Published online Nov 16, 2019. doi: 10.4253/wjge.v11.i11.541
Peer-review started: May 20, 2019
First decision: August 2, 2019
Revised: August 17, 2019
Accepted: September 11, 2019
Article in press: September 11, 2019
Published online: November 16, 2019
Processing time: 180 Days and 22.6 Hours
Oesophageal cancer is the fourth most common cause of cancer-related deaths in India. Esophageal squamous cell carcinomas (ESCCs) arise from the epithelial layer, and commonly present as polypoidal, ulcerative or ulceroproliferative growth in the oesophageal lumen. In contrast, oesophageal submucosal tumours are a distinct group of tumours arising from the mesenchyme (examples include leiomyoma, fibrovasculoma, lipoma, granular cell tumour or carcinoid), and mostly do not breach the mucosa. Oesophageal submucosal tumours are a distinct group of tumours arising from the mesenchyme, and mostly do not breach the mucosa. Complete intramural growth of an advanced primary ESCC is an exceedingly rare presentation, with only six cases reported in the literature thus far. We herein report a case of primary ESCC with complete intramural invasion that endoscopically mimics a submucosal lesion.
A 50 year old male presented with a progressive mechanical type of dysphagia for one month. His history was significant, including squamous cell carcinoma of the tongue that was treated with surgery and chemoradiation 1 year prior. Upper gastrointestinal endoscopy revealed a large, hemispherical lesion with normal-appearing overlying mucosa about 4 cm × 5 cm in size extending from 30-34 cm from incisors. The patient underwent endoscopic ultrasound (EUS), and a fine‑needle biopsy was performed, which was suggestive for squamous cell carcinoma. We herein report a case of primary ESCC with complete intramural invasion, endoscopically mimicking a submucosal lesion. The diagnosis could be established only by a EUS-guided biopsy.
This case report highlights that intramural ESCC may look like a submucosal lesion in endoscopy, and EUS biopsy is needed for final diagnosis.
Core tip: A 50 year old male presented with a progressive mechanical type of dysphagia. Upper gastrointestinal endoscopy revealed a large, hemispherical lesion with normal-appearing overlying mucosa. An endoscopic ultrasound (EUS) fine needle biopsy was done. Histopathology was consistent with well-differentiated squamous cell carcinoma. This is to highlight that intramural esophageal squamous cell carcinoma may look like a benign submucosal lesion upon endoscopy, and that a EUS biopsy is needed for final diagnosis.
- Citation: Shanmugam RM, Shanmugam C, Murugesan M, Kalyansundaram M, Gopalsamy S, Ranjan A. Oesophageal carcinoma mimicking a submucosal lesion: A case report. World J Gastrointest Endosc 2019; 11(11): 541-547
- URL: https://www.wjgnet.com/1948-5190/full/v11/i11/541.htm
- DOI: https://dx.doi.org/10.4253/wjge.v11.i11.541
Oesophageal cancer is the fourth most common cause of cancer-related deaths in India. It is prevalent among both men and women. Squamous cell carcinoma accounts for up to 80% of these cancers[1]. The etiologic factors for esophageal squamous cell carcinomas (ESCCs) show a regional variation in different parts of India, but tobacco consumption in various forms, as well as alcohol, hot beverages and poor nutrition remain the predominant predisposing factors. The majority of patients with advanced disease are symptomatic, most often presenting with dysphagia and weight loss.
ESCCs arise from the epithelial layer, and commonly present as polypoidal, ulcerative or proliferative ulcer growth in the oesophageal lumen. In contrast, oesophageal submucosal tumours are a distinct group of tumours arising from the mesenchyme (examples include leiomyoma, fibrovasculoma, lipoma, granular cell tumour or carcinoid), and mostly do not breach the mucosa. Complete intramural growth of an advanced primary ESCC is an exceedingly rare presentation, with only six cases reported in the literature thus far[2-7]. We herein report a case of primary ESCC with complete intramural invasion that endoscopically mimics a submucosal lesion. The diagnosis could only be established by an endoscopic ultrasound (EUS)-guided biopsy. This article was published after obtaining informed consent from the patient.
A 50 year old male presented with a progressive mechanical type of dysphagia for a month, which was associated with a significant loss of weight.
There was an occasional history of regurgitation present. He denies loss of appetite, retrosternal chest pain or discomfort. He also denies any history of heartburn, caustic ingestion, fever, cough, haemoptysis, change in voice, difficulty in breathing, hematemesis, melena or any drug intake.
Past history was significant for squamous cell carcinoma of the tongue, which was treated with surgery and chemoradiation 1 year prior. He lost follow up for the above. He quit smoking and alcohol after being diagnosed with tongue carcinoma.
Upon examination, his vitals were stable and there was no significant lym-phadenopathy. Oral examination was significant for a scar on the left lateral border of the tongue. His respiratory and gastrointestinal system examination was unremarkable.
He was further investigated. The basic metabolic panel was normal.
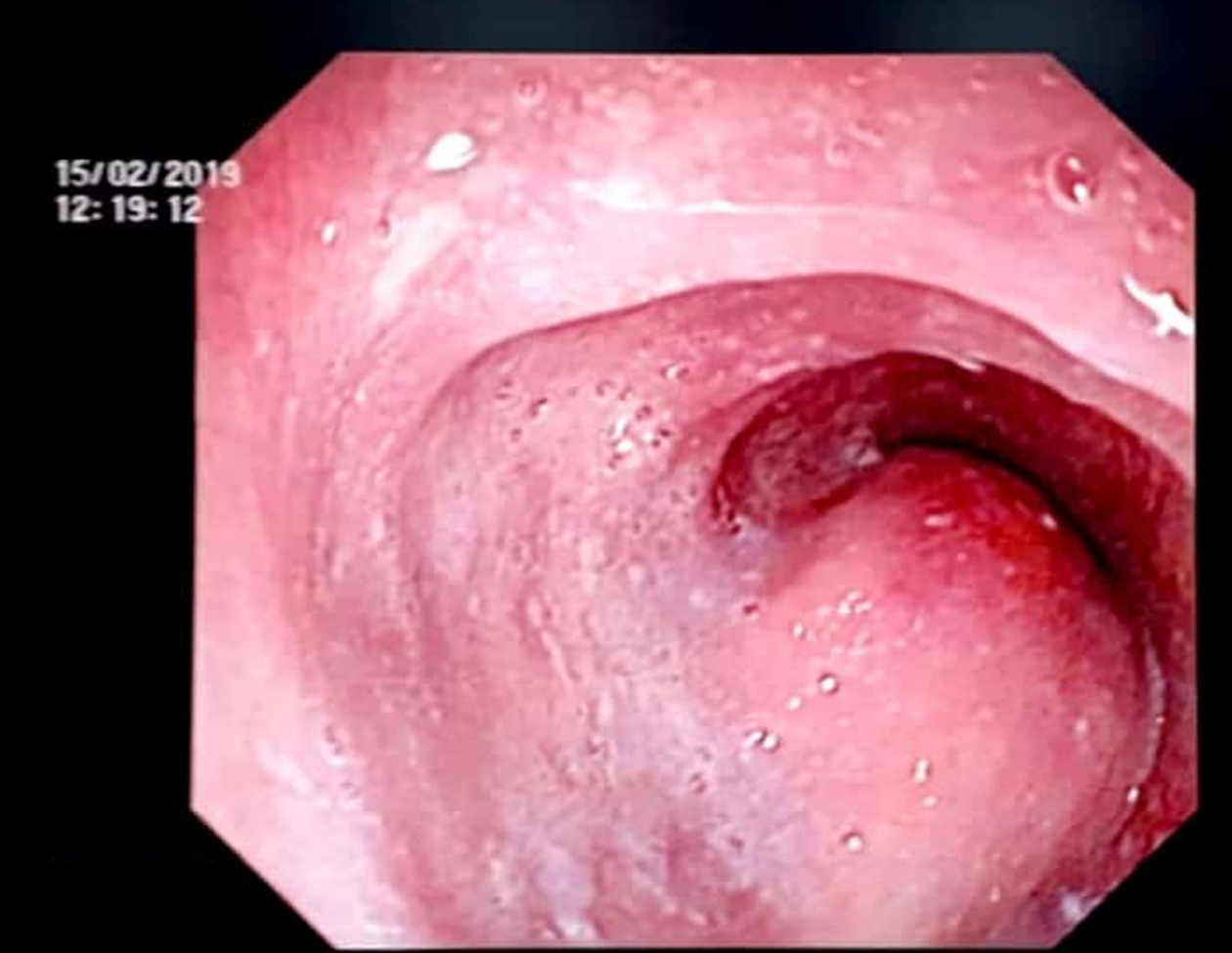
Upper gastrointestinal endoscopy was performed, which revealed a large, hemispherical lesion with a normal-appearing overlying mucosa about 4 cm × 5 cm in size and extending from 30-34 cm from the incisors, as shown in Figure 1. That impression was that is was possibly a submucosal lesion of the distal oesophagus. Endoscopic biopsy was not done, and further evaluation of the lesion was planned using EUS.
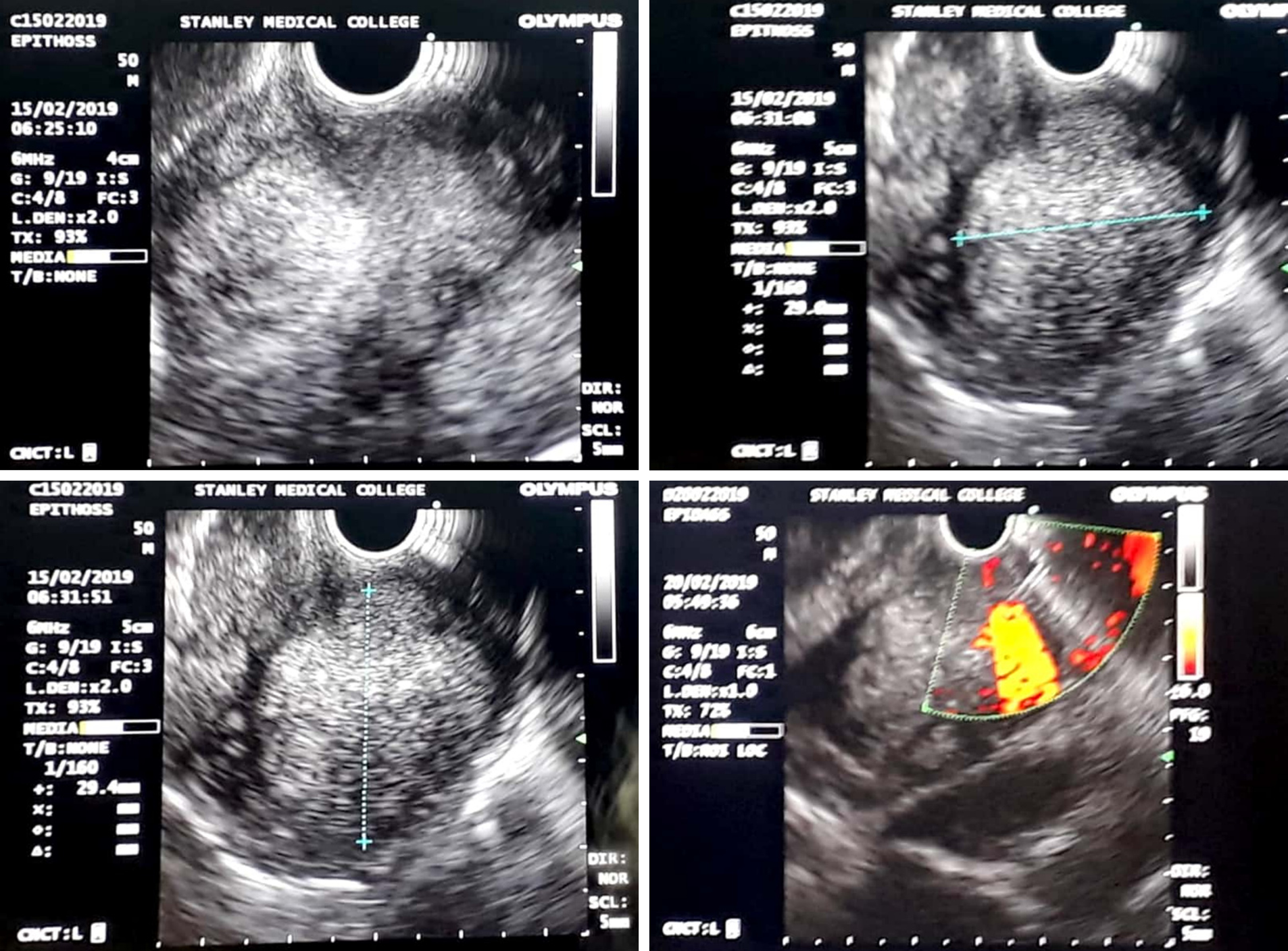
EUS was done using the linear echoendoscope model MAJ1597 (EUS scope, Olympus, Tokyo, Japan). EUS showed a large hyperechoic lesion arising from the third layer at 30 cm, as shown in Figure 2, with a provisional diagnosis of lipoma.
However, in view of the patient’s past history of malignancy, a fine needle biopsy was done using a 19-gauge Boston scientific acquired EUS fine needle biopsy device, and sent for histopathologic examination.
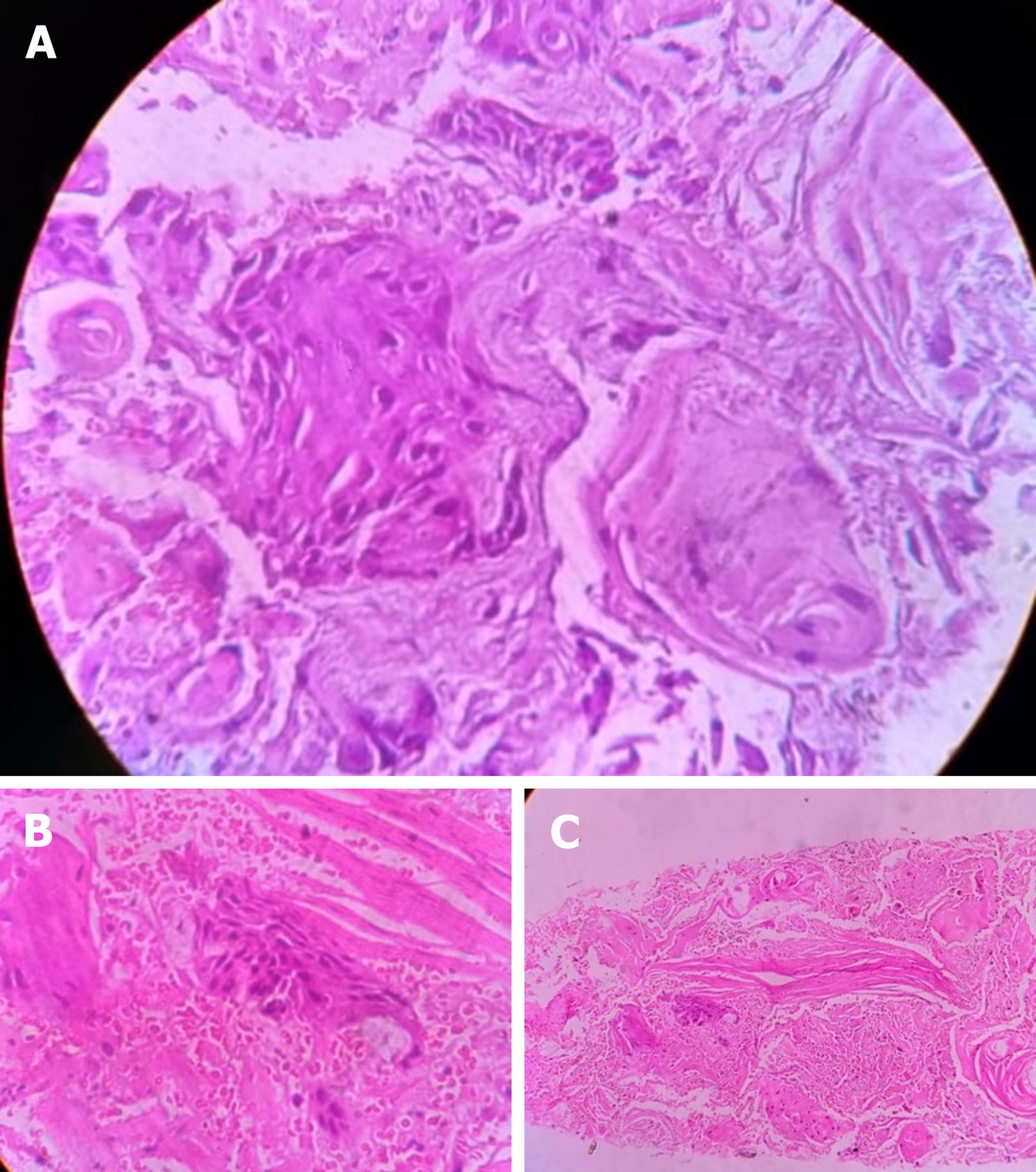
Histopathology revealed fragments of malignant neoplasm composed of cells arranged in sheets, as in Figure 3. The neoplastic cells were round to polygonal, with moderate amounts of eosinophilic cytoplasm with moderate nuclear atypia. Keratin pearl formation was abundant. Histopathology was reported as well-differentiated squamous cell carcinoma. Immunohistochemistry confirmed the same.
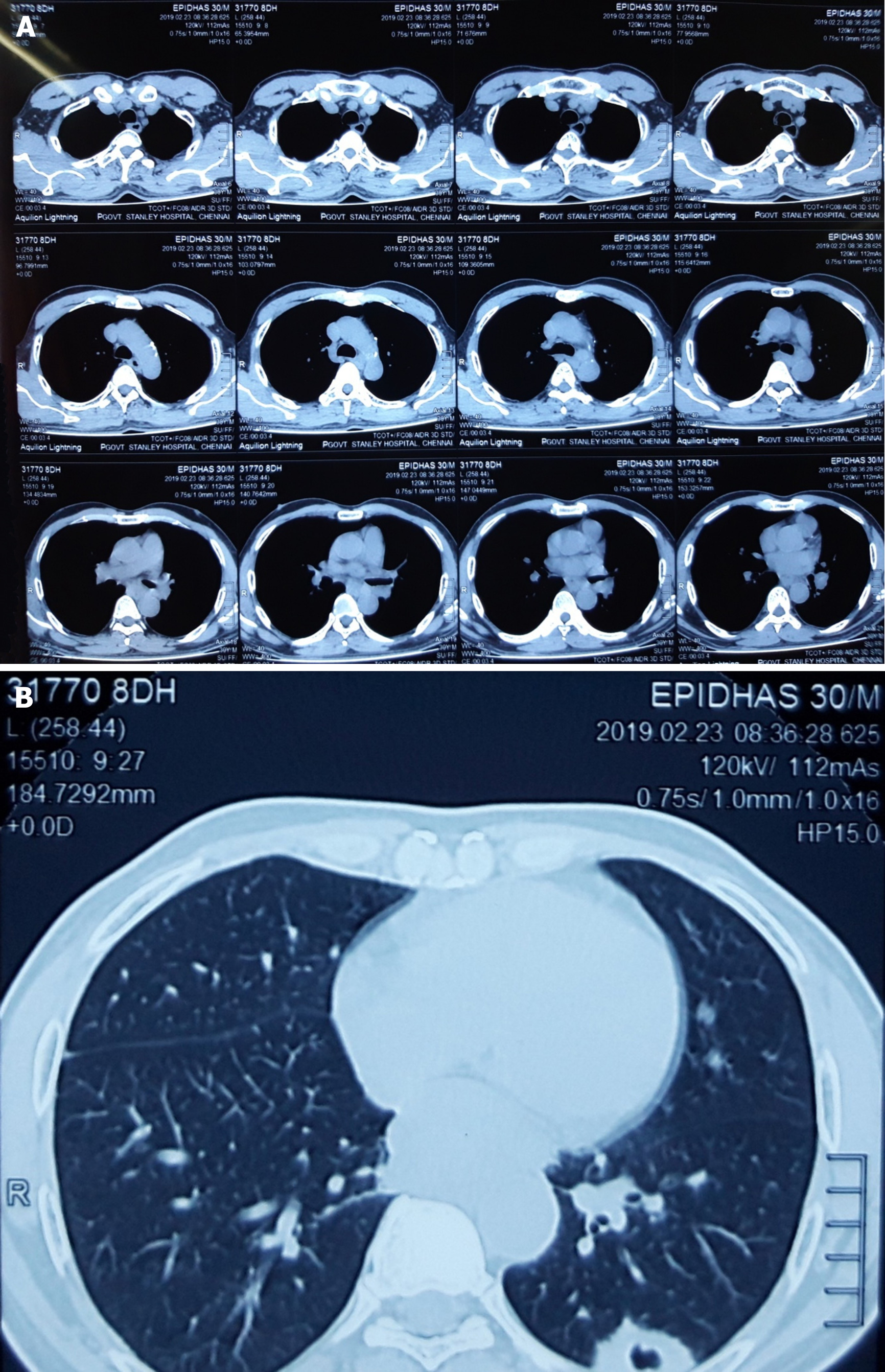
Computed tomography (CT) on the thorax was then performed. CT of the thorax with IV and oral contrast showed heterogeneously enhancing soft tissue thickening noted in the retro cardiac oesophagus, with a thickness measuring 38 mm and a length of 68 mm, with proximal oesophageal dilatation noted. The OG junction was normal. The lesion has contact with the descending thoracic aorta at about 90°. The loss of flat plane was noted between the lesion and left atrium. Cavitatory metastatic nodules measuring 26 mm × 18 mm × 33 mm were noted in the posterior basal segment of the left lower lobe. Bilateral hilar nodes were noted, as shown in Figure 4. The CT of the thorax was finally reported as a Retro cardiac oesophageal growth with lung metastasis.
Oesophageal squamous cell carcinoma stage 4.
The patient is currently receiving palliative care.
Not available.
The history of intramural ESCC dates back to a case report from McGregor et al[4], wherein a case of squamous cell carcinoma was found to arise from an oesophageal intramural squamous epithelial cyst. There were reports of oesophageal benign cysts as well as carcinoma arising from oesophageal diverticulum. However, for the first time, they reported a case of ESCC arising from an oesophageal cyst. In their case, esophagoscopy revealed a stricture upper oesophagus, and repeat biopsies only revealed mucosal hyperplasia. However, the patient was started on chemoradiation, but he later succumbed to bronchopneumonia. Autopsy demonstrated a 1.5-cm long intramural oesophageal squamous epithelial cyst, from which arose a locally invasive squamous cell carcinoma, without mucosal involvement or metastases. There are several other rare case reports of advanced primary ESCC masquerading as a completely intramural growth.
For this case report, we reviewed the literature, which elucidated the role of EUS in the evaluation of oesophageal submucosal lesions. We could find only two such cases where EUS diagnosis of a submucosal lesion was made, which upon further investigation turned out to be intramural ESCC. One such study was by Choudhary et al[2], where ESCC presented as a submucosal lesion with repeatedly negative endoscopic biopsies. The patient underwent EUS, and fine‑needle aspiration was done. The cytopathological report was suggestive of squamous cell carcinoma. There were no distant metastases in this case. The second case report was from Sonthalia et al[3]. In their report, EUS revealed a heteroechoic solid mass originating from the muscularis propria of the distal oesophagus. Cytological study of EUS-guided fine needle aspiration from the mass was suggestive of squamous cell carcinoma, which was confirmed upon immunohistochemistry. However, this case had bone metastasis. Also, there are certain limitations in EUS-guided fine needle aspiration cytology (FNAC) for the diagnosis of submucosal tumours, as the average diagnostic accuracy rate of EUS-FNA is 60–80%[3].
Compared to the above case reports, our case differs in that our patient had a past history of malignancy. In addition, an EUS fine needle biopsy was done for the evaluation of a submucosal lesion in the oesophagus, which has not been done in the past.
Gibiino et al[8] have also advocated that EUS fine-needle biopsy has high diagnostic accuracy, and is expected to move the practice of EUS from cytology to histology. This should thereby expand the utilization of EUS throughout the world, and facilitate targeted therapies as well as the monitoring of treatment response in a more biologically-driven manner.
This case report highlights that intramural ESCC may look like a submucosal lesion in endoscopy, and that EUS biopsy is therefore needed for final diagnosis.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Musella M S-Editor: Wang JL L-Editor: Filipodia E-Editor: Zhang YL
| 1. | Samarasam I. Esophageal cancer in India: Current status and future perspectives. Int J Adv Med Health Res. 2017;4:5‑10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Choudhary NS, Bansal RK, Puri R, Guleria M, Sud R. Esophageal squamous cell carcinoma presenting as submucosal lesion with repeatedly negative endoscopic biopsies. J Dig Endosc. 2016;7:153-154. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Sonthalia N, Jain SS, Surude RG, Pawar VB, Udgirkar S, Rathi PM. Primary Esophageal Intramural Squamous Cell Carcinoma Masquerading as a Submucosal Tumor: A Rare Presentation of a Common Disease. Clin Med Insights Gastroenterol. 2016;9:63-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | McGregor DH, Mills G, Boudet RA. Intramural squamous cell carcinoma of the esophagus. Cancer. 1976;37:1556-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | von Rahden BH, Brücher BL, Sarbia M. Esophageal squamous cell carcinoma with entirely intramural growth pattern. Virchows Arch. 2006;448:862-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Kishino T, Yamaguchi Y, Yamagishi T, Hashimoto T, Kyomasu Y, Mori H, Sugiyama M, Atomi Y, Saito S, Ishida H, Takahashi S. Submucosal tumor (SMT)-like esophageal squamous cell carcinoma with gastric metastasis. Hepatogastroenterology. 2000;47:1581-1584. [PubMed] |
| 7. | Schmitz KJ, König C, Riesener KP. Intramural carcinoma of the oesophagogastric junction. BMJ Case Rep. 2012;2012:bcr0320126080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Gibiino G, Larghi A. EUS-guided fine-needle biopsy for histological examination: Is it time to change our sampling technique? Endosc Ultrasound. 2018;7:71-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |