INTRODUCTION
Endoscopic clipping devices were developed by Hachisu in cooperation with Olympus Co. Ltd. (Japan) in 1980s[1]. For more than two decades, endoclips have become available worldwide with continuous technical improvements. Numerous trials and a meta-analysis have shown that clipping is an effective hemostatic method for bleeding peptic ulcers, with high rates of primary hemostasis (85%-100%), low rebleeding rates (2%-20%) and an excellent safety record[2-6]. Currently, clipping is an established mandatory technique of endoscopic hemostasis for nonvariceal upper gastrointestinal bleeding, including Mallory-Weiss syndrome[7], duodenal diverticular bleeding, Dieulafoy lesions of the stomach[8] and duodenum[9,10], as well as bleeding peptic ulcers. More recently, clipping has been widely applied to the hemostasis of lower gastrointestinal bleeding and non-hemostatic treatments including closing mucosal defects, leaks and perforations, and marking lesions prior to radiotherapy or surgery. In this review, we discuss the safety and efficacy of endoscopic clipping for the management of colonic diseases.
TECHNOLOGY OF CLIPPING DEVICES
Currently available clipping devices consist of a handle-delivery catheter system that enables development of double-pronged stainless steel clips to mechanically compress the targeted vessels and/or close a mucosal defect by tissue approximation[6]. Clipping avoids chemically or thermally induced ulceration, and thus causes minimal mucosal injury. The spectrum of devices has been expanded by the introduction of ready-to-use (disposable) clip systems and a variety of new clips distributed by several manufacturers. However, an experimental setting disclosed that operator familiarity with clipping rather than the particular clip was of relevance for successful hemostasis[11]. Applied clips slough spontaneously at approximately 2-3 wk and pass uneventfully. Clipping-induced complications are extremely rare.
CLIPPING FOR LOWER GASTROINTESTINAL TRACT DISEASES
Clipping has now been applied to various indications in the lower gastrointestinal tract, which include hemostasis for colonic diverticular bleeding, postpolypectomy bleeding, Dieulafoy lesions, acute hemorrhagic rectal ulcer, closure of colonic perforations and leaks, and identifying anatomic landmarks.
DIVERTICULAR BLEEDING
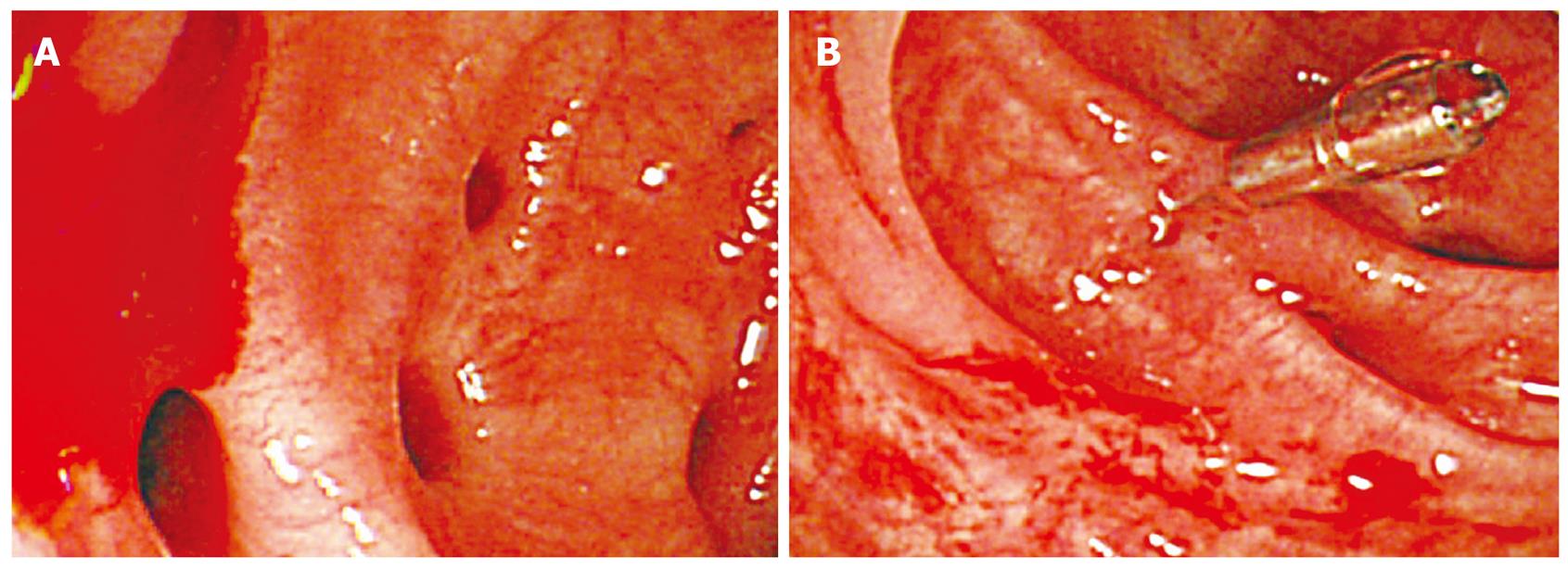
Diverticular bleeding is one of the most common causes of lower gastrointestinal bleeding. Urgent colonoscopy offers not only a diagnostic method but also a therapeutic maneuver for its management[12]. Colonoscopic hemostatic methods including adrenaline injection, thermal and electrical coagulation or combinations of these have been applied, until first reports of the efficacy of endoscopic clipping for colonic diverticular bleeding[13]. In recent times, the impact of clipping for this disorder has been increasing worldwide[14-20]. Although these reports were small case series and there are no data comparing the efficacy and safety of the various endoscopic hemostatic methods available, evidence of the safety and efficacy of clipping for colonic diverticular bleeding has been provided. Mechanical hemostasis by hemoclip application confers a theoretically decreased risk of perforation compared with thermal application in the thin-walled diverticula[21]. The clips have been placed across the margin of the diverticulum (Figure 1) or in a sequential zipper fashion, as well as directly to the vessel. In addition, retained clips may serve as a potential fluoroscopic marker to guide angiographic therapy or surgical intervention, if necessary. It is sometimes difficult to identify the stigmata of bleeding diverticulum because diverticula often are numerous and bleeding may be intermittent. Poor visualization without oral preparation is another difficulty.
Figure 1 Endoscopic clipping for the treatment of colonic diverticular bleeding.
A: An actively bleeding colonic diverticulum of the ascending colon in a 78-year-old man with chronic obstructive pulmonary disease; B: Hemostasis was achieved with a clip.
POSTPOLYPECTOMY BLEEDING
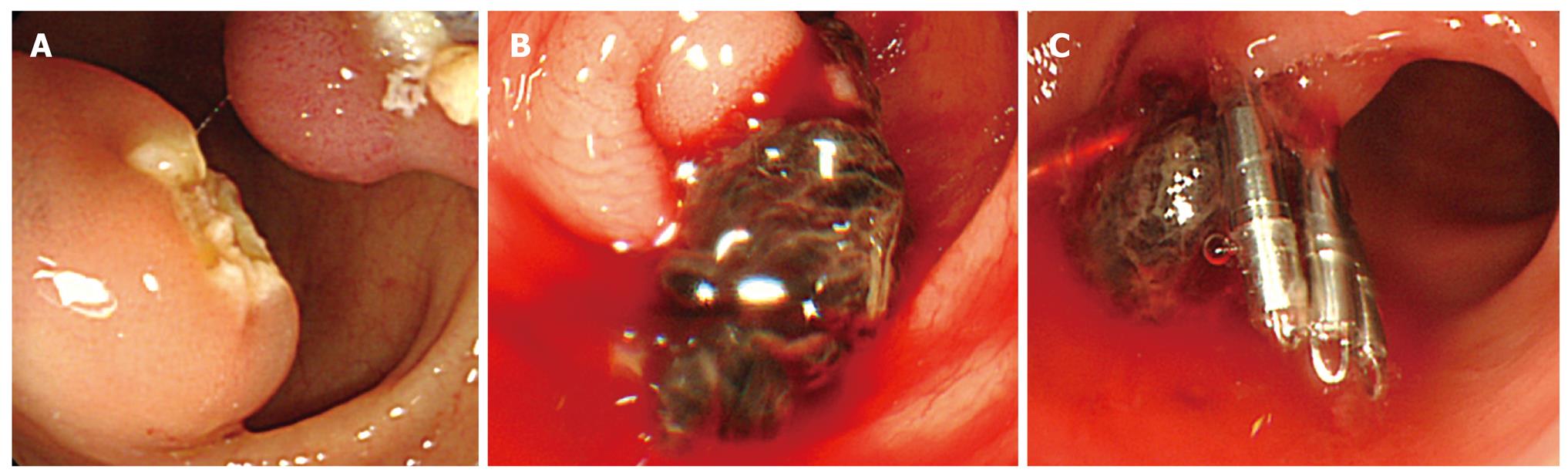
Postpolypectomy bleeding is the most frequent complication of colonoscopy, which occurs in approximately 1% of the procedures. Most cases can be managed conservatively, however, colonoscopic intervention is often required for continuous bleeding. Endoclips have been used successfully for immediate and delayed postpolypectomy bleeding[1,22]. Clipping is effective in controlling immediate postpolypectomy bleeding as well as resnaring. Despite these excellent results, there are no comparative studies of clipping versus thermal modalities. In immediate postpolypectomy bleeding, there are several possible approaches to apply clips effectively. For bleeding from a pedunculated polyp stalk or its base, the clipping is most effective when deployed across the stalk or the base to ligate the feeding vessels. For bleeding from a sessile polyp removed by endoscopic mucosal resection, the bleeding point should be clipped, followed by closure of the mucosal defect. Delayed postpolypectomy bleeding is usually caused by ulceration at the site of the polypectomy (Figure 2). Clipping is regarded as a more ideal hemostatic maneuver than cautery for this situation, because the postpolypectomy sites usually change to thermal ulcers and thus additional thermal or injection hemostatic methods may cause perforation in thin-walled colon. Although prospective randomized studies are warranted, early clipping certainly provides a safe and effective hemostasis for immediate and delayed postpolypectomy bleeding and reduces the need for transfusion and hospitalization[23].
Figure 2 Endoscopic clipping for the treatment of postpolypectomy bleeding.
A: A semipedunculated polyp was treated by an endoscopic mucosal resection technique in the sigmoid colon in a 64-year-old man with hypertension; B: Active bleeding occurred at the postpolypectomy ulcer on the next day; C: Hemostasis was achieved with clips.
The effectiveness of prophylactic clipping to prevent delayed postpolypectomy bleeding is controversial. A retrospective study of prophylactic clipping for large polyps (15-40 mm in diameter) indicated a potential for prevention[24]. In comparison, a prospective randomized controlled trial comparing the prophylactic clipping group after endoscopic mucosal resection (n = 205) and the non-clipping group (n = 208) disclosed that clipping did not decrease the occurrence of delayed bleeding (0.98% versus 0.96%, respectively)[25]. In their study, most polyps were small with a mean diameter of 7.8 mm. Although there is an argument regarding the study’s sample size, it is possible that prophylactic clipping might be effective when only larger polyps are included[26]. More recently, a large retrospective cohort study of 6617 polypectomies in 3138 patients clearly showed the risk factors of delayed postpolypectomy bleeding[27]. Hemorrhage occurred in 38 lesions (0.57%) and 37 patients (1.2%). Polyps larger than 10 mm in diameter were at a 4.5 times higher bleeding risk than smaller ones, and hypertension was the strongest patient-related predictive factor with an adjusted odds ratio of 5.6. Twenty-two patients were actively bleeding at the second colonoscopy, all of which were successfully treated with clipping.
The present perspective on colonoscopy is more complicated in older patients. Because colonic polyps are an age-related disease, polypectomies are usually performed in the elderly, who are more likely to be taking anticoagulants as well as antihypertensive medication[28]. Another interesting retrospective study of 41 polypectomies in 21 patients showed that prophylactic clipping immediately after polypectomy prevented bleeding while continuing anticoagulation therapy (international normalized ration, average 2.3, range 1.4-4.9)[29]. Although the average polyp size was 5.0 mm (3-10 mm) and the study sample was small, it has been stressed that prophylactic clipping may be helpful for anticoagulated patients at high risk of thrombosis.
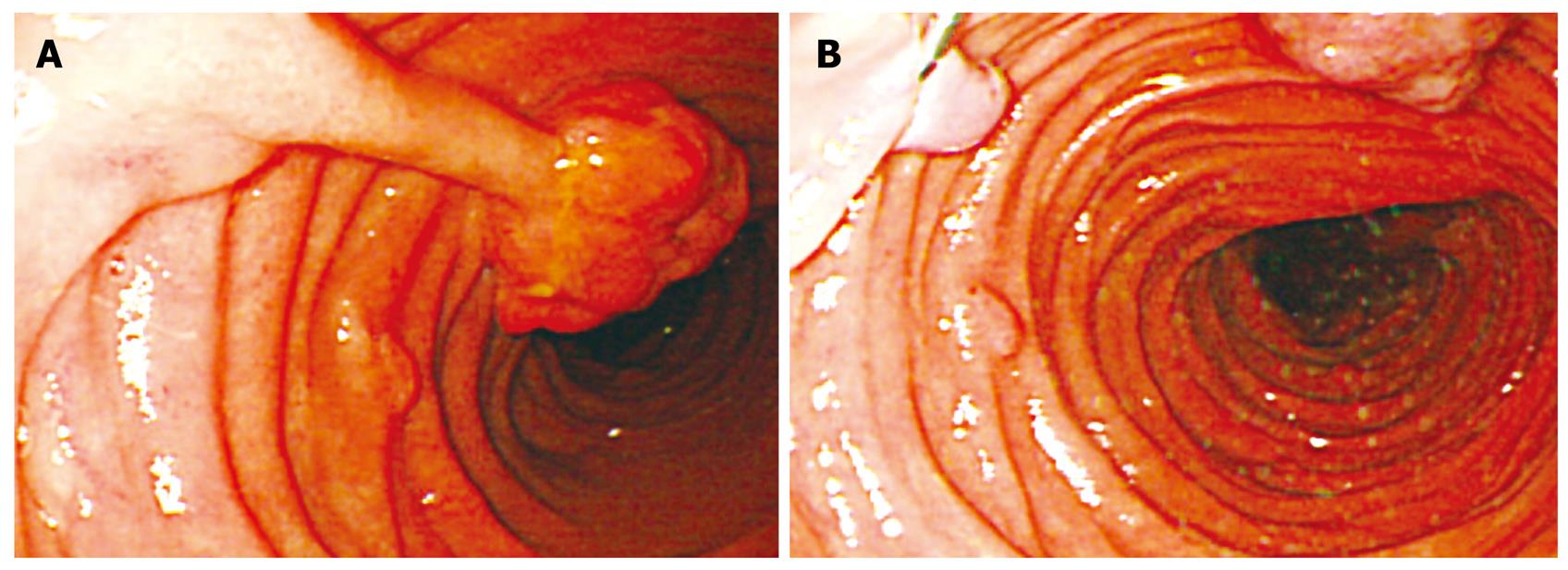
Polypectomy techniques among endoscopists is highly variable. An interesting survey disclosed that 80% of practicing endoscopists had never performed clipping on polypectomy stalks for prevention of bleeding and that academic physicians were more likely to place hemoclips on these stalks than private physicians[30]. Considering that postpolypectomy bleeding occurs in 0.57% of polypectomies[27], and if it is assumed that clipping would reduce this rate to 0%, this would yield 175 polyps needing to be prophylactically clipped to prevent one episode of bleeding[31]. It is reasonable that most physicians think it is neither practical nor cost-effective. Meanwhile, the advanced technique of endoscopic mucosal resection followed by immediate clipping for flat or depressed colonic neoplasms has been increasingly utilized[32]. Therefore, prospective randomized studies are needed to evaluate prophylactic clipping to prevent postpolypectomy bleeding in high-risk patients or with large polyps. Until such evidence is available, we believe that clipping certainly is one of the best strategies to prevent and treat postpolypectomy bleeding in high-risk patients[33] and with large polyps on the basis of our clinical experiences (Figure 3).
Figure 3 Endoscopic clipping for the prophylactic management to prevent delayed postpolypectomy bleeding.
A: A pedunculated polyp of the ileum in a 28-year-old man with Peutz-Jeghers syndrome; B: After application of a clip at the base of the long stalk to prevent delayed bleeding, the polyp was resected by snare.
OTHER DISEASES
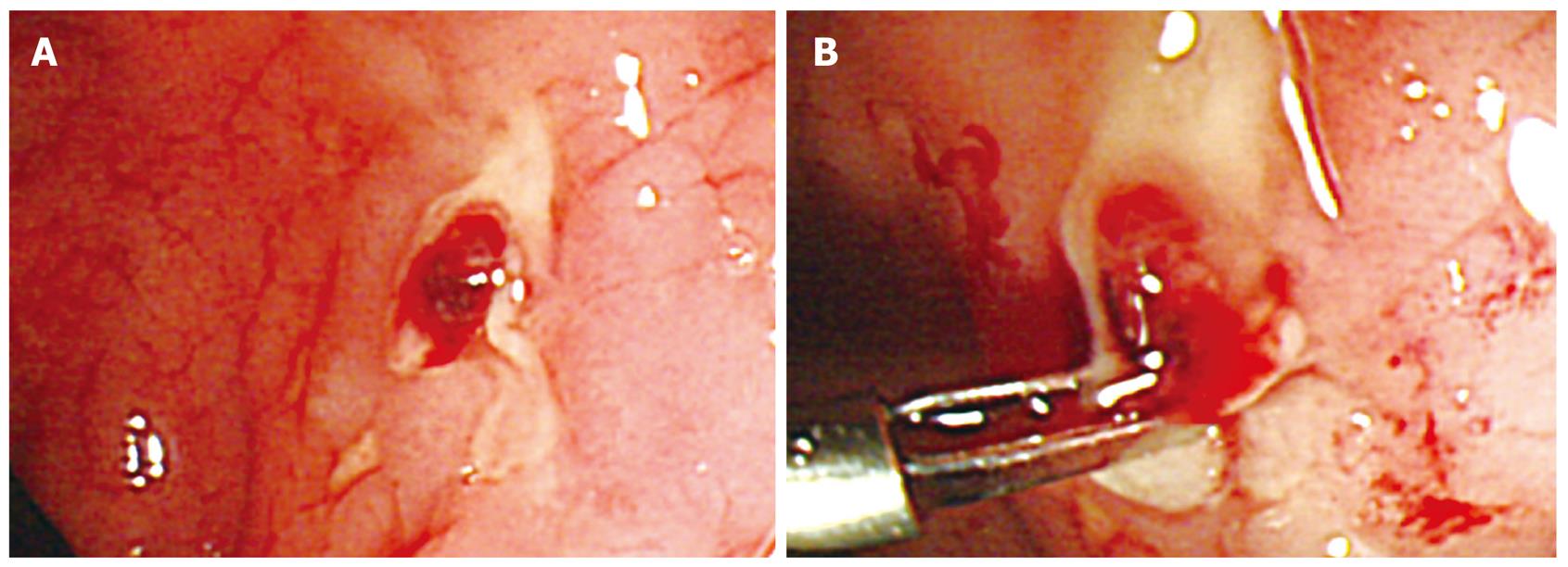
Despite the lack of comparative trials, clipping seems to be effective for the treatment of colorectal Dieulafoy lesions[34], acute hemorrhagic rectal ulcer (Figure 4)[35-37], and exposed vessels in inflammatory bowel diseases. In addition to hemostasis, clipping has been applied to endoluminal repair of iatrogenic colonic perforations, which were caused by diagnostic or therapeutic colonoscopy, to avoid surgery with a high successful rate[38].
Figure 4 Endoscopic clipping for the treatment of acute hemorrhagic rectal ulcer.
A: An exposed vessel of the rectal ulcer in a bed-ridden 70-year-old man with liver cirrhosis and severe burn; B: A clip was directly applied to the vessel.
CONCLUSION
Endoscopic clipping has been shown to be a safe and effective method of hemostasis for lower gastrointestinal bleeding including diverticular bleeding, postpolypectomy bleeding and other hemorrhagic diseases. Further studies are needed to evaluate prophylactic clipping to prevent postpolypectomy bleeding in high-risk patients.
Peer reviewer: William Robert Brugge, MD, Professor, Gastrointestinal Unit, Blake 452C Massachusetts General Hospital, Boston, MA 02114, United States
S- Editor Zhang HN L- Editor Lutze M E- Editor Ma WH