Published online May 8, 2017. doi: 10.4254/wjh.v9.i13.642
Peer-review started: November 10, 2016
First decision: December 20, 2016
Revised: March 27, 2017
Accepted: April 18, 2017
Article in press: April 20, 2017
Published online: May 8, 2017
Processing time: 179 Days and 12.8 Hours
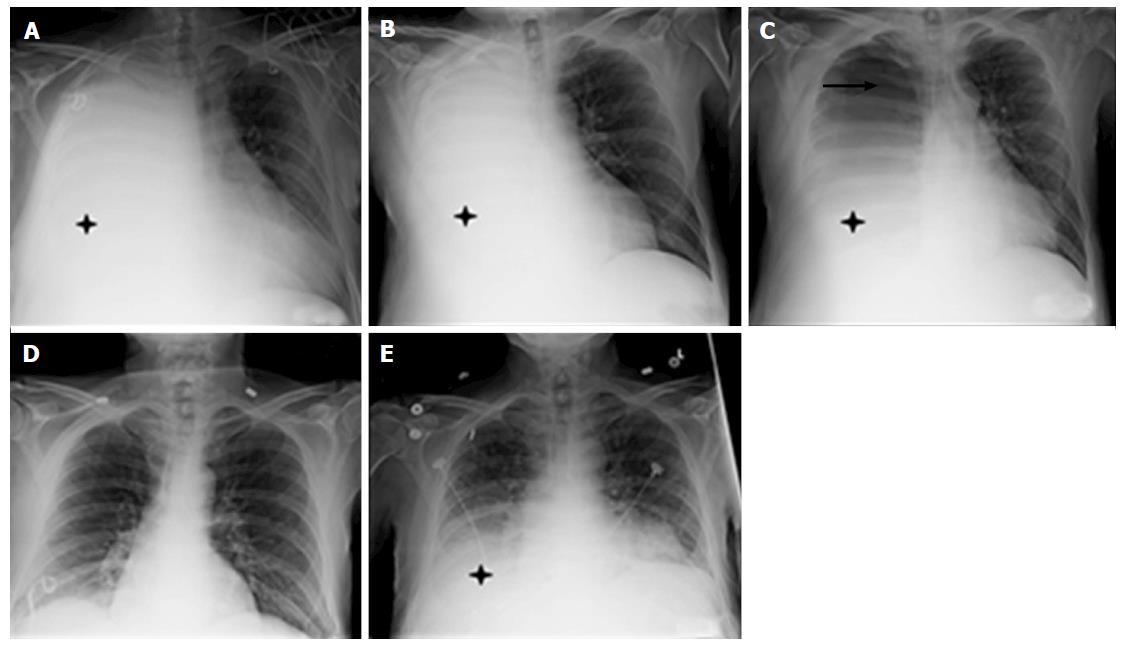
A 59-year-old male with alcoholic cirrhosis presented to our hospital with an acutely painful umbilical hernia, and 4 mo of exertional dyspnea. He was noted to be tachypneic and hypoxic. He had a massive right sided pleural effusion with leftward mediastinal shift and gross ascites, with a tense, fluid-filled, umbilical hernia. Emergent paracentesis with drain placement and a large volume thoracentesis were performed. Despite improvement in dyspnea and drainage of 15 L of ascitic fluid, the massive transudative pleural effusion remained largely unchanged. He underwent a repeat large volume thoracentesis on hospital day 4. The patient subsequently developed a tension pneumothorax, which resulted in a dramatic reduction in the effusion. A chest tube was placed and serial radiographs demonstrated resolution of the pneumothorax but recurrence of the effusion. The radiographs illustrate the movement of fluid between the peritoneal and pleural cavities. In this case, the mechanism of pleural effusion was confirmed to be a hepatic hydrothorax via an unintended tension pneumothorax. Methods to elucidate a hepatic hydrothorax include Tc99m or indocyanine green injection into the ascitic fluid followed by its demonstration above the diaphragm. The unintended tension pneumothorax in this case additionally demonstrates bi-directional flow across the diaphragm.
Core tip: Hepatic hydrothorax is usually a clinical diagnosis in patients with cirrhosis and portal hypertension who present with a transudative pleural effusion. The authors herein report an interesting case of radiological confirmation of hepatic hydrothorax through a series of chest radiographs that depict the movement of ascitic fluid between the pleural and peritoneal cavities due to a iatrogenic pneumothorax.
- Citation: Nellaiyappan M, Kapetanos A. Bi-directional hepatic hydrothorax. World J Hepatol 2017; 9(13): 642-644
- URL: https://www.wjgnet.com/1948-5182/full/v9/i13/642.htm
- DOI: https://dx.doi.org/10.4254/wjh.v9.i13.642
We read with great interest the article titled “A fascinating presentation of hepatic hydrothorax” by Gaduputi et al[1]. We would like to thank the authors for sharing the clinical images and case details which illustrate the rapid shifts in the hydrothorax in a patient who was on invasive positive pressure ventilatory support. We would like to report an interesting case of hepatic hydrothorax that we encountered in our clinical practice which also demonstrates the mechanics of hepatic hydrothorax. We believe that the images of this common, yet incompletely understood phenomenon will be of interest to your readers at large.
The patient was a 59-year-old male with Child C cirrhosis in the setting of alcohol abuse and chronic hepatitis C who presented to our hospital with an acutely painful umbilical hernia, and 4 mo of exertional dyspnea. He was noted to be tachypneic and hypoxic. He had a massive right sided pleural effusion with leftward mediastinal shift (Figure 1A, day 0, asterisk) and gross ascites with a tense, fluid-filled, umbilical hernia. Emergent paracentesis with drain placement and a large volume thoracentesis were performed. Despite improvement in dyspnea and 15 L of ascitic fluid drainage, the massive transudative effusion remained largely unchanged (Figure 1B, day 3, asterisk). He underwent a repeat large volume thoracentesis on hospital day 4. The patient subsequently developed a tension pneumothorax, with a dramatic reduction in effusion size (Figure 1C, day 4, asterisk, arrow). A chest tube was placed, after which serial radiographs demonstrated resolution of the pneumothorax and recurrence of the effusion (Figure 1D). The radiographs demonstrate the movement of fluid between the peritoneal and pleural cavities (Figure 1C and E). In this case, the mechanism of pleural effusion was confirmed to be a hepatic hydrothorax via an unintended tension pneumothorax.
The diagnosis of hepatic hydrothorax should be considered for any patient with unilateral pleural effusion without an obvious cardio pulmonary cause. For cases in which the diagnosis is not obvious based on the clinical picture, methods to elucidate a hepatic hydrothorax include Tc99m labelled sulfur/albumin or indocyanine green injection into the ascitic fluid, followed by its demonstration above the diaphragm[2,3].
The unintended tension pneumothorax in this case also demonstrates bi-directional flow across the diaphragm. As mentioned by Gaduputi et al[1], fluid dynamics in hepatic hydrothorax are driven by pressure changes and pressure differences between the pleural, peritoneal cavities. In their patient, mechanical ventilation imparted positive pressure that was transmitted to the intrapleural space thereby causing the hydrothorax to track back to the peritoneal cavity which was relatively less pressurized[1]. Similarly, in our patient, a tension pneumothorax imparted positive pressure in the pleural cavity, forcing pleural fluid back into the peritoneal cavity. In both patients, after the source of positive intrapleural pressure was eliminated, the hydrothorax recurred, highlighting bi-directional flow.
While rapid, bi-directional, hepatic hydrothoraces may represent a subset of larger diaphragmatic defects, this phenomenon may be more common than judged by the scant available literature. It is in these cases that an opportunity exists to better delineate the pathophysiology of hepatic hydrothoraces, and begin to conceive more robust therapeutic options than those currently available to patients. As it stands, hepatic hydrothorax is often a harbinger of further suffering.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Han AG, Sipos F, Wong GLH S- Editor: Kong JX L- Editor: A E- Editor: Li D
| 1. | Gaduputi V, Tariq H, Kanneganti K. A fascinating presentation of hepatic hydrothorax. World J Hepatol. 2013;5:589-591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Umino J, Tanaka E, Ichijoh T, Muraki T, Orii K, Yoshizawa K, Kiyosawa K. Hepatic hydrothorax in the absence of ascites diagnosed by intraperitoneal spraying of indocyanine green. Intern Med. 2004;43:283-288. [PubMed] |
| 3. | Bhattacharya A, Mittal BR, Biswas T, Dhiman RK, Singh B, Jindal SK, Chawla Y. Radioisotope scintigraphy in the diagnosis of hepatic hydrothorax. J Gastroenterol Hepatol. 2001;16:317-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |