Copyright
©The Author(s) 2018.
World J Gastrointest Endosc. Nov 16, 2018; 10(11): 367-377
Published online Nov 16, 2018. doi: 10.4253/wjge.v10.i11.367
Published online Nov 16, 2018. doi: 10.4253/wjge.v10.i11.367
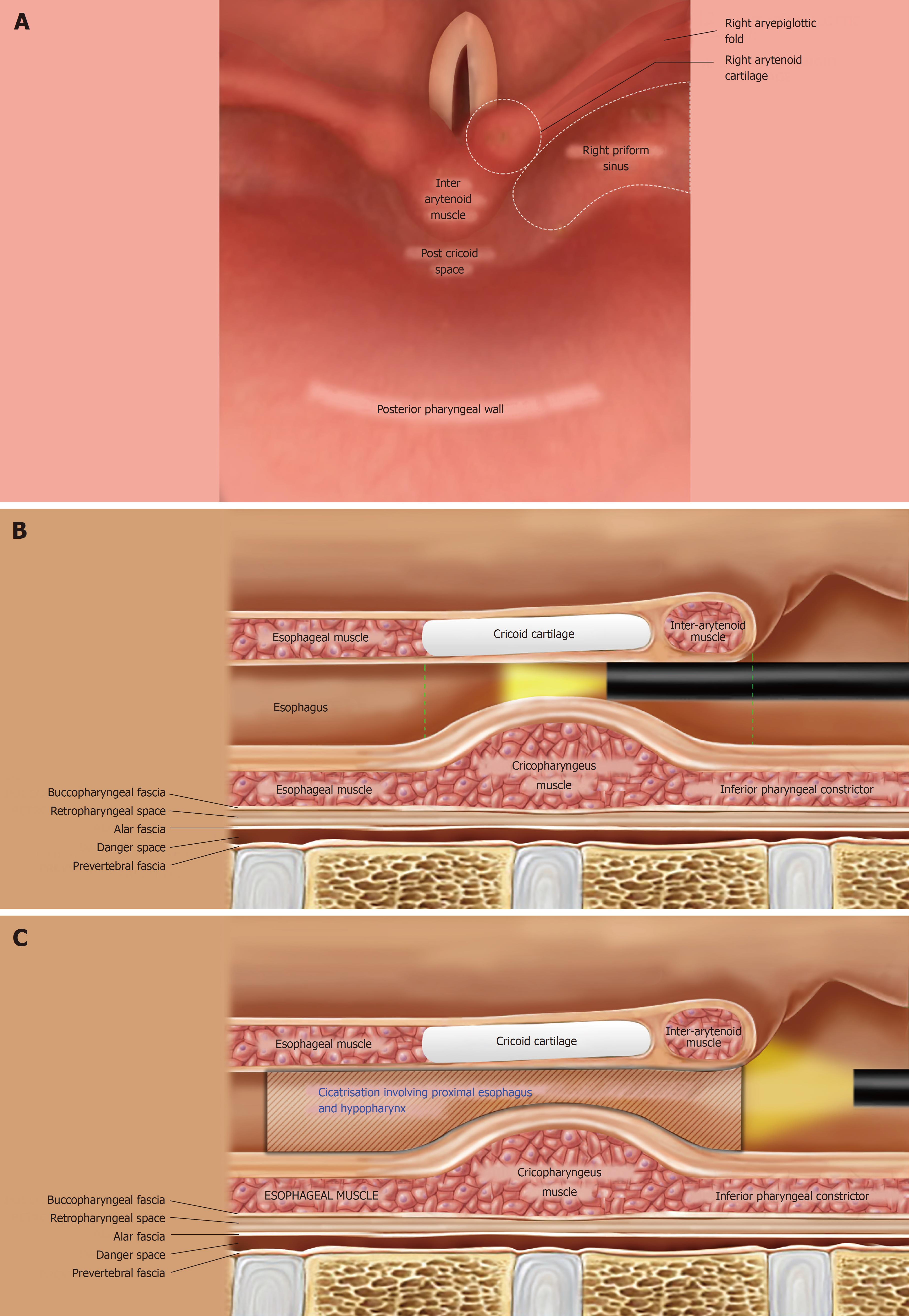
Figure 1 Anatomical consideration while addressing hypopharyngo-esophageal strictures endoscopically.
A: The normal anatomy of the adult hypopharynx as seen during flexible endoscopy, with the scope tip behind the epiglottis. The piriform sinuses are 2 inverted pyramids on either side of the larynx with their apex inferiorly at the level of cricopharyngeus muscle (CP); they are bounded medially by the aryepiglottic folds and laterally by the pharyngeal wall; B: Post-cricoid region extends from the level of arytenoid cartilages (joined by the inter-arytenoid muscle in the midline) superiorly to the inferior border of cricoid cartilage (vertical dashed green lines); C: The strictured proximal esophagus and hypopharynx in both of our cases. The fibrotic process in both extended cranially till the proximal aspect of the post-cricoid region; there was an involvement of the apical parts of piriform sinuses as well (not shown here).
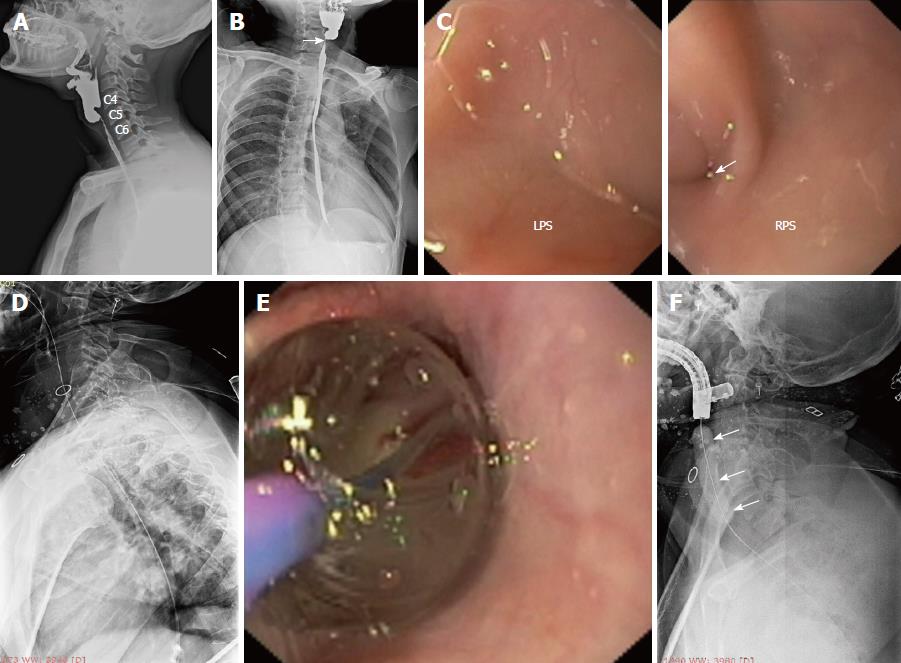
Figure 2 Near-total stricture in case 1 and its endoscopic management.
A: Lateral view of barium esophagogram showing the near-total stricture of the proximal esophagus involving the hypopharynx; B: On AP view, the near-total stricture has an eccentric proximal appearance (white arrow) and it is communicating with the right piriform sinus; C: During flexible endoscopic evaluation, the left piriform sinus (LPS) was completely obliterated in its apical region, while the right piriform sinus (RPS) showed a tiny opening (white arrow) which represents the beginning of the near-total stricture; D: A flexible guide-wire was passed across the stricture with difficulty, its correct placement was confirmed under fluoroscopy and the stricture was dilated with a 10F diathermy dilator (video 1); E, F: Subsequently, the stricture was dilated with a TTS balloon (white arrows).
Figure 3 Near-total stricture in case 1 and its endoscopic management.
A: The esophagogram after dilatation in case 1 showed a residual eccentric stricture, suggestive of persistent adhesions in the post-cricoid space and left piriform sinus; B-D: Serial endoscopic images of electroincision procedure in case 1, as the wire-guided sphincterotome was progressively moving towards the left pharyngeal wall after cutting the adhesions in the post-cricoid space and left piriform sinus; E: After electro-incision, a dilatation was given with the dilating balloon placed in the left piriform sinus; F: Follow-up esophagogram showing the completely opened-up stricture along its entire length.
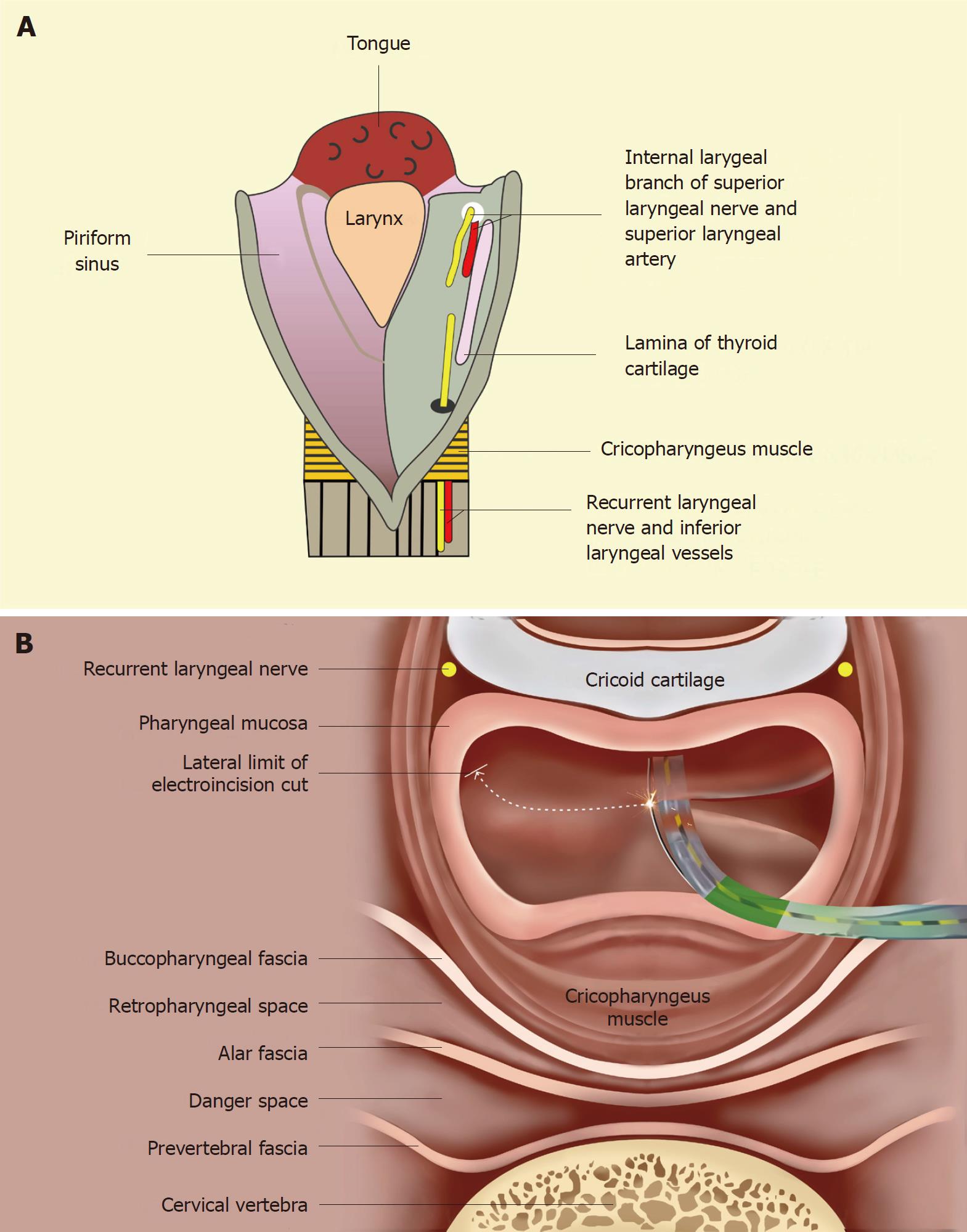
Figure 4 Anatomical considerations to prevent complications while performing the sphincterotome-assisted electroincision of the hypopharyngo-esophageal strictures.
A: An opened posterior view of the hypopharynx showing the submucosal location of the nerves and vessels within the anterior aspect of piriform sinuses. The internal branch of the superior laryngeal nerve lies cranially (proximally) while the recurrent laryngeal nerve lies caudally (inferiorly). An injury to the former may result in anesthesia of the laryngeal mucous membrane as far inferiorly as the vocal cords. An injury to the recurrent laryngeal nerve may lead to ipsilateral vocal cord paralysis. These neuro-vascular structures are important to be protected during the electroincision; B: Cross-sectional view at the level of cricopharynx showing the electro-incision of adhesions with a wire-guided sphincterotome. The sphinterotome is progressively moved laterally towards the pharyngeal wall (along the curved dashed line) with its wire cutting the adhesions in the post-cricoid space and then in the left piriform sinus. Care should be taken to stop few millimetres away from the anterior aspect of piriform sinus to avoid damage to the recurrent laryngeal nerve lying submucosally in this region. Similarly, the internal laryngeal nerve and vessel lie at the same location (in a more cranial cross-section) and need to be protected.
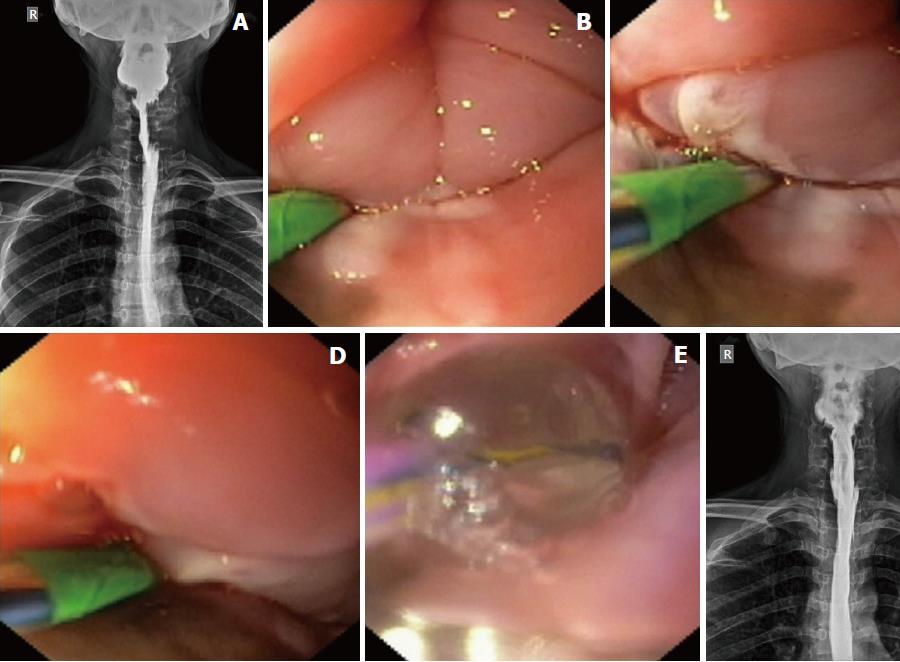
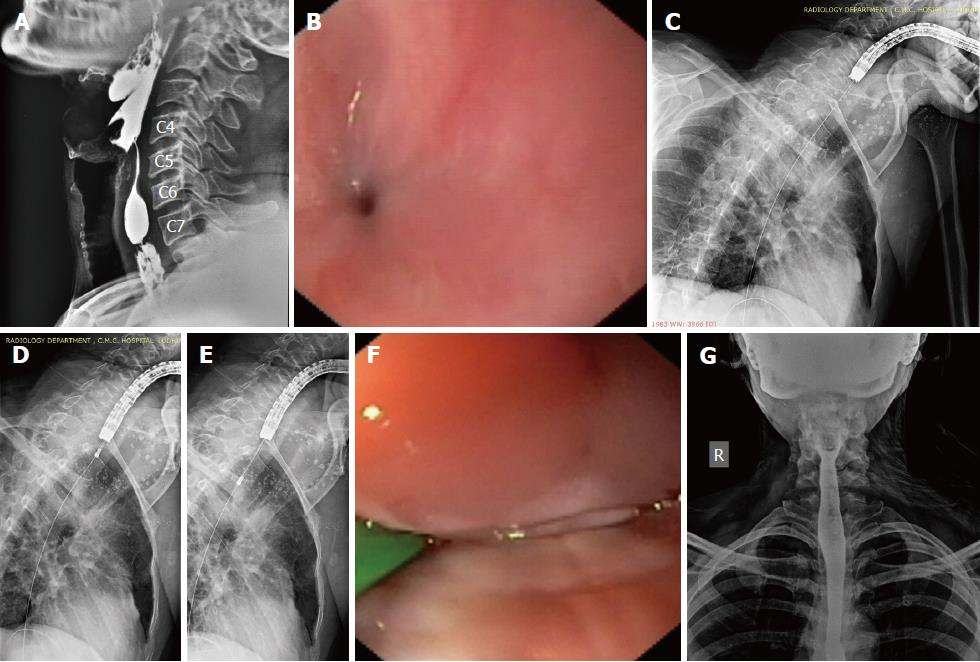
Figure 5 Near-total strictures in case 2 and their management.
A: Lateral view of the esophagogram showing the 2 near-total strictures; B: Endoscopic view through the right piriform sinus showing the tiny opening of the proximal near-total stricture. C: A flexible guide-wire was successfully passed across both the strictures; D, E: A 10F diathermic dilator being passed over the guide-wire to dilate the strictures. This was followed by balloon dilatation; F: Endoscopic view of electroincision (with a wire-guided sphincterotome) of the residual adhesions in the proximal stricture; G: The follow-up esophagogram at 2 wk of the completion of endoscopic therapy.
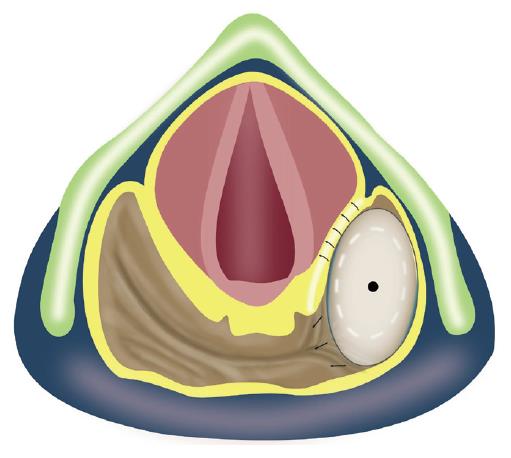
Figure 6 Graphical illustrations to depict the limitations of balloon dilatation for addressing the near-total hypopharyngeal strictures.
As the hypopharyngeal stricture is dilated with the balloon placed in one of the piriform sinuses, there is an interposition of laryngeal structures on its medial aspect. The dilating balloon cannot reach the adhesions in the post-cricoid space and the contralateral piriform sinus, which remain undisrupted. Hence, electeroincision is required to completely open-up the stricture and to prevent the recurrence of symptoms.
- Citation: Dhaliwal HS, Kumar N, Siddappa PK, Singh R, Sekhon JS, Masih J, Abraham J, Garg S. Tight near-total corrosive strictures of the proximal esophagus with concomitant involvement of the hypopharynx: Flexible endoscopic management using a novel technique. World J Gastrointest Endosc 2018; 10(11): 367-377
- URL: https://www.wjgnet.com/1948-5190/full/v10/i11/367.htm
- DOI: https://dx.doi.org/10.4253/wjge.v10.i11.367