Published online Jan 16, 2018. doi: 10.4253/wjge.v10.i1.10
Peer-review started: August 4, 2017
First decision: September 25, 2017
Revised: November 13, 2017
Accepted: December 4, 2017
Article in press: December 5, 2017
Published online: January 16, 2018
Processing time: 165 Days and 9.7 Hours
Endoscopic ultrasonography (EUS) is considered a superior investigation when compared to conventional ultrasonography for imaging gall bladder (GB) lesions as it can provide high-resolution images of small lesions with higher ultrasound frequencies. Examination of GB is frequently the primary indication of EUS imaging. Imaging during EUS may not remain restricted to one station and multi-station imaging may provide useful information. This review describes the techniques of imaging of GB by linear EUS from three different stations. The basic difference of imaging between the three stations is that effective imaging from station 1 is done above the neck of GB, from station 2 at the level of the neck of GB and from station 3 below the level of the neck of GB.
Core tip: Endoscopic ultrasonography (EUS) is superior investigation than ultrasonography for imaging gall bladder (GB). Different techniques of imaging of GB by EUS have been described by different authors but a standard technique has not been specifically described. We herein discuss the techniques of imaging of GB by linear EUS from three different stations.
- Citation: Sharma M, Somani P, Sunkara T. Imaging of gall bladder by endoscopic ultrasound. World J Gastrointest Endosc 2018; 10(1): 10-15
- URL: https://www.wjgnet.com/1948-5190/full/v10/i1/10.htm
- DOI: https://dx.doi.org/10.4253/wjge.v10.i1.10
Imaging modalities used in evaluating gall bladder (GB) diseases include transabdominal ultrasonography (USG), endoscopic ultrasonography (EUS), computerized tomography, and magnetic resonance imaging[1,2]. Although USG is considered the gold standard for GB imaging, in view of providing high resolution images; EUS has been found to be better than USG for GB lesions imaging[3-6]. Different techniques of imaging by EUS have been described by different authors for GB imaging but a standardized technique has not been mentioned[7-10]. In view of close proximity of GB to the duodenum, usually EUS imaging is restricted to duodenum[11]. Usually, endosonographers performs GB imaging from multiple stations and the initial station of imaging differs among different endosonographers[12,13]. The present review elaborates the various methods of GB imaging by linear EUS.
The GB lies on the visceral surface of the liver. The non-peritoneal upper surface of the GB is attached by connective tissue to a shallow fossa on the liver located between the right lobe and the quadrate lobe. The GB has three segments: The fundus, the body, and the left segment which is the infundibulum or neck. The fundus projects beyond the inferior margin of the liver, is covered completely in peritoneum and is in contact with the anterior abdominal wall. The body tapers towards the neck, which lies in the porta hepatis. The neck or infundibulum is hook-shaped and may show a pouch like dilation toward the right (Hartmann’s pouch). The neck turns sharply downward as it becomes continuous with the cystic duct. The mucous membrane of the cystic duct is raised up into a spiral fold that consists of five to ten irregular turns; it is continuous with a similar fold in the neck of the GB.
The images included in this review were obtained utilizing the linear echoendoscope EG-3830 UT (Pentax, Tokyo, Japan), along with a Hitachi Avius processor (Hitachi, Tokyo, Japan). The EUS image orientation on screen was as follows: Monitor’s right side corresponds to the cranial and left to the caudal end of the patient. Rotation of the echo endoscope is the most crucial aspect to GB imaging. Majority of the movements are performed in a straight position of the echo endoscope, except during EUS imaging from first part of duodenum when the scope is in a J-shaped position. Proper right/left knobs movements along with in/out movement of the echo endoscope are utilized for adequate contact with the gastrointestinal wall for proper EUS imaging.
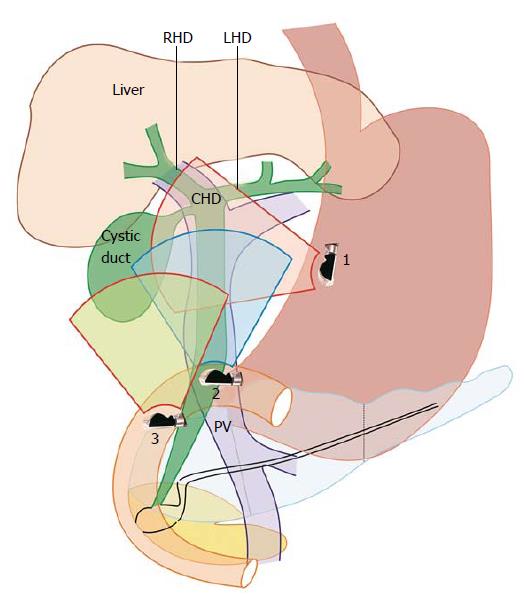
EUS of the GB can be done from the fundus of stomach, duodenal bulb, descending duodenum and antrum. The imaging from duodenal bulb and antrum are almost similar in appearance hence the description is restricted to three stations (Figure 1 and Table 1): (1) the fundus of stomach; (2) duodenal bulb and antrum; and (3) descending duodenum.
| Station | Home base structure | Main position where gall bladder is seen | Part of biliary tract seen on clockwise rotation | Part of biliary tract seen on anti-clockwise rotation |
| Station - 1: OG junction | Joining of right branch of portal vein with left branch of portal vein | Beyond the curving part of portal vein between 6-8 o’clock position | Upper 1/3rd of CBD | Neck of Gall Bladder, Fundus |
| Station - 2: Antrum of stomach/duodenal bulb | Portal vein, superior mesenteric vein | Between 2-4 o’clock position | Lower 1/3rd of CBD | Upper 1/3rd of CBD, neck of Gall Bladder and Fundus, left and right hepatic duct union |
| Station - 3: Descending duodenum | Superior mesenteric vein | Between 9-11 o’clock position | Pancreatic duct | Middle and upper 1/3rd of CBD, neck of gall bladder and fundus, left and right hepatic duct union |
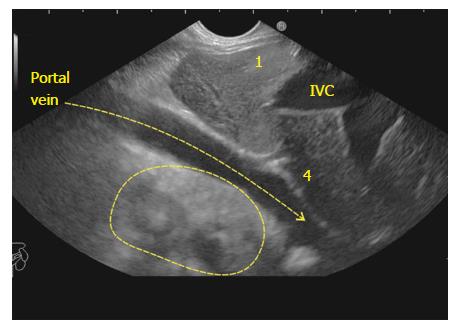
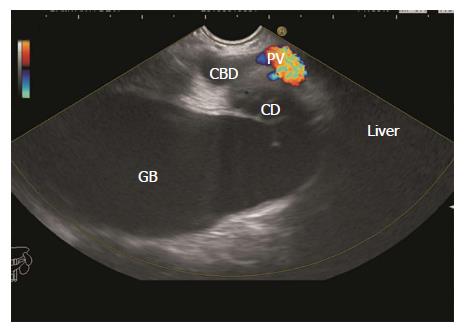
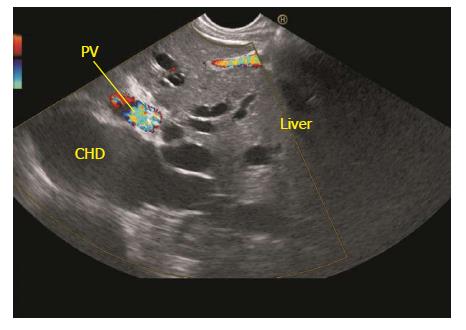
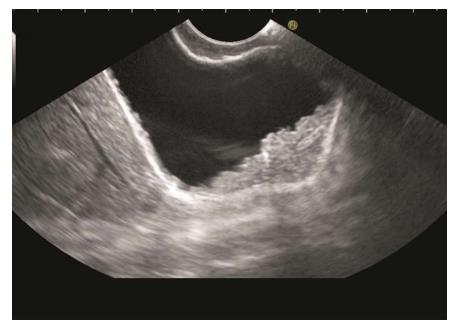
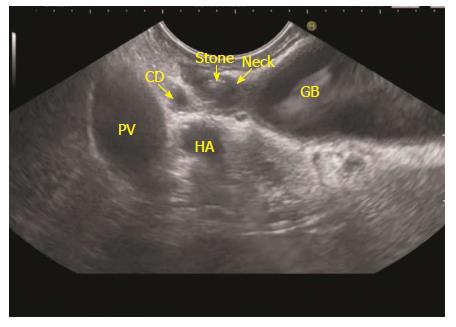
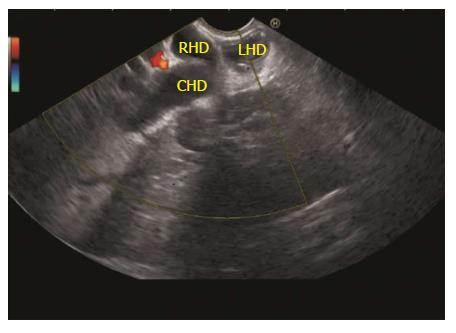
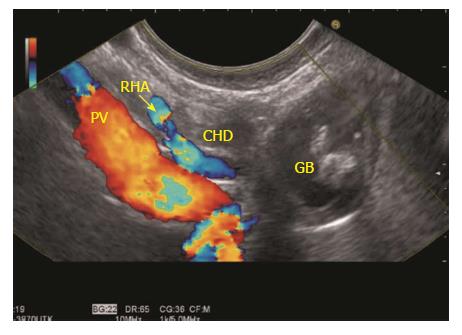
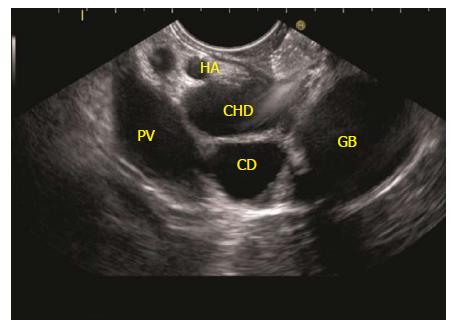
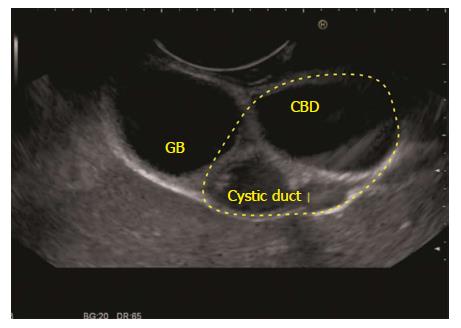
The GB lies on the far side of screen between 6 to 9 o’clock position. Movements near esophagogastric junction (40 cm) should be performed under direct vision to avoid the possibility of perforation. Initially, segment 2 and 3 portal vein tributaries are identified within the left lobe of liver. A clockwise rotation follows the tributaries which form the left branch of portal vein (PV). Further clockwise rotation traces the left branch of PV towards the liver hilum where it is joined by the right branch of PV. After the union the supraduodenal part of PV is seen as a curving vessel going from 9/11 o’clock position to 4/6 o’clock position (Figure 2). The common bile duct (CBD) and GB are seen in the area beyond the curving part of PV in the left lower quadrant of screen (Figure 3). Initially, the CBD and neck of GB are identified just beyond the PV (Figure 4). Imaging of remaining part of GB can be done by following GB down from the fundic part of stomach. This follow down of GB is possible due to EUS probe movement along the lesser curvature along with combination of three smooth movements: (1) Pushing around 25 to 30 cm; (2) 90 degree clockwise rotation; and (3) up movement of up/down knob on echo endoscope for about 90 degree. This combination of movements allows smooth pathway of EUS transducer along the lesser curvature and follows down the GB from neck towards the fundus of GB.
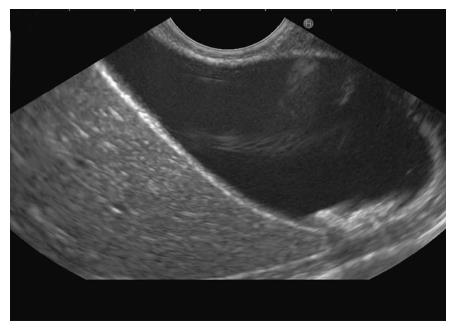
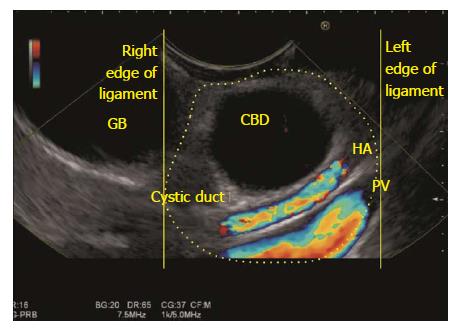
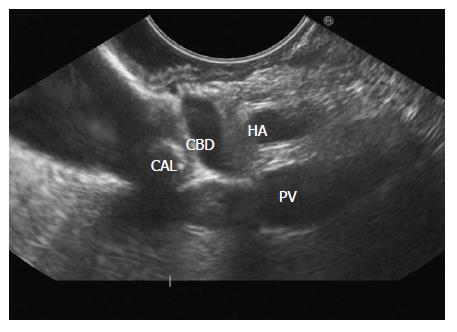
The GB lies close to the probe between 2 to 4 o’clock position. The imaging from the antrum is sometimes best done by pushing the echo endoscope from the body of stomach towards the pylorus with a hyperinflated balloon (Figure 5). The imaging from duodenum can be done without a balloon by passing the scope beyond the pylorus and pushing it into the duodenal bulb apex. The contact with the superior and anterior duodenal wall is established after sucking the air out of the lumen of duodenum, by turning in an anticlockwise direction and by moving the up and down knobs generally in a downward direction (Figures 6-10). Home base position is identified with adequate rotation and minor adjustments of both knobs, where the portal vein is seen on the far side of the screen in a long axis (Figure 11). Clockwise rotation follows the CBD towards the papilla and anticlockwise rotation makes the scanning towards the liver hilum, the upper part of CBD, the cystic duct and GB (Figures 7-9). The CBD and GB are seen in the area between the probe and portal vein and higher up between the probe and liver (Figure 12).
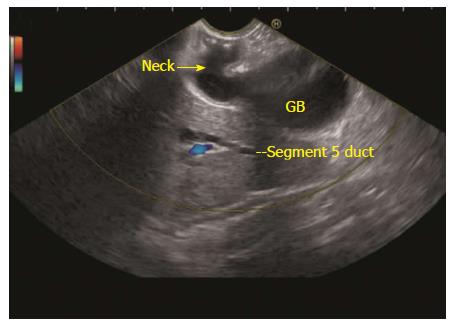
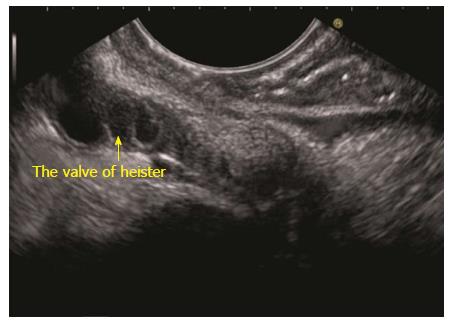
The GB lies close to the probe between 8 to 11 o’clock position. Imaging from descending duodenum requires the entry into 2nd part of duodenum followed by shortening of scope. After entry, multiple times pushing the scope in/out is required to place the echo endoscope into the descending duodenum (3rd part of duodenum). By combining three movements, i.e., slow withdrawal up to the duodenal bulb, clockwise/anticlockwise torque and upward movement of the up/down knobs in third part of duodenum, there is better visualization of lower one third of CBD. The combination of three movements should be done with a main emphasis on anticlockwise rotation. During this rotation the superior mesenteric vein can be followed all the way towards the hilum where the portal vein is seen in a rounded axis within the hepatoduodenal ligament. The anechoic bile duct can be identified and followed all the way to the liver hilum (Figures 13-15). The continuity of CBD can be seen with the cystic duct and GB. Sometimes the valve of heister can be visualized within the cystic duct (Figure 16).
The techniques described in the present paper are likely to provide the images as discussed in most of the cases and from majority of the stations. However, the reproducibility of the images may be compromised in the duodenal bulb due to the variability of the scope position and due to the balloon use. The basic concept of GB imaging by linear EUS is simple: Station 1 shows the GB at around 6 o’clock position, station 2 shows the GB at around 3 o’clock position and station 3 shows the GB at around 9 o’clock position. The difference between the three imaging is that effective imaging in station 1 lies above the neck of GB, in station 2 lies at the level of the neck of GB and station 3 lies below the level of the neck of GB. These techniques will be useful for evaluation of different kind of pathologies of GB by EUS[14-22].
Pran Prakash (Graphic designer) for his contribution in making figures and table.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kikuyama M, Souza JLS, Yan SL S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Dietrich CF. Endoscopic Ultrasound: An Introductory manual and Atlas. New York: Thieme 2006; . [DOI] [Full Text] |
| 2. | Van Dam S, Sivak MV. Gastrointestinal Endosonography. Philadelphia, Pennsylvania: Saunders 1999; . |
| 3. | Rosch T, Will U, Chang KJ. Logitudianl Endosonography: Atlas and Manual for Use in the Upper Gastrointestinal Tract. 2001;. |
| 4. | Gress FG, Ishan B. Endoscopic Ultrasonography. Massachusetts: Wiley-Blackwell 2001; . |
| 5. | Al-Haddad M. EUS in Bile Duct, Gallbladder, and Ampullary Lesions. Hawes, Paul Fockens, Shyam Varadarajulu. Endosonography. Philadelphia: Saunders 2015; 226-255 Available from: https://www.us.elsevierhealth.com/endosonography-9780323221511.html. |
| 6. | Rameshbabu CS, Wani ZA, Rai P, Abdulqader A, Garg S, Sharma M. Standard imaging techniques for assessment of portal venous system and its tributaries by linear endoscopic ultrasound: a pictorial essay. Endosc Ultrasound. 2013;2:16-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 7. | Sharma M, Rai P, Rameshbabu CS, Arya S. Imaging of the pancreatic duct by linear endoscopic ultrasound. Endosc Ultrasound. 2015;4:198-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Sharma M, Pathak A, Rameshbabu CS, Rai P, Kirnake V, Shoukat A. Imaging of pancreas divisum by linear-array endoscopic ultrasonography. Endosc Ultrasound. 2016;5:21-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Sharma M, Rai P, Rameshbabu CS, Senadhipan B. Imaging of peritoneal ligaments by endoscopic ultrasound (with videos). Endosc Ultrasound. 2015;4:15-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Sharma M, Rai P, Mehta V, Rameshbabu CS. Techniques of imaging of the aorta and its first order branches by endoscopic ultrasound (with videos). Endosc Ultrasound. 2015;4:98-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Sharma M, Rameshbabu CS, Dietrich CF, Rai P, Bansal R. Endoscopic ultrasound of the hepatoduodenal ligament and liver hilum. Endosc Ultrasound. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Pathak A, Shoukat A, Thomas NS, Mehta D, Sharma M. Seagulls of endoscopic ultrasound. Endosc Ultrasound. 2017;6:231-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Owen CC, Bilhartz LE. Gallbladder polyps, cholesterolosis, adenomyomatosis, and acute acalculous cholecystitis. Semin Gastrointest Dis. 2003;14:178-188. [PubMed] |
| 14. | Sun XJ, Shi JS, Han Y, Wang JS, Ren H. Diagnosis and treatment of polypoid lesions of the gallbladder: report of 194 cases. Hepatobiliary Pancreat Dis Int. 2004;3:591-594. [PubMed] |
| 15. | Mitake M, Nakazawa S, Naitoh Y, Kimoto E, Tsukamoto Y, Asai T, Yamao K, Inui K, Morita K, Hayashi Y. Endoscopic ultrasonography in diagnosis of the extent of gallbladder carcinoma. Gastrointest Endosc. 1990;36:562-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 40] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Vijayakumar A, Vijayakumar A, Patil V, Mallikarjuna MN, Shivaswamy BS. Early diagnosis of gallbladder carcinoma: an algorithm approach. ISRN Radiol. 2012;2013:239424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Kapoor A, Kapoor A, Mahajan G. Differentiating malignant from benign thickening of the gallbladder wall by the use of acoustic radiation force impulse elastography. J Ultrasound Med. 2011;30:1499-1507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Sugiyama M, Atomi Y, Yamato T. Endoscopic ultrasonography for differential diagnosis of polypoid gall bladder lesions: analysis in surgical and follow up series. Gut. 2000;46:250-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 94] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Azuma T, Yoshikawa T, Araida T, Takasaki K. Differential diagnosis of polypoid lesions of the gallbladder by endoscopic ultrasonography. Am J Surg. 2001;181:65-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 67] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Yang HL, Sun YG, Wang Z. Polypoid lesions of the gallbladder: diagnosis and indications for surgery. Br J Surg. 1992;79:227-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 146] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Gallahan WC, Conway JD. Diagnosis and management of gallbladder polyps. Gastroenterol Clin North Am. 2010;39:359-367, x. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 22. | Yang LP, Yang ZL, Tan XG, Miao XY. [Expression of annexin A1 (ANXA1) and A2 (ANXA2) and its significance in benign and malignant lesions of gallbladder]. Zhonghua Zhongliu Zazhi. 2010;32:595-599. [PubMed] |