Published online Dec 16, 2018. doi: 10.4253/wjge.v10.i12.400
Peer-review started: July 27, 2018
First decision: August 20, 2018
Revised: August 31, 2018
Accepted: November 15, 2018
Article in press: November 15, 2018
Published online: December 16, 2018
Processing time: 149 Days and 2.9 Hours
To compare the diagnostic accuracy of video capsule endoscopy (VCE) and double-balloon enteroscopy (DBE) in cases of obscure gastrointestinal bleeding (OGIB) of vascular origin.
MEDLINE (via PubMed), LILACS (via BVS) and Cochrane/CENTRAL virtual databases were searched for studies dated before 2017. We identified prospective and retrospective studies, including observational, cohort, single-blinded and multicenter studies, comparing VCE and DBE for the diagnosis of OGIB, and data of all the vascular sources of bleeding were collected. All patients were subjected to the same gold standard method. Relevant data were then extracted from each included study using a standardized extraction form. We calculated study variables (sensitivity, specificity, prevalence, positive and negative predictive values and accuracy) and performed a meta-analysis using Meta-Disc software.
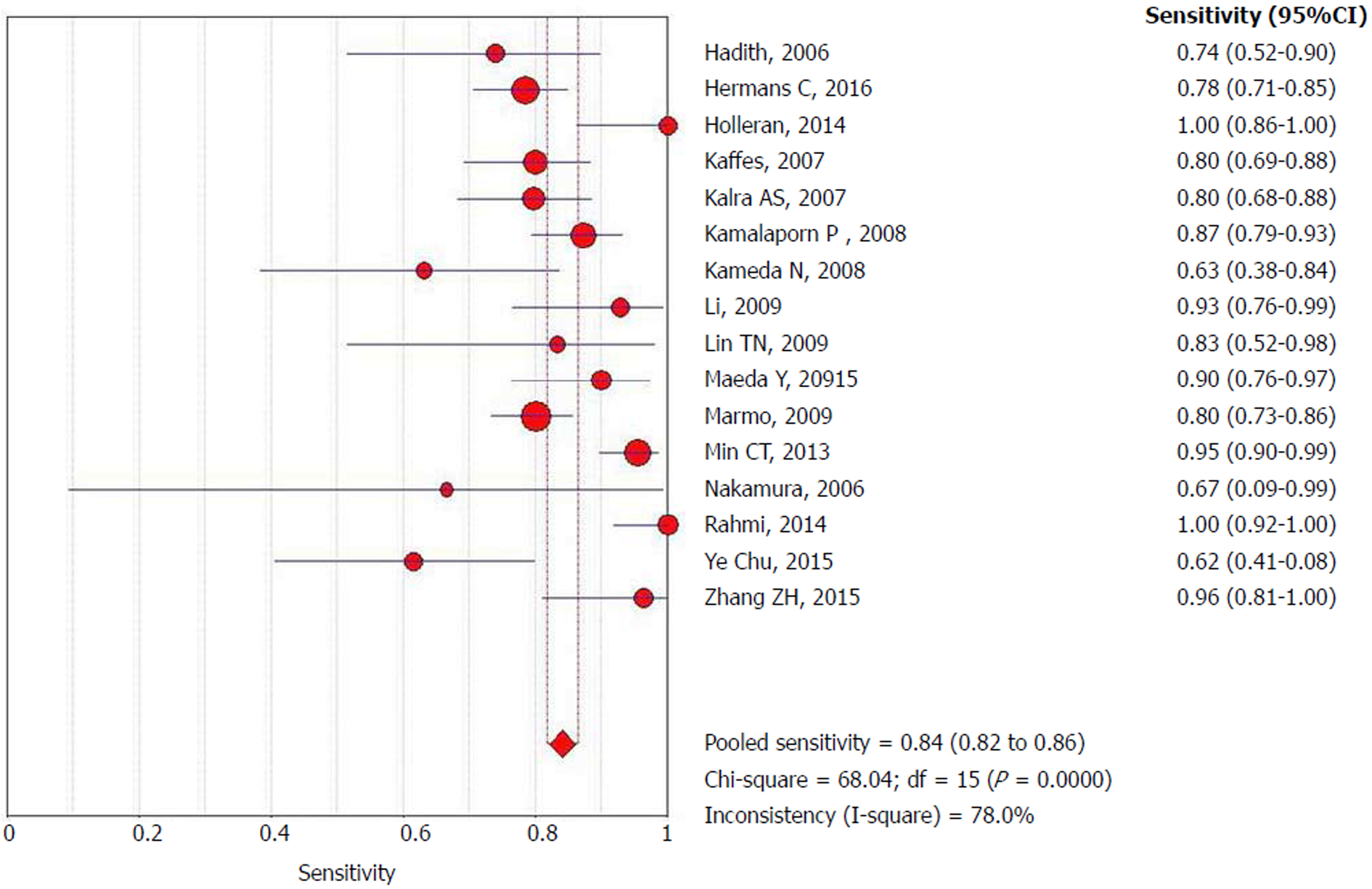
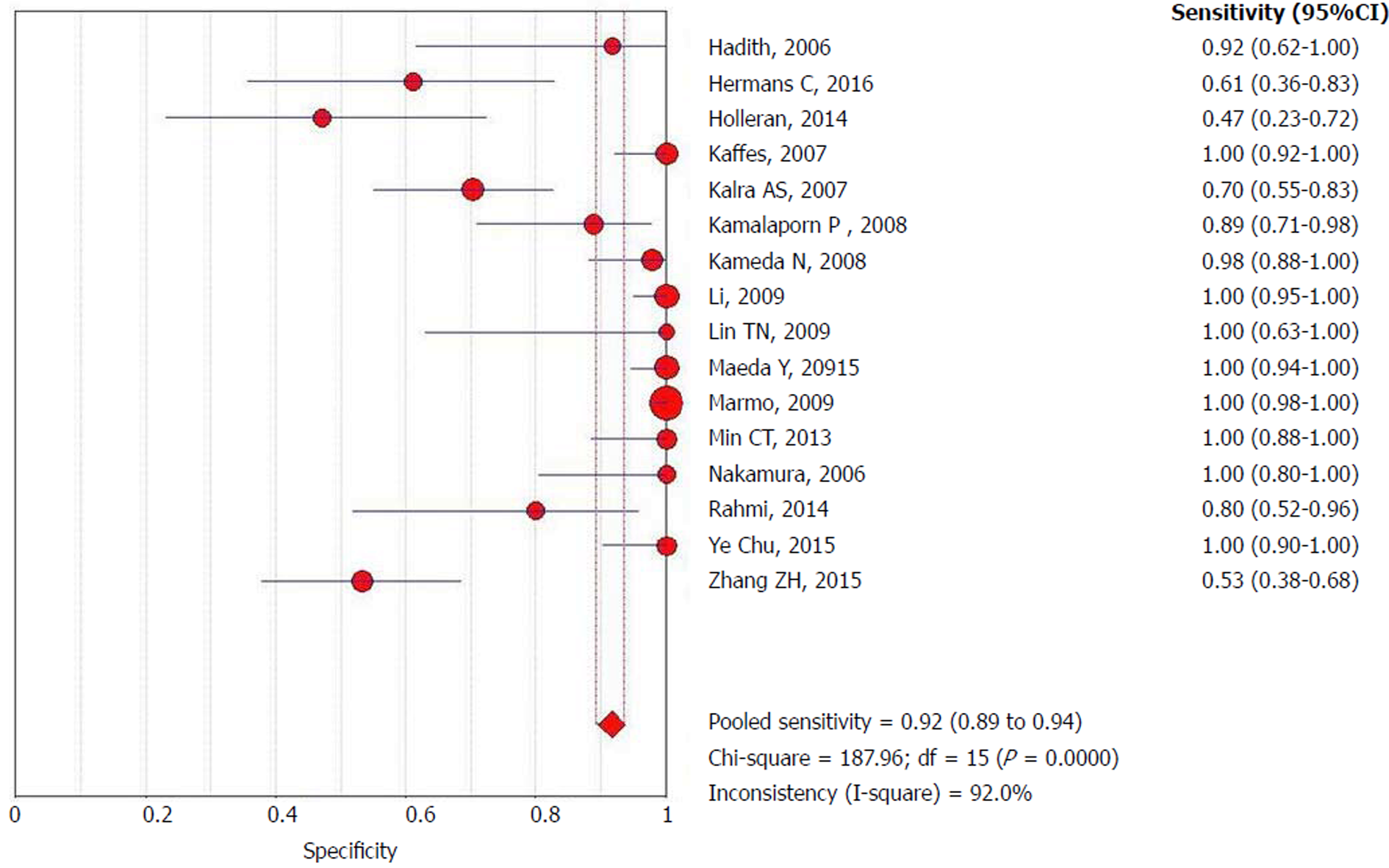
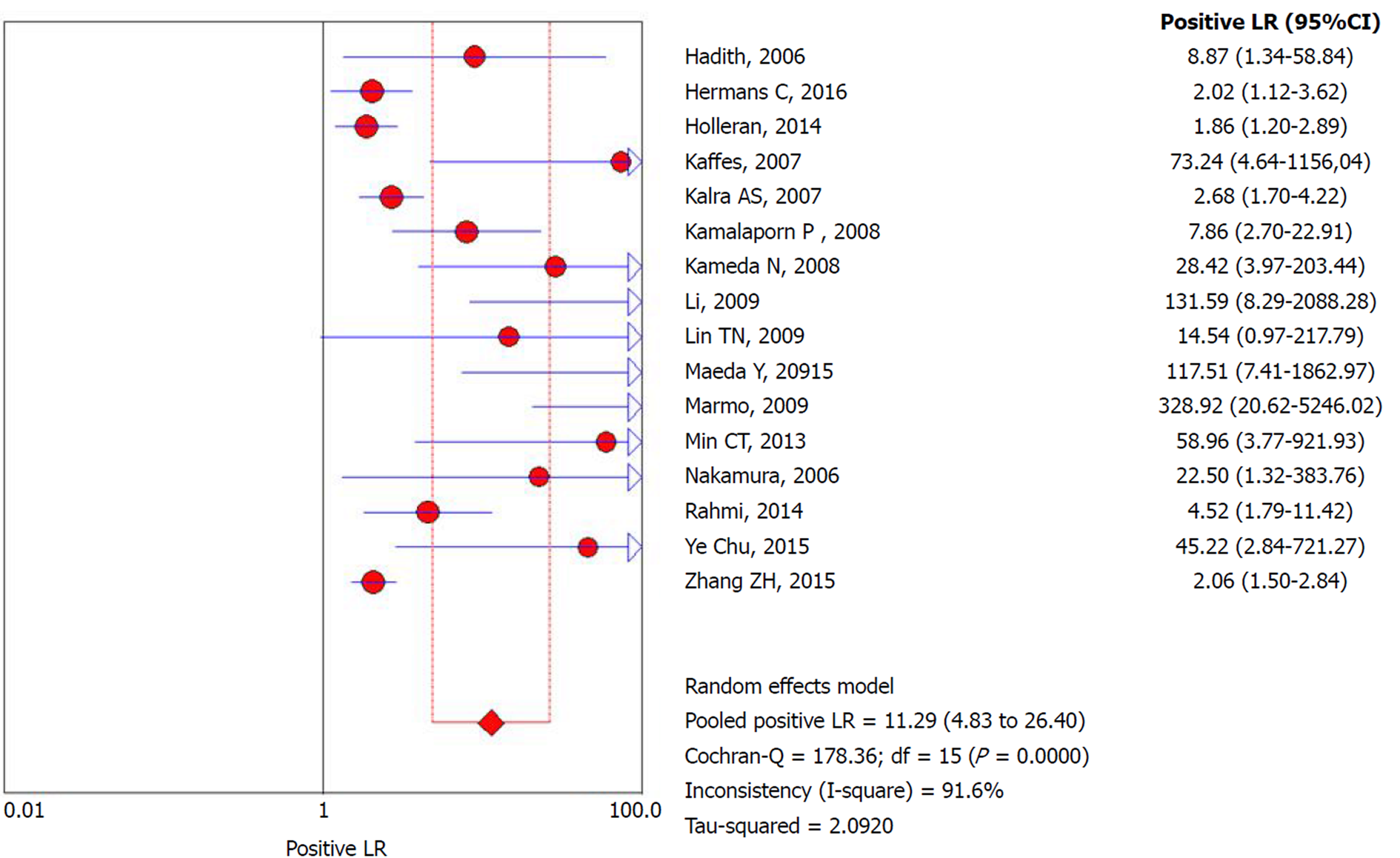
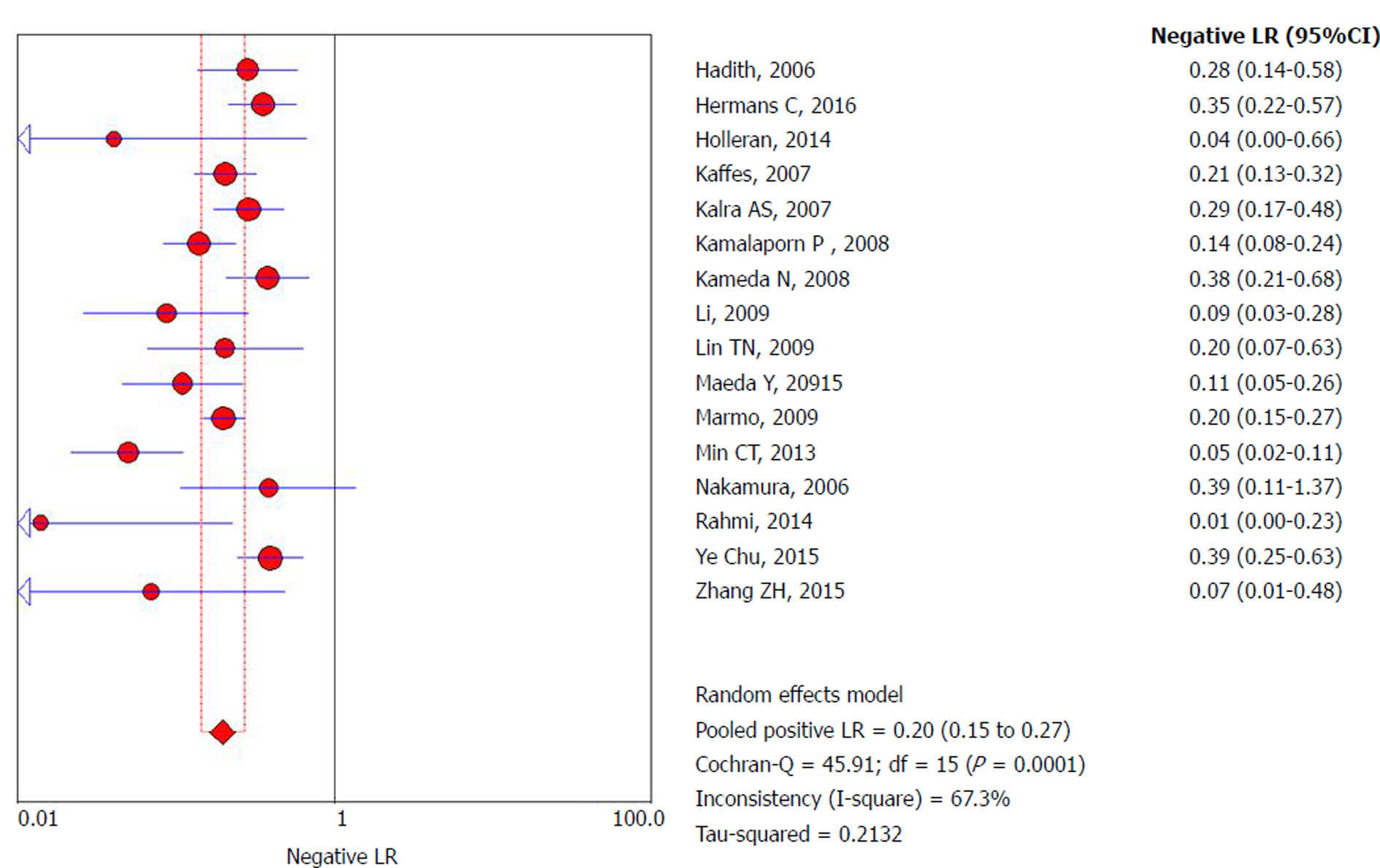
In the per-patient analysis, 17 studies (1477 lesions) were included. We identified 3150 exams (1722 VCE and 1428 DBE) in 2043 patients and identified 2248 sources of bleeding, 1467 of which were from vascular lesions. Of these lesions, 864 (58.5%) were diagnosed by VCE, and 613 (41.5%) were diagnosed by DBE. The pretest probability for bleeding of vascular origin was 54.34%. The sensitivity of DBE was 84% (95%CI: 0.82-0.86; heterogeneity: 78.00%), and the specificity was 92% (95%CI: 0.89-0.94; heterogeneity: 92.0%). For DBE, the positive likelihood ratio was 11.29 (95%CI: 4.83-26.40; heterogeneity: 91.6%), and the negative likelihood ratio was 0.20 (95%CI: 0.15-0.27; heterogeneity: 67.3%). Performing DBE after CE increased the diagnostic yield of vascular lesion by 7%, from 83% to 90%.
The diagnostic accuracy of detecting small bowel bleeding from a vascular source is increased with the use of an isolated video capsule endoscope compared with isolated DBE. However, concomitant use increases the detection rate of the bleeding source.
Core tip: We performed a systematic review and meta-analysis comparing the diagnostic accuracy of video capsule endoscopy and double-balloon enteroscopy (DBE) in cases of obscure gastrointestinal bleeding of vascular origin. This is the first systematic review in this setting. We observed that the diagnostic accuracy of detecting small bowel bleeding from a vascular source is increased with the use of an isolated video capsule endoscope compared with isolated DBE. However, concomitant use increases the detection rate of the bleeding source.
- Citation: Brito HP, Ribeiro IB, de Moura DTH, Bernardo WM, Chaves DM, Kuga R, Maahs ED, Ishida RK, de Moura ETH, de Moura EGH. Video capsule endoscopy vs double-balloon enteroscopy in the diagnosis of small bowel bleeding: A systematic review and meta-analysis. World J Gastrointest Endosc 2018; 10(12): 400-421
- URL: https://www.wjgnet.com/1948-5190/full/v10/i12/400.htm
- DOI: https://dx.doi.org/10.4253/wjge.v10.i12.400
Approximately 5% of gastrointestinal bleeding occurs between the ligament of Treitz and the ileocecal valve[1-3] and can be classified as occult when there is no overt bleeding or overt bleeding with melena or hematochezia. Obscure gastrointestinal bleeding (OGIB) includes both definitions[1,2,4].
The most common sources of OGIB in older patients are small bowel angioectasias (30% to 40%), whereas tumors (17%) are more frequent in patients under 50 years old[5,6]. Other causes include Meckel’s diverticula, radiation enteropathy, Dieulafoy’s lesions, small-bowel varices, nonsteroidal anti-inflammatory drug enteropathy and inflammatory bowel disease[7-10].
Although prior evaluation of proximal and distal parts of small bowel with upper and lower endoscopy is recommended, it is occasionally not possible to identify the bleeding source with these methods. In these cases, newer endoscopic evaluation techniques are recommended, such as video capsule endoscope (VCE) and deep enteroscopy [which encompasses spiral, single, and double-balloon enteroscopy (DBE)].
The advent of VCE in 1998 enabled direct and painless visualization of small-bowel mucosa[4,11]. DBE, which has been on the market since 2003, allows for the endoscopic scrutiny of the entire small intestine, but it has the disadvantage of being an invasive procedure.
The diagnostic and therapeutic yield of these technologies has been compared with conventional approaches of push enteroscopy (PE), intraoperative enteroscopy and radiologic methods, revealing greater diagnostic yield[12]. Few studies comparing the diagnostic success of VCE and DBE are inconclusive in determining which of these two methods is superior. Thus, we decided to compare these methods in this review.
Although numerous meta-analyses have compared the efficacy of VCE and DBE in detecting an OGIB, this is the first systematic review and meta-analysis comparing OGIBs specifically in vascular origins. The objective of this study is to compare the diagnostic accuracy of VCE and DBE in cases of OGIB of vascular origin.
This systematic review was performed in accordance with the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) recommendations and registered on PROSPERO international database (http://www.crd.york.ac.uk/prospero/) under number CRD42017078046.
Types of studies: transversal studies from which it was possible to extract information necessary to calculate using only directly or indirectly supplied data. No abstracts or data from unpublished research were accepted. There were no restrictions in terms of language or date of publication.
Types of participants: patients with overt or occult OGIB from a vascular source. There were no restrictions regarding sex, age, risk factors, or anemia level in the study participants.
Types of interventions: VCE and DBE. Only studies that completed both exams, i.e., VCE followed by DBE, were included regardless of where the procedure was performed, the type of colon cleaning, and the brand of the capsule or enteroscope.
Outcome measures: the main outcomes were sensitivity, specificity, pretest and posttest probabilities, positive and negative predictive values, and the accuracy of DBE.
To identify articles, searches were conducted using MEDLINE (via PubMed), LILACS (via BVS) and Cochrane/CENTRAL virtual databases. Databases were searched from March 2017 to April 2018 with no restriction regard the idiom or the year of publication.
The search used varied strategies depending on the database, and these strategies are specified below: (A) PubMed/MEDLINE: (angiodysplasias OR arteriovenous OR malformation OR hemorrhage OR gastrointestinal OR hemorrhages OR hematochezia OR angioectasia OR intestines OR small bowel bleeding OR intestine OR duodenum OR duodenal OR jejunum OR jejunal OR ileum OR ileal OR bleeding OR intestinal OR occult OR obscure phlebectasias) AND (double balloon OR enteroscopy OR enteroscopes OR enteroscopies OR double balloon endoscopy OR capsule endoscopy OR capsule endoscope OR full enteroscopy OR deep enteroscopy) AND (diagnosis/broad[filter]); and (B) LILACS and Cochrane/CENTRAL: enteroscopy AND capsule endoscopy AND obscure bleeding.
Articles were initially selected after an assessment of the titles and abstracts to assess the relevance of the full text. Then, abstracts were read, and those that did not fit the inclusion criteria were excluded. Two independent reviewers performed eligibility assessment and study selection. Disagreements between reviewers were resolved by consensus.
The method of data extraction from each included study consisted of completing information sheets after the paper was read. Relevant data were then extracted from each included study using a standardized extraction form. One review author extracted data from the included studies, and a second author checked the extracted data. Disagreements were resolved by discussion between the two review authors.
The selected data included age, gender, total number of patients, study design, VCE and DBE models, intestinal preparation, interval time between VCE and DBE, number of patients with diagnoses of small-bowel bleeding using VCE and DBE and number of vascular lesions found. Only bleeding from vascular lesions was considered true positive diagnostically. We classified “vascular lesions” as angiodysplasias, varices, hemangiomas, red spots, and Dieulafoy lesions. Bleeding from tumor, ulcer, erosions, polyps and masses were not classified as vascular lesions but were considered bleeding from alternative sources.
To evaluate the risk of bias and the applicability of primary diagnostic accuracy studies, we used the QUADAS-2 tool (Table 1), which is structured in four domains. The first domain is patient selection, which we described in terms of risk of bias. The second domain is a description of the index test, including analysis of how it was conducted and interpreted. The third domain is the reference standard, namely its description, conduction and interpretation. The fourth domain is flow and timing, where we recorded any patient who did not receive the index test(s) and/or reference standard, patients who were excluded from the analysis, and the time interval or any interventions that occurred between the index test(s) and the reference standard.
| Study | Hadithi et al, 2006[4] | Hermans et al, 2017[11] | Holleran et al, 2014[37] | Kaffes et al, 2007[34] | Kalra et al, 2015[16] | Kamalapor et al, 2008[30] | Kameda et al, 2008[27] | Li et al, 2010[35] | Lin et al, 2007[40] | Maeda et al, 2015[32] | Marmo et al, 2009[23] | TianMin, et al, 2013[39] | Nakamura et al, 2006[29] | Rahmi et al, 2013[33] | Chu et al, 2016[17] | Zhang, et al, 2015[15] |
| Was a consecutive or random sample of patients enrolled? | YES | UNCLEAR | UNCLEAR | YES | UNCLEAR | UNCLEAR | YES | YES | YES | YES | YES | YES | YES | YES | YES | UNCLEAR |
| Was a case-control design avoided? | YES | YES | NO | YES | YES | NO | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| Did the study avoid inappropriate exclusions? | YES | YES | YES | YES | UNCLEAR | NO | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO |
| Could the selection of patients have introduced bias? | LOW | MODERATE | HIGHT | LOW | HIGH | HIGH | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | HIGH |
| Are there concerns that the included patients do not match the review question? | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | HIGH |
| Were the index test results interpreted without knowledge of the results of the reference standard? | YES | NO | YES | NO | YES | NO | YES | UNCLEAR | UNCLEAR | UNCLEAR | YES | NO | YES | NO | NO | UNCLEAR |
| If a threshold was used, was it prespecified? Could the conduct or interpretation of the index test have introduced bias? | YES LOW | YES MODERATE | YES LOW | YES MODERATE | NO MODERATE | YES MODERATE | YES LOW | YES MODERATE | NO MODERATE | YES MODERATE | YES LOW | NO HIGH | YES LOW | YES MODERATE | YES MODERATE | YES MODERATE |
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | HIGH |
| Is the reference standard likely to correctly classify the target condition? | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | UNCLEAR |
| Were the reference standard results interpreted without knowledge of the results of the index test? | YES | NO | YES | NO | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | UNCLEAR |
| Could the reference standard, its conduct, or its interpretation have introduced bias? | LOW | MODERATE | LOW | MODERATE | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | HIGH | HIGH |
| Are there concerns that the target condition as defined by the reference standard does not match the review question? | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | LOW | HIGH | HIGH |
| Was there an appropriate interval between index test(s) and reference standard? | YES | NO | NO | NO | NO | NO | YES | YES | YES | YES | YES | YES | YES | NO | YES | UNCLEAR |
| Did all patients receive a reference standard? | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| Did all patients receive the same reference standard? | NO | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| Were all patients included in the analysis? | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| Could the patient flow have introduced bias? | MODERATE | LOW | LOW | LOW | LOW | MODERATE | LOW | LOW | LOW | LOW | LOW | LOW | LOW | MODERATE | LOW | LOW |
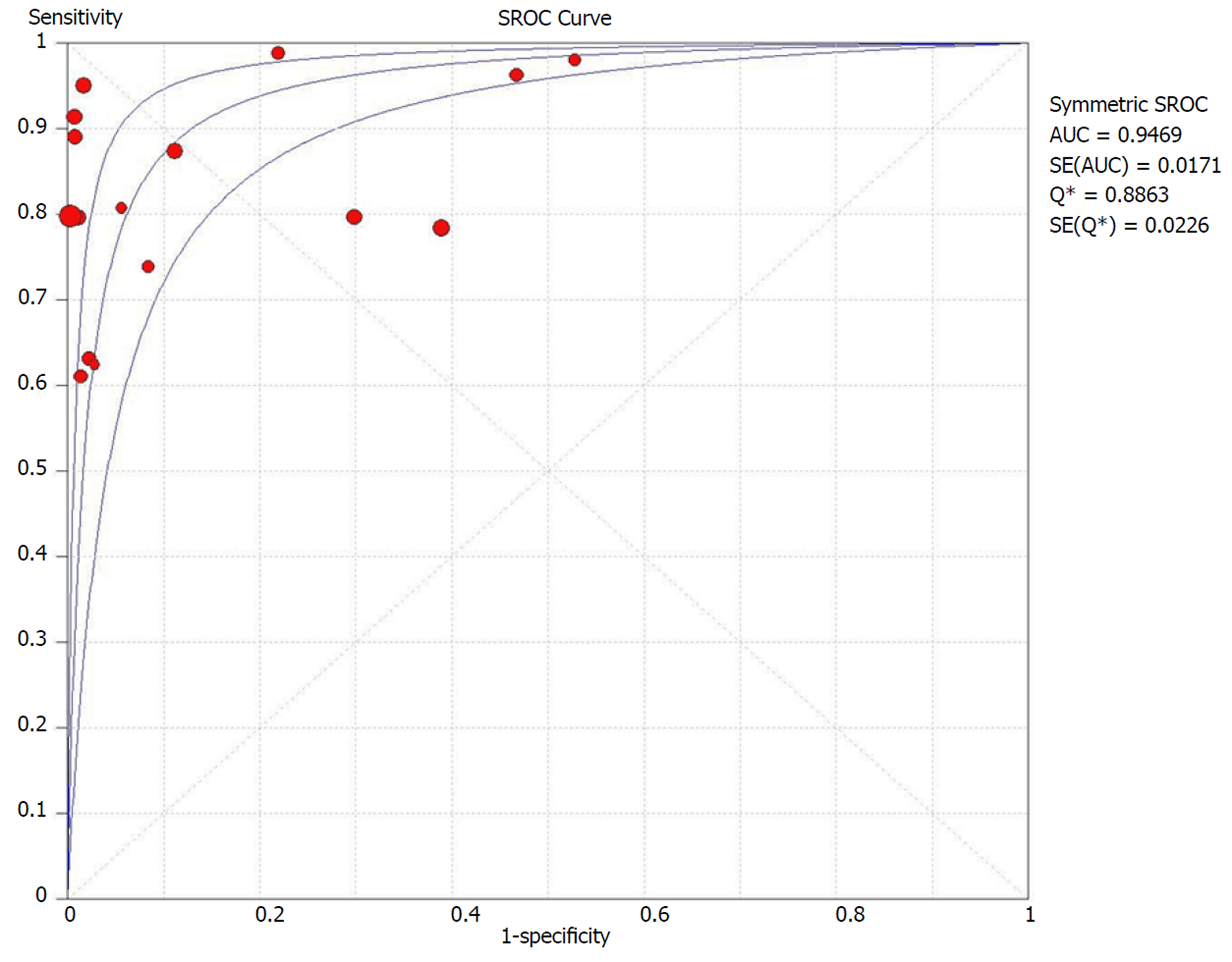
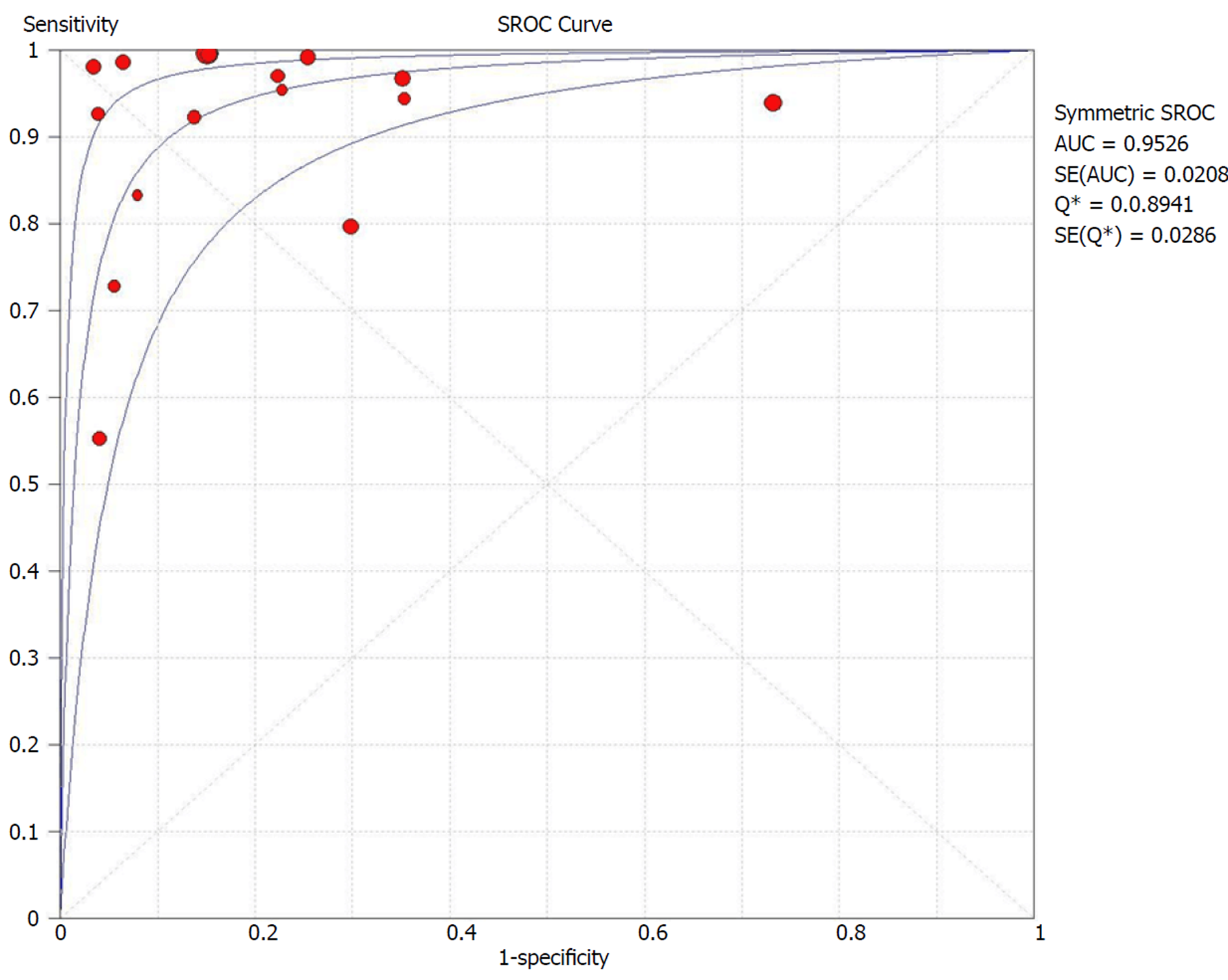
The sensitivity, specificity, pretest probability, positive and negative predictive values, and accuracy of DBE were the primary outcome measures and calculated using data provided from the original papers. Analysis was performed using capsule endoscopy as the gold standard for detection of small bowel lesions. We also created a summary receiver operating characteristic curve (sROC). All of these variables were subjected to per-lesion analyses. I-square was used to evaluate heterogeneity. Studies that remained under 50% of the sROC curve were removed.
Data were organized, and averages and standard deviations were calculated using Microsoft Excel Software 2013. Analysis was performed using the Meta-Disc 1.4 software.
In the per-patient analysis, 17 studies (1477 lesions) were included (Figure 1). In 3150 exams (1722 VCE and 1428 DBE) performed in 2043 patients, 2248 sources of bleeding were identified, of which 1467 were found to be vascular lesions and 781 were related to other sources, including tumor, ulcer, erosions, polyps and mass. Eight hundred and sixty-four (58.5%) lesions were diagnosed by VCE, and 613 (41.5%) by DBE. Of these, 605 (40.9%) were angiodysplasia; 5 (0.33%) were varices; 160 (10.8%) were described as blood and clots/bleeding, active bleeding or bleeding; 11 (0.74%) were red spots; 45 (3.04%) were described as arteriovenous malformation; 10 (0.67%) Dieulafoy lesions; 7 (0.47%) angiomas; and 74 (5.01%) were described generically as vascular lesions. Some patients were subjected to the same exam twice, and some of the sources of bleeding were identified by both exams.
The sensitivity of DBE was 84% [95% confidence interval (CI): 0.82-0.86; heterogeneity: 78.00%] (Figure 2), and the specificity was 92% (95%CI: 0.89-0.94; heterogeneity: 92.0%) (Figure 3). The positive likelihood ratio was 11.29 (95%CI: 4.83-26.40; heterogeneity: 91.6%) (Figure 4), and the negative likelihood ratio was 0.20 (95%CI: 0.15-0.27; heterogeneity: 67.3%) (Figure 5).
The posttest probability was 41.6% for DBE in the studied population and 85% for VCE. The area under the sROC curve was 0.9469 for DBE (Figure 6) and 0.9526 for VCE (Figure 7). The difference between the areas under independent ROC curves was 0.006, and the P-value was 0.41 (two-tailed).
Performing DBE after CE increased the diagnostic yield to vascular lesion by 7% from 83% to 90%
Information extracted from each paper included characteristics of trial participants (including age, gender), study design, VCE and DBE models, intestinal preparation, interval time between VCE and DBE, number of patients with diagnoses of small-bowel bleeding using VCE and DBE, number of vascular lesions found, and the source of obscure gastrointestinal bleeding (Table 2).
| Median age; range | Patient total | Study design | VCE Model | DBE Model | Preparation | Interval CE × DBE | No. of patients with diagnoses of SBB by CE/total CE performed | No. of patients with diagnoses of SBB by DBE/total DBE performed | |
| Fujimoto et al[28], 2007 | 64 (38-93) | 45 M: 25 F: 20 | Prospective study | Pillcam (Given Imaging, Yoqneam, Israel). | EN-450P5 DBE diagnostic model and/or the EN-450T5 | CE: 12 h fast + 1 L sodium sulfate/sodium bicarbonate DBE: 72 h after CE in 36 pct | 72 h | 18/45 Angiodysplasia: 6 Varices: 2 jejunal | 18/36 |
| Hadithi et al[4], 2006 | 63.2 (19-86) | 35 M:22 F: 13 | Prospective blinded study | Given M2A, Given Imaging Ltd., Yoqneam, Israel | Fuji Photo Optical Incorporated Company Fujinon Inc., Japan | CE: fast overnight after the ingestion of 1 L of sodium sulfate/sodium bicarbonate solution DBE: fast overnight after ingestion of 1 L clean prep. for the antegrade approach and bowel cleansing as for colonoscopy (4 L Klean prep) | 7 to 14 d | 21/35 AVM: 19 Fresh blood and clots: 5 | 28/35 AVM: 16 Fresh blood and clots: 2 |
| Hermans et al[11], 2017 | 69 (18-91) | 146 M: 91 F: 55 | Retrospective observational study. | Olympus VC (Olympus EndoCapsule; Tokyo, Japan) and Pillcam VC (Covidien plc, Dublin, Ireland) | Fujinon Double-Balloon Enteroscopy System (Fujinon GMBH, Germany), EN-450T5 | CE: 2 L PEG in a single or split dose DBE: 1 L PEG divided into two doses to be used twice | 111 (1–1091) days | 105/134 Angiodysplasias: 70 active bleedings without visible focus : 35 | 93/146 Angiodysplasias: 19 |
| Holleran et al[37], 2013 | 54 (16-90) | 246 M: 130 F: 116 | Retrospective comparative study | SB1 or SB2 pillcam (Given imaging, Yokneam, Israel) | Fujinon double-balloon enteroscope (EN-450P5/20, Fujinon, Inc., Saitama, Japan) | CE: No preparation was required other than an overnight fast. Anterograde DBE: overnight fast Retrograde DBE: PEG the day prior | NR* | 40/46 Angiodysplasia: 10 Active bleeding: 3 | 116/246 Angiodysplasias: 44 |
| Kaffes et al[34], 2007 | 62 ± 18 | 60 | Prospective cohort study | M2A; Given Imaging Ltd, Yoqneam, Israel) | Fujinon | CE, DBE: fasting period of 8 h before the oral procedure and a bowel preparation with a sodium (Picoprep; Pharmatel, Thornleigh, Australia) | NR* | 45/60 Angiectasia:28 Red spots: 9 Blood: 8 | 45/60 Angioectasia: 21 Red spots: 9 Blood: 8 |
| Kalra, A et al[16], 2015 | 66.6 ± 13.2 | 116 M:65 F: 51 | Retrospective review | Medtronic, Duluth, GA, the United States | Fujifilm Medical System, Stanford, CT, the United States | Retrograde DBE: bowel preparation the night before the procedure. | 1 yr | /69 | 29/69 AVM: 29 |
| Kamalaporn et al[30], 2008 | 64.1 (34-83) | 195 M: 26 F:25 | Retrospective review | Given M2A CE system (Given Imaging Ltd, Israel) | Fujinon DBE system (Fuji Photo Optical Incorporated Company, Fujinon Inc., Japan) | CE: 2 to 4 L PEG and fasted overnight, at least 8 h before the procedure DBE: 4 L PEG and fasted overnight | 139 (40 to 335) d | 181/202 studies Angiodysplasia: 33 Bleeding: 22 | 56/56 Angiodysplasia: 36 Bleeding: 9 |
| Kameda et al[27], 2008 | 62.4 (27-84) | 32 M: 13 F: 19 | Prospective single-blind trial | Pill Cam capsule (M2A, Given Imaging, Yoqneam, Israel) | DBE system (FujinonToshiba ES System, Saitama, Japan) | CE: fasting after midnight on the evening before the examination (minimum 8 h) DBE: overnight fasting and ingestion of 1 l of electrolyte lavage preparation (Niflec, Ajinomoto Pharma, Tokyo, Japan) in the morning. | 1-7 d | 29/32 Angiodysplasia: 8 bleeding: 6 | 21/32 Angiodysplasia: 7 bleeding: 6 |
| Li et al[35], 2010 | 190 | Prospective study | M2A, Given Imaging, Ltd. (Yoqneam, Israel) | Fujinon EN-450P5/ 20 and EN-450P5/28 (Fujinon Inc., Saitama, Japan) | CE: 1 L of PEG electrolyte 12 h before the procedure Anterograde DBE: fasted for 8 h. Retrograde DBE: PEG electrolytes preparation 4 h before the examination | 5.8 d (1-18) | 165/190 AVM: 7 Fresh blood or clots: 8 | 34/51 AVM: 9 Bleeding: 0 Angioma: 4 | |
| Lin et al[40], 2007 | 63.5 ± 22.7 (11-87) | 10 M:3 F:7 | Prospective study | Pill Cam SB capsule (Given Imaging, Yoqneam, Israel) | DBE: EN- 450P5 and the EN-450T5 | CE: fast overnight for 8-12 h Anterograde DBE: fasting for 6-8 h Retrograde DBE: bowel cleansing as in a colonoscopy. | 7 d | 9/10 Angiodysplasias: 3 Bleeding: 3 | 8/10 Angiodysplasias: 3 Varices: 1 Dieulafoy’s lesion: 1 |
| Maeda et al[32], 2010 | 70 (30-92) | 89 M: 48 F: 41 | Retrospective analysis | PilCam SB® (SB1, SB2, or SB3) (Covidien, Irvine, CA, the United States). | (EN-450 T5/W or EN-580 T, Fujinon Inc., Saitama, Japan) | NR* | 24 h | 58/89 Angioectasia: 8 AVM : 3 Dieulafoy lesion: 9 Varices: 2 | 29/37 Angioectasia:8 AVM: 3 Dieulafoy lesion:6 Varice: 1 |
| Marmo R et al[23], 2008 | 61.6 ± 16.2 | 193 M: 119 F: 74 | Prospective study | Pillcam SB | Fujinon Double-Balloon Enteroscopy System | Anterograde DBE: fasting period of 8 h Retrograde DBE: 4 L PEG-based preparation | 2 wk | 175/193 Vascular lesions: 74 Blood or clot: 34 | 132/193 Vascular lesions: 72 |
| Tian Min et al[39], 2013 | 55.4 (23-78) | 62 M: 34 F:28 | Prospective study | Pill Cam SB capsule | EN-450P5 and the EN-450T5 (Fujinon) | CE: 2 L to 4 L PEG and fasted overnight Anterograde DBE: fasting for 6-8 h before the procedure. Retrograde DBE: bowel cleansing as in a colonoscopy. | 15 (4-60) d | 44/62 Angiodysplasia: 26 Bleeding: 26 | 48/62 Angiodysplasia: 27 Bleeding: 30 |
| Nakamura et al[29], 2006 | 58.5 (25 ± 85) | 32 M: 21 F: 11 | Prospective and blinded | M2A, Given Imaging, | Fuji EN−450 T5/20 | CE: fluid diet for 12 h and observed a fasting period starting at midnight Anterograde DBE: fasted for 12 h Retrograde DBE: clear liquid diet on the day before the examination and PEG electrolyte lavage solution on the morning of the examination | 48 h | 19/32 Angiodysplasias: 4 Red spots: 2 | 12/28 Angiodysplasias: 2 Red spots: 2 |
| Rahmi et al[33], 2013 | 67 ± 11 | 383 M: 114 F: 269 | Prospective, multicenter study | PillCam SB device | EN-450P5 and EN-450T5; Fujinon | CE: residue-free diet 2 d before VCE ingestion; 2 L PEG solution the night before the examination; patients then fasted overnight Anterograde DBE: No bowel preparation Retrograde DBE: 4 L of a PEG solution was given the day before the procedure | 4.1 ± 6.3 mo | 266/383 Angiodysplasia: 266 | 205/266 Angiodysplasia: 190 |
| Chu et al[17], 2016 | 51.1 ± 17.1 | 121 M: 60 F: 61 | Study Cohorts | OMOM capsule endoscopic device (Jinshan Science and Technology Group Co., Ltd, Chongqing, China) | Fujinon EN-450P5/20 | CE: 2 L polyethylene glycol-based electrolyte solution 12 h prior to the test, followed by an overnight fast for bowel preparation fast Retrograde DBE: bowel preparation used for CE procedure the day before the examination | 1 wk | 115/121 Angiodysplasia: 86% Active bleeding: 6 | 29/46 Angiodysplasia: 9 |
| Zhang et al[15], 2015 | 47.19 (16-78) | 88 M: 64 F: 24 | Prospective study | Pill Cam SB | Fuji DBE system | CE: 3 liters of PEG (2 liters at 10:00 pm the night before the procedure, and 1 L with the simethicone at 4:00 am on the morning of the procedure) Anterograde DBE: fast for 6-8 h Retrograde DBE: 2 L of PEG | NR | 53/88 MAV: 14 Hemangioma: 0 Diverticulum with a Bleeding: 1 | 52/88 MAV: 10 Hemangioma: 3 Diverticulum with a Bleeding: 7 |
All studies had similar characteristics; they studied the use of VCE and DBE in the diagnoses of OGIB sources, listing the sources separately. None of the studies classified vascular lesions according to the Yano[13] or Saurin[14] classification for vascular lesions of the small bowel.
A retrograde and/or anterograde route was decided based on VCE findings. Full enteroscopy using DBE was not always performed. The interval time was different in all studies based on institutional protocols. There were different definitions for vascular lesions. Every study reported a positive predictive value greater than 90%, except Fujimori[2] (33.33%) and Zhang[15] (53.31%).
Fujimori[2] exhibited high heterogeneity in poll specificity and sensitivity in addition to a poll accuracy under the medium media on SROC curve. Therefore, we excluded this paper.
Most studies (thirteen) had a low risk of bias. In 3 studies, DBE was performed after VCE, which could introduce bias in the route used (antegrade/retrograde). QUADAS-2 revealed that most studies did not exhibit bias. All studies followed the same pattern of inclusion: positive findings for VCE with posterior use of DBE performed in the same center.
Kalra[16] used Medtronic, Duluth, and the United States VCE, whereas Chu[17] used the OMOM capsule endoscopic device. All other studies were performed using the given imaging device.
Analyzing DBE as the standard procedure resulted in the following metrics for VCE: sensitivity of 93% (95%CI: 0.91-0.95; heterogeneity: 89.0%); specificity of 82% (95%CI: 0.79-0.84; heterogeneity: 87.3%); positive likelihood ratio of 5.44 (95%CI: 3.22-9.21; heterogeneity: 88.0%); negative likelihood ratio of 0.07 (95%CI: 0.03-0.18; heterogeneity: 91.3%) and accuracy of 86.75%.
VCE and DBE were developed as new examination techniques for the small intestine and have the potential to overcome conventional enteroscopy[11]. The small bowel is difficult to inspect with endoscopic methods. Prior to evaluation of the small bowel, it is recommended to repeat an upper digestive endoscopy and a colonoscopy[18]. Although intraoperative enteroscopy is the best for observing the entire small bowel, it is the most invasive procedure.
This is the first systematic review with meta-analysis to analyze the accuracy of DBE combined with VCE in diagnosing vascular lesions as a source of small bowel bleeding. The studies selected exhibited homogeneous intervention in a large number of patients. Eligibility criteria were strict, and selection and analysis were performed using international recognized protocols to avoid bias.
Saurin et al[14] divided the small bowel lesions into three distinct groups: submucosal veins, diverticula and nodules are included in the P0 lesions group; red spots and small or isolated erosions are considered P1 lesions; and angioectasias, varices, ulcerations and tumors represent P2 lesions. Yano et al[13] divided vascular small bowel lesions into 4 types depending on their characteristics and the presence or absence of bleeding. None of the studies in this meta-analysis divided the vascular lesions according to these classifications. Many sources of obscure bleeding were of vascular origin. When an endoscopic capsule or enteroscopy examination is performed and a source of bleeding is not identified, the cause is considered to be vascular by default. Thus, flash blood and clots/bleeding, active bleeding, and bleeding were considered as vascular sources in our study.
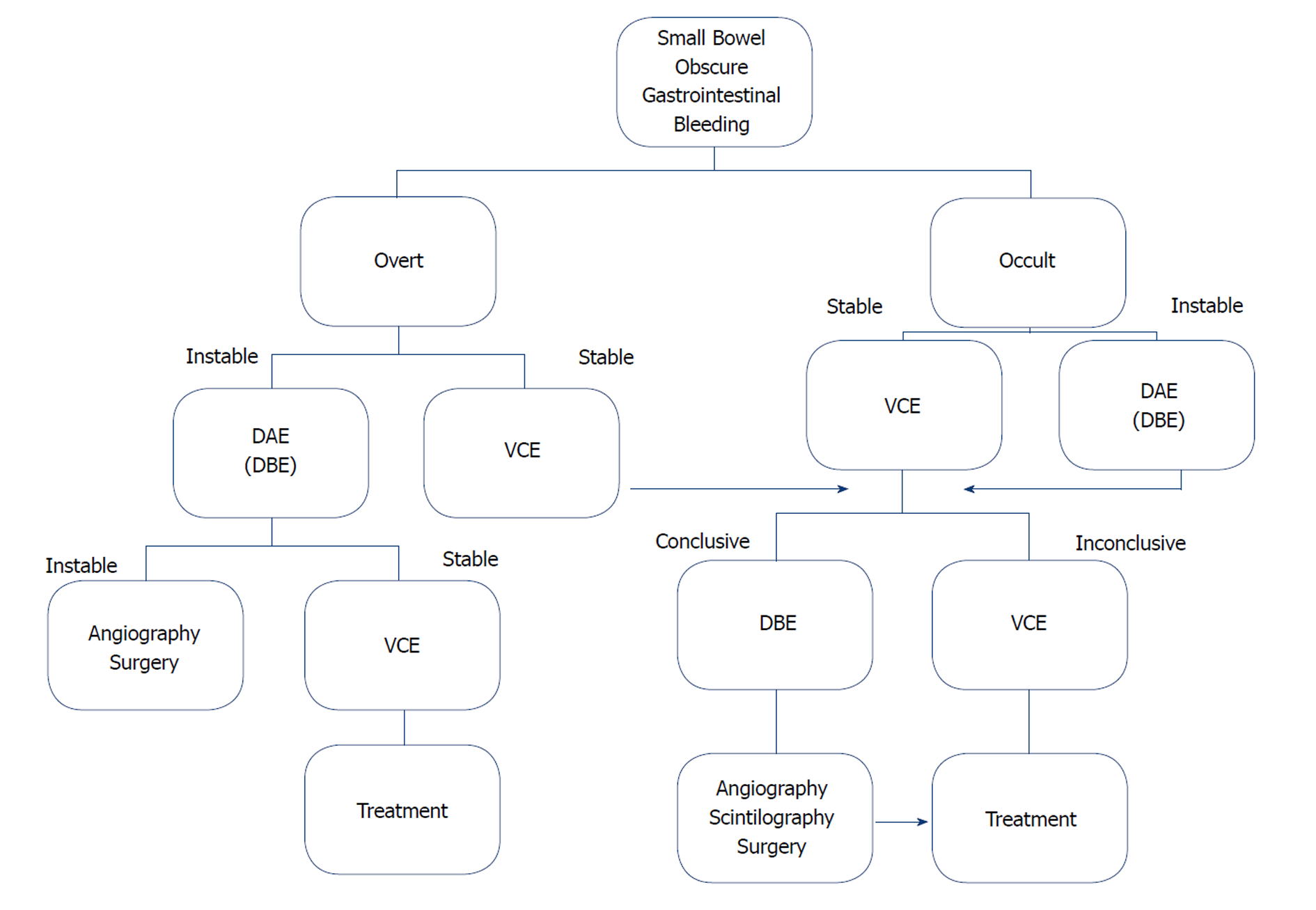
The benefits of VCE include the noninvasive nature of the test, patient acceptance, safety and diagnostic yield. However, it is limited by the inability to perform conventional endoscopic procedures, such as air insufflation, local reexamination, rinsing, biopsy, therapeutic intervention and precise identification of lesions. However, in DBE, a complete small bowel examination is typically not possible using only one route, so it often requires combined oral and rectal approaches. Diagnostic algorithms to identify gastrointestinal bleeding have suggested that VCE is best used initially to identify the lesion. DBE is best used for performing a therapeutic procedure after VCE. Thus, VCE was chosen as the gold standard in this review.
The diagnostic yield of VCE, DBE and single balloon enteroscopy (SBE) appears highest for patients with ongoing overt bleeding[19-21]. Comparing VCE and SBE, Shiani et al[19] reported a strong degree of concordance between VCE and SBE for active bleeding and clots but only moderate concordance for vascular lesions and fair concordance for ulcers. The diagnostic yield of VCE is increased if performed within 2 wk (greatest in 48 to 72 h). The timing of capsule endoscopy can influence the diagnosis and outcomes in patients with small bowel bleeding by identifying patients for early intervention, leading to endoscopic or surgical interventions or changes in medical management[22]. A study reported a high diagnostic and therapeutic yield (90%) with early (within 24 h) DBE in 10 patients with overt small bowel bleeding[23].
Regarding emergency ongoing overt OGIB, European Society of Gastrointestinal Endoscopy suggests that small bowel capsule endoscopy or device-assisted enteroscopy should be considered as a first-line approach[24]. Studies included in this meta-analysis did not differentiate the cause of bleeding as emergency or nonemergency. However, our results revealed increased accuracy of VCE to identify the vascular source of bleeding compared with DBE. This result demonstrates the ability of VCE to exclude lesions and to demonstrate the direction of the DBE. These results allow us to recommend the capsule as the first-line approach in these cases.
In the evaluation of OGIB, Martínez et al[25] demonstrated that the overall diagnostic yield of antegrade DBE is roughly equivalent to VCE; however, the diagnostic yield of DBE is increased when pre-DBE imaging is positive. A lesion source is frequently identified when pre-DBE imaging is negative or not performed. In a systematic review with 9 articles, Westerhof et al[26] reported that the diagnostic yields of CE and DBE for OGIB varied between 38% and 83% for CE and between 43% and 75% for DBE. The concordance between findings of CE with those of DBE varied between 29% and 92%, and the most frequent diagnosis was angiodysplasias. Our review reveals that DBE is reasonably sensitive and exhibits high specificity; however, it performs worse than VCE. Performing DBE after the CE increases the vascular lesion detection index by 7% from 83% to 90%.
This study is helpful for selecting the best initial diagnostic procedure in patients in whom vascular bleeding is suspected, such as cases of vascular syndromes, elderly patients and patients using anticoagulants. In many locations, these procedures are associated with high costs and are not always available at the same center. Although suggestions for the use of DBE as the first choice in obscure bleeding are reported, we have demonstrated that VCE would be the best and safest choice based on a 7% increase in diagnostic yield of DBE regardless of the severity of the case.
Variables that have been associated with an increased detection rate includes earlier VCE, inpatient status, overt GI bleeding with transfusion requirement, male sex, increasing age, use of warfarin and liver comorbidity[24]. Unfortunately, the articles did not stratify the findings according to these variables but according to the findings of the examinations, preventing very interesting data from being collected and analyzed.
A greater sensitivity of DBE in small bowel OGIB after using the VCE as the initial examination was observed. Considering the high sensibility of VCE in relation to DBE (93% × 84%), we suggest its use for suspicion of vascular lesions. Despite the low specificity noted when using VCE after DBE, its posttest result is double that of DBE (85% × 41.6%), prompting us to suggest using this feature after DBE with a negative finding. In this meta-analysis, we included studies in which VCE was performed before enteroscopy, and the route was chosen according to the possible location of the finding in the VCE. This procedure leads to an increased probability of finding the lesion with DBE. On the other hand, some enteroscopies were not completed because they only used one of the insertion pathways.
In one study[27] that attempted complete small bowel examination, all patients underwent both an antegrade and retrograde DBE procedure, whereas the DBE strategy varied in the other studies. In two studies, the antegrade or retrograde approach of DBE was chosen based on the VCE findings[2,28]. One study[29] chose the route of DBE based on the medical history. One study[4] chose the antegrade route of DBE in all cases followed by an alternate approach if considered necessary. In many studies, the decision to perform an additional DBE using the alternate route was made after considering several factors, including the results of the initial procedure, clinical indication, and patient consent. Two studies[29,30] had a single-blinded design.
The mean age of our study was 57.2 years. Angiectasias accounts for 20% to 30% of small bowel bleeding and are more commonly observed in older patients. In addition, bleeding in those who use nonsteroidal anti-inflammatory drugs and proper intestinal preparation facilitates lesion identification. The analyzed studies did not stratify the findings in the examinations regarding age, use of medications (nonsteroidal anti-inflammatory drugs), urgency/emergency indications, and bowel preparation, which prevents us from analyzing more data that would provide valuable information[31].
Although studies have assessed the diagnostic yield of VCE, PE, and device-assisted enteroscopy in OGIB, the precise significance of lesions identified and the impact on clinical outcome have not been consistently evaluated for those modalities. In the case of OGIB, a positive patient outcome should be either cessation of bleeding or resolution of anemia. Several studies have demonstrated a change in patient management and improved outcomes following VCE and device-assisted enteroscopy[32].
Of the included manuscripts, seven included patient follow-up. The mean duration of follow-up varied from 5 to 12 mo. Patients continued to exhibit bleeding in most of these studies, ranging from 65% to 81% including those whose findings were external of the small bowel[4,25,27,31,33-35].
Our study has some limitations, including nonstandardized follow-up of the patients after the exams, no standardized bowel preparation between the studies and no standard interval time between the exams. Additionally, performing DBE after a VCE exam facilitates the decision of the insertion route for enteroscopy (Figure 8). All of these limitations appear to favor DBE. The analyzed studies did not stratify the findings in the examinations regarding age, use of medications (nonsteroidal anti-inflammatory drugs), urgency/emergency of the indication, and the preparation, which prevents us from analyzing more data that would provide valuable information. These are data that would enrich the revision; however, they depend on the particularities of conduct of each author.
In conclusion, the diagnostic accuracy of detecting small bowel bleeding from a vascular source is greater with the use of an isolated VCE compared with isolated DBE. However, concomitant use increases the detection rate of the bleeding source.
Obscure gastrointestinal bleeding (OGIB) is a challenge to the professional who faces this occurrence. Although only a small part of these bleeds occurs in the midgut, the difficulty in accessing it implies a longer interval between the onset of symptoms and diagnosis and therapy. Initially, we used enteroscopes with single balloon, including spiral and double balloon overtubes, which is the most commonly used. Subsequently, the endoscopic capsule was introduced, allowing a greater index of complete observation of the small intestine with greater comfort to the patient. A weakness includes the therapeutic impossibility present in balloon enteroscopy. Due to the particularities of each of the methods, we should seek data in the available scientific literature to support our most appropriate diagnostic decision.
Video capsule endoscopy (VCE) and double-balloon enteroscopy (DBE) are recognized endoscopic diagnostic approaches for OGIB, for which vascular origins represent the most common source. Our initial motivation was to determine whether there is a preferential diagnostic approach in OGIB by vascular origin that maintains high accuracy. From the literature review about the subject, we realized some characteristics that we interpreted as important limitations in the previous works. Thereafter, this study sought to remove these limitations and to follow a rigorous methodological approach in the selection and analysis to enhance knowledge about accuracy data.
We want to compare accuracy data between the two most widespread indicated endoscopic approach methods in OGIB: VCE and DBE. It was possible to obtain a large sample of patients submitted to both methods from the literature. We believe that future systematic reviews on this issue can be based on our selection and analysis methodology. In addition, new studies that will be published can be added to update and provide a greater dimension to the theme.
This systematic review was conducted according to the PRISMA Statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and registered on PROSPERO international database. The search was performed in the electronic databases MedLine (via PubMed), LILACS (via BVS) and Cochrane/CENTRAL virtual databases. The QUADAS-2 tool was used to evaluate the risk of bias and the applicability of primary diagnostic accuracy studies and the incorporation of recent studies on the OGIB approach. All articles were read and chosen based on common consensus among three authors, and restricted inclusion criteria provide greater magnitude and accuracy.
Seventeen studies were included with 3150 exams performed in 2043 patients, resulting in the identification of 1467 vascular lesions. The specificity found for DBE is greater than that of VCE (92% vs 82%) possibly because the examiner is able to examine in more detail the alterations found when performing DBE. In contrast, the sensitivity of the VCE is greater than that of the DBE (93% vs 84%) perhaps due to the natural increase in the capacity of the lens of the capsule and the fact that the insufflation of air in the small intestine during the examination with DBE greatly increases the pressure in the organ above the capillary pressure, which prevents the lesions from being observed in this exam. The increase in the diagnostic yield to the vascular lesion is greater when the DBE is performed after VCE.
Through direct meta-analysis of the largest sample ever collected, we compared in isolation the diagnostic methods studied. The diagnostic accuracy of detecting small bowel bleeding from a vascular source is greater with VCE despite reduced specificity. This study sought to remove the bias from the lack of methodological rigor applied in the restrict inclusion criteria with the use of more than two authors for study selection and rigorous protocols accepted worldwide for the choice these studies, thus obtaining more purified results. This study also proposes that in addition to contributing to a greater specificity intrinsic to the examination, performing DBE after the use of VCE contributes to increased accuracy.
The comparison between these two methods through meta-analyses always could be influenced by the technical differences applied in each study. A pertinent study design would include multicentric study with standardized protocols of care, including initial care, standard interval time between onset of symptoms and the first exam, standardized time between the exams, and standardized patient follow-up and bowel preparation.
PRISMA Checklist: The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Brazil
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Tabibian JH, Goral V, Amornyotin S S- Editor: Dou Y L- Editor: A E- Editor: Tan WW
| 1. | Katz LB. The role of surgery in occult gastrointestinal bleeding. Semin Gastrointest Dis. 1999;10:78-81. [PubMed] |
| 2. | Fujimori S, Seo T, Gudis K, Tanaka S, Mitsui K, Kobayashi T, Ehara A, Yonezawa M, Tatsuguchi A, Sakamoto C. Diagnosis and treatment of obscure gastrointestinal bleeding using combined capsule endoscopy and double balloon endoscopy: 1-year follow-up study. Endoscopy. 2007;39:1053-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Sulbaran M, de Moura E, Bernardo W, Morais C, Oliveira J, Bustamante-Lopez L, Sakai P, Mönkemüller K, Safatle-Ribeiro A. Overtube-assisted enteroscopy and capsule endoscopy for the diagnosis of small-bowel polyps and tumors: a systematic review and meta-analysis. Endosc Int Open. 2016;4:E151-E163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Hadithi M, Heine GD, Jacobs MA, van Bodegraven AA, Mulder CJ. A prospective study comparing video capsule endoscopy with double-balloon enteroscopy in patients with obscure gastrointestinal bleeding. Am J Gastroenterol. 2006;101:52-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 184] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 5. | Foutch PG. Angiodysplasia of the gastrointestinal tract. Am J Gastroenterol. 1993;88:807-818. [PubMed] |
| 6. | Kwo PY, Tremaine WJ. Nonsteroidal anti-inflammatory drug-induced enteropathy: case discussion and review of the literature. Mayo Clin Proc. 1995;70:55-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Bartram CI, Amess JA. The diagnosis of Meckel’s diverticulum by small bowel enema in the investigation of obscure intestinal bleeding. Br J Surg. 1980;67:417-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Kodama M, Uto H, Numata M, Hori T, Murayama T, Sasaki F, Tsubouchi N, Ido A, Shimoda K, Tsubouchi H. Endoscopic characterization of the small bowel in patients with portal hypertension evaluated by double balloon endoscopy. J Gastroenterol. 2008;43:589-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Safatle-Ribeiro AV, de Oliveira RJ, Pu LZ, Caiado ÂH, de Moura EG, Ribeiro U Jr, Zilberstein B. Obscure gastrointestinal bleeding caused by intestinal lipomatosis: double-balloon endoscopic and laparoscopic views. Endoscopy. 2016;48 Suppl 1 UCTN:E61-E62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Ribeiro IB, Bernardo WM, Martins BDC, de Moura DTH, Baba ER, Josino IR, Miyahima NT, Coronel Cordero MA, Visconti TAC, Ide E. Colonic stent versus emergency surgery as treatment of malignant colonic obstruction in the palliative setting: a systematic review and meta-analysis. Endosc Int Open. 2018;6:E558-E567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 11. | Hermans C, Stronkhorst A, Tjhie-Wensing A, Kamphuis J, Balkom BV, Dahlmans R, Gilissen L. Double-Balloon Endoscopy in Overt and Occult Small Bowel Bleeding: Results, Complications, and Correlation with Prior Videocapsule Endoscopy in a Tertiary Referral Center. Clin Endosc. 2017;50:69-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | ASGE Standards of Practice Committee, Fisher L, Lee Krinsky M, Anderson MA, Appalaneni V, Banerjee S, Ben-Menachem T, Cash BD, Decker GA, Fanelli RD, Friis C, Fukami N, Harrison ME, Ikenberry SO, Jain R, Jue T, Khan K, Maple JT, Strohmeyer L, Sharaf R, Dominitz JA. The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc. 2010;72:471-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 166] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 13. | Yano T, Yamamoto H, Sunada K, Miyata T, Iwamoto M, Hayashi Y, Arashiro M, Sugano K. Endoscopic classification of vascular lesions of the small intestine (with videos). Gastrointest Endosc. 2008;67:169-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 130] [Article Influence: 7.6] [Reference Citation Analysis (1)] |
| 14. | Saurin JC, Delvaux M, Gaudin JL, Fassler I, Villarejo J, Vahedi K, Bitoun A, Canard JM, Souquet JC, Ponchon T. Diagnostic value of endoscopic capsule in patients with obscure digestive bleeding: blinded comparison with video push-enteroscopy. Endoscopy. 2003;35:576-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 315] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 15. | Zhang Q, He Q, Liu J, Ma F, Zhi F, Bai Y. Combined use of capsule endoscopy and double-balloon enteroscopy in the diagnosis of obscure gastrointestinal bleeding: meta-analysis and pooled analysis. Hepatogastroenterology. 2013;60:1885-1891. [PubMed] |
| 16. | Kalra AS, Walker AJ, Benson ME, Soni A, Guda NM, Misha M, Gopal DV. Comparison of Capsule Endoscopy Findings to Subsequent Double Balloon Enteroscopy: A Dual Center Experience. Diagn Ther Endosc. 2015;2015:438757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Chu Y, Wu S, Qian Y, Wang Q, Li J, Tang Y, Bai T, Wang L. Complimentary Imaging Modalities for Investigating Obscure Gastrointestinal Bleeding: Capsule Endoscopy, Double-Balloon Enteroscopy, and Computed Tomographic Enterography. Gastroenterol Res Pract. 2016;2016:8367519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Ribeiro IB, Rezende DT, Madruga Neto AC, Ide E, Furuya CK, De Moura DTH, De Moura EGH. Endoscopic dual therapy for giant peptic ulcer hemorrhage. Endoscopy. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Shiani A, Nieves J, Lipka S, Patel B, Kumar A, Brady P. Degree of concordance between single balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding after an initial positive capsule endoscopy finding. Therap Adv Gastroenterol. 2016;9:13-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Carey EJ, Fleischer DE. Investigation of the small bowel in gastrointestinal bleeding--enteroscopy and capsule endoscopy. Gastroenterol Clin North Am. 2005;34:719-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Gerson LB, Van Dam J. Wireless capsule endoscopy and double-balloon enteroscopy for the diagnosis of obscure gastrointestinal bleeding. Tech Vasc Interv Radiol. 2004;7:130-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | ASGE Technology Committee, Wang A, Banerjee S, Barth BA, Bhat YM, Chauhan S, Gottlieb KT, Konda V, Maple JT, Murad F, Pfau PR, Pleskow DK, Siddiqui UD, Tokar JL, Rodriguez SA. Wireless capsule endoscopy. Gastrointest Endosc. 2013;78:805-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 194] [Article Influence: 16.2] [Reference Citation Analysis (2)] |
| 23. | Marmo R, Rotondano G, Casetti T, Manes G, Chilovi F, Sprujevnik T, Bianco MA, Brancaccio ML, Imbesi V, Benvenuti S. Degree of concordance between double-balloon enteroscopy and capsule endoscopy in obscure gastrointestinal bleeding: a multicenter study. Endoscopy. 2009;41:587-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 68] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 24. | Pennazio M, Spada C, Eliakim R, Keuchel M, May A, Mulder CJ, Rondonotti E, Adler SN, Albert J, Baltes P. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2015;47:352-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 482] [Cited by in RCA: 560] [Article Influence: 56.0] [Reference Citation Analysis (1)] |
| 25. | Martínez EP, Robles EP. Capsule endoscopy and deep enteroscopy. Endoscopy. 2014;46:787-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Westerhof J, Weersma RK, Koornstra JJ. Investigating obscure gastrointestinal bleeding: capsule endoscopy or double balloon enteroscopy? Neth J Med. 2009;67:260-265. [PubMed] |
| 27. | Kameda N, Higuchi K, Shiba M, Machida H, Okazaki H, Yamagami H, Tanigawa T, Watanabe K, Watanabe T, Tominaga K. A prospective, single-blind trial comparing wireless capsule endoscopy and double-balloon enteroscopy in patients with obscure gastrointestinal bleeding. J Gastroenterol. 2008;43:434-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 28. | Otsuka T, Kawazoe S, Nakashita S, Kamachi S, Oeda S, Sumida C, Akiyama T, Ario K, Fujimoto M, Tabuchi M. Low-dose rectal diclofenac for prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: a randomized controlled trial. J Gastroenterol. 2012;47:912-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 29. | Nakamura M, Niwa Y, Ohmiya N, Miyahara R, Ohashi A, Itoh A, Hirooka Y, Goto H. Preliminary comparison of capsule endoscopy and double-balloon enteroscopy in patients with suspected small-bowel bleeding. Endoscopy. 2006;38:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 166] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 30. | Kamalaporn P, Cho S, Basset N, Cirocco M, May G, Kortan P, Kandel G, Marcon N. Double-balloon enteroscopy following capsule endoscopy in the management of obscure gastrointestinal bleeding: outcome of a combined approach. Can J Gastroenterol. 2008;22:491-495. [PubMed] |
| 31. | ASGE Standards of Practice Committee, Gurudu SR, Bruining DH, Acosta RD, Eloubeidi MA, Faulx AL, Khashab MA, Kothari S, Lightdale JR, Muthusamy VR, Yang J, DeWitt JM. The role of endoscopy in the management of suspected small-bowel bleeding. Gastrointest Endosc. 2017;85:22-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 111] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 32. | Maeda Y, Moribata K, Deguchi H, Inoue I, Maekita T, Iguchi M, Tamai H, Kato J, Ichinose M. Video capsule endoscopy as the initial examination for overt obscure gastrointestinal bleeding can efficiently identify patients who require double-balloon enteroscopy. BMC Gastroenterol. 2015;15:132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Rahmi G, Samaha E, Vahedi K, Delvaux M, Gay G, Lamouliatte H, Filoche B, Saurin JC, Ponchon T, Rhun ML. Long-term follow-up of patients undergoing capsule and double-balloon enteroscopy for identification and treatment of small-bowel vascular lesions: a prospective, multicenter study. Endoscopy. 2014;46:591-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 34. | Kaffes AJ, Siah C, Koo JH. Clinical outcomes after double-balloon enteroscopy in patients with obscure GI bleeding and a positive capsule endoscopy. Gastrointest Endosc. 2007;66:304-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 81] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 35. | Li X, Dai J, Lu H, Gao Y, Chen H, Ge Z. A prospective study on evaluating the diagnostic yield of video capsule endoscopy followed by directed double-balloon enteroscopy in patients with obscure gastrointestinal bleeding. Dig Dis Sci. 2010;55:1704-1710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement Ann Intern Med 2014; 151: 264-269. . [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47171] [Article Influence: 2948.2] [Reference Citation Analysis (0)] |
| 37. | Holleran G, Hall B, Alhinai M, Zaheer A, Leen R, Alakkari A, Mahmud N, McNamara D. Double-balloon enteroscopy in Ireland in the capsule endoscopy era. Ir J Med Sci. 2015;184:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 38. | Fuller NR, Pearson S, Lau NS, Wlodarczyk J, Halstead MB, Tee HP, Chettiar R, Kaffes AJ. An intragastric balloon in the treatment of obese individuals with metabolic syndrome: a randomized controlled study. Obesity (Silver Spring). 2013;21:1561-1570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 77] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 39. | Tian Min C, Li Hua X, Ying Lin J, Yan Mei Y, Fei L, Jun Bo Q. The role of double-balloon enteroscopy following capsule endoscopy in diagnosis of obscure Small intestinal diseases. Pak J Med Sci. 2013;29:479-484. [PubMed] |
| 40. | Lin TN, Su MY, Hsu CM, Lin WP, Chiu CT, Chen PC. Combined use of capsule endoscopy and double-balloon enteroscopy in patients with obscure gastrointestinal bleeding. Chang Gung Med J. 2008;31:450-456. [PubMed] |