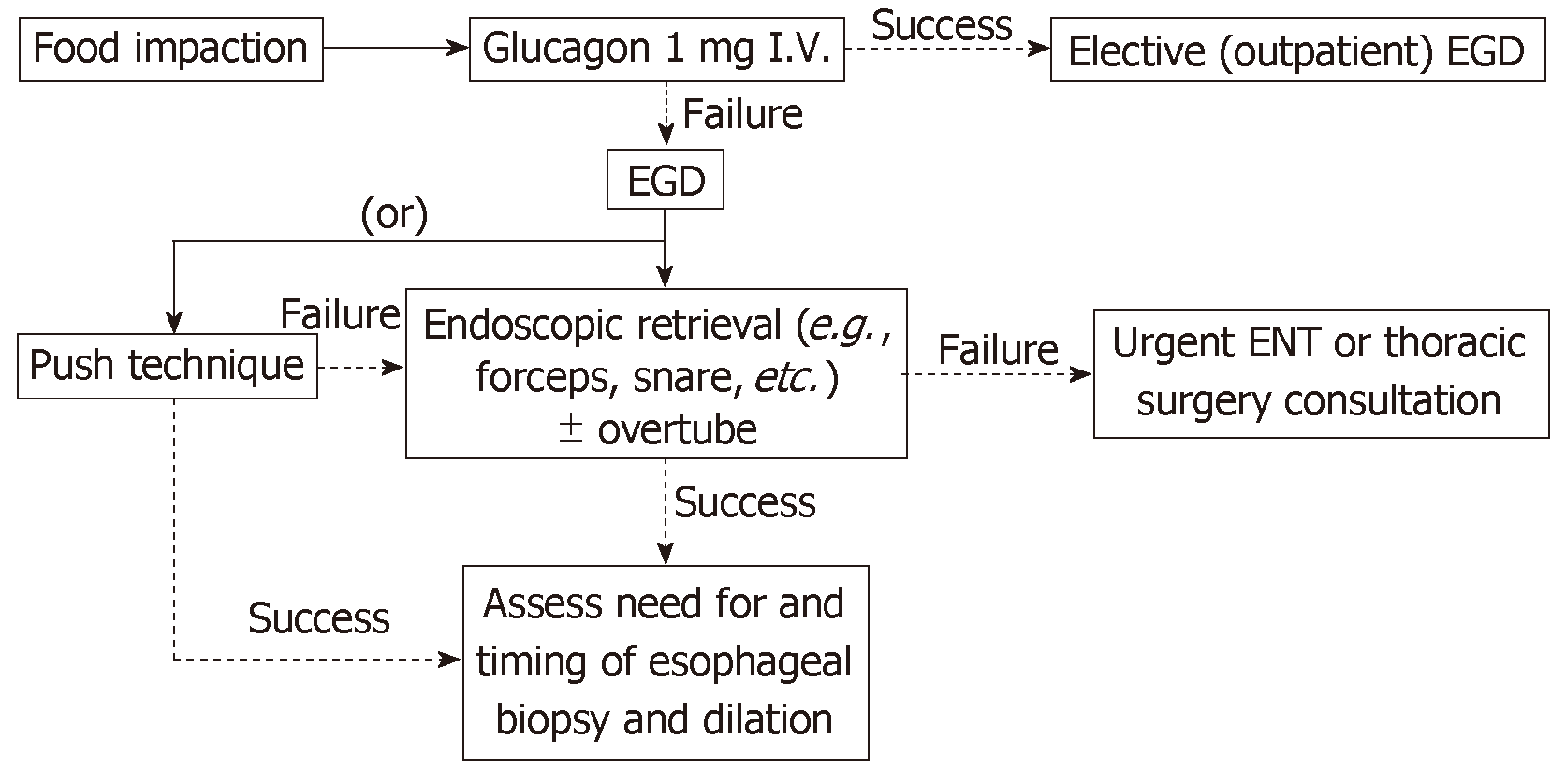
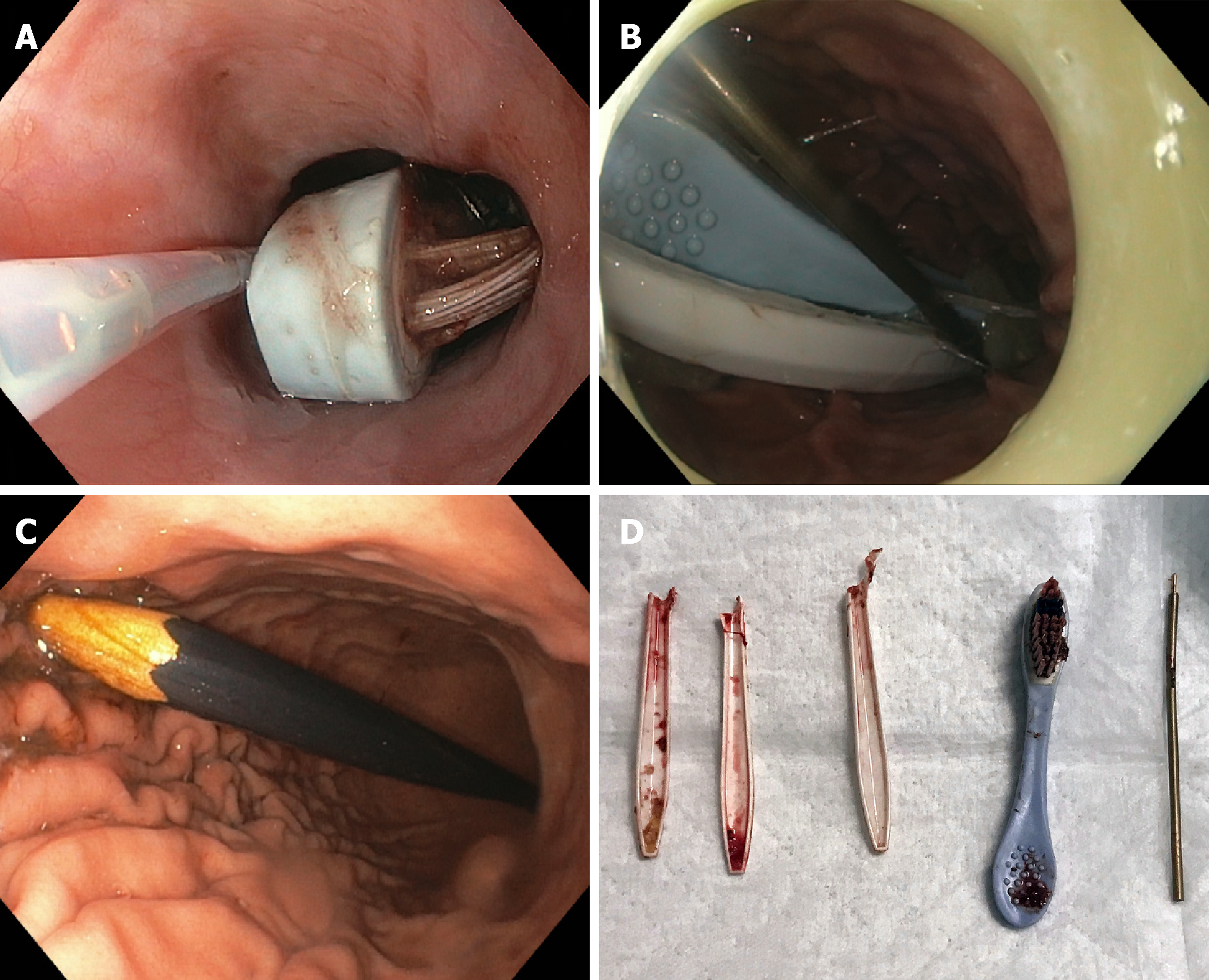
The most common EFI in adults in the Western world is impacted meat[8]. Endoscopic treatment options for disimpaction include extraction of the impacted food bolus or advancement of the bolus into the stomach, as discussed below and summarized schematically in Figure 3. Extraction may involve either en bloc or piecemeal removal, depending on the clinical circumstance, using the various accessories and devices as listed above. Radiographic assessment prior to endoscopy is not necessary unless bone fragments are suspected based on the clinical history; if present, these should serve as an alert to the endoscopist, as they may increase complexity of endoscopic treatment. As mentioned earlier, pharmacologic agents are reasonable in an attempt to promote non-invasive passage of the bolus and avoid urgent endoscopy.
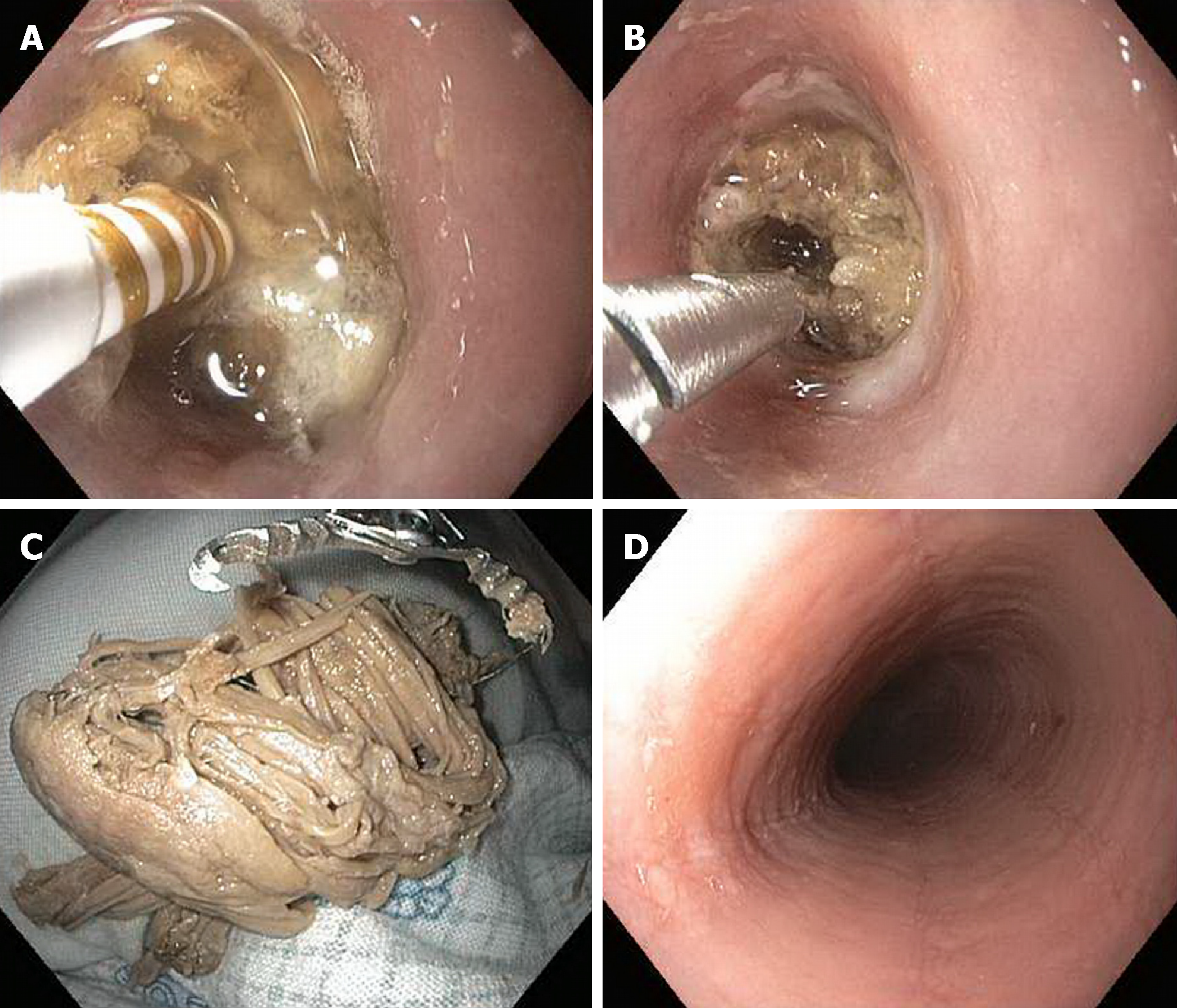
Advancement (i.e., pushing) of the bolus into the stomach is the primary means of treating EFI. Prior to doing so, however, the esophagus distal to the obstruction should be examined (by passing the endoscope around the bolus)[9,29,47,71]. The rationale for this lies in the relatively high incidence of underlying esophageal pathology associated with food impactions, thus raising concern for and risk of esophageal perforation[14,15]. Nevertheless, large published series have suggested that the push technique for soft food impaction, when performed by an experienced endoscopist, is both safe and frequently effective[101,102]. In these series, gentle pressure is applied to the middle of the food bolus in an attempt to push the object into the stomach. If this fails, pieces of the bolus are broken off, typically with forceps, followed by a repeat attempt to push the object forward. A balloon dilation technique has been described wherein a guidewire is passed through the food bolus, over which a dilating balloon is passed, inflated in the stomach, and then pulled back through the stricture; once the stricture is dilated, the food bolus is advanced into the stomach[69]. An alternative technique which the authors have recently described involves burning through a food bolus with a bipolar coagulation probe followed by securing the food bolus with opening of an Ovesco triprong anchor in the burn defect (Figures 4A-D)[103]. Regardless of the technique(s) chosen for an individual case, disimpaction attempts should not be delayed beyond 12-24 h from symptom onset given the increasing risk of complications with time[29,47,49,104,105]. In addition, and as described earlier, an overtube should be used in situations where a food bolus has become soft and fragmented, thus requiring repeated esophageal intubations, or if there is an increased risk of aspiration without an option for timely general endotracheal anesthesia.
Once food bolus advancement or extraction has been performed, in most circumstances, it is considered beneficial and safe to perform esophageal dilation (if an underlying stricture is found) in order to reduce the risk of recurrent EFI[6,29,71,101,102]. In cases of prolonged EFI, if eosinophilic esophagitis is suspected, or if underlying mucosal trauma is noted, dilation should be deferred to a later date (and often following a course of acid suppression therapy) to minimize the risk of iatrogenic perforation[71,106]. If a stricture or other luminal narrowing is not found, esophageal biopsies should be considered after the EFI has been cleared (e.g., to rule out eosinophilic esophagitis).
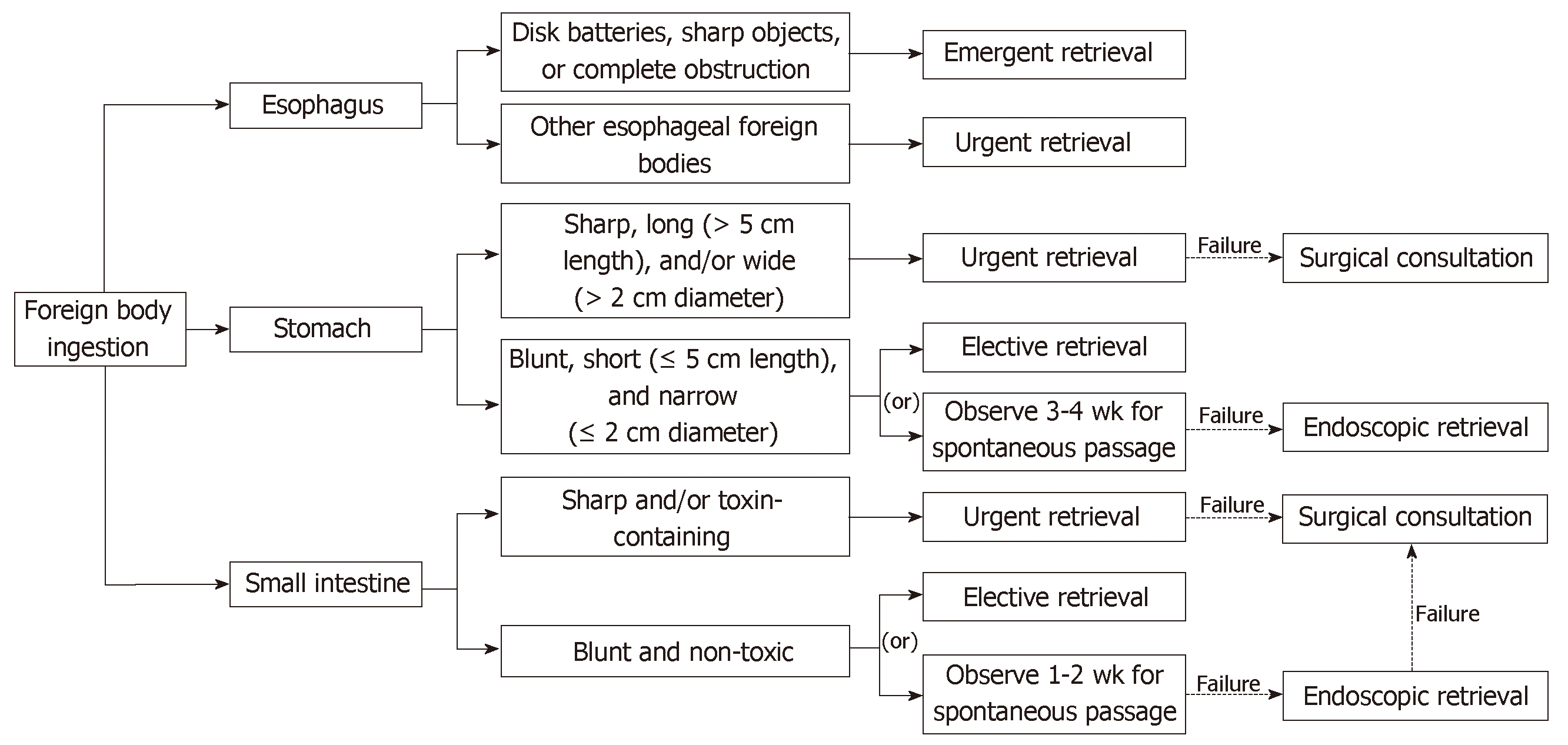
In the forthcoming subsections, we provide an overview of FOI management based on the type/characteristics of the object, as summarized schematically in Figure 5.
FOI involving short, blunt objects such as coins and buttons occurs most often in the pediatric population. When there is suspicion of such FOI in a pediatric patient, X-ray radiographs should be ordered, as impaction in the esophagus may be asymptomatic in a substantial proportion of cases[107]. Coins lodged in the esophagus should be treated with endoscopic retrieval within 12 to 24 h to allow an appropriate pre-anesthetic fast in patients who are asymptomatic[6,80]. In contrast, endoscopic retrieval of coins in the esophagus should be performed emergently in symptomatic patients who are unable to swallow secretions or have acute respiratory symptoms. If more than an hour has elapsed since the last imaging study, imaging should be repeated to confirm that the object is still in the esophagus prior to proceeding with endoscopy. Objects lodged at or above the level of the cricopharyngeus are generally best removed laryngoscopically, while impactions below this level can be removed via flexible upper endoscopy[58,107,108]. If a coin or similar object is found in a patient with several days of symptoms, the possibility of esophageal erosion by the object should be considered, and additional diagnostic evaluation, such as CT imaging, should be performed[37,80].
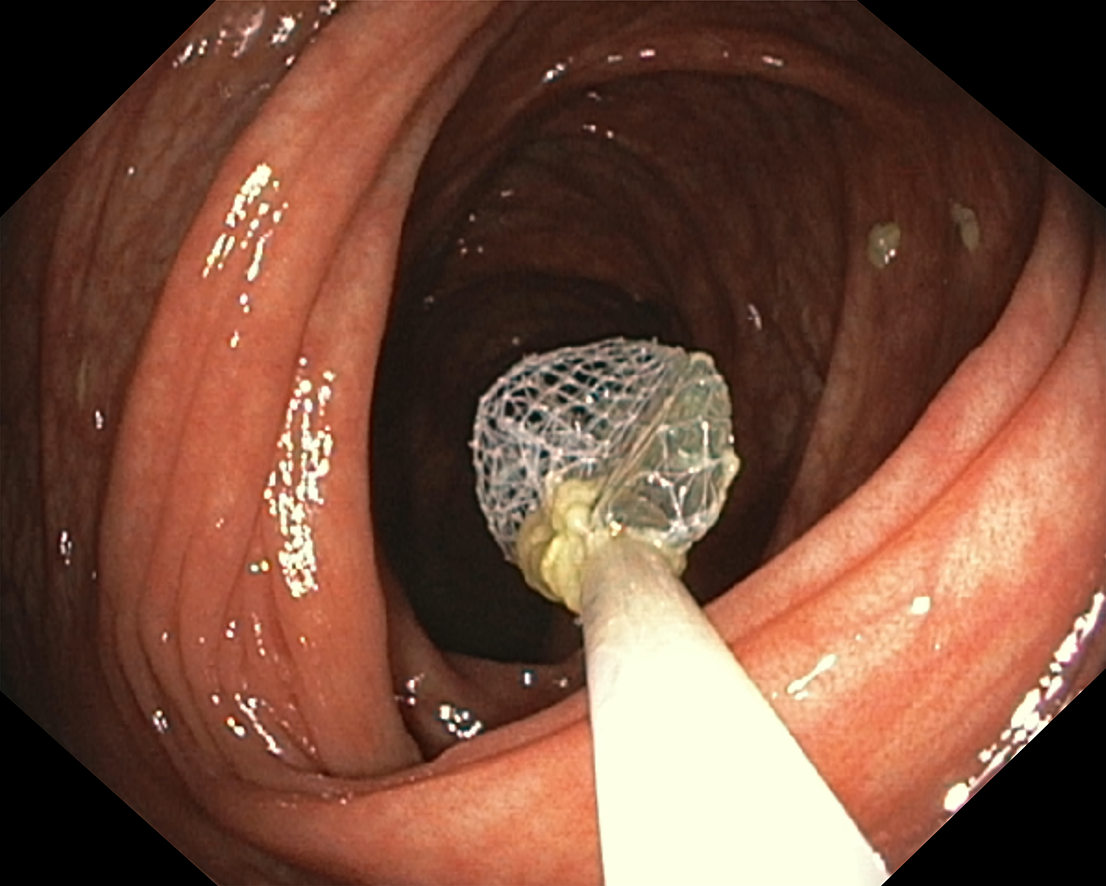
In adults, endoscopic removal can usually be achieved under moderate sedation, whereas in pediatric patients, general endotracheal anesthesia is typically required, as mentioned earlier[57]. Coins can be easily retrieved with a forceps device (e.g., rat-tooth, alligator) or a snare; smooth, spherical objects are best retrieved with a Roth retrieval net[29,109], as demonstrated in a prospective study[72]. Objects that cannot be readily grasped in the esophagus may be advanced into the stomach to facilitate grasping and retrieval[47]. The use of an overtube with an inner diameter greater than that of the ingested object provides an additional degree of safety, particularly if multiple objects are suspected or present[29]. Alternative techniques, including use of Foley balloon catheters and nasogastric tubes outfitted with magnets, have also been reported (e.g., in cases where endoscopy is not readily available)[110,111], but these approaches generally offer no advantage over or are inferior to endoscopic removal[29,68,112]. The major disadvantage to such techniques is that they provide: (1) minimal control of the object as it is being removed; (2) no airway protection; and (3) no visualization of the esophagus to assess for underlying pathology or complications (e.g., mucosal injury)[47]. Once the ingested (blunt, short) object enters the stomach, conservative outpatient management is usually appropriate[6,9,29], and the majority of objects will pass spontaneously within 4 to 6 d. However, spherical objects > 2.5 centimeters in diameter (or smaller in pediatric patients) are less likely to pass the pylorus, and if retained for > 3-4 wk (or less, depending on composition) or remaining in the same location for > 1 wk, should generally be removed endoscopically[8,29,47,54]. A regular diet can usually be continued while patients monitor their stools for passage of the foreign body. As long as a patient remains asymptomatic, radiographs evaluating the progression of small blunt objects can be performed weekly[8,13]. If symptoms of fever, vomiting, or abdominal pain arise, immediate CT imaging is warranted followed by prompt endoscopic and/or surgical evaluation[3,6,8,29].
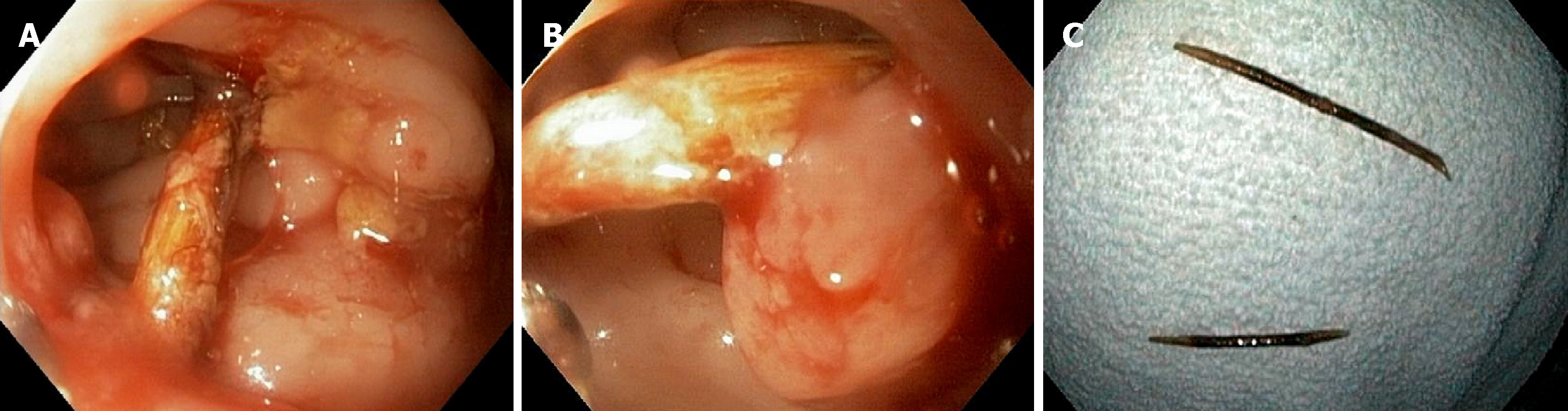
A myriad of sharp and/or pointed FOIs have been described, and these may be accidental or intentional. In children, most such ingestions are accidental; in adults, sharp bones (e.g., fish, chicken) and toothpicks (Figure 6A-C) are usually ingested accidentally, whereas most other sharp and/or pointed FOIs (e.g., pins, needles, razorblades, nails, straightened paper clips) are intentional[29,80]. Patients suspected of sharp and/or pointed FOI must be thoroughly evaluated to define the nature, location, and potential complications related to the object. Since many such objects are not readily visible by plain films, CT imaging may be considered in lieu of (and may be more cost-effective than) simple radiographs[35-38,113], and endoscopy should follow a negative radiologic examination to ensure absence or passage of the FOI, or to provide therapy[56].
Sharp and/or pointed FOIs represent a potential medical emergency given their potential for serious complications, with earlier intervention associated with a lower risk of complications[29,105,114,115]. As with other FOIs, sharp objects lodged at or above the cricopharyngeus should be retrieved via direct laryngoscopy, while objects below this area should be retrieved via flexible endoscopy[116]. Objects will generally pass through the GI tract uneventfully once entering the stomach, though the risk of potential complication is not insignificant[13,80]. Therefore, retrieval should be pursued if within safe endoscopic reach (e.g., in the stomach or proximal small bowel)[29,82,117]. Otherwise, these pointed objects, as with others, may be followed with noninvasive imaging studies to document their passage or failure to progress, in which case surgical consultation should be obtained[8,29]. In the interim, patients should be advised to immediately report abdominal pain, persistent fever, vomiting, hematemesis, or melena.
In the management of sharp and/or pointed FOI, Chevalier Jackson’s axiom: “Advancing points puncture, trailing do not”[8] can be helpful to remember. In this, the father of modern endoscopy of the upper airway and esophagus referred to the ability to minimize risk of mucosal injury during retrieval of sharp objects by orienting the object with its sharp point trailing during extraction. Endoscopic retrieval of such objects can be accomplished with a variety of accessories and devices, including a forceps or snare, depending on the particular object and endoscopist experience[6,47,72]. To further provide mucosal as well as airway protection, overtube use is advisable, or alternatively, the endoscope tip can be fitted with a protector hood, as mentioned previously[23,77,81]. Some endoscopists prefer endotracheal intubation for removal of sharp-pointed objects, but this is seldom required from a procedural perspective if an overtube or protector hood is used[47,82].
Although typically not sharp, long and/or large (> 5 cm) objects (e.g., toothbrushes, pens, eating utensils, dental appliances) may carry considerable risk of complications when ingested (Figure 7). The majority of such objects are unlikely to spontaneously traverse the duodenal sweep and should thus be removed[3,6,118]. Width/thickness of the object should also be considered in addition to length. The GI tract of younger (pediatric) patients is smaller, thus modified dimension criteria should be applied in these patients.
In general, endoscopic retrieval of long or large objects can be performed after an interval of pre-procedural fasting as long as the patient is asymptomatic. A variety of devices and accessories can be used for endoscopic retrieval; commonly, the object is best grasped with a snare or Roth retrieval net and then maneuvered into an overtube[80] (Figure 8). Once this is achieved, the entire apparatus (i.e., foreign object, overtube, and endoscope) can then be removed from the patient in one motion so as to avoid losing grasp of the object within the overtube[29,119].
Due to their small size, slippery texture, as well as increasing prevalence in many everyday electronics (e.g., hearing aids, watches, toys, calculators, etc.), disk and button battery ingestion is on the rise, with children under the age of 5 responsible for most cases[6,120,121]. Direct pressure applied to the mucosa by the battery (leading to pressure necrosis), leakage of strongly alkaline contents (causing chemical damage), and generation of an electrical current (due to the production of hydroxide at the negative pole of the battery, resulting in a high pH), contribute to the high risk of liquefactive necrosis and mural perforation that can rapidly occur when a disk battery is lodged in the esophagus[29,122,123]. Lithium battery ingestions are particularly dangerous given their generally larger size and ability to generate more electrical current in a short period of time[124]. Thus, the use of honey (dosed at 10 mL every 10 min) in the prehospital setting, or sucralfate (dosed at 10 mL every 10 min) in the emergency department setting, has been suggested to coat the battery and delay hydroxide generation and exposure[125,126]. In fact, the National Capital Poison Center has recently updated their Battery Ingestion Triage and Treatment Guideline to incorporate the aforementioned suggestions (for up to 12 h after ingestion of a lithium coin battery)[127]. Of note, however, honey should not be given to children under the age of 1 year due to the risk of infantile botulism[128].
Once discovered on imaging, batteries lodged in the esophagus should be emergently removed, as damage to the esophageal mucosa and deeper tissues can occur within hours[129,130]. Endoscopic retrieval using a retrieval net is often successful for this indication[72]. An alternative method is to use a through-the-scope balloon, whereby a balloon is passed through the working channel beyond the foreign body. The balloon is then inflated, and the entire endoscope and balloon are withdrawn, thus pulling the battery up and out of the body[8]. To protect the airway, an overtube or endotracheal tube is necessary with the aforementioned method. In cases where retrieval of the battery from the esophagus is not possible, the foreign body should be advanced into the stomach, grasped or otherwise captured therein, and then removed. The National Capital Poison Center now also recommends endoscopic irrigation of the injured esophagus with 150 mL of 0.25% acetic acid immediately after battery removal (in an attempt to neutralize injury from alkaline batteries)[127,130], but no studies have been performed to evaluate whether this intervention improves outcomes, and the risks may outweigh the benefits in cases where there is no endoscopically visible chemical injury.
Batteries that have spontaneously progressed beyond the esophagus do not necessarily need to be retrieved unless the patient has signs or symptoms of GI tract injury[129]. A large-diameter (> 20 mm) battery remaining in the stomach longer than 48 h, as documented by repeat imaging, however, should be removed (even in the absence of signs or symptoms of injury)[6,131]. Use of emetics and cathartics has been reported, but this practice is not recommended and may be harmful[6,29,131]. Once beyond the duodenum, the majority of batteries, even those that are large and/or long, will be passed out of the body within 72 h[120] unless a pathologic narrowing (e.g., from adhesions) is present. Radiographs can be obtained every 3 to 4 d to ensure progress and ultimate passage[6].
Ingestion of magnets can cause severe GI injury and even death. The number of magnets is important, as ingestion of a single magnet is unlikely to result in GI complications, whereas ingestion of more than one magnet may be exceedingly hazardous because of the attractive force generated between magnets, which can lead to fistulization, obstruction, mural necrosis, and perforation[6,80].
Imaging should be considered following magnet ingestion to localize the magnet(s), determine their size, and evaluate for the development of complications. It has been suggested that, when possible, any and all magnets be removed, even if only one magnet is reported or visualized on imaging, as undetected magnets or other ingested metal objects together with a magnet can lead to significant injury[132]. In many instances, however, if a magnet is not large and is already beyond the reach of an upper endoscope or enteroscope, careful monitoring for continued passage through the GI tract is preferable[80,133].
Internal concealment of narcotics or other illicit drugs wrapped in plastic or contained in latex condoms, referred to as “body packing,” is a form of drug trafficking[134,135]. Although historically a phenomenon seen only in adults, cases of pediatric body packers (i.e., smuggling “mules”) have been reported[80,136,137]. Drug packets can usually be seen by non-invasive imaging modalities (particularly CT)[138,139]. Use of activated charcoal to bind drug and decrease drug absorption or bowel irrigation with polyethylene glycol solution to promote evacuation may be attempted, but data to support these practices are limited. Paraffin or mineral-oil-based laxatives should be avoided due to their ability to degrade latex and thus increase risk of drug exposure[140]. When imaging is equivocal and/or patient history is unreliable, diagnostic endoscopy can be considered to confirm the presence, location, and number of drug packets. Endoscopic removal, however, should typically not be attempted given the risk of packet rupture, drug leakage, and potentially fatal ensuing events. A Swiss study of 132 patients found the risk of drug packet rupture when left to pass the GI tract on its own to be nil (though the authors acknowledged that variations in risk may exist between different countries based on the quality of the packaging)[141]. Surgical intervention is generally indicated in cases with failure of the packet(s) to progress spontaneously, signs or symptoms of GI obstruction, or suspected packet rupture[47]. On a similar note, endoscopic removal of detergent packets (also known as “laundry pods”) is not recommended, as these packets dissolve quickly, and attempted removal can lead to aspiration and other complications[142].
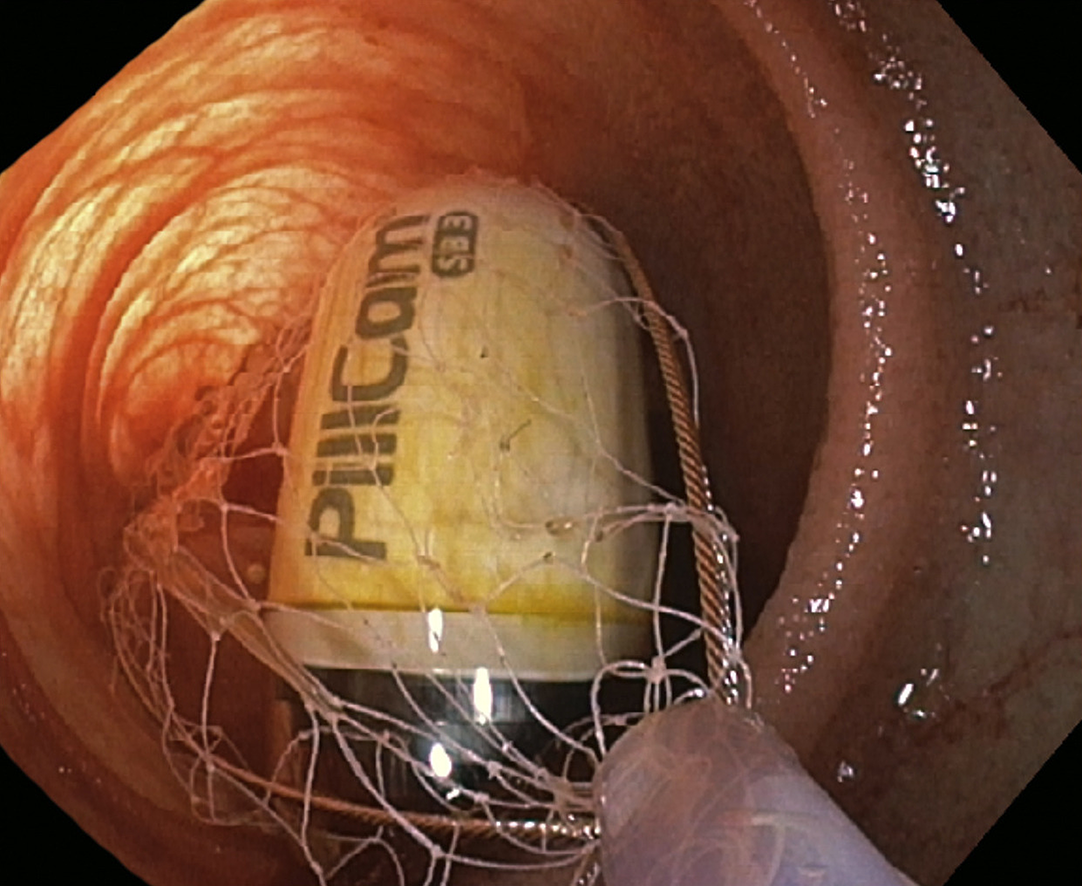
If an object has already passed through the upper GI tract, it will typically continue to pass through the small intestine, into the colon, and out of the body. In some instances, however (e.g., in the setting of jejunal or ileal strictures related to Crohn’s disease or radiation), retention may occur in the midgut, i.e., in the small intestine beyond the reach of a standard upper endoscope. In such instances, enteroscopy (e.g., push, balloon-assisted, and laparoscopically assisted) can facilitate access to and removal of retained objects as well as identification of a cause for retention. For example, case reports and series have described the successful use of anterograde and retrograde balloon enteroscopy to retrieve retained video endoscopy capsules (Figure 9)[143-146] as well as other FOIs[147]. Although data on enteroscopy for retrieval of ingested foreign bodies from the midgut are currently limited, accessories such as hoods, baskets, and forceps, do exist for balloon enteroscopes, and thus it represents an option in select cases. In the interim, clinical decision making regarding enteroscopy in the management of FOIs should consider variables such as the nature of the FOI, patient stability, underlying disease and anatomical factors, anterograde vs. retrograde approach, availability of appropriate endoscopic accessories, need for fluoroscopy, and endoscopist expertise[6].
Colorectal foreign objects can result from anterograde passage of ingested objects down to the colorectum (Figure 8) or from direct retrograde insertion. Retrograde insertion is usually a result of sexual practices, psychiatric illness, or illicit drug smuggling. Patients with colorectal foreign objects may be asymptomatic or may present with a variety of symptoms, including GI bleeding, tenesmus, large bowel obstruction, peritonitis, or perforation. Blunt objects lying low (distally) in the rectum may be amenable to digital removal under moderate sedation; objects in a more proximal location may require sigmoidoscopic or colonoscopic removal. For sharp and/or pointed objects, a digital rectal exam should be deferred; such objects should be removed under direct visualization, generally with a protector hood or similar apparatus. Large objects (e.g., vibrator or bottle) usually require general anesthesia and anal sphincter dilation or retraction, and some may even necessitate the use of a large-caliber rigid proctoscope (usually performed by a colorectal surgeon). In rare instances, laparotomy may be required.
FOI and EFI are common clinical problems which generally require multidisciplinary care coordination. This review has provided evidence- and experience- based guidance and updates regarding the diagnosis and management of FOI and EFI in their various forms and presentations. In many instances, endoscopy is safe and effective and generally the treatment of choice for both FOI and EFI. To further improve patient outcomes associated with these clinical scenarios, well-designed RCTs evaluating pharmacologic, imaging, and endoscopic aspects of the care of patients presenting with FOI and/or EFI may be considered to better formulate evidence-based, cost-effective management strategies.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Morelli L S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | Mowry JB, Spyker DA, Cantilena LR, McMillan N, Ford M. 2013 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 31st Annual Report. Clin Toxicol (Phila). 2014;52:1032-1283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 390] [Cited by in RCA: 320] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 2. | Cevik M, Gókdemir MT, Boleken ME, Sogut O, Kurkcuoglu C. The characteristics and outcomes of foreign body ingestion and aspiration in children due to lodged foreign body in the aerodigestive tract. Pediatr Emerg Care. 2013;29:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 3. | Palta R, Sahota A, Bemarki A, Salama P, Simpson N, Laine L. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc. 2009;69:426-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 150] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 4. | Poynter BA, Hunter JJ, Coverdale JH, Kempinsky CA. Hard to swallow: a systematic review of deliberate foreign body ingestion. Gen Hosp Psychiatry. 2011;33:518-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Volpi A, Laforgia R, Lozito C, Panebianco A, Punzo C, Ialongo P, Carbotta G, Sederino MG, Minafra M, Paterno A, Palasciano N. Ingestion of foreign bodies among prisoners: a ten years retrospective study at University Hospital of Southern Italy. G Chir. 2017;38:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | ASGE Standards of Practice Committee. Ikenberry SO, Jue TL, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Decker GA, Fanelli RD, Fisher LR, Fukami N, Harrison ME, Jain R, Khan KM, Krinsky ML, Maple JT, Sharaf R, Strohmeyer L, Dominitz JA. Management of ingested foreign bodies and food impactions. Gastrointest Endosc. 2011;73:1085-1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 501] [Article Influence: 35.8] [Reference Citation Analysis (1)] |
| 7. | Peng A, Li Y, Xiao Z, Wu W. Study of clinical treatment of esophageal foreign body-induced esophageal perforation with lethal complications. Eur Arch Otorhinolaryngol. 2012;269:2027-2036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc. 1995;41:39-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 356] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 9. | Birk M, Bauerfeind P, Deprez PH, Häfner M, Hartmann D, Hassan C, Hucl T, Lesur G, Aabakken L, Meining A. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:489-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 388] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 10. | Dalal PP, Otey AJ, McGonagle EA, Whitmill ML, Levine EJ, McKimmie RL, Thomas AC, Cook CH, Papadimos TJ, Reilley TE, Bergese SD, Steinberg SM, Stawicki SP, Evans DC. Intentional foreign object ingestions: need for endoscopy and surgery. J Surg Res. 2013;184:145-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Weiland ST, Schurr MJ. Conservative management of ingested foreign bodies. J Gastrointest Surg. 2002;6:496-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Huang BL, Rich HG, Simundson SE, Dhingana MK, Harrington C, Moss SF. Intentional swallowing of foreign bodies is a recurrent and costly problem that rarely causes endoscopy complications. Clin Gastroenterol Hepatol. 2010;8:941-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Vizcarrondo FJ, Brady PG, Nord HJ. Foreign bodies of the upper gastrointestinal tract. Gastrointest Endosc. 1983;29:208-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 120] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Sperry SL, Crockett SD, Miller CB, Shaheen NJ, Dellon ES. Esophageal foreign-body impactions: epidemiology, time trends, and the impact of the increasing prevalence of eosinophilic esophagitis. Gastrointest Endosc. 2011;74:985-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 159] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 15. | Desai TK, Stecevic V, Chang CH, Goldstein NS, Badizadegan K, Furuta GT. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointest Endosc. 2005;61:795-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 272] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 16. | Remedios M, Jones D, Kerlin P. Eosinophilic oesophagitis: epidemiology, pathogenesis and management. Drugs. 2011;71:527-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Marçal N, Soares JB, Pereira G, Guimarães J, Gonçalves M, Godinho T. The management of ingested foreign bodies in an Ear Nose and Throat Emergency Unit: prospective study of 204 cases. Acta Otorrinolaringol Esp. 2013;64:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Damghani M, Halavati N, Motamedi N. Foreign body in the upper airway and oesophagus: a seven years study from Iran. J Pak Med Assoc. 2011;61:859-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Orji FT, Akpeh JO, Okolugbo NE. Management of esophageal foreign bodies: experience in a developing country. World J Surg. 2012;36:1083-1088. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Bekele A. Aerodigestive foreign bodies in adult ethiopian patients: a prospective study at tikur anbessa hospital, ethiopia. Int J Otolaryngol. 2014;2014:293603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Kamath P, Bhojwani KM, Prasannaraj T, Abhijith K. Foreign bodies in the aerodigestive tract--a clinical study of cases in the coastal belt of South India. Am J Otolaryngol. 2006;27:373-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Li ZS, Sun ZX, Zou DW, Xu GM, Wu RP, Liao Z. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest Endosc. 2006;64:485-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 160] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 23. | Zhang S, Cui Y, Gong X, Gu F, Chen M, Zhong B. Endoscopic management of foreign bodies in the upper gastrointestinal tract in South China: a retrospective study of 561 cases. Dig Dis Sci. 2010;55:1305-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | Jafari SA, Khalesi M, Partovi S, Kiani M, Ahanchian H, Kianifar H. Ingested Foreign Bodies Removed by flexible Endoscopy in Pediatric Patients: A 10-year Retrospective Study [corrected]. Iran J Otorhinolaryngol. 2014;26:175-179. [PubMed] |
| 25. | Cheng W, Tam PK. Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg. 1999;34:1472-1476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 197] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 26. | Al Lawati TT, Al Marhoobi R. Patterns and Complications of Ingested Foreign Bodies in Omani Children. Oman Med J. 2018;33:463-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Majola NF, Kong VY, Mangray H, Govindasamy V, Laing GL, Clarke DL. An audit of ingested and aspirated foreign bodies in children at a university hospital in South Africa: The Pietermaritzburg experience. S Afr Med J. 2018;108:205-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Connolly AA, Birchall M, Walsh-Waring GP, Moore-Gillon V. Ingested foreign bodies: patient-guided localization is a useful clinical tool. Clin Otolaryngol Allied Sci. 1992;17:520-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 35] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc. 1995;41:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 168] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 30. | Chowdhury CR, Bricknell MC, MacIver D. Oesophageal foreign body: an unusual cause of respiratory symptoms in a three-week-old baby. J Laryngol Otol. 1992;106:556-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Panieri E, Bass DH. The management of ingested foreign bodies in children--a review of 663 cases. Eur J Emerg Med. 1995;2:83-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 71] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 32. | Diaconescu S, Gimiga N, Sarbu I, Stefanescu G, Olaru C, Ioniuc I, Ciongradi I, Burlea M. Foreign Bodies Ingestion in Children: Experience of 61 Cases in a Pediatric Gastroenterology Unit from Romania. Gastroenterol Res Pract. 2016;2016:1982567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 33. | Caravati EM, Bennett DL, McElwee NE. Pediatric coin ingestion. A prospective study on the utility of routine roentgenograms. Am J Dis Child. 1989;143:549-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 38] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 34. | Henderson CT, Engel J, Schlesinger P. Foreign body ingestion: review and suggested guidelines for management. Endoscopy. 1987;19:68-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 92] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 35. | Marco De Lucas E, Sádaba P, Lastra García-Barón P, Ruiz-Delgado ML, González Sánchez F, Ortiz A, Pagola MA. Value of helical computed tomography in the management of upper esophageal foreign bodies. Acta Radiol. 2004;45:369-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 36. | Eliashar R, Dano I, Dangoor E, Braverman I, Sichel JY. Computed tomography diagnosis of esophageal bone impaction: a prospective study. Ann Otol Rhinol Laryngol. 1999;108:708-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 37. | Ma J, Kang DK, Bae JI, Park KJ, Sun JS. Value of MDCT in diagnosis and management of esophageal sharp or pointed foreign bodies according to level of esophagus. AJR Am J Roentgenol. 2013;201:W707-W711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 38. | Zhu Z, Li W, Zhang L, Hu J, Wang W, Ma Z. The predictive role of dual source CT for esophageal foreign bodies. Am J Otolaryngol. 2014;35:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 39. | Takada M, Kashiwagi R, Sakane M, Tabata F, Kuroda Y. 3D-CT diagnosis for ingested foreign bodies. Am J Emerg Med. 2000;18:192-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 40. | Bassett KE, Schunk JE, Logan L. Localizing ingested coins with a metal detector. Am J Emerg Med. 1999;17:338-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 41. | Doraiswamy NV, Baig H, Hallam L. Metal detector and swallowed metal foreign bodies in children. J Accid Emerg Med. 1999;16:123-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | James V, Hamzah HB, Ganapathy S. Handheld Metal Detector Screening for Metallic Foreign Body Ingestion in Children. J Vis Exp. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 43. | Hamzah HB, James V, Manickam S, Ganapathy S. Handheld Metal Detector for Metallic Foreign Body Ingestion in Pediatric Emergency. Indian J Pediatr. 2018;85:618-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 44. | Nation J, Jiang W. The utility of a handheld metal detector in detection and localization of pediatric metallic foreign body ingestion. Int J Pediatr Otorhinolaryngol. 2017;92:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 45. | Guelfguat M, Kaplinskiy V, Reddy SH, DiPoce J. Clinical guidelines for imaging and reporting ingested foreign bodies. AJR Am J Roentgenol. 2014;203:37-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 46. | Rybojad B, Niedzielska G, Niedzielski A, Rudnicka-Drozak E, Rybojad P. Esophageal foreign bodies in pediatric patients: a thirteen-year retrospective study. ScientificWorldJournal. 2012;2012:102642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 47. | Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ 2nd, Waring JP, Fanelli RD, Wheeler-Harbough J; American Society for Gastrointestinal Endoscopy. Guideline for the management of ingested foreign bodies. Gastrointest Endosc. 2002;55:802-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 361] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 48. | Park JH, Park CH, Park JH, Lee SJ, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS, Kim SJ. [Review of 209 cases of foreign bodies in the upper gastrointestinal tract and clinical factors for successful endoscopic removal]. Korean J Gastroenterol. 2004;43:226-233. [PubMed] |
| 49. | Loh KS, Tan LK, Smith JD, Yeoh KH, Dong F. Complications of foreign bodies in the esophagus. Otolaryngol Head Neck Surg. 2000;123:613-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 50. | Geng C, Li X, Luo R, Cai L, Lei X, Wang C. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a retrospective study of 1294 cases. Scand J Gastroenterol. 2017;52:1286-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 52. | Velitchkov NG, Grigorov GI, Losanoff JE, Kjossev KT. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg. 1996;20:1001-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 261] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 53. | Hachimi-Idrissi S, Corne L, Vandenplas Y. Management of ingested foreign bodies in childhood: our experience and review of the literature. Eur J Emerg Med. 1998;5:319-323. [PubMed] |
| 54. | Kim JK, Kim SS, Kim JI, Kim SW, Yang YS, Cho SH, Lee BS, Han NI, Han SW, Chung IS, Chung KW, Sun HS. Management of foreign bodies in the gastrointestinal tract: an analysis of 104 cases in children. Endoscopy. 1999;31:302-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 55. | Libânio D, Garrido M, Jácome F, Dinis-Ribeiro M, Pedroto I, Marcos-Pinto R. Foreign body ingestion and food impaction in adults: better to scope than to wait. United European Gastroenterol J. 2018;6:974-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 56. | Ciriza C, García L, Suárez P, Jiménez C, Romero MJ, Urquiza O, Dajil S. What predictive parameters best indicate the need for emergent gastrointestinal endoscopy after foreign body ingestion? J Clin Gastroenterol. 2000;31:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 57. | Gmeiner D, von Rahden BH, Meco C, Hutter J, Oberascher G, Stein HJ. Flexible versus rigid endoscopy for treatment of foreign body impaction in the esophagus. Surg Endosc. 2007;21:2026-2029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 58. | Russell R, Lucas A, Johnson J, Yannam G, Griffin R, Beierle E, Anderson S, Chen M, Harmon C. Extraction of esophageal foreign bodies in children: rigid versus flexible endoscopy. Pediatr Surg Int. 2014;30:417-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 59. | Herranz-Gonzalez J, Martinez-Vidal J, Garcia-Sarandeses A, Vazquez-Barro C. Esophageal foreign bodies in adults. Otolaryngol Head Neck Surg. 1991;105:649-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 60. | Bennett AM, Sharma A, Price T, Montgomery PQ. The management of foreign bodies in the pharynx and oesophagus using transnasal flexible laryngo-oesophagoscopy (TNFLO). Ann R Coll Surg Engl. 2008;90:13-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 61. | Chu KM, Choi HK, Tuen HH, Law SY, Branicki FJ, Wong J. A prospective randomized trial comparing the use of omeprazole-based dual and triple therapy for eradication of Helicobacter pylori. Am J Gastroenterol. 1998;93:1436-1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 62. | Yuki T, Ishihara S, Okada M, Kusunoki R, Moriyama I, Amano Y, Kinoshita Y. Double-balloon endoscopy for treatment of small bowel penetration by fish bone. Dig Endosc. 2012;24:281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 63. | Miehlke S, Tausche AK, Brückner S, Aust D, Morgner A, Madisch A. Retrieval of two retained endoscopy capsules with retrograde double-balloon enteroscopy in a patient with a history of complicated small-bowel disease. Endoscopy. 2007;39 Suppl 1:E157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 64. | Safatle-Ribeiro AV, Couto DS, Ferreira de Souza T, Lorenzi F, Hourneaux de Moura EG, Sakai P. Single-balloon endoscopy for removing a foreign body in the small bowel (with video). Gastrointest Endosc. 2009;70:781-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 65. | Flynn AD, Chiorean MV. Retrieval of a large foreign body from the ileum with double-balloon enteroscopy (with videos). Gastrointest Endosc. 2014;79:519-20; discussion 520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 66. | Saeed ZA, Michaletz PA, Feiner SD, Woods KL, Graham DY. A new endoscopic method for managing food impaction in the esophagus. Endoscopy. 1990;22:226-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 67. | Chávez Rossell M. [New technique for safe removal of impacted foreign bodies in the upper gastrointestinal tract using reusable variceal "cap" (cup, cap or cylinder)]. Rev Gastroenterol Peru. 2012;32:150-156. [PubMed] |
| 68. | Schunk JE, Harrison AM, Corneli HM, Nixon GW. Fluoroscopic foley catheter removal of esophageal foreign bodies in children: experience with 415 episodes. Pediatrics. 1994;94:709-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 69. | Siddiqui AA, Harford WV, Spechler SJ. Through-the-scope, wire-guided esophageal dilation for the treatment of food impaction. Dig Dis Sci. 2008;53:2394-2396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 70. | Kay M, Wyllie R. Suture technique for endoscopic removal of unusual foreign bodies. Gastrointest Endosc. 2007;66:865; author reply 865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 71. | Triadafilopoulos G, Roorda A, Akiyama J. Update on foreign bodies in the esophagus: diagnosis and management. Curr Gastroenterol Rep. 2013;15:317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 72. | Faigel DO, Stotland BR, Kochman ML, Hoops T, Judge T, Kroser J, Lewis J, Long WB, Metz DC, O'Brien C, Smith DB, Ginsberg GG. Device choice and experience level in endoscopic foreign object retrieval: an in vivo study. Gastrointest Endosc. 1997;45:490-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 44] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 73. | Nelson DB, Bosco JJ, Curtis WD, Faigel DO, Kelsey PB, Leung JW, Mills MR, Smith P, Tarnasky PR, VanDam J, Wassef WY. ASGE technology status evaluation report. Endoscopic retrieval devices. February 1999. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc. 1999;50:932-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 74. | Kirchner GI, Zuber-Jerger I, Endlicher E, Gelbmann C, Ott C, Ruemmele P, Schölmerich J, Klebl F. Causes of bolus impaction in the esophagus. Surg Endosc. 2011;25:3170-3174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 75. | Kelley JE, Leech MH, Carr MG. A safe and cost-effective protocol for the management of esophageal coins in children. J Pediatr Surg. 1993;28:898-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 76. | Conners GP. A literature-based comparison of three methods of pediatric esophageal coin removal. Pediatr Emerg Care. 1997;13:154-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 77. | Zhang S, Wang J, Wang J, Zhong B, Chen M, Cui Y. Transparent cap-assisted endoscopic management of foreign bodies in the upper esophagus: a randomized, controlled trial. J Gastroenterol Hepatol. 2013;28:1339-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 78. | Spurling TJ, Zaloga GP, Richter JE. Fiberendoscopic removal of a gastric foreign body with overtube technique. Gastrointest Endosc. 1983;29:226-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 79. | ASGE Technology Committee. Tierney WM, Adler DG, Conway JD, Diehl DL, Farraye FA, Kantsevoy SV, Kaul V, Kethu SR, Kwon RS, Mamula P, Pedrosa MC, Rodriguez SA. Overtube use in gastrointestinal endoscopy. Gastrointest Endosc. 2009;70:828-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 80. | Kay M, Wyllie R. Pediatric foreign bodies and their management. Curr Gastroenterol Rep. 2005;7:212-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 170] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 81. | Bertoni G, Sassatelli R, Conigliaro R, Bedogni G. A simple latex protector hood for safe endoscopic removal of sharp-pointed gastroesophageal foreign bodies. Gastrointest Endosc. 1996;44:458-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 82. | Smith MT, Wong RK. Foreign bodies. Gastrointest Endosc Clin N Am. 2007;17:361-382, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 83. | Tibbling L, Bjorkhoel A, Jansson E, Stenkvist M. Effect of spasmolytic drugs on esophageal foreign bodies. Dysphagia. 1995;10:126-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 41] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 84. | Robbins MI, Shortsleeve MJ. Treatment of acute esophageal food impaction with glucagon, an effervescent agent, and water. AJR Am J Roentgenol. 1994;162:325-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 85. | Al-Haddad M, Ward EM, Scolapio JS, Ferguson DD, Raimondo M. Glucagon for the relief of esophageal food impaction does it really work? Dig Dis Sci. 2006;51:1930-1933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 86. | Sodeman TC, Harewood GC, Baron TH. Assessment of the predictors of response to glucagon in the setting of acute esophageal food bolus impaction. Dysphagia. 2004;19:18-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 87. | Thimmapuram J, Oosterveen S, Grim R. Use of glucagon in relieving esophageal food bolus impaction in the era of eosinophilic esophageal infiltration. Dysphagia. 2013;28:212-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 88. | Colon V, Grade A, Pulliam G, Johnson C, Fass R. Effect of doses of glucagon used to treat food impaction on esophageal motor function of normal subjects. Dysphagia. 1999;14:27-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 89. | Trenkner SW, Maglinte DD, Lehman GA, Chernish SM, Miller RE, Johnson CW. Esophageal food impaction: treatment with glucagon. Radiology. 1983;149:401-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 55] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 90. | Rice BT, Spiegel PK, Dombrowski PJ. Acute esophageal food impaction treated by gas-forming agents. Radiology. 1983;146:299-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 34] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 91. | Karanjia ND, Rees M. The use of Coca-Cola in the management of bolus obstruction in benign oesophageal stricture. Ann R Coll Surg Engl. 1993;75:94-95. [PubMed] |
| 92. | Smith JC, Janower ML, Geiger AH. Use of glucagon and gas-forming agents in acute esophageal food impaction. Radiology. 1986;159:567-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 93. | Lee J, Anderson R. Best evidence topic report. Effervescent agents for oesophageal food bolus impaction. Emerg Med J. 2005;22:123-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 94. | Leopard D, Fishpool S, Winter S. The management of oesophageal soft food bolus obstruction: a systematic review. Ann R Coll Surg Engl. 2011;93:441-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 95. | Ignotus PI, Grundy A. Disimpaction of swallowed bolus. BMJ. 1989;298:1359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 96. | Thomas L, Webb C, Duvvi S, Jones T, Reddy KT. Is buscopan effective in meat bolus obstruction? Clin Otolaryngol. 2005;30:183-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 97. | Basavaraj S, Penumetcha KR, Cable HR, Umapathy N. Buscopan in oesophageal food bolus: is it really effective? Eur Arch Otorhinolaryngol. 2005;262:524-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 98. | Tutuian R; Clinical Lead Outpatient Services and Gastrointestinal Function Laboratory. Adverse effects of drugs on the esophagus. Best Pract Res Clin Gastroenterol. 2010;24:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 99. | Giordano A, Adams G, Boies L, Meyerhoff W. Current management of esophageal foreign bodies. Arch Otolaryngol. 1981;107:249-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 53] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 100. | ANDERSEN HA, BERNATZ PE, GRINDLAY JH. Perforation of the esophagus after use of a digestant agent: report of case and experimental study. Ann Otol Rhinol Laryngol. 1959;68:890-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 101. | Vicari JJ, Johanson JF, Frakes JT. Outcomes of acute esophageal food impaction: success of the push technique. Gastrointest Endosc. 2001;53:178-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 77] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 102. | Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective, observational study. Gastrointest Endosc. 2001;53:193-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 161] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 103. | Saffouri GB, Gomez V, Tabibian JH, Wong Kee Song LM. Burn and anchor: a novel food impaction retrieval technique. Gastrointest Endosc. 2016;83:1029-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 104. | Chaikhouni A, Kratz JM, Crawford FA. Foreign bodies of the esophagus. Am Surg. 1985;51:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 105. | Chaves DM, Ishioka S, Félix VN, Sakai P, Gama-Rodrigues JJ. Removal of a foreign body from the upper gastrointestinal tract with a flexible endoscope: a prospective study. Endoscopy. 2004;36:887-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 68] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 106. | Kerlin P, Jones D, Remedios M, Campbell C. Prevalence of eosinophilic esophagitis in adults with food bolus obstruction of the esophagus. J Clin Gastroenterol. 2007;41:356-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 147] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 107. | Hodge D, Tecklenburg F, Fleisher G. Coin ingestion: does every child need a radiograph? Ann Emerg Med. 1985;14:443-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 52] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 108. | Yalçin S, Karnak I, Ciftci AO, Senocak ME, Tanyel FC, Büyükpamukçu N. Foreign body ingestion in children: an analysis of pediatric surgical practice. Pediatr Surg Int. 2007;23:755-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 109. | Asge Technology Committee. Diehl DL, Adler DG, Conway JD, Farraye FA, Kantsevoy SV, Kaul V, Kethu SR, Kwon RS, Mamula P, Rodriguez SA, Tierney WM. Endoscopic retrieval devices. Gastrointest Endosc. 2009;69:997-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 110. | Hawkins DB. Removal of blunt foreign bodies from the esophagus. Ann Otol Rhinol Laryngol. 1990;99:935-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 46] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 111. | Paulson EK, Jaffe RB. Metallic foreign bodies in the stomach: fluoroscopic removal with a magnetic orogastric tube. Radiology. 1990;174:191-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 112. | Campbell JB, Foley LC. A safe alternative to endoscopic removal of blunt esophageal foreign bodies. Arch Otolaryngol. 1983;109:323-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 113. | Shrime MG, Johnson PE, Stewart MG. Cost-effective diagnosis of ingested foreign bodies. Laryngoscope. 2007;117:785-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 114. | Wu WT, Chiu CT, Kuo CJ, Lin CJ, Chu YY, Tsou YK, Su MY. Endoscopic management of suspected esophageal foreign body in adults. Dis Esophagus. 2011;24:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 115. | Zhang X, Jiang Y, Fu T, Zhang X, Li N, Tu C. Esophageal foreign bodies in adults with different durations of time from ingestion to effective treatment. J Int Med Res. 2017;45:1386-1393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 116. | Jeen YT, Chun HJ, Song CW, Um SH, Lee SW, Choi JH, Kim CD, Ryu HS, Hyun JH. Endoscopic removal of sharp foreign bodies impacted in the esophagus. Endoscopy. 2001;33:518-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 117. | Selivanov V, Sheldon GF, Cello JP, Crass RA. Management of foreign body ingestion. Ann Surg. 1984;199:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 118. | Blaho KE, Merigian KS, Winbery SL, Park LJ, Cockrell M. Foreign body ingestions in the Emergency Department: case reports and review of treatment. J Emerg Med. 1998;16:21-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 67] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 119. | Chinitz MA, Bertrand G. Endoscopic removal of toothbrushes. Gastrointest Endosc. 1990;36:527-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 120. | Litovitz TL. Battery ingestions: product accessibility and clinical course. Pediatrics. 1985;75:469-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 121. | Litovitz T, Whitaker N, Clark L. Preventing battery ingestions: an analysis of 8648 cases. Pediatrics. 2010;125:1178-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 166] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 122. | Gordon AC, Gough MH. Oesophageal perforation after button battery ingestion. Ann R Coll Surg Engl. 1993;75:362-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 123. | Krom H, Visser M, Hulst JM, Wolters VM, Van den Neucker AM, de Meij T, van der Doef HPJ, Norbruis OF, Benninga MA, Smit MJM, Kindermann A. Serious complications after button battery ingestion in children. Eur J Pediatr. 2018;177:1063-1070. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 124. | Marom T, Goldfarb A, Russo E, Roth Y. Battery ingestion in children. Int J Pediatr Otorhinolaryngol. 2010;74:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 125. | Anfang RR, Jatana KR, Linn RL, Rhoades K, Fry J, Jacobs IN. pH-neutralizing esophageal irrigations as a novel mitigation strategy for button battery injury. Laryngoscope. 2019;129:49-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 126. | Soto PH, Reid NE, Litovitz TL. Time to perforation for button batteries lodged in the esophagus. Am J Emerg Med. 2018;pii:S0735-6757(18)30594-1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 127. | National Capital Poison Center. National Capital Poison Center Button Battery Ingestion Triage and Treatment Guideline. 2018; Available from: https://www.poison.org/battery/guideline. |
| 128. | Rosow LK, Strober JB. Infant botulism: review and clinical update. Pediatr Neurol. 2015;52:487-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 129. | Rosenfeld EH, Sola R, Yu Y, St Peter SD, Shah SR. Battery ingestions in children: Variations in care and development of a clinical algorithm. J Pediatr Surg. 2018;53:1537-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 130. | Jatana KR, Rhoades K, Milkovich S, Jacobs IN. Basic mechanism of button battery ingestion injuries and novel mitigation strategies after diagnosis and removal. Laryngoscope. 2017;127:1276-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 99] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 131. | Litovitz T, Schmitz BF. Ingestion of cylindrical and button batteries: an analysis of 2382 cases. Pediatrics. 1992;89:747-757. [PubMed] |
| 132. | Butterworth J, Feltis B. Toy magnet ingestion in children: revising the algorithm. J Pediatr Surg. 2007;42:e3-e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 133. | Sola R, Rosenfeld EH, Yu YR, St Peter SD, Shah SR. Magnet foreign body ingestion: rare occurrence but big consequences. J Pediatr Surg. 2018;53:1815-1819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 134. | Lancashire MJ, Legg PK, Lowe M, Davidson SM, Ellis BW. Surgical aspects of international drug smuggling. Br Med J (Clin Res Ed). 1988;296:1035-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 135. | Booker RJ, Smith JE, Rodger MP. Packers, pushers and stuffers--managing patients with concealed drugs in UK emergency departments: a clinical and medicolegal review. Emerg Med J. 2009;26:316-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 136. | Beno S, Calello D, Baluffi A, Henretig FM. Pediatric body packing: drug smuggling reaches a new low. Pediatr Emerg Care. 2005;21:744-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 137. | Traub SJ, Kohn GL, Hoffman RS, Nelson LS. Pediatric "body packing". Arch Pediatr Adolesc Med. 2003;157:174-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 35] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 138. | Cranston PE, Pollack CV, Harrison RB. CT of crack cocaine ingestion. J Comput Assist Tomogr. 1992;16:560-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 139. | Bulakci M, Kalelioglu T, Bulakci BB, Kiris A. Comparison of diagnostic value of multidetector computed tomography and X-ray in the detection of body packing. Eur J Radiol. 2013;82:1248-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 140. | White N, Taylor K, Lyszkowski A, Tullett J, Morris C. Dangers of lubricants used with condoms. Nature. 1988;335:19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 141. | Heymann-Maier L, Trueb L, Schmidt S, Carron PN, Hugli O, Heymann E, Yersin B. Emergency department management of body packers and body stuffers. Swiss Med Wkly. 2017;147:w14499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 142. | Kurowski JA, Kay M. Caustic Ingestions and Foreign Bodies Ingestions in Pediatric Patients. Pediatr Clin North Am. 2017;64:507-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 143. | Lee BI, Choi H, Choi KY, Ji JS, Kim BW, Cho SH, Park JM, Lee IS, Choi MG, Chung IS. Retrieval of a retained capsule endoscope by double-balloon enteroscopy. Gastrointest Endosc. 2005;62:463-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 144. | May A, Nachbar L, Ell C. Extraction of entrapped capsules from the small bowel by means of push-and-pull enteroscopy with the double-balloon technique. Endoscopy. 2005;37:591-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 145. | Makipour K, Modiri AN, Ehrlich A, Friedenberg FK, Maranki J, Enestvedt BK, Heller S, Tokar J, Haluszka O. Double balloon enteroscopy: effective and minimally invasive method for removal of retained video capsules. Dig Endosc. 2014;26:646-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 146. | Le L, Fung BM, Tabibian JH. Capsule Endoscopy for Refractory Iron Deficiency Anemia in Crohn's Disease: Captivating Pathology, Hybrid Therapy. Gastroenterology. 2018;155:276-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 147. | Neumann H, Fry LC, Rickes S, Jurczok C, Malfertheiner P, Mönkemüller K. A 'double-balloon enteroscopy worth the money': endoscopic removal of a coin lodged in the small bowel. Dig Dis. 2008;26:388-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 148. | Elhanafi S, Chandrasekhara V, Tabibian JH. Endoscopic Removal of Shattered Glass From the Cecum. Am J Gastroenterol. 2017;112:15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |