Copyright
©The Author(s) 2015.
World J Gastrointest Endosc. Oct 10, 2015; 7(14): 1114-1128
Published online Oct 10, 2015. doi: 10.4253/wjge.v7.i14.1114
Published online Oct 10, 2015. doi: 10.4253/wjge.v7.i14.1114
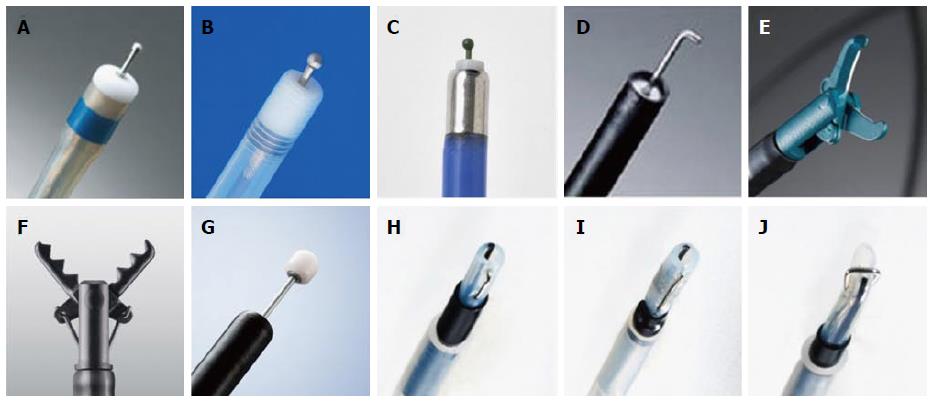
Figure 1 Distal attachments for colorectal endoscopic submucosal dissection.
A: D-201; B: F-050; C: M-02; D: Short ST-hood.
Figure 2 Various types of endoknives used for colorectal endoscopic submucosal dissection.
A: DualKnife; B: FlushKnife BT; C: Jet B-knife; D: Hooknife; E: SBknifeJr; F: Clutch cutter; G: ITknife-nano; H: Mucosectom-short blade; I: Mucosectom-long blade; J: Swanblade.
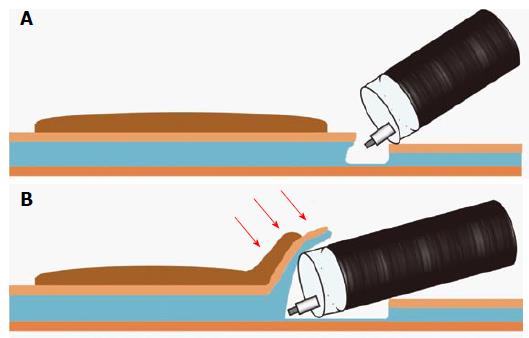
Figure 3 Schema of the mucosal flap.
A: After injecting a solution in the submucosal layer, mucosal incision and deeper cut are made; B: Continuing to dissect the submucosal layer allows the creation of the “mucosal flap” (Red arrows point to the “mucosal flap”). Inserting the distal attachment under the mucosal flap provides good counter-traction to the submucosal layers and allows good visualization of the operative field. Therefore, completion of the mucosal flap facilitates subsequent submucosal dissection.
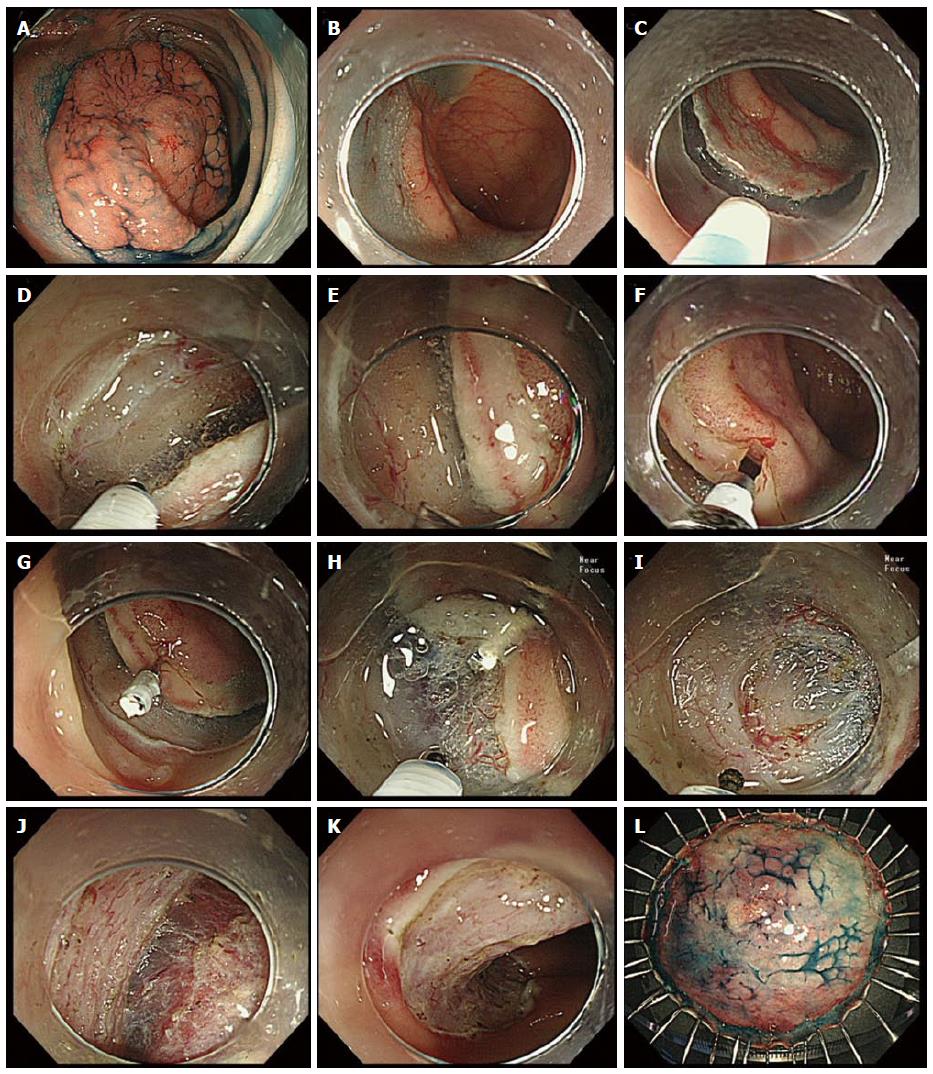
Figure 4 Endoscopic submucosal dissection of a laterally spreading tumor, non-granular type lesion using the clip-flap method.
A: A 45 mm, LST-NG was located at the sigmoid colon. The patient was first positioned so that the bowel wall containing the lesion was uppermost, and this maximizes the assistance of gravity during ESD; B: Submucosal injection was performed from the anal side; C: Mucosal incision from the anal side was made using FlushKnife BT; D: Deeper cut of the anal side was made; E: The submucosal layer could not be adequately visualized because it was hidden by the exfoliated mucosa at this region. Insertion of the distal attachment under the exfoliated mucosa was difficult because of the tight space between the exfoliated mucosa and muscle, despite the condition after submucosal injection; F: After the width of endoclip’s prongs was slightly narrowed, the edge of the exfoliated mucosa was clipped with an endoclip while lifting the exfoliated mucosa with the prongs of the endoclip, so that the deep layer of the submucosa was not grasped by the endoclip; G: The endoclip was attached to the exfoliated mucosa. The tail end of the endoclip attached to the mucosa slightly fell toward the intestinal lumen due to gravity, allowing the attachment to be easily inserted under the endoclip; H: The distal attachment was inserted under the endoclip, and then mucosa and the submucosal layer were elevated by the endoclip. The submucosal layer could be clearly visualized and dissected with the endoknife under the direct vision; I: The distal attachment could be inserted under the exfoliated mucosa by cutting the vasculature; J: Following mucosal flap formation, the submucosal layer could be dissected more easily; K: Dissection was completed following complete circumferential incision without any complications. Artificial ulcer after ESD; L: Resected specimen. Histopathological examination confirmed intramucosal cancer, and margin (-). LST-NG: Laterally spreading tumor, non-granular type; ESD: Endoscopic submucosal dissection.
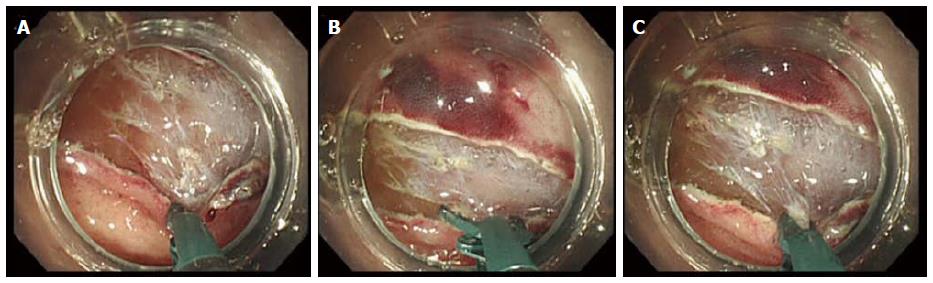
Figure 5 Three steps of safe submucosal dissection using a scissor-type endoknife (SBknifeJr) in case of a vertical approach.
A: The endoscope was rotated and the exfoliated mucosa was turned down with a tip of an endoknife to clearly visualize the submucosal layer to be dissected along with the scissor tips; B: The edges of the scissor-type endoknife was opened; C: The submucosal layer under the exfoliated mucosa could be safely dissected by grasping and pulling up with the endoknife before application of an electrical current. Repeating these procedures led to the creation of the mucosal flap and successful endoscopic submucosal dissection.
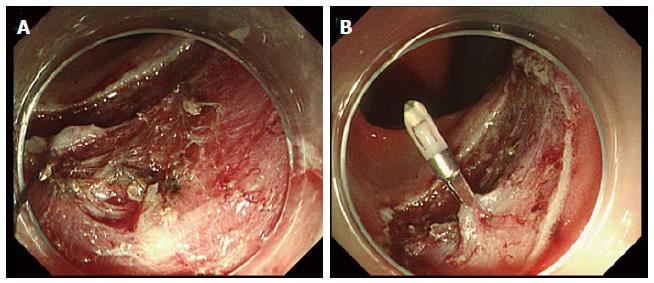
Figure 6 Management of perforation by clipping.
A: Perforation occurring during colorectal endoscopic submucosal dissection; B: Perforation closure using an endoclip.
- Citation: Yamamoto K, Michida T, Nishida T, Hayashi S, Naito M, Ito T. Colorectal endoscopic submucosal dissection: Recent technical advances for safe and successful procedures. World J Gastrointest Endosc 2015; 7(14): 1114-1128
- URL: https://www.wjgnet.com/1948-5190/full/v7/i14/1114.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i14.1114