Copyright
©2010 Baishideng Publishing Group Co.
World J Gastrointest Endosc. Oct 16, 2010; 2(10): 325-334
Published online Oct 16, 2010. doi: 10.4253/wjge.v2.i10.325
Published online Oct 16, 2010. doi: 10.4253/wjge.v2.i10.325
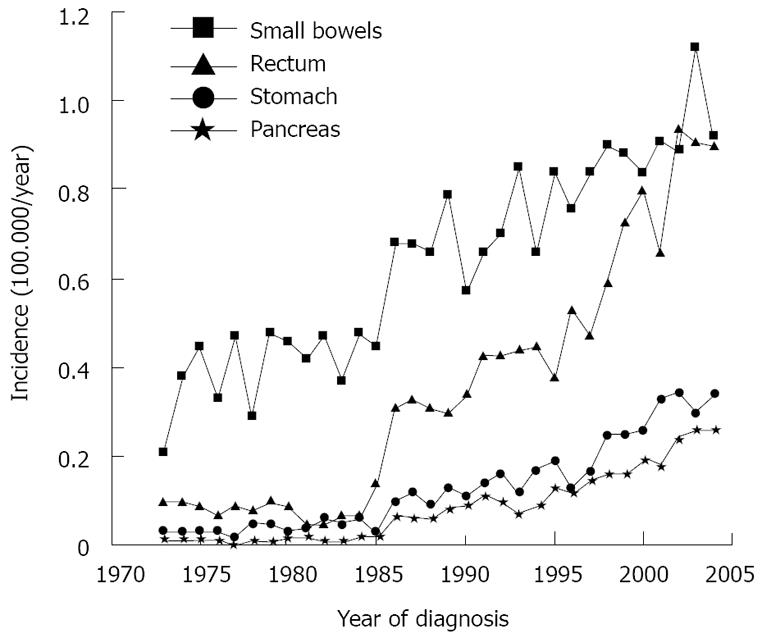
Figure 1 Epidemiological rise in the frequency of neuroendocrine neoplasms of the small bowel, rectum, stomach or pancreas in the United State.
Modified from Modlin et al[1].
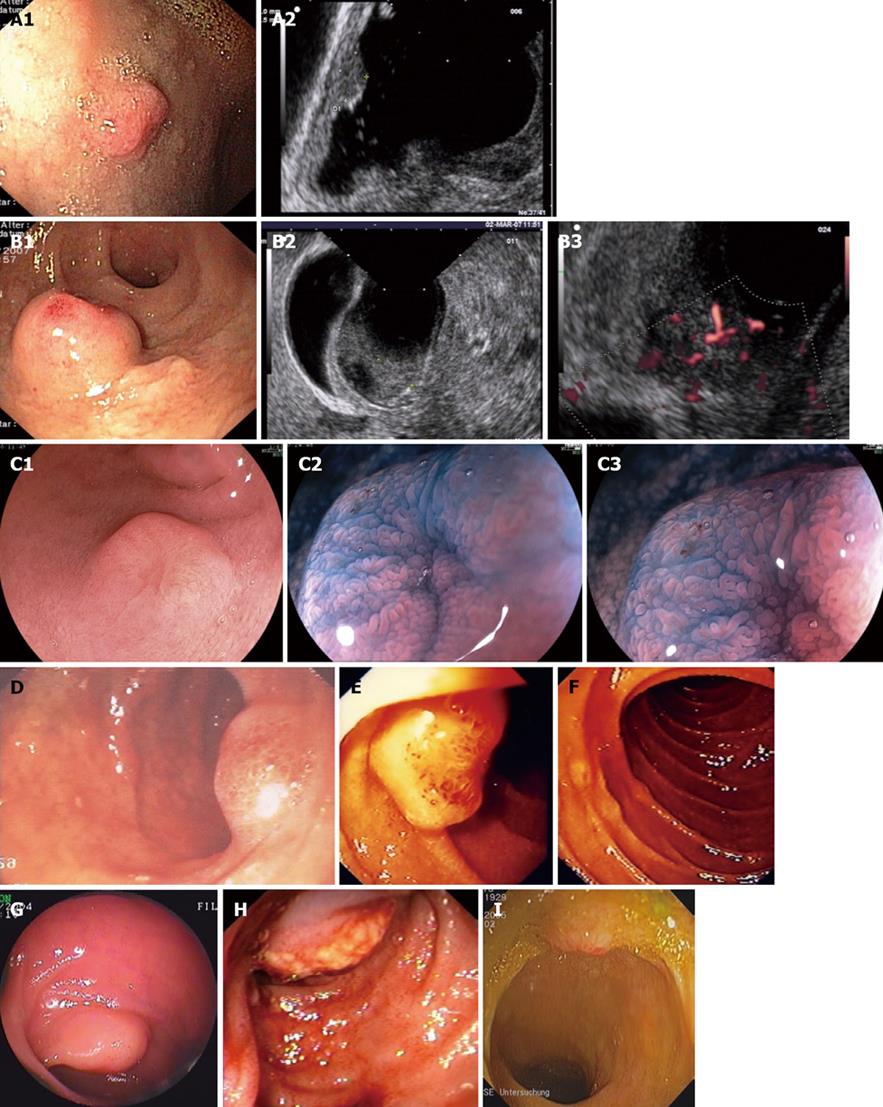
Figure 2 Endoscopic images of well-differentiated (G1), small intestinal neuroendocrine tumors.
A: 8 mm measuring neuroendocrine tumor (NET) in the duodenal bulb (A1). Endoscopic ultrasound shows the infiltration of mucosa and submucosa (A2). The duodenal NET exhibits a low echogenic pattern on endosonography (EUS); B: Duodenal NET of 21 mm size (B1), the muscularis propria is not infiltrated endosonographically (B2). The tumor shows a low echogenic pattern on EUS. The tumor (B3) shows a good arterial perfusion (by Doppler sonography); C: 10 mm-sized duodenal NET (C1). The chromoendoscopy (with indigo carmine) (C2) and the zoom endoscopy (C3) show an intact villous pattern and a crater-like retraction of the mucosa at the center of the tumor (modified from reference [77]); D: Sporadic gastrinoma of the duodenal bulb; E: Sporadic gastrinoma of the second part of the duodenum; F: Multiple duodenal gastrinomas in a patient with multiple endocrine neoplasia type 1 disease; G: 12 mm-sized NET of the distal ileum. Both tumor localisation and histological diagnosis were established using double balloon enteroscopy[34]. Ileal NETs present multifocally in 26%-30% of patients; H-I: 14 mm-sized NET of the terminal ileum. The primary tumor was located 8 cm proximal to the ileocecal valve. Ileocolonoscopy allowed not only tumor localization, but also histological verification of ileal NET disease (modified from reference [77]).
- Citation: Scherübl H, Jensen RT, Cadiot G, Stölzel U, Klöppel G. Neuroendocrine tumors of the small bowels are on the rise: Early aspects and management. World J Gastrointest Endosc 2010; 2(10): 325-334
- URL: https://www.wjgnet.com/1948-5190/full/v2/i10/325.htm
- DOI: https://dx.doi.org/10.4253/wjge.v2.i10.325