Copyright
©The Author(s) 2015.
World J Gastrointest Endosc. Mar 16, 2015; 7(3): 213-223
Published online Mar 16, 2015. doi: 10.4253/wjge.v7.i3.213
Published online Mar 16, 2015. doi: 10.4253/wjge.v7.i3.213
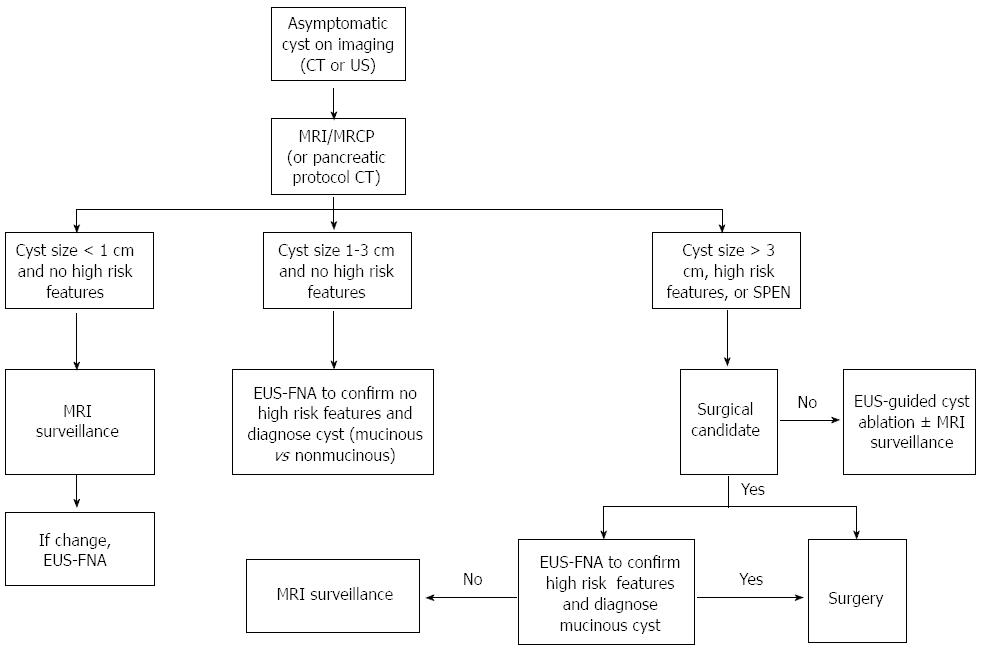
Figure 1 Approach using endoscopic ultrasound in the diagnosis of asymptomatic pancreatic cystic lesions.
CT: Computed tomography; EUS: Endoscopic ultrasound; EUS-FNA: Endoscopic ultrasound-guided fine needle aspiration; MRCP: Magnetic resonance cholangiography; MRI: Magnetic resonance imaging; SPEN: Solid pseudopapillary neoplasm; US: Ultrasound.
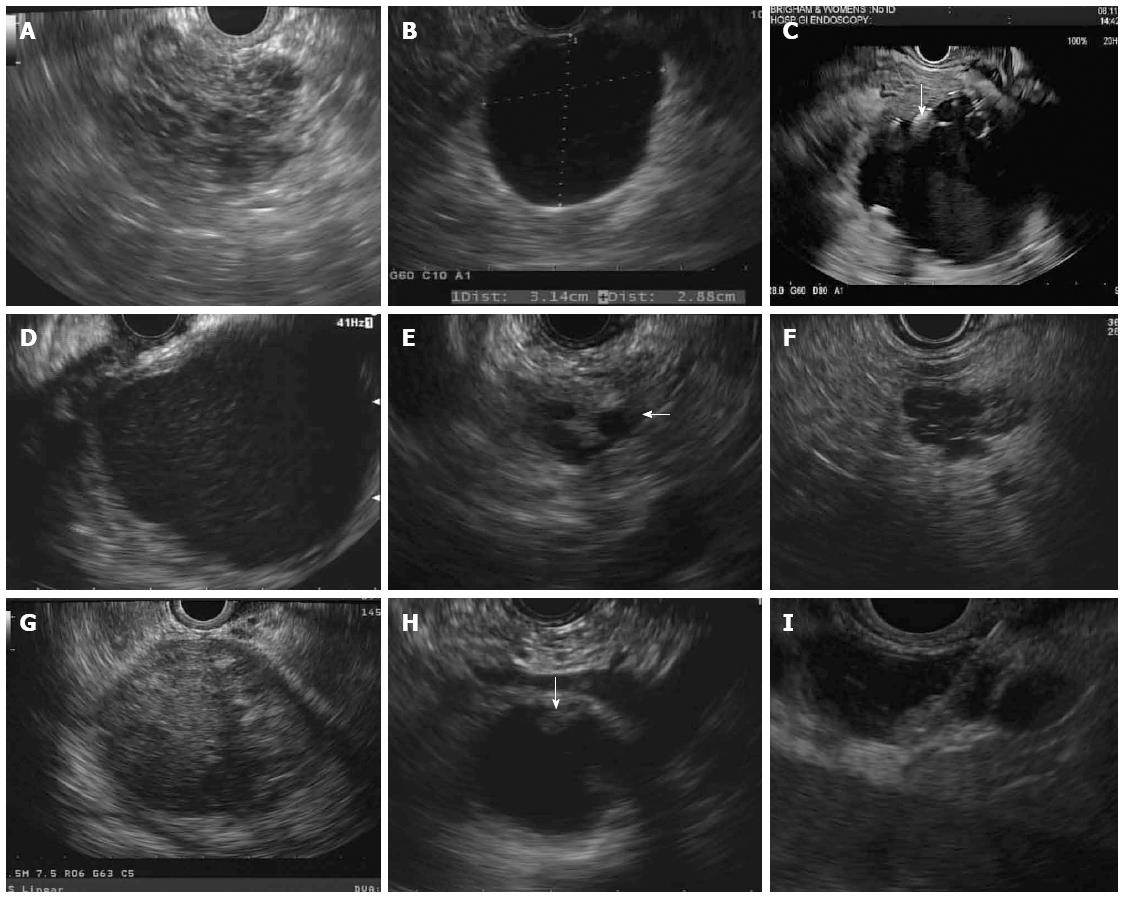
Figure 2 Endoscopic ultrasound imaging.
A: A lobular microcystic lesion consistent with serous cystadenoma; B: A smooth, unilocular, thin walled cyst consistent with mucinous cystic neoplasm; C: A cyst with peripheral calcification (arrow) and debris layering at the bottom of the cyst consistent with pseudocyst; D: A thick walled cyst filled with debris representing walled-off pancreatic necrosis; E: A cyst communicating with a nondilated main pancreatic duct (arrow) representing branch duct intraductal papillary mucinous neoplasm; F: A multiseptated lobular cyst appearing like a “cluster of grapes” consistent with branch duct intraductal papillary mucinous neoplasm; G: A well-defined heterogeneous mass-like lesion with hyperechoic foci and small anechoic focus diagnosed as solid pseudopapillary neoplasm on cytology; H: A unilocular cyst with mucus (arrow) appearing hypoechoic relative to the adjacent pancreatic parenchyma with a smooth hyperechoic rim; I: Endoscopic ultrasound-guided fine needle aspiration of a nodule which appears isoechoic with pancreatic parenchyma without a hyperechoic rim within a dilated main pancreatic duct. Cytology showed adenocarcinoma.
- Citation: Kadiyala V, Lee LS. Endosonography in the diagnosis and management of pancreatic cysts. World J Gastrointest Endosc 2015; 7(3): 213-223
- URL: https://www.wjgnet.com/1948-5190/full/v7/i3/213.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i3.213