Copyright
©The Author(s) 2015.
World J Gastrointest Endosc. May 16, 2015; 7(5): 496-509
Published online May 16, 2015. doi: 10.4253/wjge.v7.i5.496
Published online May 16, 2015. doi: 10.4253/wjge.v7.i5.496
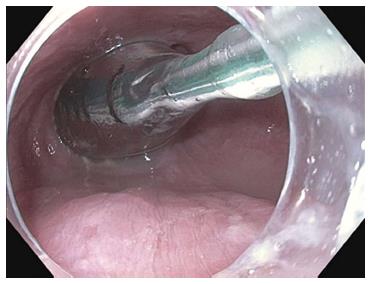
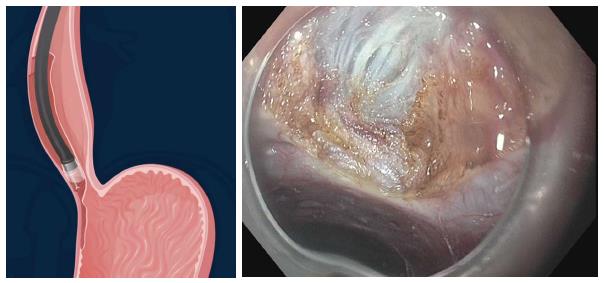
Figure 1 Endosocopic image of the endoluminal functional lumen imaging probe assessing the esophagogastric junction via impedence planimetry.
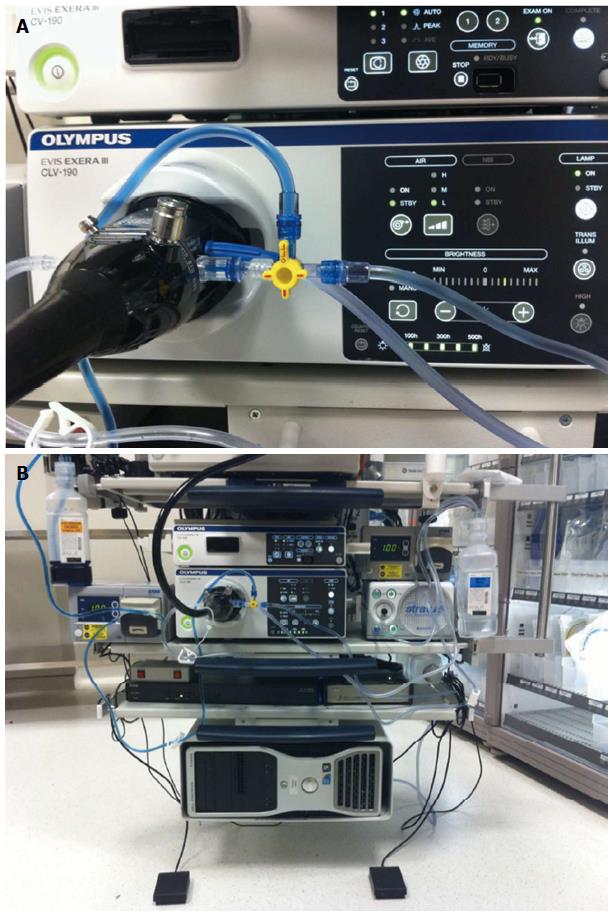
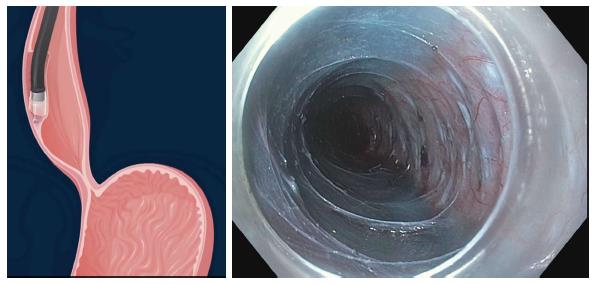
Figure 2 Endoscope setup for jet injection of dyed saline.
A: One bottle of saline and a second bottle of saline mixed with indigo carmine are directly connected to the water jet channel via a stopcock; B: Separate foot pedals control injection of either pure saline for optimizing visual field or dyed saline for submucosal tunneling.
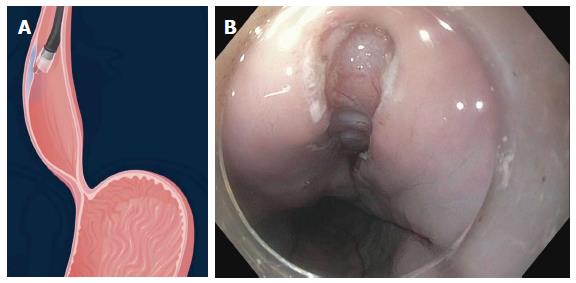
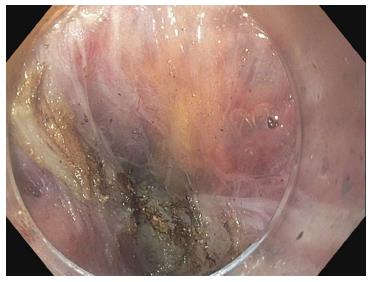
Figure 3 Longitudinal mucosal incision 1.
5 to 2 cm on the anterior esophageal wall.
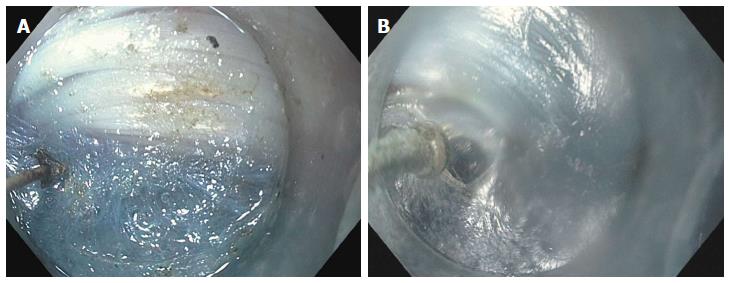
Figure 4 Creation of the submucosal tunnel.
A: Dissection of the submucosal fibers using spray coagulation with the triangular tip knife (KD 640L, Olympus, Center Valley, PA, United States); B: Dissection of the submucosal fibers using the hybridKnife (ERBE, Tubingen, Germany) which allows for both submucosal dissection and fluid injection into the submucosal space.
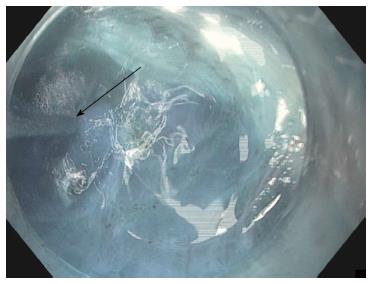
Figure 5 Repeated jet injection (arrow) of dyed saline is performed during submucosal tunneling to improve the demarcation between the submucosal layer and muscularis propria whenever the submucosal dissection plane becomes unclear.
Figure 6 Submucosal tunnel after the submucosal fibers have been dissected away.
The myotomy can now be commenced.
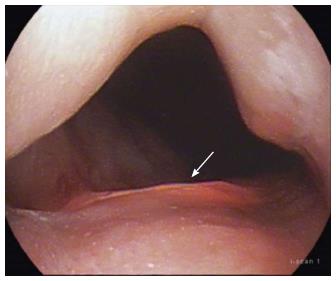
Figure 7 Transillumination can be seen 2 cm below the gastroesophageal junction indicating that the submucosal tunnel can be extended a further 1 cm prior to commencing the myotomy.
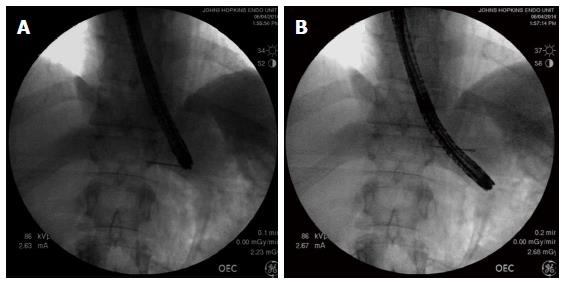
Figure 8 Using fluoroscopy to assess the adequacy of gastric myotomy during peroral endoscopic myotomy.
A: The needle is fluoroscopically lined up with the tip of the endoscope and leveled with the EGJ; B: The endoscope has a diameter of 1 cm, and therefore, the endoscope tip is measured to be 3 cm below the needle marking the EGJ. EGJ: Esophagogastric junction.
Figure 9 Selective myotomy of the circular muscle fibers.
The longitudinal muscle fibers have been preserved.
Figure 10 Splitting of the longitudinal muscle fibers despite attempted selective cardiomyotomy.
Peritoneal fat can be seen through the translucent adventitia.
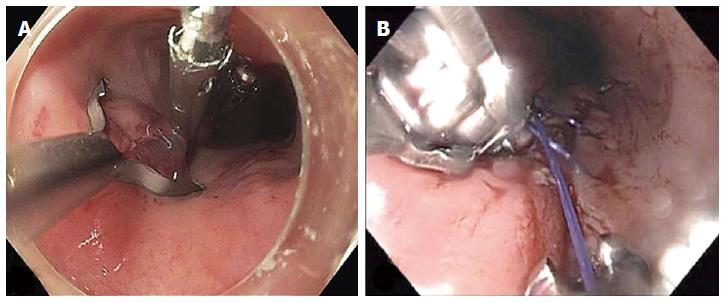
Figure 11 Closure of the mucosal entry after completion of the myotomy.
A: A posterior mucosal incision was closed with three endoscopic clips; B: A posterior mucosal incision was closed with a running suture pattern using transoral flexible endoscopic suturing (OverStitch; Apollo Endosurgery, Austin, TX, United States).
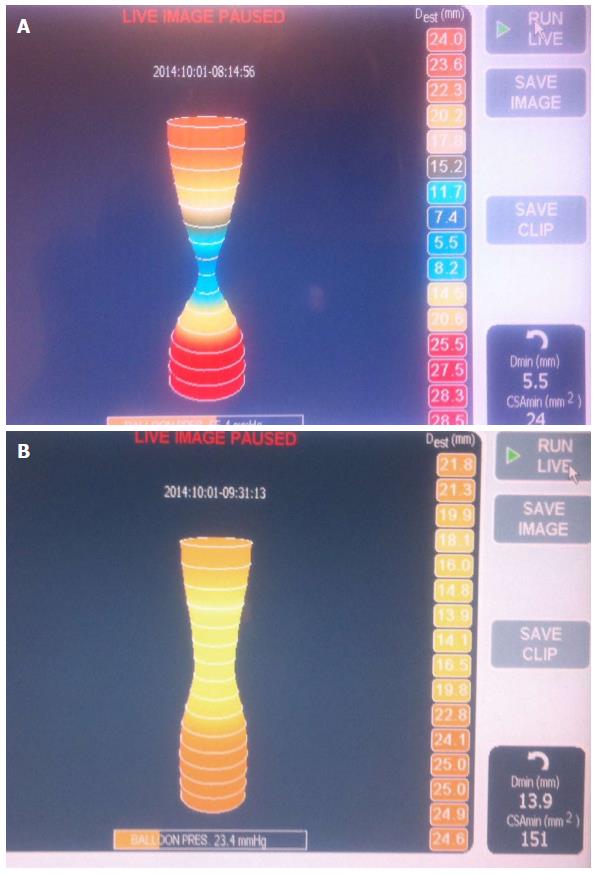
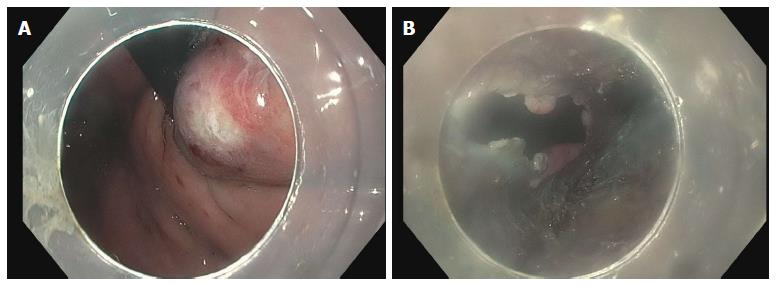
Figure 12 Endoluminal functional lumen-imaging probe (EndoFLIP; Crospon, Galway, Ireland).
A: EndoFLIP measurements performed prior to commencement of POEM. A tight hourglass shape at the EGJ can be seen; B: On completion of the myotomy the waist is widened with a corresponding increase in the distensibility index. POEM: Peroral endoscopic myotomy; EGJ: Esophagogastric junction.
Figure 13 Inadvertent mucosotomy at the gastric cardia.
A: Coagulation injury seen on the gastric mucosa at the level of the cardia during the process of submucosal tunneling; B: The procedure continued, however, on completion of the myotomy a frank 12 mm mucosotomy was now present.
Figure 14 Bleeding encountered during gastric myotomy.
This was treated with the use of coagulation graspers.
- Citation: Kumbhari V, Khashab MA. Peroral endoscopic myotomy. World J Gastrointest Endosc 2015; 7(5): 496-509
- URL: https://www.wjgnet.com/1948-5190/full/v7/i5/496.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i5.496