Published online Nov 28, 2017. doi: 10.4254/wjh.v9.i33.1253
Peer-review started: May 10, 2017
First decision: June 30, 2017
Revised: September 1, 2017
Accepted: September 15, 2017
Article in press: September 15, 2017
Published online: November 28, 2017
Processing time: 203 Days and 4.8 Hours
Heart failure (HF) following liver transplant (LT) surgery is a distinct clinical entity with high mortality. It is known to occur in absence of obvious risk factors. No preoperative workup including electrocardiogram, echocardiography at rest and on stress, reasonably prognosticates the risk. In patients of chronic liver disease, cirrhotic cardiomyopathy, alcoholic cardiomyopathy, and stress induced cardiomyopathy have each been implicated as a cause for HF after LT. However distinguishing one etiology from another not only is difficult, several etiologies may possibly coexist in a given patient. Diagnostic dilemma is further compounded by the fact that presentation and management of HF irrespective of the possible underlying cause, remains the same. In this case series, 6 cases are presented and in the light of existing literature modification in the preoperative workup are suggested.
Core tip: Heart failure following liver transplant surgery occurs in absence of any obvious risk factors and is associated with high mortality. No preoperative workup including electrocardiogram, echocardiography at rest and on stress, reasonably prognosticates the risk. While cirrhotic cardiomyopathy, alcoholic cardiomyopathy, and stress induced cardiomyopathy each have been implicated, distinguishing one from another is difficult and several etiologies may possibly coexist. In this case series, 6 cases are presented and in the light of existing literature modification in the preoperative workup are suggested.
- Citation: Tandon M, Karna ST, Pandey CK, Chaturvedi R. Diagnostic and therapeutic challenge of heart failure after liver transplant: Case series. World J Hepatol 2017; 9(33): 1253-1260
- URL: https://www.wjgnet.com/1948-5182/full/v9/i33/1253.htm
- DOI: https://dx.doi.org/10.4254/wjh.v9.i33.1253
Heart failure (HF) is defined as “Inability of the heart to keep up with the demands on it and, specifically, failure of the heart to pump blood with normal efficiency”. HF following liver transplant (LT) surgery is recognized as a distinct clinical entity with a prevalence of 3%-7%[1,2].
On retrospective analysis of 360 recipients who underwent liver transplantation at our tertiary care institute from 2011 to 2016, we identified six patients who developed heart failure in the immediate postoperative period. We diagnosed heart failure by severely decreased left ventricle ejection fraction (LVEF) on echocardiography. Clinical presentation was similar in all six recipients, only two survived. The details of each case are presented with discussion of different etiologies and specific management (Table 1).
| (S No.) Demography, age, gender, etiology MELD score | Cardiology workup EKG, QTc, CI, echocardiography EF, DSE | Clinical course: Intraop, post op | CPKMB % of Ck on diagnosis of HF (normal 3%-5%)[25] | Possible underlying cause of heart failure in decreasing order of possibility | Outcome |
| (1) 38 yr, male, cryptogenic, MELD 16 | QTc < 445 ms CI: Present EF: 65% DSE: Inconclusive | Uneventful LDLT; Extubated POD 1; Pul. Edema POD 2; EF: 25% | 16.80% | CiCd ABS CAD ALC | EF recovered to 40% on POD 4; EF: 55% on discharge at POD 25; Survived to discharge; |
| (2) 53 yr, male, ethanol MELD 35 | QTc: 519 ms CI: Absent EF: 65% DSE: Negative for inducible ischemia | Uneventful LDLT; Portal vein thrombectomy; Terlipressin infusion preop and intraop; POD 1: EF: 25%; Gram negative sepsis with MOD | 15.10% | ALC CiCd CAD ABS | EF recovered to 55% at POD 10; Died |
| (3) 55 yr, female, EHPVO with intraparenchymal extension, MELD 15 | QTc: 532 ms CI: Absent EF: 65% DSE: Negative for inducible ischemia | Turbulent LDLT; Increasing inotrope and vasopressor requirement; EF: 20%; Severe vasoplegia | 14.68% | ABS CiCd CAD ALC | EF never recovered; Vasoplegia did not respond; Died |
| (4) 26 yr female, ALF | QTc: 540 ms CI: Absent EF: 70% DSE: Not done | Uneventful LDLT; Re-exploration POD2 for bleed; SVT; EF: 25%; | 14.84% | ABS CiCd CAD ALC | EF recovered to 50% at POD 4; Died |
| (5) 40 yr, male, ethanol MELD 21 | QTc: 550 ms CI: Absent EF: 65% DSE: Negative for inducible ischemia | Uneventful DDLT POD1: EF: 30% | Not done | ALC CiCd ABS CAD | EF recovered to 40% at POD 4; Survived |
| (6) 38 yr, male, ethanol MELD 32 | QTc: 550 ms CI: Absent EF: 65% DSE: Negative for inducible ischemia | Uneventful; POD 1: EF: 20%; Recurrent SVT | 39.40% | ALC CiCd ABS CAD | EF never recovered; Died |
A 38-year-old male with cryptogenic chronic liver disease with a “model for end stage disease” (MELD) score of 16 underwent uneventful live related liver transplantation. No abnormality was detected in preoperative electrocardiogram (EKG) and resting echocardiography. The Dobutamine stress echocardiography (DSE) was inconclusive due to chronotropic incompetence (failure to achieve target heart rate). Patient was weaned from mechanical ventilation and trachea was extubated six hours after surgery.
Twelve hours after extubation, patient complained of dyspnoea with coarse crepitations suggestive of pulmonary edema unresponsive to diuretics necessitating reintubation with supportive mechanical ventilation. Soon, hemodynamic instability sets in with increasing inotropes requirement to maintain perfusion pressures. Transthoracic Echocardiography (TTE) diagnosed left ventricle (LV) systolic failure with LVEF of 25% and increased systemic vascular resistance (SVR) of 1400 dynes.sec.cm-5. “Troponin T” test was negative but Creatine kinase-MB (CK-MB) was elevated (16.8% of CK).
Pharmacologic intervention was aimed at decreasing pre- and after load using-injection Labetalol, and Nitroglycerine. Low perfusion pressure (mean blood pressure-50 mmHg) was accepted. SVR was maintained between 800-900 dynes.sec.cm-5. Mechanical ventilation was continued for 4 d. LV ejection fraction improved over the period from 25% to 40%. Patient was weaned off mechanical ventilation on POD 5 (postoperative day). Labetalol infusion was continued and was replaced with oral doses from POD 8 onwards. Patient made complete recovery and was discharged from hospital with LVEF of 55% on POD 26.
A 53-year-old male with ethanol related CLD, MELD score of 35, chronic smoker with 6 mo abstinence presented for LT. His preoperative TTE at rest showed normal ejection fraction of 65% with absence of inducible ischemia on DSE. His ECG was unremarkable but for a prolonged rate corrected QT (QTc) interval of 519 ms. Patient had acute kidney injury (AKI) for which Terlipressin infusion was started in the preoperative period and was continued perioperatively. His portal vein was thrombosed and required thrombectomy.
On POD 1, inotropes requirement increased with a high normal SVR and low stroke volume variation (< 10%). On TTE, LV systolic failure with LV EF of 25% was diagnosed. Hemodynamic parameters were supported using Dobutamine and Nor-adrenaline infusion. “Troponin T” test was inconclusive while Creatine kinase-MB (CK-MB) was elevated (15.1% of CK). Supportive care with mechanical ventilation was continued and LVEF improved over next 10 d. However, sepsis with gram negative infections led to multi-organ dysfunction resulting in patient mortality on the 14th POD.
A 55-year-old female with cirrhosis due to extrahepatic portal vein obstruction with intraparenchymal extension with MELD of 9 presented for LT surgery. Her TTE at rest as well as DSE was normal. On her ECG, QTc interval was prolonged (532 ms). Packed red blood cells (15 units) were transfused during the surgery on account of blood loss during dissection of her native liver. In the immediate postoperative period, with progressive increase in inotropes and vasopressors requirement, it became difficult to maintain perfusion pressures. LV failure with EF of 20% was diagnosed on Transesophageal echocardiography (TEE). CK-MB was raised (14.68% of CK). In spite of maximal therapeutic management, hemodynamics deteriorated on second postoperative day leading to multiorgan dysfunction and death.
A 26-year-old female with acute liver failure of unknown etiology with normal preoperative TTE, an unremarkable EKG but for a prolonged QTc interval (540 ms) underwent uneventful liver transplantation. She was weaned off respiratory support after overnight mechanical ventilation. The postoperative course was complicated with hemoperitoneum on second day necessitating emergency laparotomy. Bleeder was identified and repaired. During this surgery, she had an episode of ventricular tachycardia which responded to lignocaine bolus. Subsequent to VT, LV EF was decreased (25%). The “Troponin T” test was inconclusive while CK-MB was increased (14.84% of CK). Over next four days, LV EF improved to 40%. Hemodyamics were supported during this period using dobutamine infusion which was then tapered and trachea was extubated after successful sponataneous breathing trial. However, on 7th POD, sepsis was diagnosed with positive microbiological cultures which led to multiorgan dysfunction and refractory vasoplegia. She succumbed to septic shock and died on POD 18.
A 40-year-old male with ethanol related CLD with MELD score of 21 presented for LT. Preoperative EKG and TTE at rest were normal with LVEF of 60%. DSE was negative for inducible ischemia. After uneventful deceased donor liver transplantation (DDLT), patient was weaned off mechanical ventilation, 5 h after the surgery. On POD 1, patient developed respiratory distress with pulmonary edema, global hypokinesia with LVEF of 30% was diagnosed on TTE. Troponin T card test was negative. Systemic vascular resistance was 1250 dynes.sec.cm-5. Noninvasive mechanical ventilation support was instituted along with preload and after-load reduction with Nitroglycerine infusion and Tablet Amlodepine. Tablet Prazocin was added subsequently. Patient improved symptomatically. LVEF improved to 40% by POD 4. Nitroglycerine infusion was tapered off while Tablet Prazocin and Tablet Amlodepine were continued. Patient was discharged to home with normal LVEF.
A 38-year-old male with ethanol related CLD with MELD score of 32 underwent deceased donor liver transplant (DDLT). His preoperative Echocardiography was negative for inducible ischemia with minimal left to right intrapulmonary shunting with prolongation of QTc interval on EKG. Patient was weaned off mechanical ventilation on POD 2. On postoperative day 3, he developed low cardiac output with pulmonary edema with LVEF of 20% on TTE. CK-MB was elevated (39.4% of CK). Mechanical ventilation with tracheal intubation was initiated while hemodynamic was supported using Nitroglycerine and Levosimendan infusion. Patient developed recurrent tachyarrhythmia in absence of any obvious electrolyte disorder for which Amiodarone was given. Patient was weaned off mechanical ventilation after 2 d but had to be re-intubated very next day on account of repeat episode of supra-ventricular tachycardia (SVT) with pulmonary edema. Subsequently several attempts to wean off mechanical ventilation were not successful. SVT continued to re-occur. Tracheostomy was done and patient was given increasing duration of spontaneous breath trials. However LVEF failed to improve and patient died on POD 29.
We observed heart failure after LT even with normal preoperative echocardiography, negative DSE for inducible ischemia and without any obvious cause. Literature suggests a “non-ischemic” cause for the systolic failure with after LT[3,4].
Cardiac risk factors have been identified in patients with chronic liver disease. These include coronary artery disease (CAD) (6%-26%), valvular heart disease (27.5%), asymptomatic foramen ovale (4%), cirrhotic cardiomyopathy (CiCd) (40%-90%), portopulmonary hypertension (2%-14%) and other diseases like amylodosis and hemochromatosis (45%). Cumulative risk of mortality in presence of these risk factors has been calculated to be 50%. Of these, presence of cirrhotic cardiomyopathy alone is associated with 3%-7% risk of severe HF in the post-operative period with 45% risk of mortality[5].
General: Presence of diabetes, hypertension, mean arterial pressure ≤ 65 mmHg, mean pulmonary artery pressure ≥ 30 mmHg, mean pulmonary capillary wedge pressure ≥ 15 mmHg, hemodialysis and brain natriuretic peptide (BNP) level (> 50 pg/mL) have been found to be predictive for the development of new-onset systolic heart failure after liver transplantation[1,5].
Etiology specific cirrhotic cardiomyopathy: Cirrhotic cardiomyopathy (CiCd) is defined as a “form of chronic cardiac dysfunction in patients with cirrhosis, characterized by blunted contractile responsiveness to stress, and/or altered diastolic relaxation with electrophysiological abnormalities in the absence of other known cardiac disease”[6].
QTc interval prolongation is a typical feature of CiCD. It is observed more frequently in patients who died after LT than in survivors and QTc interval > 450 ms have been found to be predictive for the development of new-onset systolic heart failure after liver transplantation[7]. We found increased preoperative QTc > 450 ms in 4 out of the 6 recipients with CLD who developed postoperative heart failure. Chronotropic incompetence, another feature of CiCd, was however observed only in one of these 6 recipients.
Alcoholic cardiomypopathy: Alcoholic cardiomyopathy shares pathophysoiology with CiCd. However, the co-existence of liver disease due to cirrhosis may give rise to diagnostic confusion and is therefore a diagnosis of exclusion[8]. Three out of these 6 recipients with postoperative heart failure had ethanol related liver disease and therefore could have had alcoholic cardiomyopathy. Association between Alcoholic cardiomyopathy and Supraventricular arrhythmias is known[9]. Alcoholics with simultaneous cardiomyopathy and cirrhosis are known to have a poor prognosis[10]. Case number 6 discussed in this report had supraventricular arrhythmias in the setting of HF after LT for ethanol related CLD and he did not survive.
Coronary artery disease: The prevalence of CAD in LT candidates over the age of 45-50 years ranges between 6% and 26%. Two of our patients were older than 50-year-old but had no symptoms suggestive of cardiac disease. Even preoperative DSE was negative for inducible ischemia.
Due to presence of ascites, poor nutritional status, cachexia, limited physical activity, it is difficult to diagnosis CAD in patients with CLD. In presence of limited physical activity, presenting signs and symptoms of angina and or angina equivalent are either not present or are not attributable to CAD. DSE has limited usefulness for diagnosing CAD in patients with CLD as it is often inconclusive in such patients due to chronotropic incompetence with resultant failure to achieve target heart rate. Similarly Dipyridamole or Adenosine nuclear myocardial perfusion scan also remain inconclusive as coronary vasculature is already maximally dilated in cirrhotics and therefore like DSE, are relied upon for their negative predictive value only.
Alternative tests like Single-photon emission computed tomography (SPECT) scanning, Cardiac magnetic resonance imaging, Carotid intima-media thickness, and Coronary artery calcification score (CACS) measured by computerized tomography have also been used to investigate presence of coronary artery disease though they have their own limitations[11].
Stress-related cardiomyopathy: Early-onset HF after surgery, directly reflects surgery related stress to the myocardium or hemodynamic changes. Stress related cardiomyopathy therefore cannot be missed as a cause of systolic heart failure in the perioperative period of non-cardiac surgery[12]. Similar conclusion was drawn by Mandell et al[1] who concluded that patients having HF after LT, either suffered from stress cardiomyopathy and therefore had no evidence of impaired contraction before the event or the echocardiographic predictors of HF were masked by circulatory changes in patients with cirrhosis.
Stress induced cardiomyopathy, or acute broken heart syndrome (ABS) also known as Takotsubo cardiomyopathy is understood to be caused by catecholamine surge which leads to diffuse microvascular spasm to cause myocardial stunning and HF. ABS and myocardial infarction (MI) share similar clinical and ECG presentation and blood biochemical tests.
To distinguish fromMI and for diagnosing ABS, Mayo clinic has therefore proposed following 4 point criteria[13]: (1) transient LV Systolic dysfunction (hypokinesis, akinesis, dyskinesis): The wall motion abnormalities are typically regional and extend beyond a single epicardial coronary distribution; (2) absence of obstructive coronary disease or angiographic evidence of acute plaque rupture. If coronary disease is found, the diagnosis of stress cardiomyopathy can still be made if the wall motion abnormalities are not in the distribution of the coronary disease; (3) new electrocardiographic abnormalities (either ST-segment elevation and/or T wave inversion) or modest elevation in cardiac troponin; and (4) absence of pheochromocytoma or myocarditis.
Patients in this case series satisfied 3 out of the 4 criteria except for the absence of obstructive coronary lesion or angiographic evidence of acute plaque rupture, which could not be ruled out in absence of coronary angiogram.
Serum cardiac troponin levels and brain natriuretic peptide (BNP) or N-terminal pro-BNP are elevated in most patients with stress cardiomyopathy in the International Takotsubo Registry study[14]. In the patients discussed, while Troponin card test was negative and BNP levels were not done, CPK MB was elevated. These patients therefore could have had ABS manifesting as HF.
In the present case series, only two patients, case No. 2 and 3, aged 53 and 55 years and possibly case No. 5 aged 40 in view of age and lifestyle were at risk of having CAD and these three patients were able to achieve target heart rates on DSE (Otherwise a limitation in patients with cirrhosis of Liver). DSE in these patients was negative for inducible ischemia. Considering this with ongoing hemodynamic instability and presence of global and not regional wall motion abnormality specific to any coronary artery supplied region and the younger age of rest of the patients, decision was taken to not to do coronary angiogram in these patients.
Most patients discussed in this case series had several possible etiologies responsible for the observed heart failure which could not have been definitely identified from one another. In absence of coronary angiogram, evidence against CAD is only circumstantial and therefore cannot be completely ruled out. Diagnosis of ALC and CiCd also cannot be certainly made except on the basis of history of ethanol abuse and presence underlying chronic liver disease. Similarly the diagnosis of ABS in absence of coronary angiogram does not entirely satisfy the Mayo’s diagnostic criteria and is also possibly a diagnosis of convenience. It is also possible that several etiologies might be coexisting and therefore the high mortality in these patients.
In a prospective study of “myocardial injury after noncardiac surgery” (MINS), troponin elevations, any peak Troponin T (TnT) of 0.03 ng/mL or greater, without a non-ischemic explanation (e.g., sepsis and pulmonary embolus) was diagnostic of MINS[15]. Patients with MINS were at higher risk of congestive heart failure (OR, 10.34; 95%CI: 7.99-13.37, P < 0.001) compared with patients who did not suffer MINS. In another study, mortality increased exponentially as a function of peak postoperative troponin concentration[16].
In the setting of surgery for LT, Coss et al[17] in a multivariate analysis of 230 transplant recipients found that an abnormal pretransplant troponin I level (> 0.07 ng/mL) predicted postoperative cardiovascular complications in their patients. They concluded that raised Toponin I levels > 50 pg/mL indicate latent cardiac dysfunction that is not recognized by conventional screening methods[17].
While quantitative assay of troponin is not available at our institute, we observed negative test on qualitative analysis using Trop T sensitive test Card test (detects Troponin T ≥ 0.1 ng/mL in blood). Creatine kinase-MB (CK-MB) was done and was significantly elevated soon after the clinical and echocardiography diagnosis of HF in our patients in absence of any other identifiable cause for the same.
Another novel marker, BNP level and QTc interval > 450 ms were concluded to be predictive for the development of new-onset systolic heart failure after LT in a study by Qureshi et al[3].
Therapeutic strategies for addressing this acute and possibly life-threatening complication of heart failure after LT are not well defined. Similarly there is no established treatment for patients suffering MINS. In light of findings of decreased 30 d mortality in POISE trial (PeriOperative Ischemic Evaluation), acetyl-salicylic acid and statin therapy may possibly benefit patients who suffer MINS[18-20].
CiCd, Alcoholic cardiomyopathy, and ABS, all are characterized by inotropic incompetence. After LT, blood pressure is known to rise significantly which may possibly precipitate inotropic incompetence and subsequent HF in such patients[21,22]. Management of heart failure in the post-LT period therefore does not differ from usual heart failure therapies. Diuretics, inotropes, inodilators and vasopressor support form the foundation pillars of treatment.
Heart failure guidelines, such as those adopted by the European Society of Cardiology or the American College of Cardiology/American Heart Association should be followed. Cardio-selective Beta-blockers, ACE inhibitors or angiotensin receptor blockers (ARBs), diuretics and digitalis may be used for management of HF after LT. It is important to treat the adrenergic surge causing raised systemic vascular resistance and also to manage the preload to avoid further worsening of cardiac function. In our case series, LVEF of 4 out of 6 patients recovered with use of therapy aimed at decreasing pre- and after load and adrenergic surge.
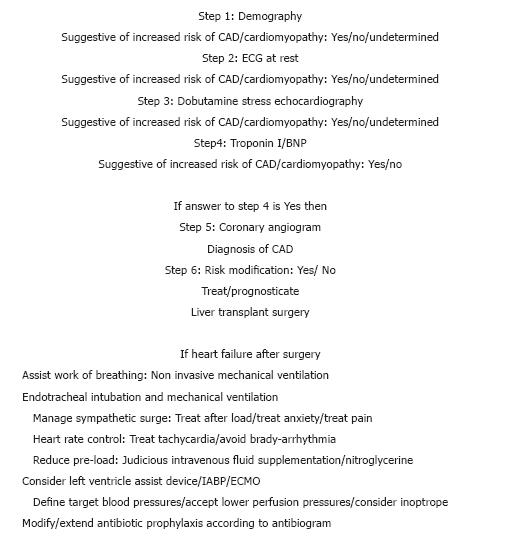
Several authors have reported successful outcome after aggressive management of HF following LT using extracorporeal membrane oxygenator (ECMO) and ventricular assist device (VAD), though cost may be a constraint[4,23,24]. Considering advances in clinically applied biomarkers and success of aggressive measures in managing such cases, a stepwise approach to identify patients at risk and for management should be adopted (Figure 1).
In our series, out of 6 patients, only 2 survived despite recovery of EF. Survival therefore is perhaps determined by factors other than myocardial performance like duration and severity of liver disease, presentation either acute or chronic, age of the patient, co-morbid conditions and presence of sepsis. Two patients who survived were relatively younger, aged 38 and 40 years and had chronic and not acute liver disease. Those who did not survive either had ALF or increased severity of CLD as reflected in their MELD scores or additional insult in form of sepsis in the setting of HF.
In conclusion, high MELD, Acute liver failure and sepsis in the setting of Heart failure after LT are probably associated with grave prognosis. While different etiologies may cause HF after LT, combination of several may possibly coexist. It may be prudent to routinely do quantitative Troponin I and/or BNP levels before LT surgery to identify and prognosticate recipients likely to be complicated by heart failure. While Heart Rate control, preload and after-load reduction are the pillars of management, ECMO and VAD may allow sufficient time for recovery of heart failure. In view of the limitations of the commonly used diagnostic modalities and poor outcome, better aides to identify patients at risk are needed which would require greater interdisciplinary interaction involving clinicians and laboratory scientists. Till such time, this entity, Heart failure after Liver transplant continues to remain an enigma.
Patients of acute liver failure and of chronic liver disease, presenting with systolic heart failure within 7 d after the liver transplant surgery in absence of any preoperatively identified and obvious predisposing risk factor.
Systolic heart failure was diagnosed on basis of clinical presentation and echocardiography with greatly reduced left ventricle ejection fraction.
Liver graft dysfunction and severe sepsis may cause hemodynamic instability and were ruled out. Underlying cause for the observed systolic heart failure could not be made.
Creatine kinase-MB was elevated upon diagnosis of systolic heart failure after liver transplant. Troponin T sensitive card test was negative.
Severely reduced left ventricle ejection fraction was diagnosed on echocardiography.
Could not be made conclusively.
Respiration was assisted. Hemodynamics supported using inotropes and inodilators and beta blockers, aimed at preload and after load reduction. Sedation and analgesia were taken care of to reduce sympathetic adrenergic activity.
Cirrhotic cardiomyopathy and alcohol cardiomyopathy have been described as specific clinical entities that describe cardiomyopathy in setting of underlying chronic liver disease and with history of alcohol indulgence respectively. Acute broken heart syndrome describes the cardiomyopathy typically seen under stressful conditions and not necessarily after surgery and is said to resemble acute myocardial infarction.
In absence of established clinical features and limitations of existing prevalent diagnostic modalities, Bio-chemical makers like BNP and Troponin I may be routinely done as part of preoperative workup of patients posted for liver transplant surgery to help identify patients at greater risk of heart failure after the surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chuang WL, Ohkohchi N, Rodriguez-Peralvarez ML S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Mandell MS, Seres T, Lindenfeld J, Biggins SW, Chascsa D, Ahlgren B, Wachs M, Bambha KM. Risk factors associated with acute heart failure during liver transplant surgery: a case control study. Transplantation. 2015;99:873-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Eimer MJ, Wright JM, Wang EC, Kulik L, Blei A, Flamm S, Beahan M, Bonow RO, Abecassis M, Gheorghiade M. Frequency and significance of acute heart failure following liver transplantation. Am J Cardiol. 2008;101:242-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 3. | Qureshi W, Mittal C, Ahmad U, Alirhayim Z, Hassan S, Qureshi S, Khalid F. Clinical predictors of post-liver transplant new-onset heart failure. Liver Transpl. 2013;19:701-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Schnell F, Donal E, Lorho R, Lavoué S, Gacouin A, Compagnon P, Boudjema K, Mabo P, Le Tulzo Y, Camus C. Severe left-sided heart failure early after liver transplantation. Liver Transpl. 2009;15:1296-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Ripoll C, Yotti R, Bermejo J, Bañares R. The heart in liver transplantation. J Hepatol. 2011;54:810-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Møller S, Henriksen JH. Cardiovascular complications of cirrhosis. Gut. 2008;57:268-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 281] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 7. | Mohamed R, Forsey PR, Davies MK, Neuberger JM. Effect of liver transplantation on QT interval prolongation and autonomic dysfunction in end-stage liver disease. Hepatology. 1996;23:1128-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 128] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | George A, Figueredo VM. Alcoholic cardiomyopathy: a review. J Card Fail. 2011;17:844-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | George A, Figueredo VM. Alcohol and arrhythmias: a comprehensive review. J Cardiovasc Med (Hagerstown). 2010;11:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Henriksen JH, Møller S. Cardiac and systemic haemodynamic complications of liver cirrhosis. Scand Cardiovasc J. 2009;43:218-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Davidson CJ, Gheorghiade M, Flaherty JD, Elliot MD, Reddy SP, Wang NC, Sundaram SA, Flamm SL, Blei AT, Abecassis MI. Predictive value of stress myocardial perfusion imaging in liver transplant candidates. Am J Cardiol. 2002;89:359-360. [PubMed] |
| 12. | Silvestre OM, Farias AQ, Bacal F. Early-onset and late-onset heart failure after liver transplantation. Liver Transpl. 2014;20:122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Kawai S, Kitabatake A, Tomoike H; Takotsubo Cardiomyopathy Group. Guidelines for diagnosis of takotsubo (ampulla) cardiomyopathy. Circ J. 2007;71:990-992. [PubMed] |
| 14. | Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015;373:929-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1401] [Cited by in RCA: 1717] [Article Influence: 171.7] [Reference Citation Analysis (1)] |
| 15. | Botto F, Alonso-Coello P, Chan MT, Villar JC, Xavier D, Srinathan S, Guyatt G, Cruz P, Graham M, Wang CY, Berwanger O, Pearse RM, Biccard BM, Abraham V, Malaga G, Hillis GS, Rodseth RN, Cook D, Polanczyk CA, Szczeklik W, Sessler DI, Sheth T, Ackland GL, Leuwer M, Garg AX, Lemanach Y, Pettit S, Heels-Ansdell D, Luratibuse G, Walsh M, Sapsford R, Schünemann HJ, Kurz A, Thomas S, Mrkobrada M, Thabane L, Gerstein H, Paniagua P, Nagele P, Raina P, Yusuf S, Devereaux PJ, Devereaux PJ, Sessler DI, Walsh M, Guyatt G, McQueen MJ, Bhandari M, Cook D, Bosch J, Buckley N, Yusuf S, Chow CK, Hillis GS, Halliwell R, Li S, Lee VW, Mooney J, Polanczyk CA, Furtado MV, Berwanger O, Suzumura E, Santucci E, Leite K, Santo JA, Jardim CA, Cavalcanti AB, Guimaraes HP, Jacka MJ, Graham M, McAlister F, McMurtry S, Townsend D, Pannu N, Bagshaw S, Bessissow A, Bhandari M, Duceppe E, Eikelboom J, Ganame J, Hankinson J, Hill S, Jolly S, Lamy A, Ling E, Magloire P, Pare G, Reddy D, Szalay D, Tittley J, Weitz J, Whitlock R, Darvish-Kazim S, Debeer J, Kavsak P, Kearon C, Mizera R, O’Donnell M, McQueen M, Pinthus J, Ribas S, Simunovic M, Tandon V, Vanhelder T, Winemaker M, Gerstein H, McDonald S, O’Bryne P, Patel A, Paul J, Punthakee Z, Raymer K, Salehian O, Spencer F, Walter S, Worster A, Adili A, Clase C, Cook D, Crowther M, Douketis J, Gangji A, Jackson P, Lim W, Lovrics P, Mazzadi S, Orovan W, Rudkowski J, Soth M, Tiboni M, Acedillo R, Garg A, Hildebrand A, Lam N, Macneil D, Mrkobrada M, Roshanov PS, Srinathan SK, Ramsey C, John PS, Thorlacius L, Siddiqui FS, Grocott HP, McKay A, Lee TW, Amadeo R, Funk D, McDonald H, Zacharias J, Villar JC, Cortés OL, Chaparro MS, Vásquez S, Castañeda A, Ferreira S, Coriat P, Monneret D, Goarin JP, Esteve CI, Royer C, Daas G, Chan MT, Choi GY, Gin T, Lit LC, Xavier D, Sigamani A, Faruqui A, Dhanpal R, Almeida S, Cherian J, Furruqh S, Abraham V, Afzal L, George P, Mala S, Schünemann H, Muti P, Vizza E, Wang CY, Ong GS, Mansor M, Tan AS, Shariffuddin II, Vasanthan V, Hashim NH, Undok AW, Ki U, Lai HY, Ahmad WA, Razack AH, Malaga G, Valderrama-Victoria V, Loza-Herrera JD, De Los Angeles Lazo M, Rotta-Rotta A, Szczeklik W, Sokolowska B, Musial J, Gorka J, Iwaszczuk P, Kozka M, Chwala M, Raczek M, Mrowiecki T, Kaczmarek B, Biccard B, Cassimjee H, Gopalan D, Kisten T, Mugabi A, Naidoo P, Naidoo R, Rodseth R, Skinner D, Torborg A, Paniagua P, Urrutia G, Maestre ML, Santaló M, Gonzalez R, Font A, Martínez C, Pelaez X, De Antonio M, Villamor JM, García JA, Ferré MJ, Popova E, Alonso-Coello P, Garutti I, Cruz P, Fernández C, Palencia M, Díaz S, Del Castillo T, Varela A, de Miguel A, Muñoz M, Piñeiro P, Cusati G, Del Barrio M, Membrillo MJ, Orozco D, Reyes F, Sapsford RJ, Barth J, Scott J, Hall A, Howell S, Lobley M, Woods J, Howard S, Fletcher J, Dewhirst N, Williams C, Rushton A, Welters I, Leuwer M, Pearse R, Ackland G, Khan A, Niebrzegowska E, Benton S, Wragg A, Archbold A, Smith A, McAlees E, Ramballi C, Macdonald N, Januszewska M, Stephens R, Reyes A, Paredes LG, Sultan P, Cain D, Whittle J, Del Arroyo AG, Sessler DI, Kurz A, Sun Z, Finnegan PS, Egan C, Honar H, Shahinyan A, Panjasawatwong K, Fu AY, Wang S, Reineks E, Nagele P, Blood J, Kalin M, Gibson D, Wildes T; Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Writing Group, on behalf of The Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Investigators; Appendix 1. The Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Study Investigators Writing Group; Appendix 2. The Vascular events In noncardiac Surgery patIents cOhort evaluatioN Operations Committee; Vascular events In noncardiac Surgery patIents cOhort evaluatioN VISION Study Investigators. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014;120:564-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 529] [Cited by in RCA: 653] [Article Influence: 59.4] [Reference Citation Analysis (0)] |
| 16. | Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) Study Investigators, Devereaux PJ, Chan MT, Alonso-Coello P, Walsh M, Berwanger O, Villar JC, Wang CY, Garutti RI, Jacka MJ, Sigamani A, Srinathan S, Biccard BM, Chow CK, Abraham V, Tiboni M, Pettit S, Szczeklik W, Lurati Buse G, Botto F, Guyatt G, Heels-Ansdell D, Sessler DI, Thorlund K, Garg AX, Mrkobrada M, Thomas S, Rodseth RN, Pearse RM, Thabane L, McQueen MJ, VanHelder T, Bhandari M, Bosch J, Kurz A, Polanczyk C, Malaga G, Nagele P, Le Manach Y, Leuwer M, Yusuf S. Association between postoperative troponin levels and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2012;307:2295-2304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 660] [Cited by in RCA: 745] [Article Influence: 57.3] [Reference Citation Analysis (0)] |
| 17. | Coss E, Watt KD, Pedersen R, Dierkhising R, Heimbach JK, Charlton MR. Predictors of cardiovascular events after liver transplantation: a role for pretransplant serum troponin levels. Liver Transpl. 2011;17:23-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71-86. [PubMed] |
| 19. | Mills EJ, Rachlis B, Wu P, Devereaux PJ, Arora P, Perri D. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. J Am Coll Cardiol. 2008;52:1769-1781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 395] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 20. | Devereaux PJ, Xavier D, Pogue J, Guyatt G, Sigamani A, Garutti I, Leslie K, Rao-Melacini P, Chrolavicius S, Yang H, Macdonald C, Avezum A, Lanthier L, Hu W, Yusuf S; POISE (PeriOperative ISchemic Evaluation) Investigators. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med. 2011;154:523-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 461] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 21. | Schreen D, Caramelli B. [Hemodynamic instability in liver transplant: a challenge for the intensivist]. Rev Assoc Med Bras (1992). 2006;52:113-117. [PubMed] |
| 22. | Tandon M, Singh A, Saluja V, Dubey G, Pandey VK, Pandey CK, Karna ST, Singh SA. Post-operative hypertension, a surrogate marker of the graft function and predictor of survival in living donor liver transplant recipients: A retrospective study. Indian J Anaesth. 2016;60:463-469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Auzinger G, Willars C, Loveridge R, Vercueil A, Best T, Wendon J. Extracorporeal membrane oxygenation before and after adult liver transplantation: worth the effort? Crit Care. 2014;18:P203. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Moguilevitch M, Rufino M, Leff J, Delphin E. Novel approach for heart failure treatment after liver transplantation. Liver Transpl. 2015;21:1103-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |