Published online Jan 16, 2018. doi: 10.4253/wjge.v10.i1.23
Peer-review started: August 7, 2017
First decision: August 29, 2017
Revised: September 25, 2017
Accepted: December 5, 2017
Article in press: December 5, 2017
Published online: January 16, 2018
Processing time: 161 Days and 9.5 Hours
To organize post-procedure satisfaction data into a useful reference and analyze patient-centered parameters to find trends that influence patient satisfaction.
A robust database of two cohorts of outpatients that underwent an endoscopic procedure at Georgetown University Hospital at two separate three-month intervals ranging from November 2012 to January 2013 and November 2015 to January 2016 was compiled. Time of year was identical to control for weather/seasonal issues that may have contributed to the patient experience. The variables recorded included age, sex, body mass index (BMI), type of procedure, indication for procedure, time of the procedure, length of the procedure, type of prep used, endoscopist, satisfactory score, and comments/reasons for score. For continuous variables, differences in averages were tested by two sample t-test, Wilcoxon rank sum test, and ANOVA as appropriate. For categorical variables, differences in proportions between two groups were tested by χ2 test. Correlation test and linear regression analyses were conducted to examine relationships between length of procedure and continuous predictors. A P value < 0.05 used to indicate statistically significant relationship.
The primary outcome of this study was to assess if telephone outreach after an endoscopic intervention was a satisfactory method of obtaining post-procedure satisfaction scores from patients at a tertiary care center. With the addition of post-procedure calls, instilled in January 2014, the response rate was 40.5% (508/1256 patients) from a prior completion rate of 3.4% (31/918) with the mail out survey initially. There was a statistically significant improved response rate pre and post intervention with P < 0001. The secondary outcome of this study was to assess if we could use predictive analytics to identify independent predictors of procedure length, such as gender, age, type of procedure, time of procedure, or BMI. The combined pre and post intervention data was used in order to optimize the power to identify independent predictors of procedure length. The total number of patient’s data analyzed was 2174. There was no statistically significant difference in procedure length between males and females with P value 0.5282. However, there was a small (1 min), but statistically significant difference (P = 0.0185) in procedure length based on the time of day the procedure took place, with afternoon procedures having a longer duration than morning procedures. The type of procedure was an independent predictor of procedure length as demonstrated with P value < 0.0001. There is a statistically significant correlation between age and procedure length, although it is only a weak relationship with a correlation coefficient < 0.3. Contrary to patient age, BMI did not have a statistically significant correlation with procedure length (P = 0.9993), which was also confirmed by linear regression analysis.
Our study proves calling patients after endoscopy improves post-procedure satisfaction response rates and changing procedural time allotment based on patient characteristics would not change endoscopic workflow.
Core tip: We analyzed the post-endoscopy survey system that had been implemented and largely ignored in the past in order to understand where we are succeeding and failing in our endoscopy suite in regards to the overall patient experience. We also looked at patient-centered parameters that could influence procedure length, which is a common surrogate for satisfaction, to reflect on current practices and allow for process improvements in order to optimize the patient experience in our endoscopy suite.
- Citation: Munjal A, Steinberg JM, Mossaad A, Kallus SJ, Mattar MC, Haddad NG. Post-endoscopic procedure satisfaction scores: Can we improve? World J Gastrointest Endosc 2018; 10(1): 23-29
- URL: https://www.wjgnet.com/1948-5190/full/v10/i1/23.htm
- DOI: https://dx.doi.org/10.4253/wjge.v10.i1.23
According to the recently published article, Quality Indicators Common to All GI Endoscopic Procedures[1], a key post-procedure quality measure should include factors that can improve with endoscopy. It is recognized that patient satisfaction is an important outcome measure as it pertains to both the patient and the endoscopy unit. Poor experiences in the endoscopy unit may lead to non-compliance with endoscopic screening and/or monitoring[2]. Quality measures are put in place so that there is constant oversight and evaluation of the process, guaranteeing continued improvement. A commonly used survey known as the modified Group Health Association of America patient satisfaction survey (mGHAA-9) focuses on key points throughout the patient’s experience, including, waiting time, manners of the staff and doctor, doctor skills and explanation of the procedure[3]. Currently, the mGHAA-9 is not in use at Georgetown University Hospital; rather, every patient that has an outpatient procedure receives a follow-up call asking him/her to rank the experience on a scale of 1-3. This formal post-procedural call system was implemented in January 2014 and is carried out by our administrative personnel. This data is filed in the electronic medical record and has been largely ignored to date.
The purpose of this study is to organize the post-procedure satisfaction data into a useful and minable reference in order to understand our successes and failures in our endoscopy suite. Furthermore, by looking at various patient-centered parameters such as age, sex, body mass index (BMI) and procedural parameters including length of procedure, type of procedure, and the time of day a procedure is performed, we intended to find trends in these factors that might influence the overall outcome. Statistical analysis of this information will allow for reflection on current practices and lead to process improvements in order to optimize the patient experience in our endoscopy suite at Georgetown University Hospital, and perhaps help to construct a universal protocol that could be adopted by other institutions nationwide that would enhance the patient experience.
Our investigators compiled a robust database of two cohorts of outpatients that underwent an endoscopic procedure ranging from EGDs, colonoscopies, flexible sigmoidoscopy, ileoscopy, single and double balloon enteroscopies, ERCPs and endoscopic ultrasound at Georgetown University Hospital at two separate three-month intervals. The first was between November 1st 2012 and January 31st 2013, and the second was from November 1st 2015 through January 31st 2016. Those months were chosen, as they were the most up to date in regards to available survey data at the start of the study. The time of year remained identical to control for possible weather/seasonal issues that may have contributed to the patient experience. Patients’ charts were then reviewed with all personal health information being de-identified. The variables recorded included: Patient age, sex, BMI, type of procedure, indication for procedure, time of day the procedure took place, length of procedure, type of prep used (if any), endoscopist, satisfaction score, and comments/reasons for score (if recorded). It should be noted that our institution adopted a post-procedure call survey system in January 2014 to obtain patient feedback and satisfaction scores. Prior to January 2014, the method for attaining patient satisfaction information was via a letter that was mailed to the patient’s home.
Our primary outcome was to assess improvement in response rates from a mailed out survey via the postal service to telephone outreach to assess post-procedure satisfaction scores. The secondary analysis, and more informative aspect of the study, was to see if the use of predictive analytics could identify independent predictors of procedure length, which could then be focused on to optimize patient experience in the endoscopy unit at this tertiary care facility.
Means and standard deviations for continuous variables and frequencies and percentages for categorical variables are respectively provided in the following tables below. For the continuous variables, differences in the averages between two groups were tested by two sample t-test and Wilcoxon rank sum test as appropriate. ANOVA was used to examine differences in the averages between three or more groups. For categorical variables, differences in proportions between two groups were tested by χ2 test. Correlation test and linear regression analyses were conducted to examine the relationship between length of procedure and continuous predictors. A P value < 0.05 was used to determine a statistically significant relationship.
The primary outcome of this study was to assess if telephone outreach after an endoscopic intervention was a satisfactory method of obtaining post-procedure satisfaction scores from patients at a tertiary care center. With the addition of post-procedure calls, instilled in January 2014, the response rate increased to 40.5% (508/1256 patients). Prior to the calls, the documented post-procedure satisfaction survey completion rate via mailed out surveys was 3.4% (31/918). With the implementation of the phone call survey, we are able to show a statistically significant improved response rate pre and post intervention (Table 1).
| Characteristics | Pre intervention, n = 918 | Post intervention, n = 1256 | P value |
| Response rate (satisfaction score) | 31 (3.4%) | 508 (40.5%) | < 0.0001 |
The secondary outcome of this study was to assess if we could use predictive analytics to identify independent predictors of procedure length, such as gender, age, type of procedure, time of procedure, or BMI. The combined pre and post intervention data was used in order to optimize the power of the study to identify independent predictors of procedure length which is often used as a surrogate for patient satisfaction and can allow for changes to the work flow within the endoscopy suite to better suit their needs. The total number of patient’s data analyzed was 2174. Table 2 examines independent predictors including gender as well as timing of the procedure, particularly morning vs afternoon. In regards to gender, there was no statistically significant difference in procedure length between males and females. However, there was a small, 1-min, but statistically significant difference in procedure length based on the time of day the procedure took place, with afternoon procedures having a longer duration than morning procedures.
| Time of procedure | ||||||
| Female, n = 1162 | Male, n = 1012 | P value | AM, n = 1089 | PM, n = 1084 | P value | |
| Procedure length | 20.6 ± 12.1 | 20.9 ± 12.6 | 0.5282 | 20.1 ± 11.8 | 21.3 ± 12.8 | 0.0185 |
As would be expected, the type of procedure was an independent predictor of procedure length as demonstrated in Table 3. The final two variables that were analyzed to assess if they were independent predictors of procedure length were age and BMI. Table 4 shows the relationship between mean age and BMI and length of procedure for the combined pre and post intervention group. The average age of patients in the study was 58 years old and average procedure length was 20.7 min. The average BMI of the patient population was 27. Table 5 looks at the strength of the relationship between age and BMI and procedure length. While there is a statistically significant correlation between age and procedure length, it is a weak relationship being defined as correlation coefficients < 0.3 as weak, correlation coefficient > 0.3 but < 0.5 as moderate, correlation coefficient > 0.5 but < 0.7 as strong, correlation coefficient > 0.7 as a perfect correlation. Contrary to patient age, BMI did not have a statistically significant correlation with procedure length (P value 0.9993). Linear regression analysis also confirmed no statistically significant relationship between BMI and procedure length (data not shown).
| Procedure | ||||||||
| Colonoscopy, n = 981 | EGD, n = 714 | EUS, n = 301 | ERCP, n = 116 | Enteroscopy, n = 36 | Flex sig, n = 20 | Ileoscopy, n = 6 | P value | |
| Procedure length | 22.1 ± 10.1 | 18.6 ± 13.1 | 17.4 ± 10.7 | 23.0 ± 12.7 | 49.2 ± 19.3 | 14.8 ± 9.7 | 18.8 ± 15.2 | < 0.0001 |
| Variable | n | Mean | Std Dev |
| Age | 2174 | 57.97286 | 15.84377 |
| Body mass index | 2030 | 27.18420 | 7.01924 |
| Length of procedure | 2174 | 20.71665 | 12.31821 |
| Pearson correlation coefficients, n = 2174 | ||
| Age | Length of procedure | |
| Age | 1.00000 | 0.07781 |
| 0.0003 | ||
| Length of procedure | 0.07781 | 1.00000 |
| BMI | Length of procedure | |
| 0.0003 | ||
| BMI | 1.00000 | -0.00002 |
| 0.9993 | ||
| Length of procedure | -0.00002 | 1.00000 |
| 0.9993 | ||
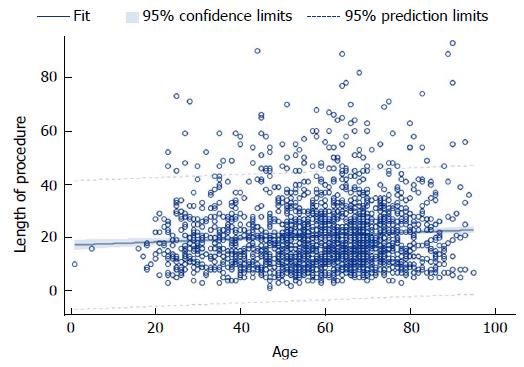
Figure 1 is a FitPlot of the relationship between age and procedure length. As is shown by the positive slope in the graph, there is a statistically significant relationship, albeit small. Using a linear regression analysis, the relationship between age and procedure length was confirmed (data not shown), and it can be concluded that for every year increase in age, there is a 0.06-min (3.6 s) increase in length of procedure.
In this retrospective study analyzing patient satisfaction following an endoscopic procedure at a tertiary care center, a number of statistically significant findings were observed. Most importantly, our research demonstrates that following the January 2014 implementation of a formal post-endoscopic telephone call to patients, patient response dramatically increased from a response rate of 40.5% compared to 3.4% initially with the mailed out survey. This finding highlights the importance of provider-initiated follow-up in obtaining patient feedback. Implementing this phone call system as a means of direct communication with patients at other locations who do not currently utilize such a process could potentially increase response rates in patient feedback, as was seen in our center so that endoscopy centers, same day surgery centers, or entire hospital systems can better meet the needs of their patients. As our phone communication requires live callers from our endoscopy center, a future study to investigate whether the use of an automated system would similarly result in increased patient response rates, would be of particular interest for optimum resource management. Ultimately, a reporting system that approaches 100% response rate should be achieved. Even with the strides made in the implementation of post-procedure telephone calls, we still fall far short of our goal of 100% response rate. This may require patient’s filling out surveys prior to discharge from the endoscopy suite, vs scheduling early, post-procedure follow-up visits where this data can be obtained, vs email or text message response systems. Future studies on how best to meet the needs of our ever-changing population are needed to identify the best practices.
Similar studies by Rasool et al[4], Trujillo-Benavides et al[5] and Qureshi et al[6] using the modified GHAA-9 questionnaire showed patient satisfaction rates of close to 90%. Waiting times for the appointment, waiting time before the procedure, and inadequate explanations were identified as the most common reasons leading to patient dissatisfaction. Interestingly, in a study performed by Del Río et al[7], a one question survey was administered at the end of the procedure rating the overall performance and then the modified GHAA-9 questionnaire was used 3 wk later. The results of both the questionnaires did not adequately correlate, which may influence survey practices in order to improve patient satisfaction in the future as the one question post-endoscopic question survey is a common practice in many universities including here at Georgetown University. It is possible that this is related to post-procedural complications that may occur after the patient has left the endoscopy suite and is therefore not reflected in the initial survey. Salmon et al[8] created a 31-item questionnaire to evaluate satisfaction in colonoscopy. However, this was not an easily used method for survey using telephone interviews per Del Río et al[7]. It is important to also note that our study included all endoscopic procedures ranging from EGDs to balloon enteroscopies and colonoscopies, which have significant differences in invasiveness and length of procedure and may lead to variances in patient satisfaction. Feedback that is provided with such questionnaires is important in leading to improvement in endoscopy practices in the future as it identifies patients’ thoughts and concerns.
Further analysis in our study focused on whether there were any independent variables that predicted shorter length of procedure, which was used as a surrogate outcome for patient satisfaction. Many factors have been associated with procedure length including age[9,10,11], sex[9,10,12], BMI[9,10,13], quality of bowel preparation[9,11], history of prior hysterectomy[12,14], diverticulosis[10], constipation[10,11], fellow involvement[15], lower endoscopist annual case volume[9,16], and two-person method[17] although many of these studies have had conflicting results[18]. A few studies have shown that patients with a lower BMI are more likely to have an incomplete colonoscopy or longer insertion time, which may be directly correlated to the amount of visceral fat although our study revealed no correlation[9,10,13]. Other factors such as the endoscopist’s skill level, instrument used, coordination of the team, and anesthesia administered are also linked to procedure length[19,20,21] and may be confounding factors that lead to conflicting results in prior studies. In a study performed by Hsu et al[17], it was shown that female sex, poor quality of bowel preparation, smaller waist circumference and older age were predictors of a longer cecal intubation time. The differences in sexes are thought to be secondary to women having longer colons and less visceral fat, which predisposes them to loop formation[9,16,22]. In our study, we were not able to show any such difference between sexes. Of particular interest is the finding that procedure length increased with patient age, with statistical analysis showing that for every year increase in age, there is a 0.06-min (3.6 s) increase in length of procedure. This was ultimately determined to be a weak relationship after further statistical analysis in our study, Anderson et al[10], Kim et al[11] and Hsu et al[17]. Also found that older age was associated with increased procedure length. It has been reported that the length of the colon increases with age causing increased compliance and decreased elasticity likely contributing to this association[23]. When scheduling time slots for endoscopic procedures, it would then be unreasonable to allot more dedicated procedure time for older patients as compared to younger patients given this small difference in procedure time. Not surprisingly, procedure type was an independent predictor of procedure length as is a direct reflection of the invasiveness of the procedure. Timing of the procedure, in particular morning vs afternoon, also showed a statistically significant difference in regards to procedure length. There was a one-min increase in procedure length for procedures completed in the afternoon. It can be postulated that this is related to physician fatigue or overall delays that may occur in the workflow of the endoscopy suite that translates into delays as the day goes on. By tailoring endoscopic services to our patients, ideally this would improve workflow while simultaneously enhancing the patient experience.
Limitations in this study include analyzing data at only one endoscopic center in a retrospective fashion. As our center is a university affiliated tertiary referral center in a major metropolitan area, perhaps our findings would not be entirely generalizable or extrapolated to other smaller, community institutions or private practices in rural areas. As our post-endoscopic satisfaction survey telephone calls depended on our institution’s administrative personnel, there is also a possibility for systems errors in accurate documentation in the EMR. Furthermore, if an attempt was made in contacting a patient post-procedurally was unsuccessful, it typically was recorded as such in the EMR. Unfortunately, there were some records that were missing entirely, and therefore, make it unclear if any attempt was made to call the patient. One variable that was not considered was cost of procedure and patient insurance. Health care disparities often drive patients’ experiences in the health care system, and perhaps looking further into this topic within our own institution would prove to be an influential factor in patient satisfaction.
In conclusion, our study proves that calling patients after they undergo endoscopy can drastically improve post-procedure satisfaction response rates (3.4% increased to 40.5%). However, the ideal method of obtaining post-procedure satisfaction responses has yet to be implemented in our endoscopy suite. The secondary aim of this study, to identify independent variables that directly affect length of procedure, found statistical significance for patient age, but interestingly, did not find patient’s BMI to influence length of procedure. We can conclude based on our data that changing the scheduling or time allotted for procedures based on age or weight would not drastically change the flow in the endoscopy suite.
Patient satisfaction is an important outcome measure for both the patient and endoscopy unit. Poor experiences may lead to non-compliance with endoscopic screening and/or monitoring. Quality measures are instated to ensure oversight and evaluation of processes guaranteeing continued improvement. A commonly used survey known as the modified Group Health Association of America patient satisfaction survey (mGHAA-9) focuses on key points throughout the patient’s experience, including, waiting time, manners of the staff and doctor, doctor skills and explanation of the procedure3. Currently, the mGHAA-9 is not in use at Georgetown University Hospital; rather, every patient that has an outpatient procedure receives a follow up call asking him/her to rank the experience on a scale of 1-3. This formal post procedural call system was implemented in January 2014 and is carried out by our administrative personnel. This data is filed in the electronic medical record and has been largely ignored to date.
The purpose of this study is to organize the post-procedure satisfaction data into a useful reference as well as analyze various patient-centered parameters to find trends that might influence the overall outcome and lead to process improvements in order to optimize the patient experience. Our primary outcome was to assess improvement in response rates from a mailed out survey via the postal service to telephone outreach to assess post-procedure satisfaction scores. The secondary analysis, and more informative aspect of the study, was to see if the use of predictive analytics could identify independent predictors of procedure length, which could then be focused on to optimize patient experience in the endoscopy unit at this tertiary care facility.
Our primary outcome was to assess improvement in response rates from a mailed out survey via the postal service to telephone outreach to assess post-procedure satisfaction scores. The secondary analysis, and more informative aspect of the study, was to see if the use of predictive analytics could identify independent predictors of procedure length, which could then be focused on to optimize patient experience in the endoscopy unit at this tertiary care facility. Statistical analysis of this information will allow for reflection on current practices and lead to process improvements in order to optimize the patient experience in our endoscopy suite at Georgetown University Hospital, and perhaps help to construct a universal protocol that could be adopted by other institutions nationwide that would enhance patient experience.
A database of two cohorts of outpatients that underwent endoscopic procedures at Georgetown University Hospital was compiled. Several patient-related and procedure-related variables were recorded. For continuous and categorical variables, differences in averages were tested by two sample t-test, Wilcoxon rank sum test, ANOVA and χ2 test as appropriate. Correlation test and linear regression analyses were also conducted to examine relationships between length of procedure and continuous predictors.
With the addition of post-procedure calls, instilled in January 2014, the response rate was 40.5%. Prior to the calls, the documented post procedure satisfaction survey completion rate was 3.4%. There was a statistically significant improved response rate pre and post intervention. Upon analysis of patient-related variables, there was also a statistically significant relationship that was seen between age and procedure length. Our study proves that calling patients after they undergo endoscopy can drastically improve post procedure satisfaction response rates. However, the ideal method of obtaining post procedure satisfaction responses has yet to be implemented. The secondary aim of this study, to identify independent variables that directly affect length of procedure, which is often a surrogate for patient satisfaction, found statistical significance for patient age, but not body mass index (BMI).
Our research demonstrates that following the January 2014 implementation of a formal post-endoscopic telephone call to patients, patient response dramatically increased (satisfaction survey response rate of 40.5% compared to 3.4%). This finding highlights the importance of provider-initiated follow-up in obtaining patient feedback. Implementing this phone call system as a means of direct communication with patients at other locations who do not currently utilize such a process could potentially increase response rates in patient feedback, as was seen in our center so that endoscopy centers, same day surgery centers, or entire hospital systems can better meet the needs of their patients. As our phone communication requires live callers from our endoscopy center, a future study to investigate whether the use of an automated system would similarly result in increased patient response rates, would be of particular interest for optimum resource management. Ultimately, a reporting system that approaches 100% response rate should be achieved. Even with the strides made in the implementation of post procedure telephone calls, we still fall far short of our goal of 100% response rate. This may require patient’s filling out surveys prior to discharge from the endoscopy suite, vs scheduling early, post procedure follow-up visits where this data can be obtained, vs email or text message response systems. Future studies on how best to meet the needs of our ever-changing population are needed to identify best practices. The secondary aim of this study, to identify independent variables that directly affect length of procedure, which is often a surrogate for patient satisfaction, found statistical significance for patient age, time of the day of the procedure and type of procedure, but not BMI or sex. We can conclude based on our data that changing the scheduling or time allotted for procedures based on these characteristics would not drastically change the flow in the endoscopy suite.
The research is able to show that following the January 2014 implementation of a formal post-endoscopic telephone call to patients, patient response improves dramatically. This finding highlights the importance of provider-initiated follow-up in obtaining patient feedback. Implementing this phone call system as a means of direct communication with patients at other locations who do not currently utilize such a process could potentially increase response rates in patient feedback, as was seen in our center so that endoscopy centers, same day surgery centers, or entire hospital systems can better meet the needs of their patients. As our phone communication requires live callers from our endoscopy center, a future study to investigate whether the use of an automated system would similarly result in increased patient response rates, would be of particular interest for optimum resource management. Ultimately, a reporting system that approaches 100% response rate should be achieved. Even with the strides made in the implementation of post-procedure telephone calls, we still fall far short of our goal of 100% response rate. This may require patient’s filling out surveys prior to discharge from the endoscopy suite, vs scheduling early, post-procedure follow-up visits where this data can be obtained, vs email or text message response systems which should be studies in a prospective fashion. Future studies on how best to meet the needs of our ever-changing population are needed to identify the best practices. Limitations in this study also include analyzing data at only one endoscopic center in a retrospective fashion. As our center is a university affiliated tertiary referral center in a major metropolitan area, perhaps our findings would not be entirely generalizable or extrapolated to other smaller, community institutions or private practices in rural areas and should be studied in those settings in a similar fashion as ours.
Manuscript source: Unsolicited Manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Dogan UB, Sterpetti AV, Tomizawa M S- Editor: Chen K L- Editor: A E- Editor: Li D
| 1. | Rizk MK, Sawhney MS, Cohen J, Pike IM, Adler DG, Dominitz JA, Lieb JG 2nd, Lieberman DA, Park WG, Shaheen NJ, Wani S. Quality indicators common to all GI endoscopic procedures. Gastrointest Endosc. 2015;81:3-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 106] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 2. | Eckardt AJ, Swales C, Bhattacharya K, Wassef WY, Phelan NP, Zubair S, Martins N, Patel S, Moquin B, Anwar N. Open access colonoscopy in the training setting: which factors affect patient satisfaction and pain? Endoscopy. 2008;40:98-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Allen JI. Quality assurance for gastrointestinal endoscopy. Curr Opin Gastroenterol. 2012;28:442-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Rasool S, Ahmed S, Siddiqui S, Salih M, Jafri W, Hamid S. Evaluation of quality and patient satisfaction during endoscopic procedure: a cross sectional study from south Asian country. J Pak Med Assoc. 2010;60:990-995. [PubMed] |
| 5. | Trujillo-Benavides OE, Altamirano-García AA, Baltazar-Montúfar P, Maroun-Marun C, Méndez-Del Monte R, Torres-Rubí D. [Level of satisfaction from patients who undergone an endoscopic procedure and related factors]. Rev Gastroenterol Mex. 2010;75:374-379. [PubMed] |
| 6. | Qureshi MO, Shafqat F, Ahmed S, Niazi TK, Khokhar N. Factors affecting patient satisfaction during endoscopic procedures. J Coll Physicians Surg Pak. 2013;23:775-779. [PubMed] |
| 7. | Del Río AS, Baudet JS, Fernández OA, Morales I, Socas Mdel R. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol. 2007;19:896-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Salmon P, Shah R, Berg S, Williams C. Evaluating customer satisfaction with colonoscopy. Endoscopy. 1994;26:342-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Bernstein C, Thorn M, Monsees K, Spell R, O’Connor JB. A prospective study of factors that determine cecal intubation time at colonoscopy. Gastrointest Endosc. 2005;61:72-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 150] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Anderson JC, Messina CR, Cohn W, Gottfried E, Ingber S, Bernstein G, Coman E, Polito J. Factors predictive of difficult colonoscopy. Gastrointest Endosc. 2001;54:558-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 179] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 11. | Kim WH, Cho YJ, Park JY, Min PK, Kang JK, Park IS. Factors affecting insertion time and patient discomfort during colonoscopy. Gastrointest Endosc. 2000;52:600-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 159] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 12. | Cirocco WC, Rusin LC. Factors that predict incomplete colonoscopy. Dis Colon Rectum. 1995;38:964-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 140] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Anderson JC, Gonzalez JD, Messina CR, Pollack BJ. Factors that predict incomplete colonoscopy: thinner is not always better. Am J Gastroenterol. 2000;95:2784-2787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 151] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Church JM. Complete colonoscopy: how often? And if not, why not? Am J Gastroenterol. 1994;89:556-560. [PubMed] |
| 15. | Krishnan P, Sofi AA, Dempsey R, Alaradi O, Nawras A. Body mass index predicts cecal insertion time: the higher, the better. Dig Endosc. 2012;24:439-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Liang CM, Chiu YC, Wu KL, Tam W, Tai WC, Hu ML, Chou YP, Chiu KW, Chuah SK. Impact factors for difficult cecal intubation during colonoscopy. Surg Laparosc Endosc Pecutan Tech. 2012;22:443-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Hsu CM, Lin WP, Su MY, Chiu CT, Ho YP, Chen PC. Factors that influence cecal intubation rate during colonoscopy in deeply sedated patients. J Gastroenterol Hepatol. 2012;27:76-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 18. | Hsieh YH, Kuo CS, Tseng KC, Lin HJ. Factors that predict cecal insertion time during sedated colonoscopy: the role of waist circumference. J Gastroenterol Hepatol. 2008;23:215-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Hansen JJ, Ulmer BJ, Rex DK. Technical performance of colonoscopy in patients sedated with nurse-administered propofol. Am J Gastroenterol. 2004;99:52-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Mui LM, Ng EK, Chan KC, Ng CS, Yeung AC, Chan SK, Wong SK, Chung SC. Randomized, double-blinded, placebo-controlled trial of intravenously administered hyoscine N-butyl bromide in patients undergoing colonoscopy with patient-controlled sedation. Gastrointest Endosc. 2004;59:22-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Yoshikawa I, Honda H, Nagata K, Kanda K, Yamasaki T, Kume K, Tabaru A, Otsuki M. Variable stiffness colonoscopes are associated with less pain during colonoscopy in unsedated patients. Am J Gastroenterol. 2002;97:3052-3055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Saunders BP, Fukumoto M, Halligan S, Jobling C, Moussa ME, Bartram CI, Williams CB. Why is colonoscopy more difficult in women? Gastrointest Endosc. 1996;43:124-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Sadahiro S, Ohmura T, Yamada Y, Saito T, Taki Y. Analysis of length and surface area of each segment of the large intestine according to age, sex and physique. Surg Radiol Anat. 1992;14:251-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 94] [Article Influence: 2.8] [Reference Citation Analysis (0)] |