Copyright
©2012 Baishideng Publishing Group Co.
World J Gastrointest Endosc. Jun 16, 2012; 4(6): 201-211
Published online Jun 16, 2012. doi: 10.4253/wjge.v4.i6.201
Published online Jun 16, 2012. doi: 10.4253/wjge.v4.i6.201
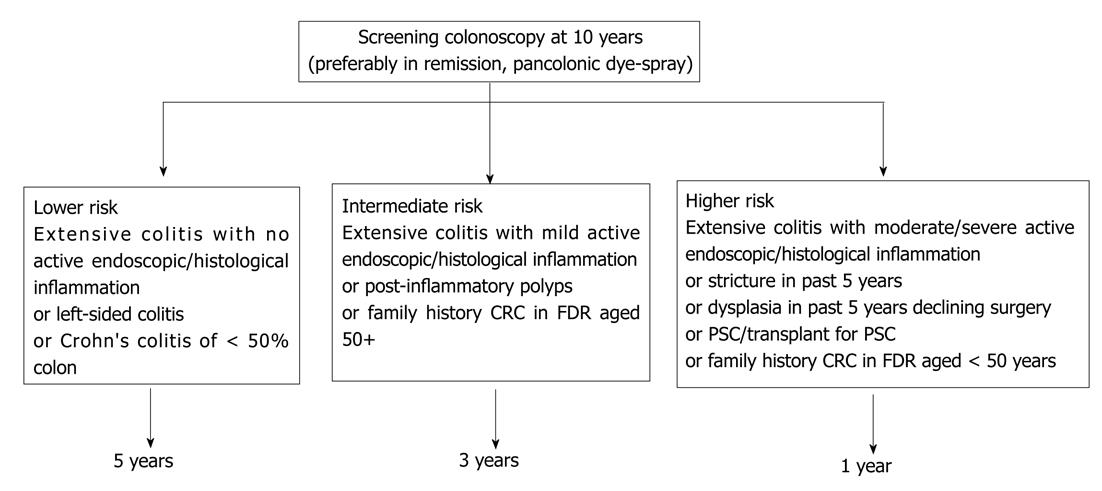
Figure 1 British Society of Gastroenterology guidelines on surveillance of colitis.
PSC: Primary sclerosing cholangitis; CRC: Colorectal cancer.
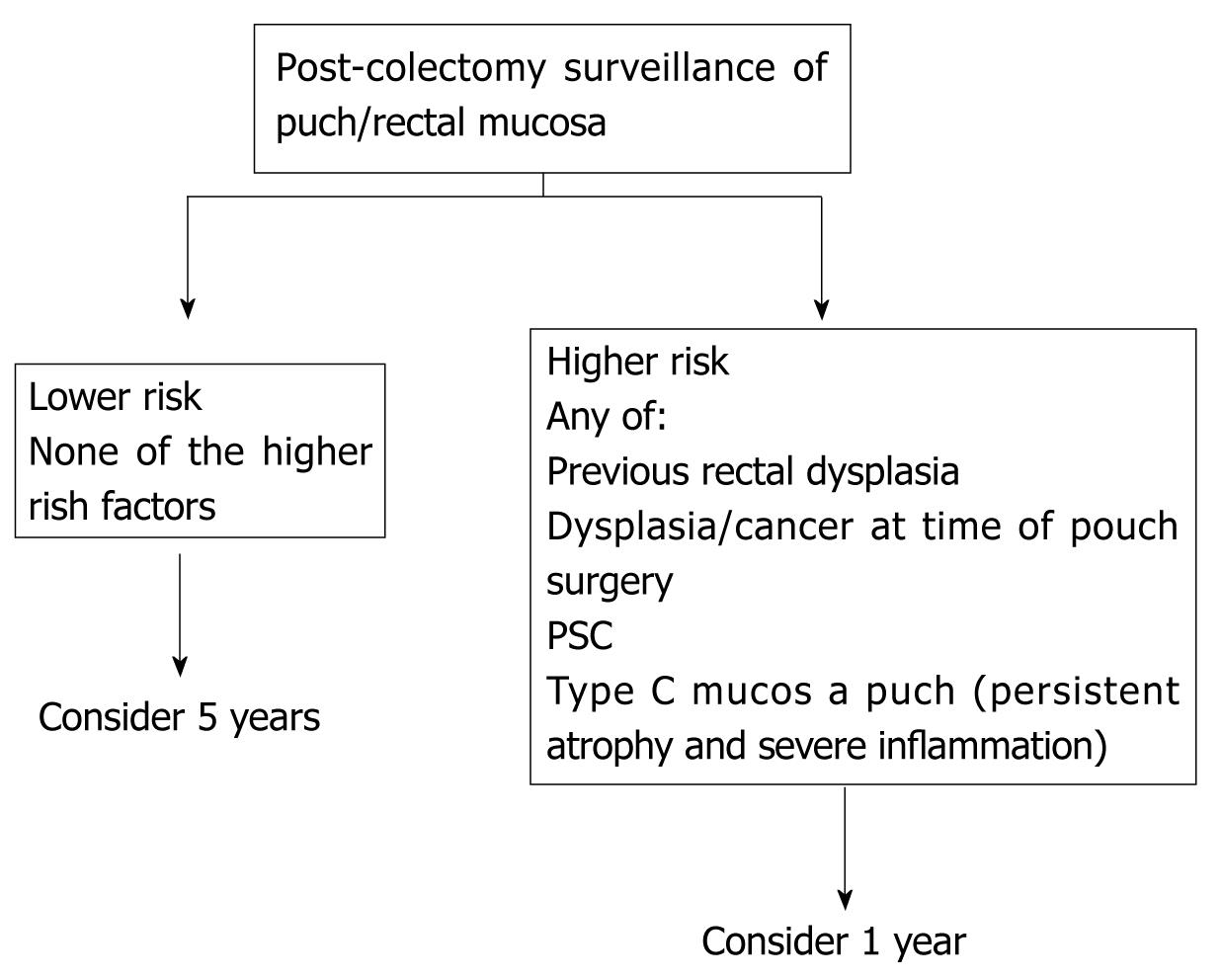
Figure 2 British Society of Gastroenterology surveillance recommandations post colectomy.
PSC: Primary sclerosing cholangitis.
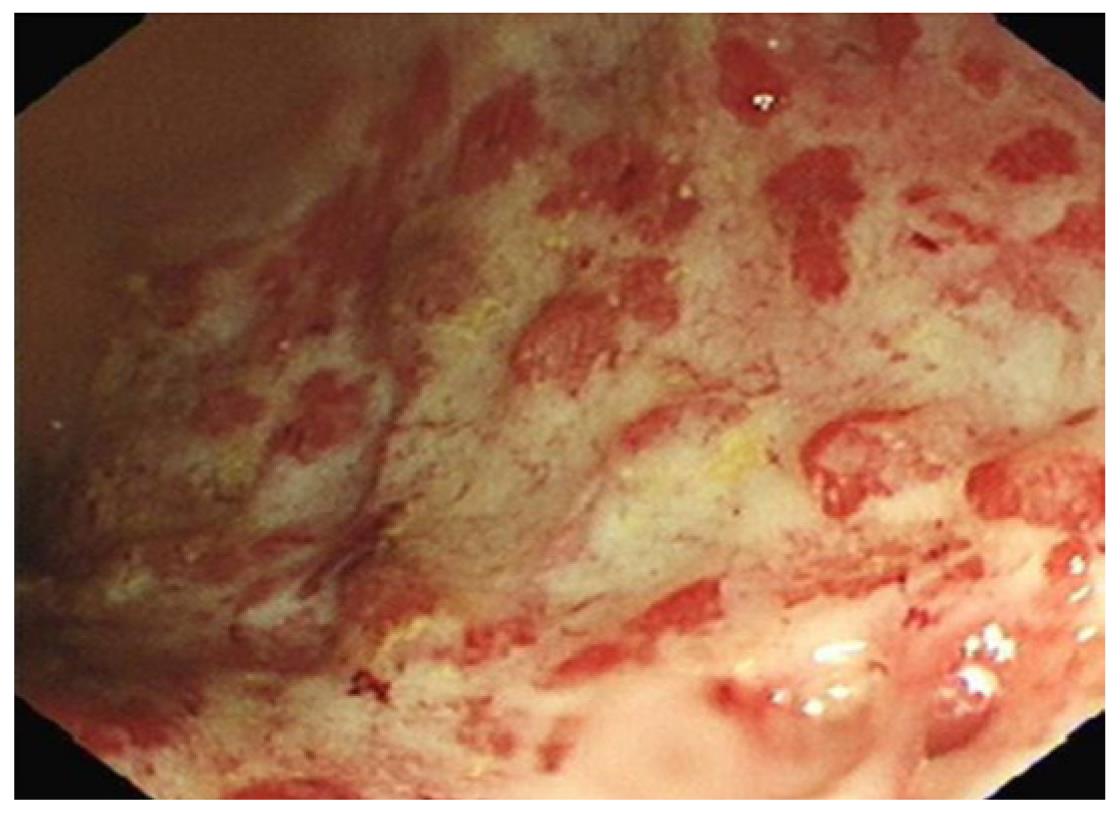
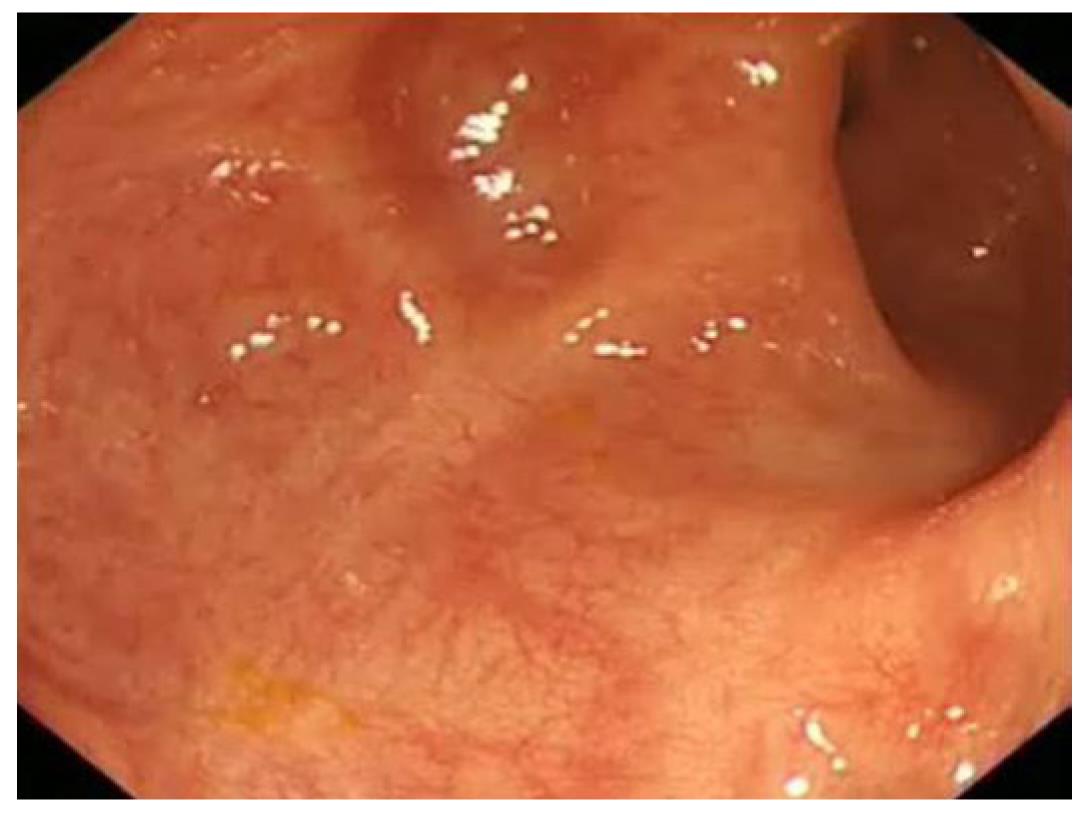
Figure 3 Severe colitis (Sutherland score 3).
Friable, granular mucosa with exudates overlying the surface, ulcers and sub mucosal oedema of rectum.
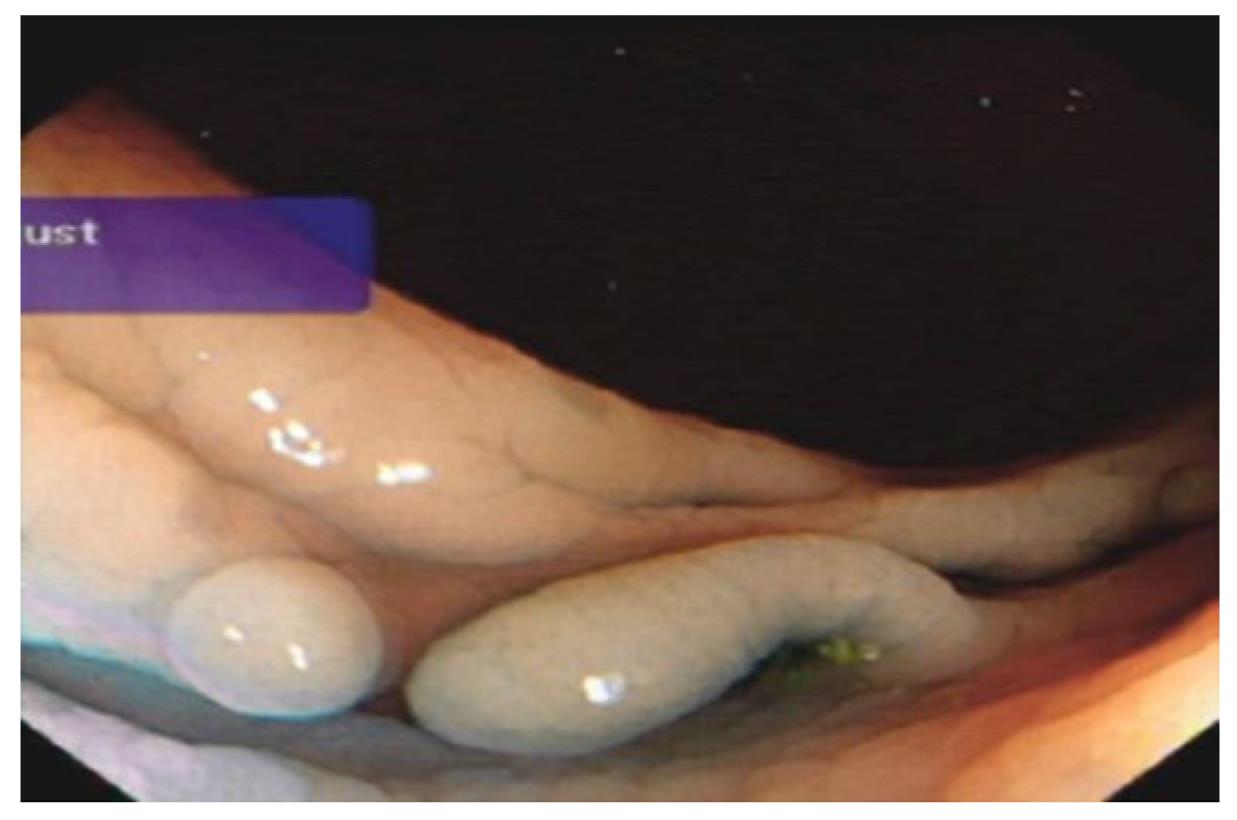
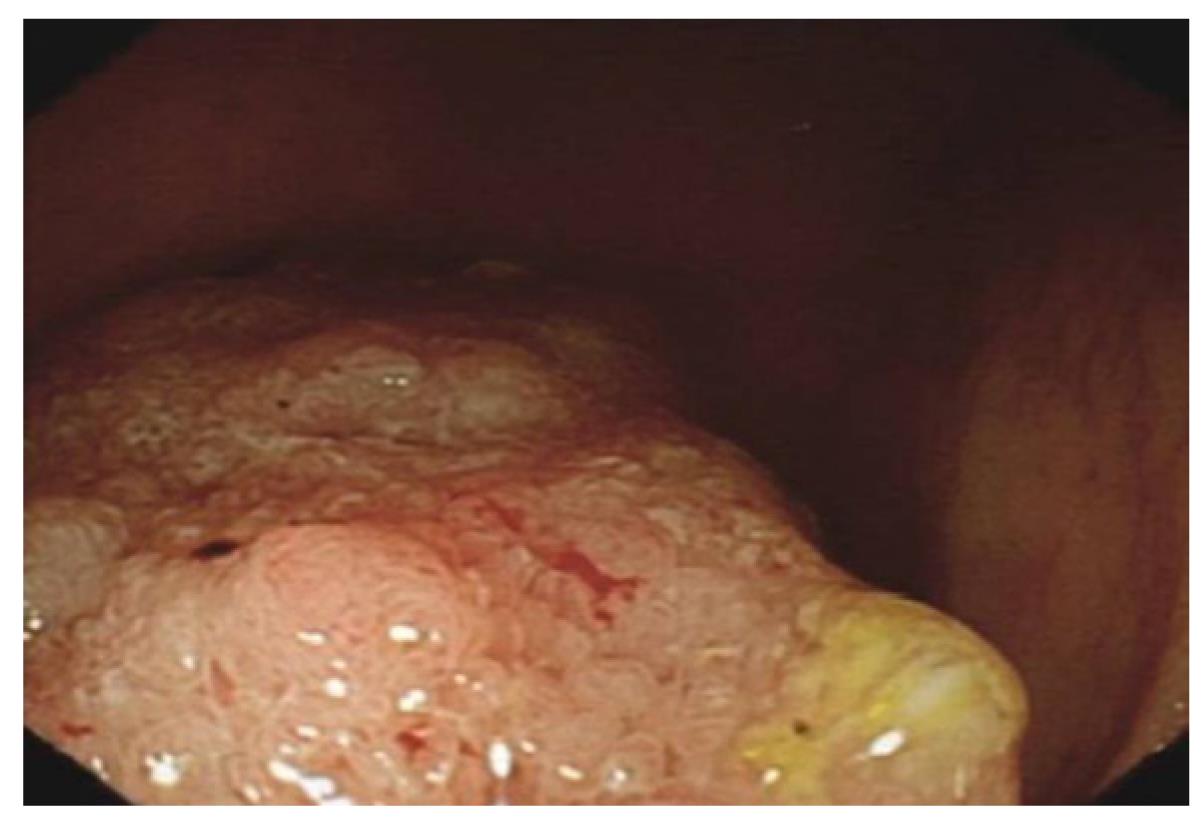
Figure 4 Post inflammatory polyp in transverse colon in a patient with ulcerative colitis.
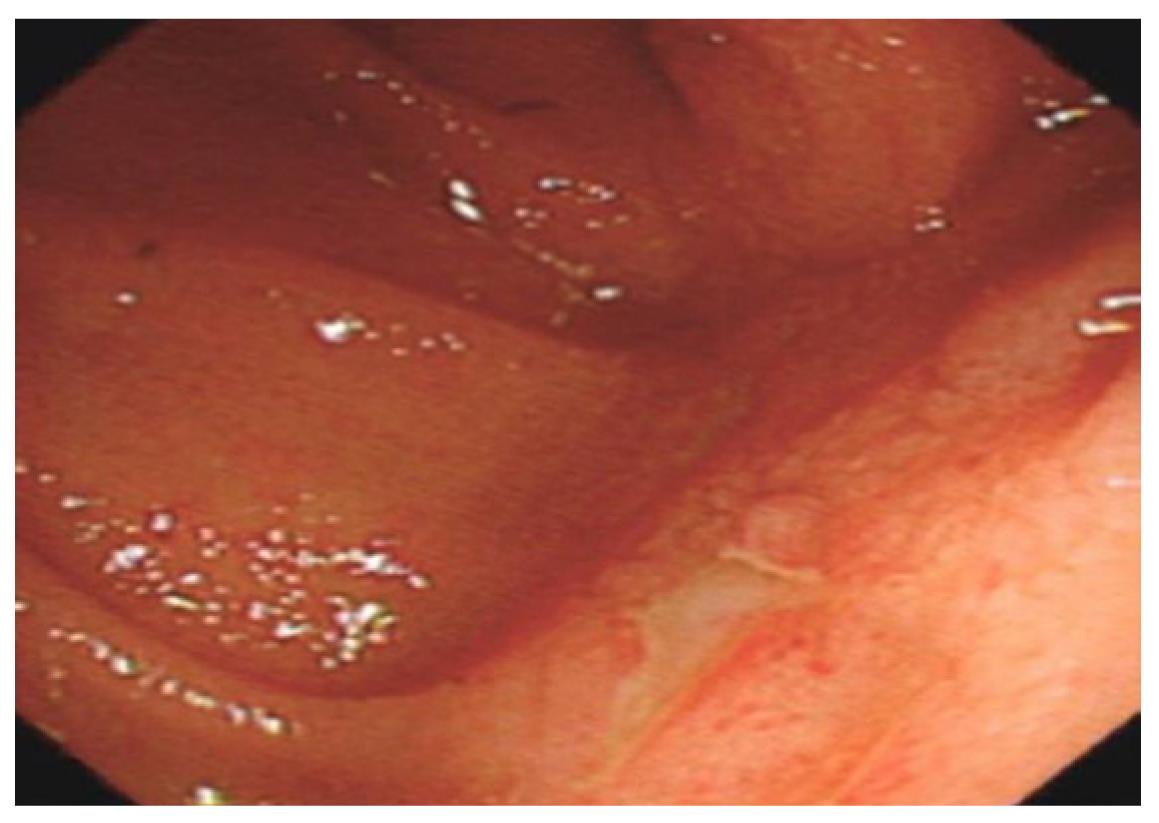
Figure 5 Extensive scarring of sigmoid colon in a patient with long history of colitis.
Figure 6 Shortened tubular colon in a patient with pan colitis.
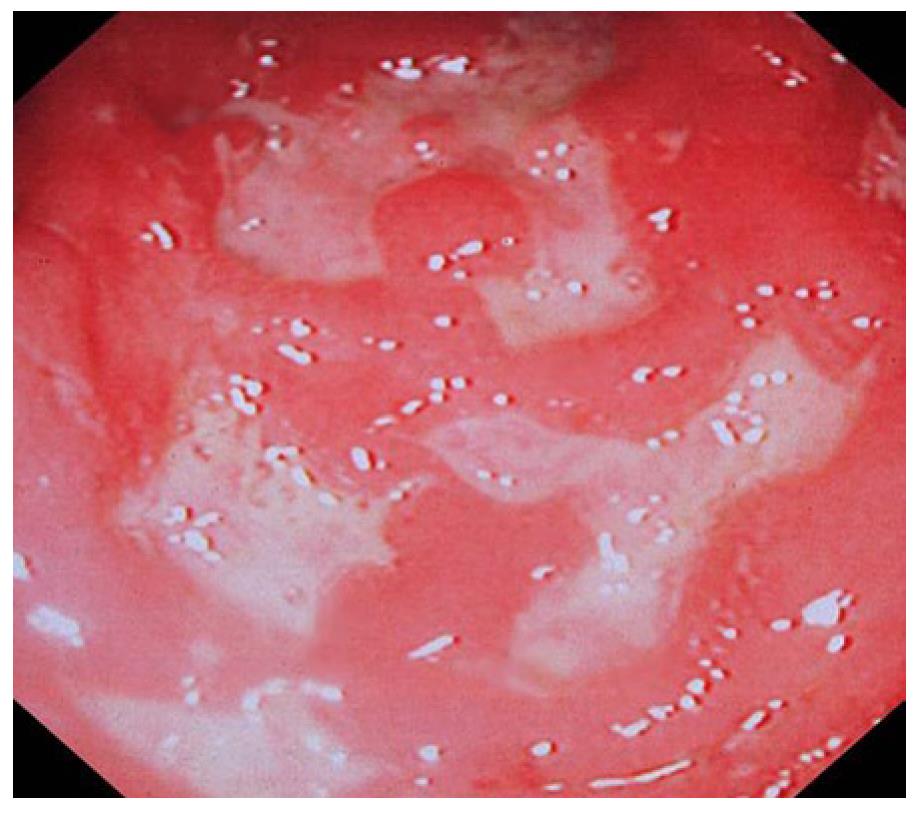
Figure 7 Deep ulcers, sub mucosal oedema and haemorrhages in the sigmoid colon in a patient with Crohn’s colitis.
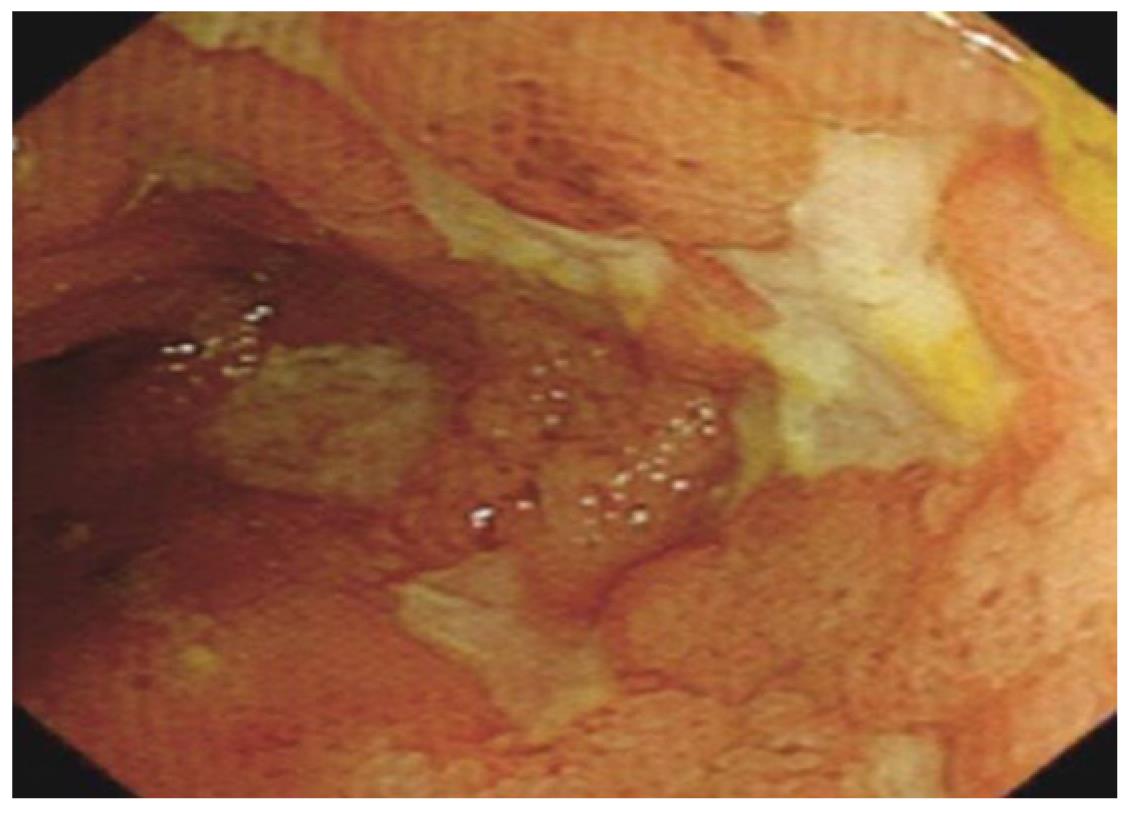
Figure 8 Multiple linear, deep ulcers with normal islands of intervening mucosa in the terminal ileum indicates severe Crohn’s disease.
Figure 9 Linear pyloric ulcer and surrounding sub mucosal oedema-pyloric Crohn’s disease.
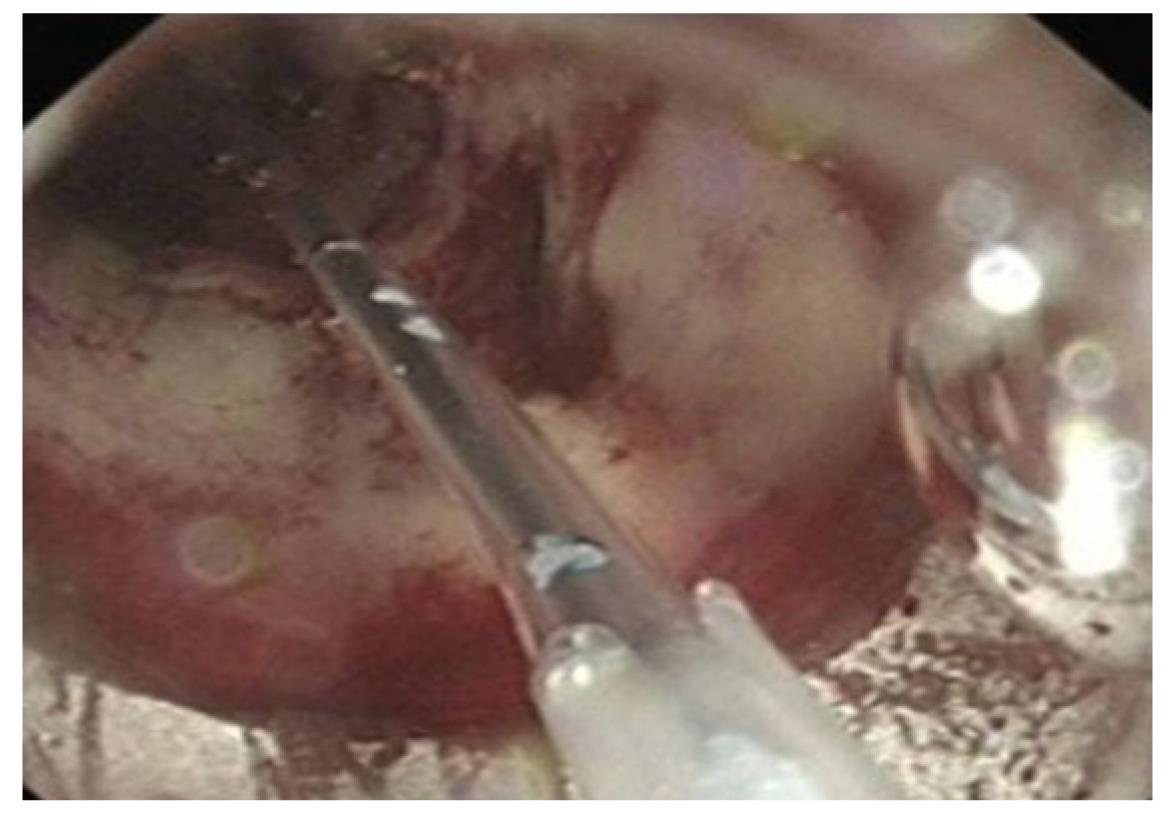
Figure 10 Balloon dilatation of Crohn’s stricture.
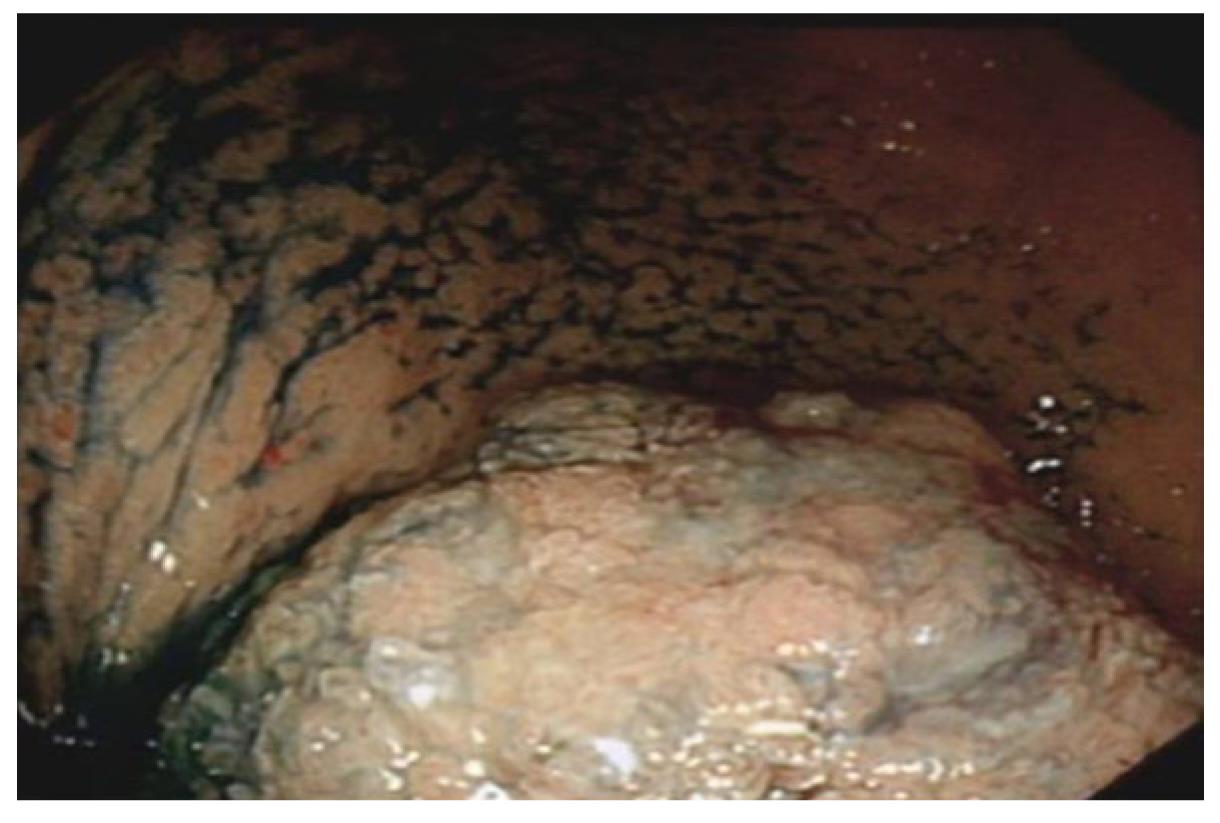
Figure 11 Dysplasia-associated lesions/masse in caecal pole in a patient with a long history of pancolitis.
Figure 12 Dysplasia-associated lesions/masse in caecal pole after dye spray.
Figure 13 Aphthous ulcer in the neo terminal ileum in a patient who had ileorectal anastomosis( indicates recurrence of Crohn’s disease).
Note healthy surrounding mucosa.
Figure 14 Pin hole stricture in the neo terminal ileum (Crohn’s disease).
- Citation: Rameshshanker R, Arebi N. Endoscopy in inflammatory bowel disease when and why. World J Gastrointest Endosc 2012; 4(6): 201-211
- URL: https://www.wjgnet.com/1948-5190/full/v4/i6/201.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i6.201