Copyright
©The Author(s) 2016.
World J Gastrointest Endosc. Jan 25, 2016; 8(2): 56-66
Published online Jan 25, 2016. doi: 10.4253/wjge.v8.i2.56
Published online Jan 25, 2016. doi: 10.4253/wjge.v8.i2.56
Figure 1 “Bird-beak” esophagram.
Barium esophagram of a 16-year-old male demonstrating a dilated proximal esophagus with smooth tapering distally; findings consistent with achalasia.
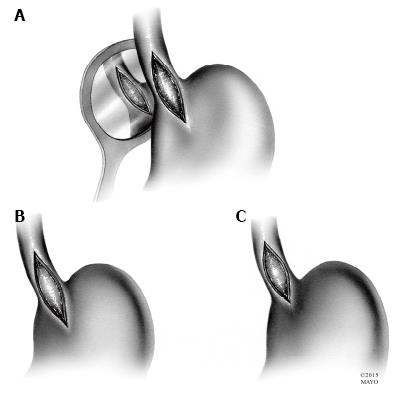
Figure 2 Esophageal myotomies.
A: The original Heller myotomy, consisting of both anterior and posterior disruption of esophageal fibers; B: The most commonly performed Heller myotomy, with extension onto the stomach for 2-3 cm; C: Heller myotomy with minimal extension onto the stomach.
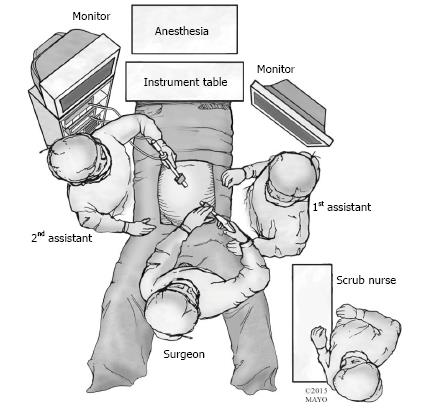
Figure 3 Patient positioning and operating room setup.
The patient is placed in the modified lithotomy position and the surgeon stands between the patient’s legs. First and second assistants are to the right and left of the patient.
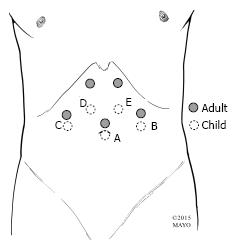
Figure 4 Trocar placement.
Example trocar arrangements. A: Laparoscope; B: Babcock clamp or instrument to divide short gastrics; C: Liver retractor; D and E: Ports for dissecting and suturing; E: Electrocautery or ultrasonic shears for myotomy. The laparoscope is generally placed through a transumbilical port in children. The remaining ports are usually placed more caudad than in adults, with variable size (3 mm or 5 mm, rarely 10 mm), location, and function depending on patient body size/habitus and surgeon preference.
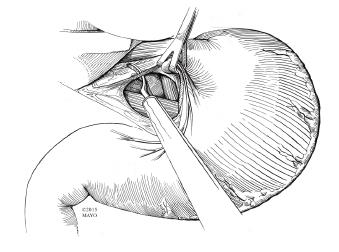
Figure 5 Incision of the gastrohepatic ligament.
After retraction of the liver cephalad, the gastrohepatic ligament is incised and the lesser sac is entered. Blunt dissection is used to first identify the right crus of the diaphragm.
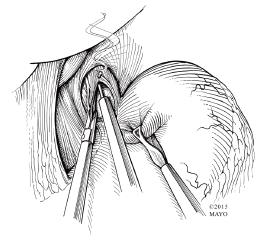
Figure 6 Myotomy with hook cautery.
Electrocautery is used to begin the myotomy. It is performed at the 11 o’clock position on the anterior surface of the esophagus, taking care to avoid injury to the overlying vagus nerve. Once the submucosa is visible, blunt dissection is then typically employed to fully expose the mucosa.
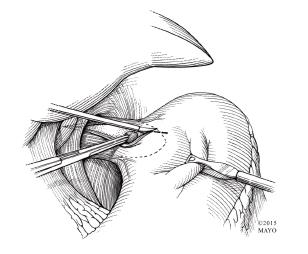
Figure 7 Myotomy with sharp and blunt dissection.
Sharp and blunt dissection avoid the risk of thermal injury to the mucosa during myotomy.
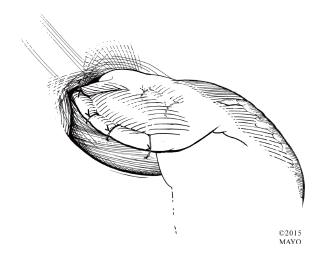
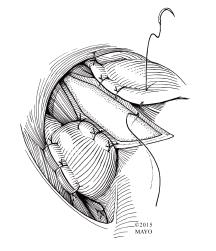
Figure 8 Anterior (Dor) fundoplication.
The anterior (Dor) fundoplication is the most common fundoplication performed in children undergoing laparoscopic Heller myotomy. The fundus of the stomach is rolled over the myotomy and secured to the right and left edges of the cut esophageal muscle and crura. The myotomy is concealed. Additional stitches are placed from the anterior gastric fundus to the rim of the esophageal hiatus to relieve tension from the right sided sutures.
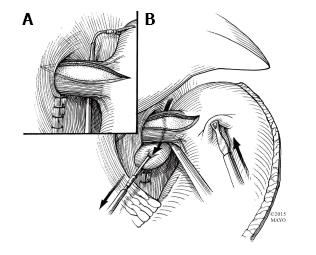
Figure 9 Passing gastric fundus posteriorly for Toupet fundoplication.
A: Once the fundus is fully mobilized, it is handled by passing a grasper from right to left, posterior to the esophagus and gastroesophageal junction; B: The fundus is then pulled to the right and toward the right cut edge of the myotomy.
Figure 10 Posterior (Toupet) fundoplication.
The stomach is secured to the right and left crura as well as the right and left cut edges of esophageal muscle, completing the posterior fundoplication. The myotomy remains exposed.
- Citation: Pandian TK, Naik ND, Fahy AS, Arghami A, Farley DR, Ishitani MB, Moir CR. Laparoscopic esophagomyotomy for achalasia in children: A review. World J Gastrointest Endosc 2016; 8(2): 56-66
- URL: https://www.wjgnet.com/1948-5190/full/v8/i2/56.htm
- DOI: https://dx.doi.org/10.4253/wjge.v8.i2.56