Copyright
©The Author(s) 2023.
World J Gastrointest Endosc. Nov 16, 2023; 15(11): 666-675
Published online Nov 16, 2023. doi: 10.4253/wjge.v15.i11.666
Published online Nov 16, 2023. doi: 10.4253/wjge.v15.i11.666
Figure 1 Esophagogastroduodenoscopy.
A: Right behind the upper esophageal sphincter is visualizing the base of a non-epithelial tumor, which continues distally throughout the esophagus, freely locating and occupying almost the entire space of the esophageal lumen; B: On retroflection, the distal part of the non-epithelial neoplasm splits into two parts, visible in the gastric lumen. Diastases of the diaphragmatic crura is up to 5-6 cm with sliding of cardia and fungus above the diaphragm during examination - signs of sliding hiatal cardiofundal hernia.
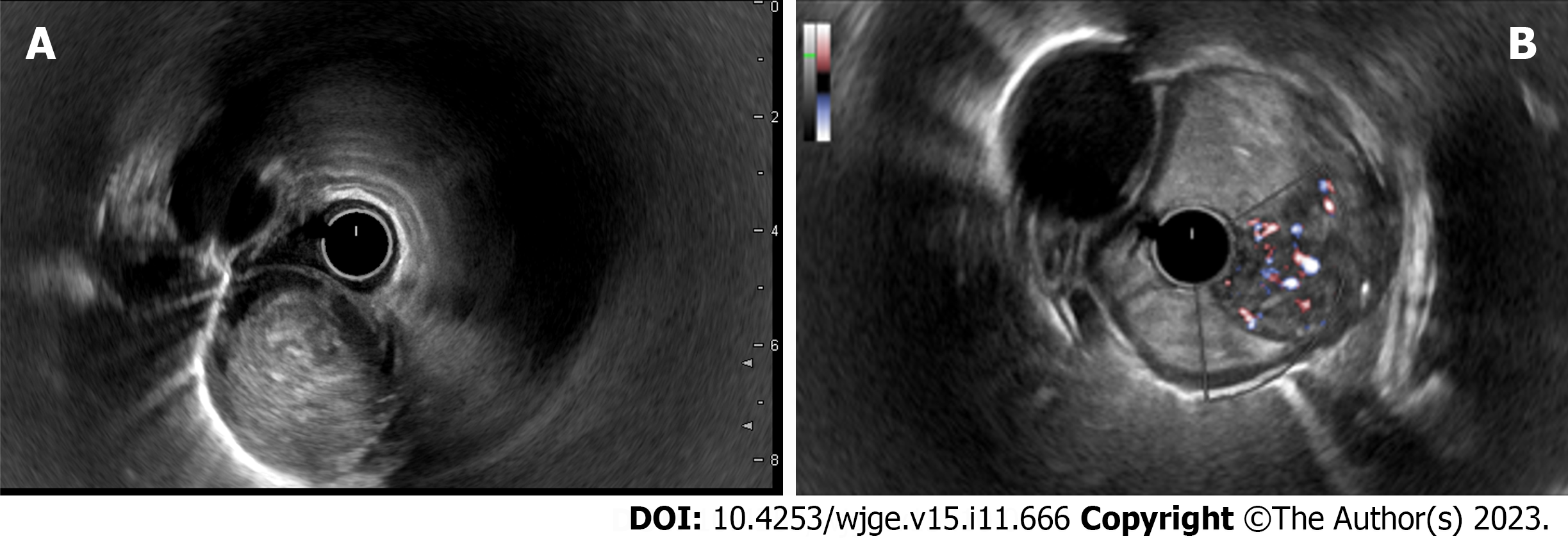
Figure 2 Endosonography of the esophagus.
A: A heterogeneous hypoechoic mass with a smooth and clear borders, cylindrically shaped, originating from submucosal layer (3rd echo layer); B: A doppler color mode shows a hypervascular zone at the base of the tumor with multiple large feeding vessels, up to 4-5 mm in diameter, extending along the wall of the esophagus.
Figure 3 Chest computed tomography scan.
A: Coronal plane; B: Sagittal plane. Computed tomography with intravenous contrast enhancement revealed an expansion of the esophagus up to 5-6 cm in the distal part, a hypervascular neoplasm in the lumen of the esophagus extending throughout the entire esophageal length from upper esophageal sphincter to the gastric cardia with the maximum diameter of the tumor up to 6 cm.
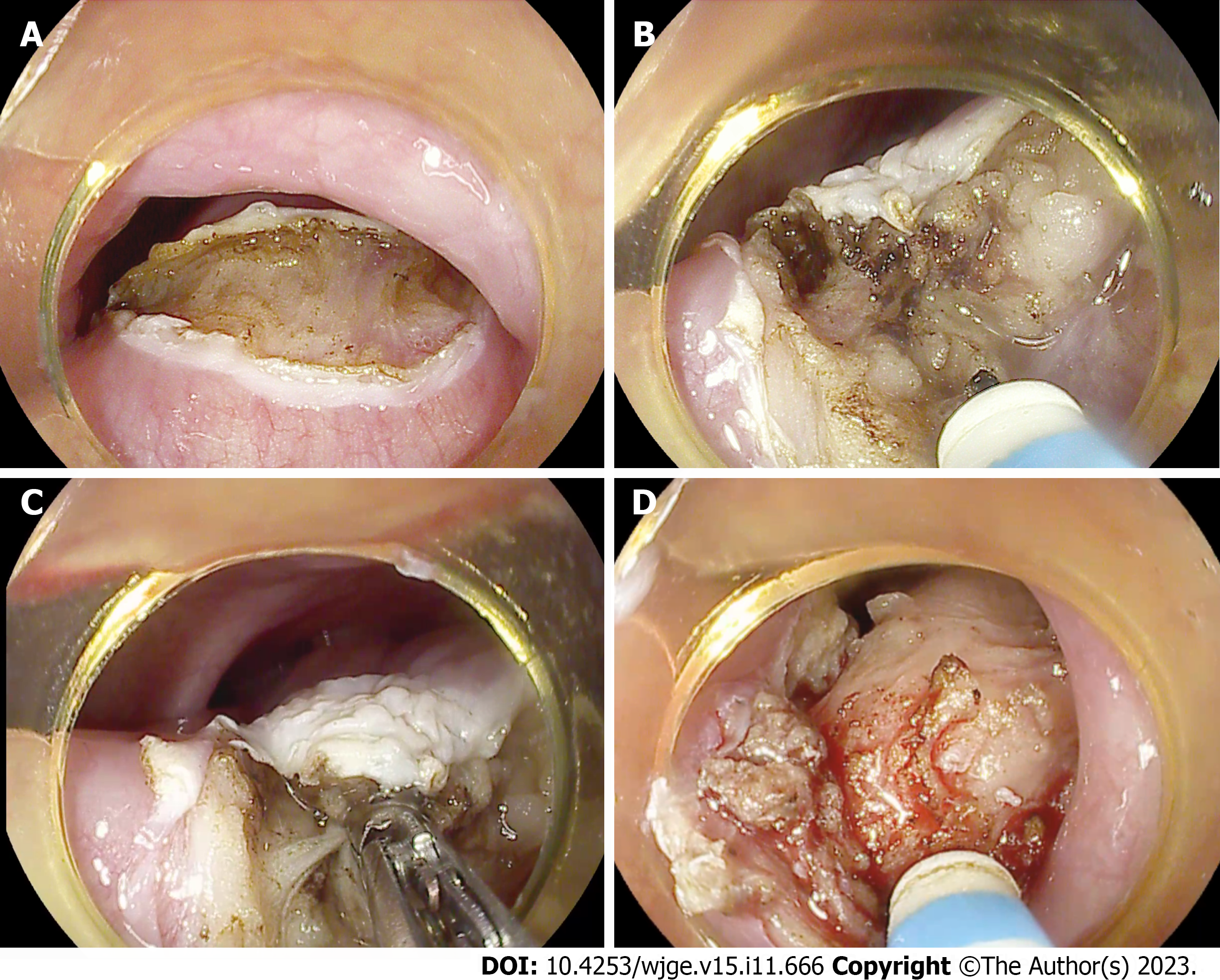
Figure 4 Endoscopic steps of the surgery.
A: Dissection of the mucosal and submucosal layers behind UES at the base of the tumor; B: Endoscopic submucosal dissection using endoscopic needle-knife; C: Coagulation of large feeding vessels in the submucosal layer using the coagrasper; D: The tumor is almost fully mobilized from the esophageal wall at its base.
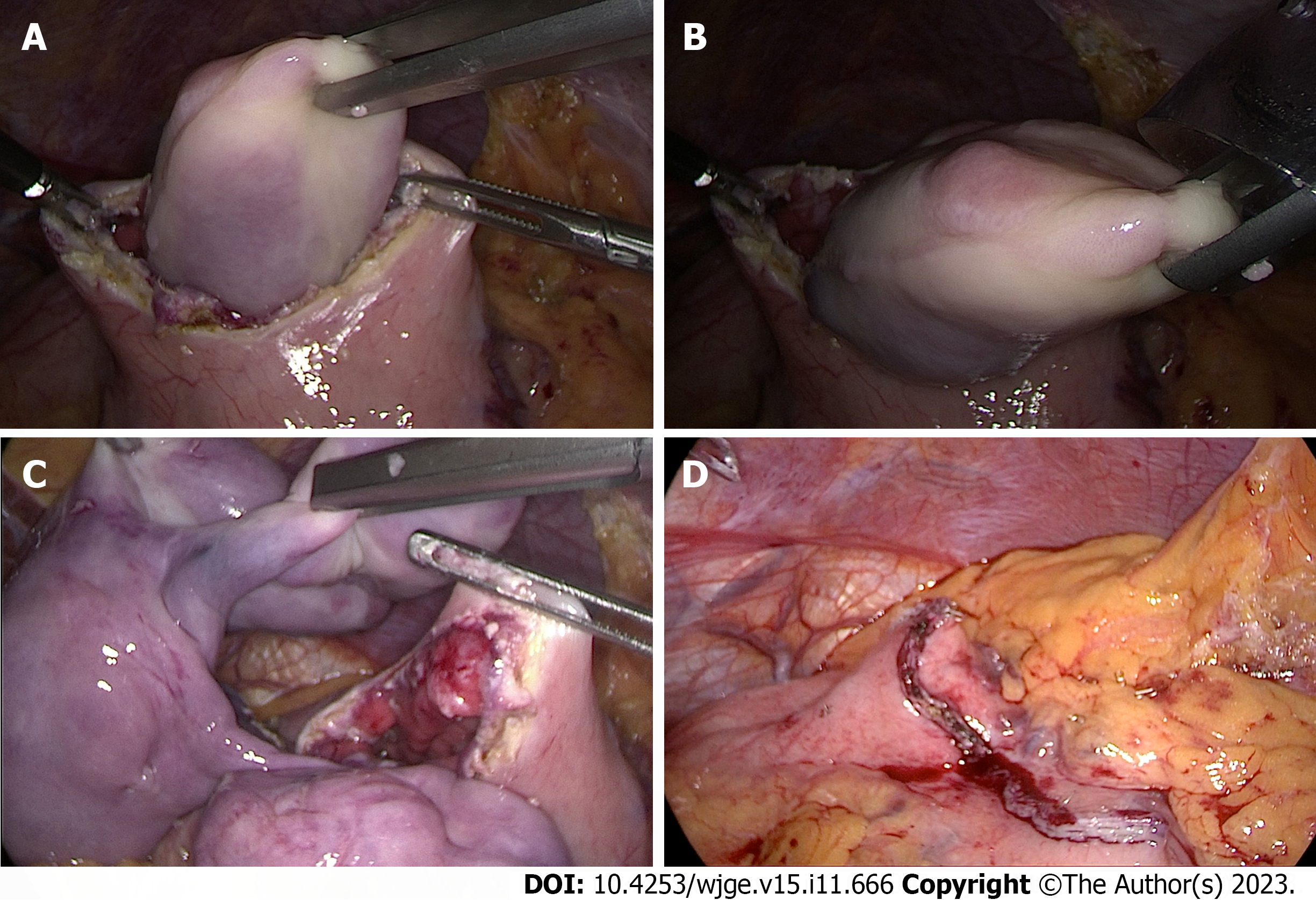
Figure 5 Laparoscopic steps of the surgery.
A: Using a laparoscopic grasper, the tumor is captured through a gastrotomy on the anterior wall of the gastric body; B: Removal of the tumor from the gastric body after it was completely brought down from the esophagus; C: The complete extraction of the tumor from the stomach into abdominal cavity; D: Gastrotomy closure with laparoscopic EndoGIA stapler suture.
Figure 6 Specimen.
The removed specimen represents a tumor of an irregular elongated shape splitting into two parts at the distal end, 25 cm × 4 cm × 6 cm in size, with a smooth surface covered by intact mucosa. The area of endoscopic submucosal dissection at the tumor's base is 11 centimeters long (marked with square bracket).
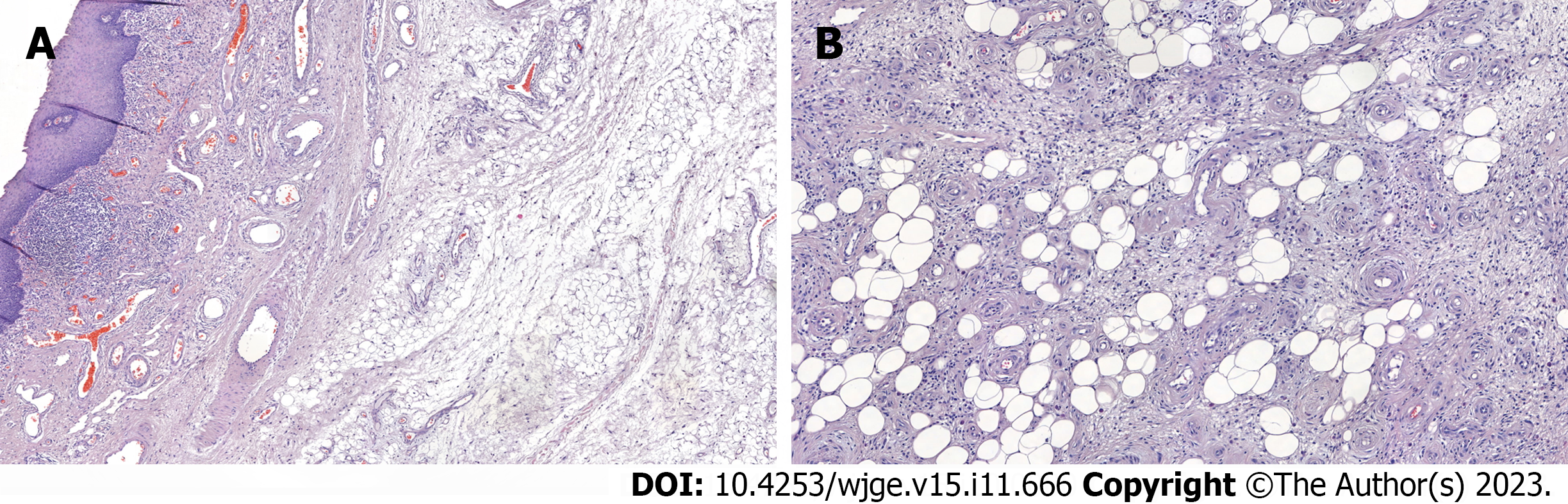
Figure 7 Morphology.
A and B: The tumor is represented by adipose tissue, separated by wide fields of sclerotic fibrous tissue with numerous vessels and cells of the inflammatory infiltrate. The adipocytes are uninuclear and different-sized. Among the fibrous tissue there are hyperchromic cells with angular nuclei. Morphology report: fibrovascular polyp with foci of highly differentiated liposarcoma, tumor tissue at the sight of endoscopic dissection is not determined, R0, М 8850/3; Grade 1.
Figure 8 Follow-up esophagoscopy three months after surgery.
A: A white linear scar is observed in the submucosal layer behind the upper esophageal sphincter, where endoscopic dissection was previously performed (marked with white arrows). There are no residual tumor fragments and no signs of narrowing of the lumen at the sight of dissection; B: No alterations in the esophageal lumen along its entire length.
- Citation: Dzhantukhanova S, Avetisyan LG, Badakhova A, Starkov Y, Glotov A. Hybrid laparo-endoscopic access: New approach to surgical treatment for giant fibrovascular polyp of esophagus: A case report and review of literature. World J Gastrointest Endosc 2023; 15(11): 666-675
- URL: https://www.wjgnet.com/1948-5190/full/v15/i11/666.htm
- DOI: https://dx.doi.org/10.4253/wjge.v15.i11.666