Copyright
©2012 Baishideng Publishing Group Co.
World J Gastrointest Endosc. Nov 16, 2012; 4(11): 489-499
Published online Nov 16, 2012. doi: 10.4253/wjge.v4.i11.489
Published online Nov 16, 2012. doi: 10.4253/wjge.v4.i11.489
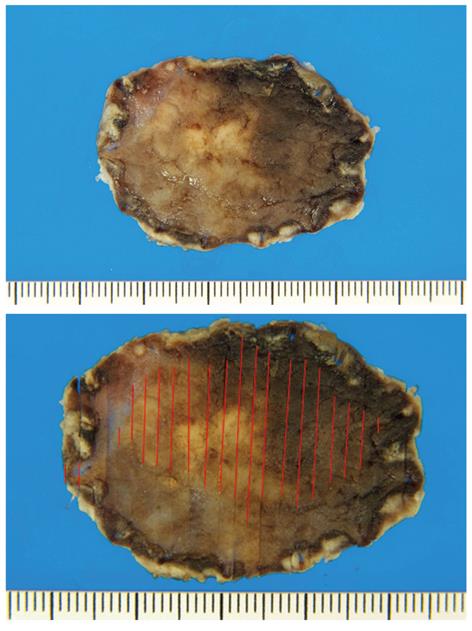
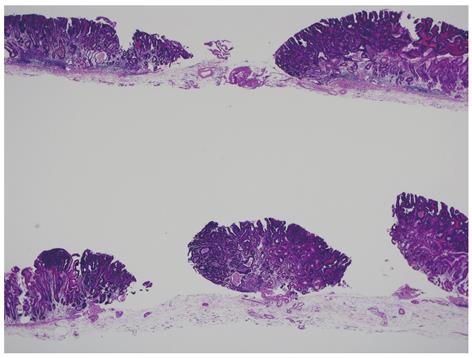
Figure 1 Endoscopic submucosal dissection materials with incidental lesions not found before treatment.
These cases are found in a percentage of endoscopic submucosal dissection materials. The incidental lesion shows a positive margin. It should be kept in mind that a lesion may not be single but multiple in endoscopic submucosal dissection specimens. This accurate mapping of the lesion is helpful to make a treatment strategy after endoscopic submucosal dissection specimen.
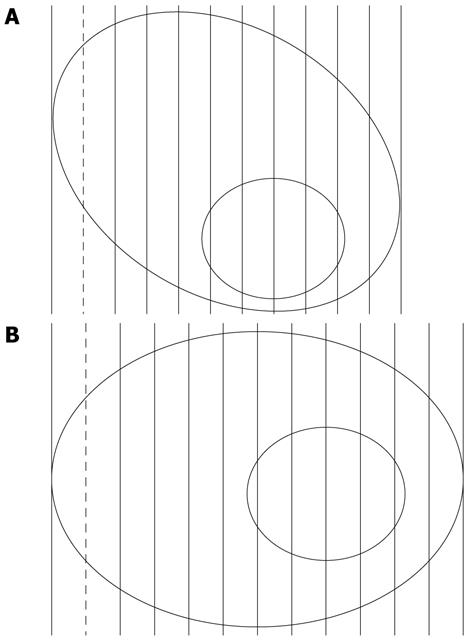
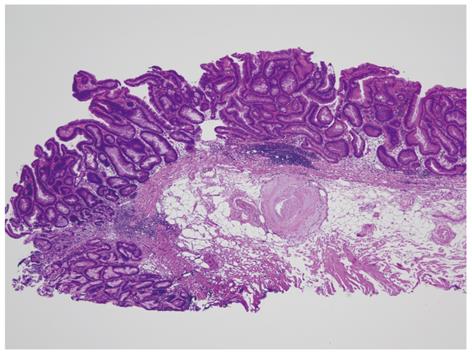
Figure 2 Cutting.
A: General cutting of endoscopic submucosal dissection material. The final glass slide is of the reversed section of the solid line. Therefore, it is recommended that the tumor area should not be included in the portion of the dotted line; B: Cutting of endoscopic submucosal dissection material with a tumor close to the cut margin. Endoscopic submucosal dissection specimen should be cut in parallel sections which are perpendicular to the tangent of the closest margin.
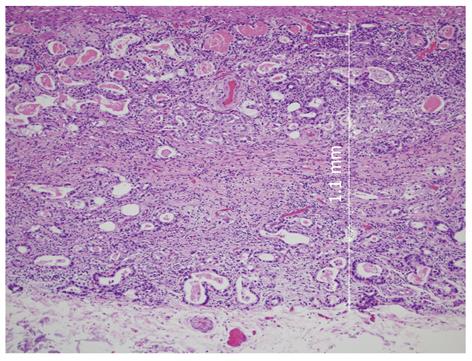
Figure 3 How to measure the depth in pT1b2 cases.
Depth of a pT1b case indicates the distance from the lower edge of the muscularis mucosae to the invasive front of tumor.
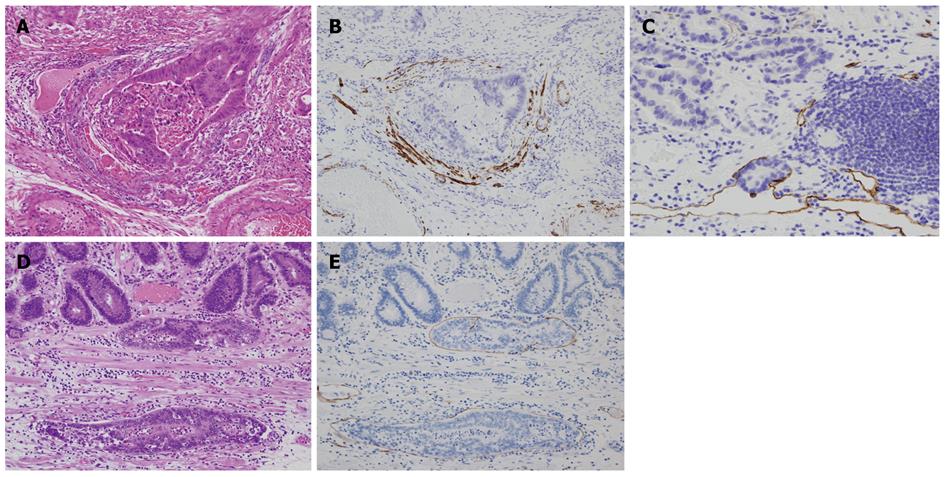
Figure 4 Evaluation of vessel invasion and lymphatic invasion.
Venous invasion is evaluated by using a double staining with Victoria blue and hematoxylin-eosin (A) and immunohistochemistry of desmin (B). Lymphatic invasion is demonstrated by immunostaining of D2-40 (C). Lymphatic invasion is noted in the lamina propria (D: Hematoxylin-eosin stain; E: Immunohistochemistry of D2-40).
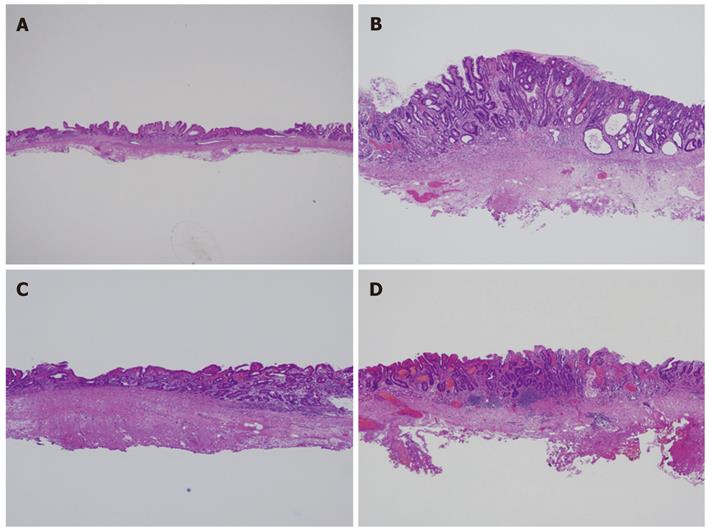
Figure 5 Ulcer scar vs biopsy scar.
Biopsy scar is a very localized lesion (A and B) and is noted at the site of biopsy. Therefore, clinical information is important. On the other hand, ulcer scar due to tumor is usually an expansive lesion (C and D). Clinical information of no history of biopsy is also useful.
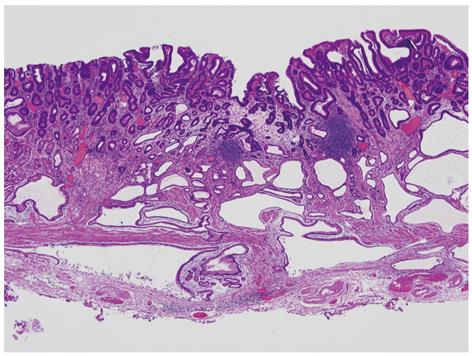
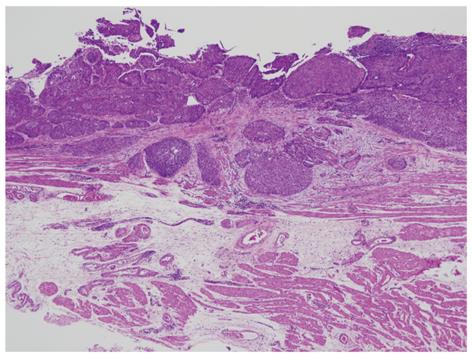
Figure 6 Heterotopic submucosal glands (= gastritis cystica profunda).
Heterotopic submucosal glands can be misdiagnosed endoscopically as an ulcer due to submucosal invasion. These lesions should be described in the pathology report and the lesional mapping diagram.
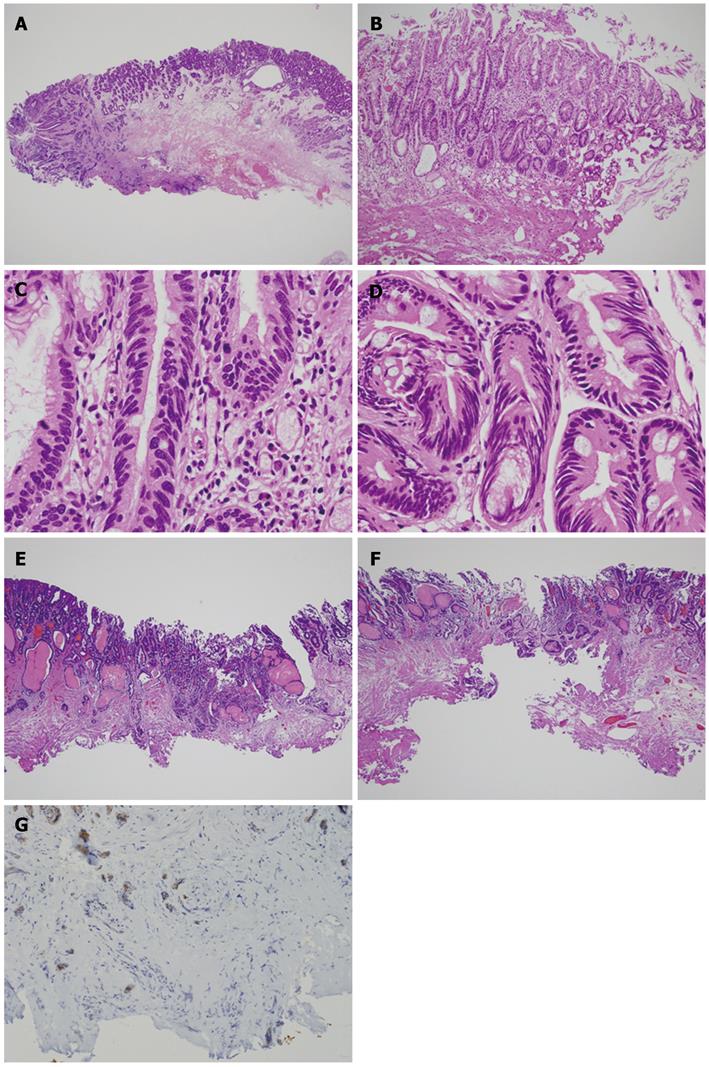
Figure 7 Cases of positive horizontal margin and vertical margin.
In most cases, a positive margin is easily recognized (A); Some cases show marked degeneration by treatment (B); By careful microscopic examination, adenocarcinoma cells (C) can be distinguished from intestinalized epithelium (D). A positive vertical margin at the submucosal layer (E) or at the lamina propria (F) should be described in the pathology report. A positive vertical margin can be easily detected by using immunohistochemistry of keratin (G).
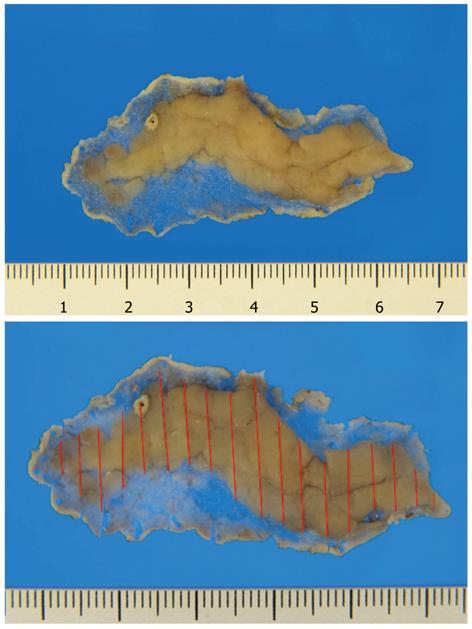
Figure 8 Cutting of a sessile polypoid lesion.
Non-tumor areas around the polypoid lesion are very thin. The submucosal layer of the tumor portion is also thin. Therefore, caution should be taken when preparing the specimen so that a false positive diagnosis of the vertical margin will not be made.
Figure 9 Mucosal tears due to overextension during the tissue fixation.
Figure 10 Positive horizontal margin in the colonic endoscopic submucosal dissection.
In appropriate pathology specimens, the evaluation of the margin is relatively easy.
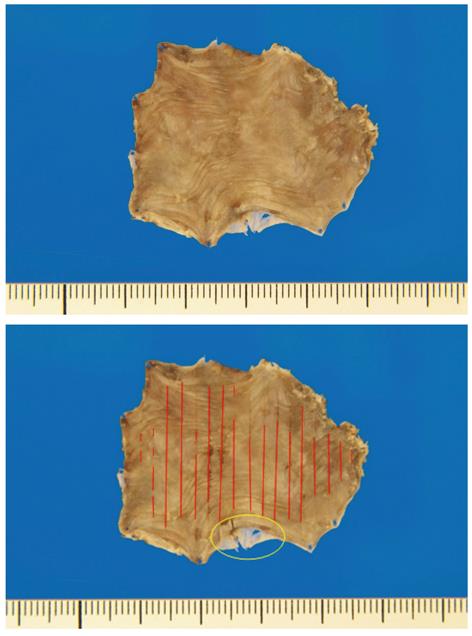
Figure 11 Early esophageal cancer in endoscopic submucosal dissection specimen.
The marginal portion (squamous epithelium) of the specimen is very thin. Therefore, it is difficult to make a section (yellow circle) and may cause false positivity of the surgical margin.
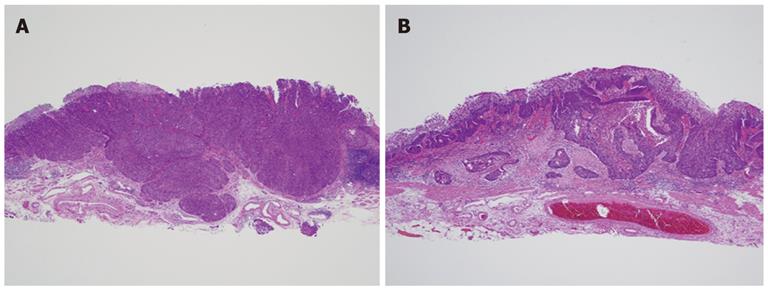
Figure 12 Invasive patterns in squamous cell carcinoma of the esophagus.
Expansive pattern (A) and infiltrative pattern (B) should be described in the pathology report.
Figure 13 pT1a-superficial muscularis mucosae case.
The lower portion of the picture shows two-layered muscularis mucosae. In esophageal cancers with pT1a-MM (M3), the depth of invasion is divided into three (pT1a-superficial muscularis mucosae, pT1a-lamina propria mucosae and pT1a-deep muscularis mucosae).
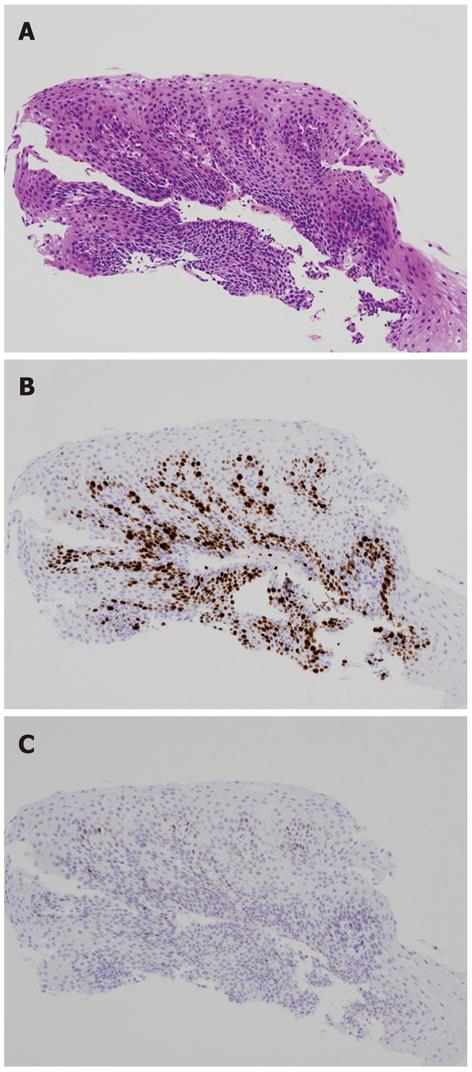
Figure 14 Evaluation of horizontal margin in the esophageal endoscopic submucosal dissection.
Compared to hematoxylin-eosin stain (A); immunohistochemical stainings of Ki-67 (B) and p53 (C) highlight the lesion.
- Citation: Nagata K, Shimizu M. Pathological evaluation of gastrointestinal endoscopic submucosal dissection materials based on Japanese guidelines. World J Gastrointest Endosc 2012; 4(11): 489-499
- URL: https://www.wjgnet.com/1948-5190/full/v4/i11/489.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i11.489