Published online Feb 8, 2017. doi: 10.4254/wjh.v9.i4.167
Peer-review started: September 1, 2016
First decision: September 29, 2016
Revised: October 21, 2016
Accepted: December 7, 2016
Article in press: December 9, 2016
Published online: February 8, 2017
Processing time: 160 Days and 23.1 Hours
The low perioperative morbidity and shorter hospital stay associated with laparoscopic hepatectomy have made it an often-used option at many liver centers, despite the fact that many patients with hepatocellular carcinoma have cirrhosis, which makes the procedure more difficult and dangerous. Type of surgical procedure proves not to be a primary risk factor for poor outcomes after hepatic resection for hepatocellular carcinoma, the available evidence clearly shows that laparoscopic hepatectomy is an effective alternative to the open procedure for patients with early-stage hepatocellular carcinoma, even in the presence of cirrhosis. Whether the same is true for patients with intermediate or advanced disease is less clear, since laparoscopic major hepatectomy remains a technically demanding procedure.
Core tip: Type of surgical procedure proves not to be a primary risk factor for poor outcomes after hepatic resection for hepatocellular carcinoma, the available evidence clearly shows that laparoscopic hepatectomy is an effective alternative to the open procedure for patients with early-stage hepatocellular carcinoma, even in the presence of cirrhosis.
- Citation: Zhong JH, Peng NF, Gu JH, Zheng MH, Li LQ. Is laparoscopic hepatectomy superior to open hepatectomy for hepatocellular carcinoma? World J Hepatol 2017; 9(4): 167-170
- URL: https://www.wjgnet.com/1948-5182/full/v9/i4/167.htm
- DOI: https://dx.doi.org/10.4254/wjh.v9.i4.167
Recently, a large propensity score study comparing laparoscopic and open hepatectomy for treating hepatocellular carcinoma (HCC) was published in Ann Surg[1]. This parallel comparison comes at an important time, because technical and procedural improvements have led to increasing use of laparoscopic hepatectomy, including for more extensive hepatectomy and particularly in cases of left lateral sectionectomy[2]. In fact, the low perioperative morbidity and shorter hospital stay associated with laparoscopic hepatectomy have made it an often-used option at many liver centers[3-8], despite the fact that many patients with HCC have cirrhosis, which makes the procedure more difficult and dangerous. The long-term benefits of laparoscopic hepatectomy remain controversial, and this study[1] provides the first evidence that it is associated with better long-term overall survival (OS) than open hepatectomy (P = 0.033).
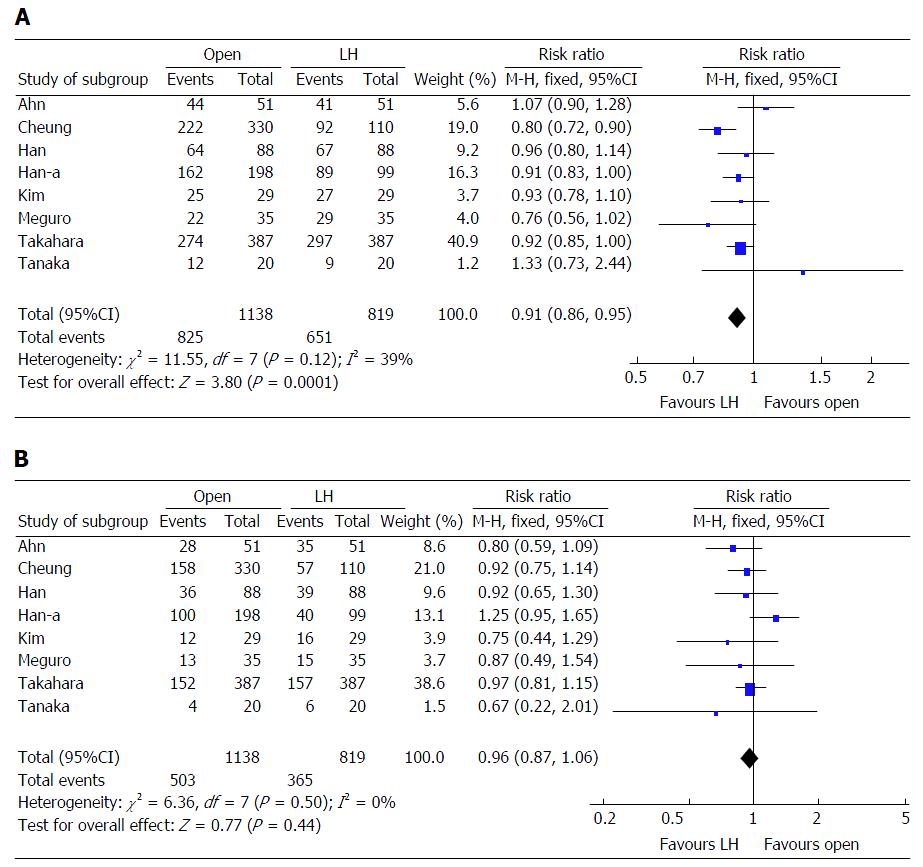
Our own clinical experience and evidence in the literature suggest that mortality risk following liver resection depends primarily not on the type of surgical procedure but on tumor-related factors[9-11]. In order to examine this possibility in more detail, we reviewed all randomized controlled trials and other studies involving propensity score analysis comparing laparoscopic and open hepatectomy published in 2014-2016. We identified 10 studies involving 2275 patients, comprising one from China[1], five from South Korea[12-16], three from Japan[17-19], and one from Italy[20] (Table 1). Across these 10 studies, 90% of patients had single tumors and 84% underwent minor hepatectomy. This means that most patients had early-stage HCC and surgical procedures were relatively straight forward. In 7 of 10 studies (accounting for 73% of all patients), laparoscopic hepatectomy was associated with a significantly lower rate of perioperative morbidity. None of the studies found significant differences in perioperative mortality or disease-free survival (DFS) between the laparoscopic and open procedures. Eight of the 10 studies (accounting for 86% of all patients) reported 5-year OS and DFS[1,12-15,17-19]. Meta-analyses based on these eight studies revealed that patients in the laparoscopic group had significantly higher 5-year OS than those in the open group [risk ratio (RR) = 0.91, 95% confidence interval (95%CI): 0.86-0.95, P < 0.001; I2 = 39%; Figure 1A], but similar 5-year DFS (RR = 0.96, 95%CI: 0.87-1.06, P = 0.440; I2 = 0%; Figure 1B). Similar results were obtained when the study by Cheung et al[1] was excluded.
| Ref. | Country | Included period | Open/laparoscopic | P value | |||||
| Sample size, n | Minor hepatectomy, % | Single tumor, % | Perioperative morbidity, %, P value | Perioperative mortality, %, P value | Overall survival | Disease free survival | |||
| Ahn et al[12] | South Korea | 2005-2013 | 51/51 | 94/96 | 100/100 | 9.8/5.9, 0.470 | 0/0, 1.000 | 0.173 | 0.519 |
| Cheung et al[1] | China | 2002-2015 | 330/110 | 88/90 | 89/91 | 4.8/1.8, 0.2661 | 1.8/0, 0.342 | 0.033 | 0.141 |
| Han et al[13] | South Korea | 2004-2013 | 88/88 | 68/65 | 80/76 | 20.4/12.5, 0.042 | 1.1/1.1, 1.000 | 0.944 | 0.944 |
| Han et al[14] | South Korea | 2002-2012 | 198/99 | 85/84 | 87/93 | 24.7/13.1, 0.020 | - | 0.086 | 0.701 |
| Kim et al[15] | South Korea | 2000-2012 | 29/29 | 100/100 | 83/97 | 13.8/37.9, 0.018 | - | 0.267 | 0.929 |
| Meguro et al[17] | Japan | 2003-2011 | 35/35 | - | 83/80 | 25.7/25.7, 1.000 | - | 0.672 | 0.954 |
| Sposito et al[20] | Italy | 2006-2013 | 43/43 | 100/100 | 81/86 | 48.8/18.6, 0.004 | 0/0, 1.000 | 0.802 | 0.990 |
| Takahara et al[18] | Japan | 2000-2010 | 387/387 | 79/77 | - | 13.0/6.7, 0.003 | 1.0/0.3, 0.178 | 0.358 | 0.422 |
| Tanaka et al[19] | Japan | 2007-2014 | 20/20 | - | 85/90 | 45.0/0, 0.001 | 0/0, 1.000 | 0.606 | 0.533 |
| Yoon et al[16] | South Korea | 2007-2011 | 174/58 | 88/93 | 100/100 | 22.4/6.9, 0.020 | - | 0.480 | 0.31 |
Thus, substantial evidence suggests that laparoscopic hepatectomy is associated with significantly better long-term OS than open hepatectomy. It is possible that this reflects less tissue manipulation - and therefore less hematogenous dissemination of malignant tumor cells-in “no-touch” anterior-approach laparoscopic hepatectomy[1]. However, the two techniques were associated with similar DFS, indicating similar rates of tumor recurrence, which is the main cause of death among HCC patients. In fact, patients in the two groups across all 10 studies showed similar tumor characteristics, including diameter, number, vascular invasion, and New Edmondson grade. Since these characteristics are the main risk factors of tumor recurrence, the available evidence appears to be consistent with the idea that mortality risk following liver resection depends on tumor-related factors and not on type of surgical procedure.
To examine this hypothesis rigorously, at least two questions must be answered. One is whether differences in blood loss and surgical complexity may help explain the difference in OS. Six of the 10 studies[1,13,16-19] reported significantly less blood loss in the laparoscopic group, yet the studies did not report whether tumors were close to the hepatic vein or portal hepatis, which would make the surgery more complex and increase risk of blood loss. Another question is whether economic differences may help explain the OS difference. Since laparoscopic hepatectomy costs substantially more than open hepatectomy, it stands to reason that patients opting for the laparoscopic procedure may be in a better financial position. This raises the possibility that such patients also receive better postoperative therapies, such as antiviral therapy, liver-protecting therapy, and/or psychological intervention. Such patients may also receive more extensive and/or more aggressive therapy after tumor recurrence. All these factors may explain the observed long-term OS advantage of laparoscopic hepatectomy over open hepatectomy. Therefore, assessing the long-term impact of this procedure requires large randomized controlled trials that take surgical complexity and patient financial condition into account. At least, comparative studies with propensity score analysis should adjust surgical complexity and financial condition between groups.
Even if, as we suspect, type of surgical procedure proves not to be a primary risk factor for poor outcomes after resection, the available evidence clearly shows that laparoscopic hepatectomy is an effective alternative to the open procedure for patients with early-stage HCC, even in the presence of cirrhosis. Whether the same is true for patients with intermediate or advanced disease is less clear, since laparoscopic major hepatectomy remains a technically demanding procedure. Even so, we agree that laparoscopic hepatectomy is an alternative choice for treatment of HCC.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kao JT, Yang T S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Cheung TT, Dai WC, Tsang SH, Chan AC, Chok KS, Chan SC, Lo CM. Pure Laparoscopic Hepatectomy Versus Open Hepatectomy for Hepatocellular Carcinoma in 110 Patients With Liver Cirrhosis: A Propensity Analysis at a Single Center. Ann Surg. 2016;264:612-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 140] [Article Influence: 15.6] [Reference Citation Analysis (1)] |
| 2. | Cheung TT, Poon RT, Dai WC, Chok KS, Chan SC, Lo CM. Pure Laparoscopic Versus Open Left Lateral Sectionectomy for Hepatocellular Carcinoma: A Single-Center Experience. World J Surg. 2016;40:198-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Li W, Zhou X, Huang Z, Zhang K, Luo X, Zhong J, Chen Y. Short-term and long-term outcomes of laparoscopic hepatectomy, microwave ablation, and open hepatectomy for small hepatocellular carcinoma: a 5-year experience in a single center. Hepatol Res. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Dong HH, Mei B, Liu FL, Zhang ZW, Zhang BX, Huang ZY, Chen XP, Zhang WG. Laparoscopic versus traditional open splenectomy for hepatocellular carcinoma with hypersplenism. J Huazhong Univ Sci Technolog Med Sci. 2016;36:519-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Guro H, Cho JY, Han HS, Yoon YS, Choi Y, Periyasamy M. Current status of laparoscopic liver resection for hepatocellular carcinoma. Clin Mol Hepatol. 2016;22:212-218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Martin RC, Mbah NA, St Hill R, Kooby D, Weber S, Scoggins CR, Maithel SK. Laparoscopic versus open hepatic resection for hepatocellular carcinoma: improvement in outcomes and similar cost. World J Surg. 2015;39:1519-1526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Memeo R, de’Angelis N, Compagnon P, Salloum C, Cherqui D, Laurent A, Azoulay D. Laparoscopic vs. open liver resection for hepatocellular carcinoma of cirrhotic liver: a case-control study. World J Surg. 2014;38:2919-2926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 134] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 8. | Toriguchi K, Hatano E, Sakurai T, Seo S, Taura K, Uemoto S. Laparoscopic liver resection in obese patients. World J Surg. 2015;39:1210-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Zhong JH, Ke Y, Gong WF, Xiang BD, Ma L, Ye XP, Peng T, Xie GS, Li LQ. Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma. Ann Surg. 2014;260:329-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 375] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 10. | Zhong JH, You XM, Lu SD, Wang YY, Xiang BD, Ma L, Wu FX, Yuan WP, Chen Y, Li LQ. Historical Comparison of Overall Survival after Hepatic Resection for Patients With Large and/or Multinodular Hepatocellular Carcinoma. Medicine (Baltimore). 2015;94:e1426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Zhong JH, Rodríguez AC, Ke Y, Wang YY, Wang L, Li LQ. Hepatic resection as a safe and effective treatment for hepatocellular carcinoma involving a single large tumor, multiple tumors, or macrovascular invasion. Medicine (Baltimore). 2015;94:e396. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 107] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 12. | Ahn KS, Kang KJ, Kim YH, Kim TS, Lim TJ. A propensity score-matched case-control comparative study of laparoscopic and open liver resection for hepatocellular carcinoma. J Laparoendosc Adv Surg Tech A. 2014;24:872-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Han DH, Choi SH, Park EJ, Kang DR, Choi GH, Choi JS. Surgical outcomes after laparoscopic or robotic liver resection in hepatocellular carcinoma: a propensity-score matched analysis with conventional open liver resection. Int J Med Robot. 2015;12:735-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Han HS, Shehta A, Ahn S, Yoon YS, Cho JY, Choi Y. Laparoscopic versus open liver resection for hepatocellular carcinoma: Case-matched study with propensity score matching. J Hepatol. 2015;63:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 199] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 15. | Kim H, Suh KS, Lee KW, Yi NJ, Hong G, Suh SW, Yoo T, Park MS, Choi Y, Lee HW. Long-term outcome of laparoscopic versus open liver resection for hepatocellular carcinoma: a case-controlled study with propensity score matching. Surg Endosc. 2014;28:950-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 16. | Yoon SY, Kim KH, Jung DH, Yu A, Lee SG. Oncological and surgical results of laparoscopic versus open liver resection for HCC less than 5 cm: case-matched analysis. Surg Endosc. 2015;29:2628-2634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 17. | Meguro M, Mizuguchi T, Kawamoto M, Ota S, Ishii M, Nishidate T, Okita K, Kimura Y, Hirata K. Clinical comparison of laparoscopic and open liver resection after propensity matching selection. Surgery. 2015;158:573-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Takahara T, Wakabayashi G, Beppu T, Aihara A, Hasegawa K, Gotohda N, Hatano E, Tanahashi Y, Mizuguchi T, Kamiyama T. Long-term and perioperative outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci. 2015;22:721-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 200] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 19. | Tanaka S, Takemura S, Shinkawa H, Nishioka T, Hamano G, Kinoshita M, Ito T, Kubo S. Outcomes of Pure Laparoscopic versus Open Hepatic Resection for Hepatocellular Carcinoma in Cirrhotic Patients: A Case-Control Study with Propensity Score Matching. Eur Surg Res. 2015;55:291-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Sposito C, Battiston C, Facciorusso A, Mazzola M, Muscarà C, Scotti M, Romito R, Mariani L, Mazzaferro V. Propensity score analysis of outcomes following laparoscopic or open liver resection for hepatocellular carcinoma. Br J Surg. 2016;103:871-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |