Published online Feb 28, 2016. doi: 10.4254/wjh.v8.i6.307
Peer-review started: August 21, 2015
First decision: October 13, 2015
Revised: January 11, 2016
Accepted: January 27, 2016
Article in press: January 29, 2016
Published online: February 28, 2016
Processing time: 188 Days and 12.2 Hours
Bacterial infection is common and accounts for major morbidity and mortality in cirrhosis. Patients with cirrhosis are immunocompromised and increased susceptibility to develop spontaneous bacterial infections, hospital-acquired infections, and a variety of infections from uncommon pathogens. Once infection develops, the excessive response of pro-inflammatory cytokines on a pre-existing hemodynamic dysfunction in cirrhosis further predispose the development of serious complications such as shock, acute-on-chronic liver failure, renal failure, and death. Spontaneous bacterial peritonitis and bacteremia are common in patients with advanced cirrhosis, and are important prognostic landmarks in the natural history of cirrhosis. Notably, the incidence of infections from resistant bacteria has increased significantly in healthcare-associated settings. Serum biomarkers such as procalcitonin may help to improve the diagnosis of bacterial infection. Preventive measures (e.g., avoidance, antibiotic prophylaxis, and vaccination), early recognition, and proper management are required in order to minimize morbidity and mortality of infections in cirrhosis.
Core tip: Bacterial infection is common and accounts for major morbidity and mortality in cirrhosis. Patients with cirrhosis are immunocompromised and increased susceptibility to develop spontaneous bacterial infections, hospital-acquired infections, and a variety of infections from uncommon pathogens. Once infection develops, the excessive response of pro-inflammatory cytokines on a pre-existing hemodynamic derangement in cirrhosis further predispose the development of serious complications such as shock, acute-on-chronic liver failure, renal failure, and death. The incidence of resistant bacteria has continually increased, especially in healthcare-associated settings. Preventive measures, early recognition and proper management are necessary to minimize morbidity and mortality of infections in cirrhosis.
- Citation: Bunchorntavakul C, Chamroonkul N, Chavalitdhamrong D. Bacterial infections in cirrhosis: A critical review and practical guidance. World J Hepatol 2016; 8(6): 307-321
- URL: https://www.wjgnet.com/1948-5182/full/v8/i6/307.htm
- DOI: https://dx.doi.org/10.4254/wjh.v8.i6.307
In the past decades, there have been several improvements in the management of cirrhotic patients, such as antiviral therapy and management of portal hypertension and liver transplantation (LT). However, the mortality of infection in cirrhosis is still high and has not changed substantially. Cirrhosis is an immunocompromised state that predisposes patients to spontaneous bacterial infections, hospital-acquired infections, and a variety of infections from uncommon pathogens. Once infection develops, the excessive response of pro-inflammatory cytokines on a pre-existing hemodynamic derangement in cirrhosis further facilitate the development of severe complications such as septic shock, acute-on-chronic liver failure (ACLF), multiple organ failure, and death. Accordingly, bacterial infection in patients with cirrhosis is very common in clinical practice and sepsis is the main reason of intensive care unit admission and death among such patients. The incidence of resistant bacteria has been increasing, especially in healthcare-associated settings. Preventive measures, early recognition, and proper management are necessary to minimize morbidity and mortality of infections in cirrhosis.
Patients with cirrhosis are in a state of immune dysfunction, in parallel with a state of excessive activation of pro-inflammatory cytokines, referred to as cirrhosis-associated immune dysfunction syndrome, which predisposes the patient for infections[1,2]. Portosystemic shunting allows less gut-derived bacteria and their products to be cleared from portal circulation by the liver, which contains about 90% of the reticuloendothelial cells in the body[1-5]. Nearly all components of systemic immune response are significantly impaired in cirrhosis, including a decrease in phagocytic activity, a reduction in serum albumin, complement and protein C activities, and an impaired opsonic activity both in serum and ascitic fluid[1-4,6-10]. Genetic polymorphisms of toll-like receptor (TLR) and nucleotide-binding oligomerisation domain 2 (NOD2) genes could be responsible for bacterial translocation (BT) and increase infection risk in cirrhosis by altering the TLR’s ability to bind to lipopolysaccharide or endotoxins[11,12]. Further, cirrhosis-associated immune dysfunction may further complicate by additional factors such as malnourishment[13] and alcohol drinking[14] (Table 1).
| Natural barriers | Fragile, thin and/or edematous skin |
| Alteration of GI motility and mucosal permeability | |
| Alteration of GI bacterial flora, bacterial overgrowth | |
| ↑ GI mucosal ulcerations | |
| Hepatic RES activity | Portosystemic shunting |
| Kupffer cells - ↓ number, impaired function | |
| Cellular defense mechanisms | RES - ↓ activation, ↓ chemotaxis, ↓ phagocytosis, ↓ production of pro-inflammatory cytokines (IL-1, IL-6, IL-18, TNF-α) |
| PMN - ↓ lifespan, ↓ intracellular killing activity, ↓ phagocytosis, ↓ chemotaxis | |
| Serum factors | ↓ Complement levels (C3, C4, CH50) |
| ↓ Opsonic activity | |
| ↓ Protein C activity | |
| Iatrogenic and treatment-related factors | ↑ Invasive procedure and catheters |
| Frequent hospitalization | |
| Immunosuppressive agents (autoimmune hepatitis, post-transplantation) | |
| Interferon therapy (viral hepatitis) | |
| Proton pump inhibitors | |
| Other compelling factors | Malnutrition |
| Alcohol drinking |
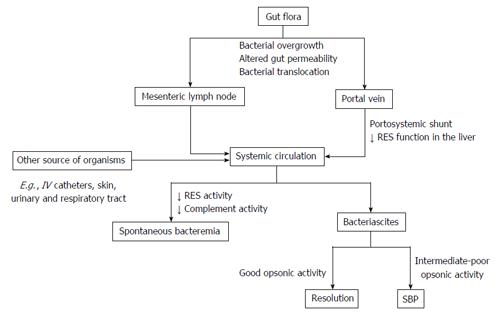
BT is the migration of viable native bacteria from gut lumen through systemic circulation via mesenteric lymph nodes (MLN) and portal vein. Although this can be a healthy phenomenon, BT has increased pathologically compromising effects in cirrhosis[15-17]. The diagnosis of BT relies on the isolation of viable bacteria in MLN, while the detection of bacterial DNA in serum or ascitic fluid is proposed as a useful surrogated marker[15-18]. It has been shown that oral administration of radio-labeled Escherichia coli (E. coli) to cirrhotic rats revealed the detection of these bacteria not only in the gut lumen but also in the MLN and ascites[19]. Several experimental and clinical studies have suggested that small intestinal overgrowth, increased intestinal permeability, impaired intestinal motility, lack of bile acids, sympathetic overactivity, and local innate and adaptive immunological alterations (e.g., impaired leukocyte recruitment, altered T-cell activation, TLR and NOD2 mutation) are important factors involved in the pathogenesis of BT[11,12,17,20,21].
BT is pathogenetically linked to the development of infections, particularly spontaneous bacterial infections, and other serious complications in cirrhosis[15-17]. Apart from infections, bacterial DNA and bacterial products, such as endotoxin, can translocate to extra-intestinal sites and promote host immunological and hemodynamic responses, which is associated with the development of systemic pro-inflammatory and hyperdynamic circulatory state in cirrhosis[16,18]. The pathological translocation of viable bacteria occurs in the decompensated stage, while the rate and degree of translocating bacterial products also increases in the earlier stages of cirrhosis[15]. Notably, treatment with non-selective beta-blockers has been shown to ameliorate intestinal permeability and reduce BT[22].
Patients with cirrhosis are susceptible to the development of severe infection, septic shock, and organ failure[1,2,23]. In cirrhosis, bacterial infection is associated with a dysregulated cytokine response, which transforms helpful responses against infections into excessive, damaging inflammation[1,2,23]. Nitric oxide is strikingly released in cirrhotic patients with sepsis and is a key driver of circulation dysfunction in this setting[23,24]. A pre-existing hyperdynamic circulatory state in patients with advanced cirrhosis predisposes detrimental complications from a sepsis-induced nitric oxide and cytokine storm which subsequently leads to intractable hypotension, insufficient tissue perfusion, multiple organ failure and death[1-3,23].
Bacterial infection accounts for about 30%-50% death in patients with cirrhosis[3,24,25]. Infections present in 32%-34% of hospitalized patients with cirrhosis, which is 4-5 folds higher than hospitalized patients in general, and is especially higher in those with gastrointestinal bleeding (45%-60%)[26-28].
Common types of infections in patients with cirrhosis include spontaneous bacterial peritonitis (SBP) (25%-31%), urinary tract infection (UTI) (20%-25%), pneumonia (15%-21%), bacteremia (12%), and soft tissue infection (11%)[2,27,29]. The major causative organisms are gram-negative bacteria, e.g., E. coli, Klebsiella spp. and Enterobacter spp., whereas gram positive bacteria, especially Enterococci and staphylococcus aureus, comprise about 20% and anaerobes only 3%[2]. Risk factors of infection by gram positive bacteria are recent or current hospitalization, receiving quinolones prophylaxis, and invasive procedures[27,28,30].
Healthcare-associated is defined as infections diagnosed within 48 h of hospital admission in patients with any prior 90-d healthcare contact and nosocomial is defined as infections diagnosed after 48 h of admission. These infections are increasingly common in cirrhosis, frequently resistant to antibiotics (up to 64%) and are associated with bad outcomes[30]. In a large prospective study of cirrhotic patients with infections (> 650 infectious episodes)[31], multi-resistant bacteria (18%) were isolated in 4%, 14%, and 35% of community-acquired, healthcare-associated, and nosocomial infections, respectively (P < 0.001). The main resistant organism was extended-spectrum β-lactamase (ESBL)-producing Enterobacteriaceae, followed by Pseudomonas aeruginosa, methicillin-resistant Staphylococcus aureus (MRSA), and Enterococcus faecium[31]. There was a significantly higher incidence of septic shock and death from infections caused by resistant bacteria. Notably, the efficacy of empirical antibiotic treatment was decreased in nosocomial infections (40%), compared to community-acquired and healthcare-associated episodes (83% and 73%, respectively; P < 0.0001), especially in SBP, UTI, and pneumonia (26%, 29% and 44%, respectively)[31]. Due to an increasingly use of broad spectrum antibiotics (ATB), it is speculated that infections with multi-resistant gram-negative organisms and Enterococci will be largely more common and more problematic in the near future.
The common types of infections in cirrhosis and suggested empiric therapy are summarized in Table 2[32]. In addition, the common clinical features and risk factors of less common pathogens are summarized in Table 3[2]. It should be noted that the data regarding these less common pathogens derived from case reports and series from various regions of the world, in which the patterns of infection and ATB usage varies among reports. In real-life practice, empirical ATB should be selected based upon types of infection, individual risk factors, and the local epidemiological pattern of resistant bacteria, then narrow-downed according to the culture and ATB susceptibility testing.
| Types of infection | Common responsible bacteria | Suggested empirical antibiotic |
| SBP, spontaneous bacteremia, SBE | Enterobacteriaceae | 1st line: Cefotaxime or ceftriaxone or BL-BI IV |
| S. pneumoniae | Options: Ciprofloxacin PO for uncomplicated SBP1; carbapenems IV for nosocomial | |
| S. viridans | infections in areas with a high prevalence of ESBL | |
| BL-BI may prefer in those with suspicious for enterococcal infection2 | ||
| Pneumonia | Enterococci | Community-acquired: ceftriaxone or BL-BI IV + macrolide or levofloxacin IV/PO |
| S. pneumoniae | Nosocomial and health care-associated infections: Meropenem or cetazidime IV + | |
| H. infuenzae | ciprofloxacin IV (IV vancomycin or linezolid should be added in patients with risk | |
| M. pneumoniae | factors for MRSA3) | |
| Legionella spp. | ||
| Enterobacteriaceae | ||
| P. aeruginosa | ||
| S. aureus | ||
| Urinary tract infection | Enterobacteriaceae | 1st line: Ceftriaxone or BL-BI IV in patients with sepsis. Ciprofloxacin or |
| E. faecalis | cotrimoxazole PO in uncomplicated infections | |
| E. faecium | Options: In areas with a high prevalence of ESBL, IV carbapenems for nosocomial infections and sepsis (+ IV glycopeptides for severe sepsis); and nitrofurantoin PO for uncomplicated cases | |
| Skin and soft tissue infections | S. aureus | Community-acquired: Ceftriaxone + cloxacillin IV or BL-BI IV |
| S. pyogenes | Nosocomial: Meropenem or cetazidime IV + glycopeptides IV | |
| Enterobacteriaceae | ||
| P. aeruginosa | ||
| Vibrio vulnificus | ||
| Aeromonas spp. | ||
| Meningitis | S. pneumoniae | Community-acquired: Cefotaxime or ceftriaxone IV + vancomycin IV |
| Enterobacteriaceae | Ampicillin IV should be added if L. monocytogenes is suspected4 | |
| L. monocytogenes | Nosocomial: Meropenem + vancomycin IV | |
| N. meningitidis |
| Pathogens | Common clinical syndrome | Risk factors | Remarks |
| Aeromonas spp. (A. hydrophila, A. sobria, A. aquariorum)[120-126] | SBP, bacteremia, SSTI, enterocolitis | Contaminated food and water | Increased incidence |
| Diabetes | High mortality (20%-60%), especially when | ||
| Most reports were from East Asia | presence of hypotension on admission | ||
| Campylobacter spp.[127,128] | Bacteremia, SBP | Alcoholic | Increased incidence |
| High mortality (10% in bacteremia) | |||
| Clostridium spp. (C. perfringens, C. bifermentans, C. septicum)[4,129,130] | SSTI | Diabetes | Increased incidence |
| Very high mortality (54%-65%) | |||
| Clostridium difficile[108,131-133] | ATB-associated diarrhea and colitis | Broad-spectrum ATB | Increased incidence |
| Hospitalization | Higher mortality (14%) when compare to non-cirrhotics | ||
| PPIs | Increased cost and length of hospital stay | ||
| Enterococcus spp. (E. faecium, E. faecalis, E. galinarum)[134-136] | SBP, bacteremia, UTI, endocarditis, biliary tract infection | Healthcare-associated infection | Increased incidence |
| Quinolone prophylaxis | High mortality (30% in bacteremia; 60% in SBP) | ||
| Increased incidence of VRE colonization and infection in liver transplant setting | |||
| Listeria monocytogenes[137,138] | SBP, bacteremia, meningitis | Hemochromatosis | Increased incidence |
| Mycobacterium TB[2,139,140] | Pulmonary TB, TB peritonitis, TB lymphadenitis, disseminated TB | Alcoholic | Increased incidence, especially extrapulmonary forms (> |
| Developing countries | 50% of TB peritonitis cases in the United States had | ||
| Exposed to TB case | underlying cirrhosis) | ||
| High mortality (22%-48%) | |||
| Increased risk for multi-drug resistant TB | |||
| Increased risk for anti-TB-induced hepatotoxicity | |||
| Pasteurella multocida[141-143] | SBP, bacteremia septic arthritis, meningitis | Presence of ascites (TB peritonitis) | Increased incidence |
| Domestic animal (cats or dogs) bites or scratches | High mortality (10%-40% in bacteremia) | ||
| Staphylococcus aureus[45,144,145] | SSTI, UTI, SBP, bacteremia, endocarditis | Alcoholic | Increased incidence of MRSA carriage and infection |
| Invasive procedures | High mortality (30% in bacteremia) | ||
| Hospitalization | Removal of the eradicable focus was associated with | ||
| decreased mortality | |||
| Streptococcus bovis[146,147] | Bacteremia, SBP meningitis, endocarditis, septic arthritis | Quinolone prophylaxis | Increased incidence |
| Colonic lesion(s): Adenoma or | High mortality (up to 40% in bacteremia with | ||
| adenocarcinoma (presence in | advanced cirrhosis) | ||
| 18%-40% of cases) | Colonic lesion(s) was present in 18%-40% of cases | ||
| Alcoholic | |||
| Streptococcus group B[148-150] | SSTI, bacteremia, SBP, meningitis, pneumonia | Post endoscopic sclerotherapy and banding ligation | Increased incidence |
| High mortality (10%-25% in SBP and bacteremia; | |||
| 45% in meningitis) | |||
| Streptococcus pneumoniae[89-92] | Pneumonia, SBP bacteremia, SSTI, meningitis | Alcoholic | Increased incidence of invasive pneumococcal disease |
| Post-splenectomy | High mortality (10%-20%) | ||
| Not vaccinated | |||
| Vibrio spp. (V. vulnificus, non-o1 V. cholera, V. parahemolyticus)[151-153] | SSTI, bacteremia, gastroenteritis, diarrhea, SBP | Hemochromatosis | Increased incidence |
| Exposed to seawater and undercooked seafoods | Very high mortality (50%-60% in bacteremia; 24% in SSTI) | ||
| Most reports were from East Asia | |||
| Yersinia spp. (Y. enterocolitica, Y. pseudotuberculosis)[154,155] | Bacteremia, SBP, hepatosplenic abscesses | Hemochromatosis | Increased incidence (in hemochromatosis) |
| Exposed to animals and | High mortality (50% in bacteremia) | ||
| contaminated foods |
It is crucial, but often difficult to make an early diagnosis of bacterial infections in cirrhosis due to non-specific manifestations, which are indistinguishable from other non-infectious causes of systemic inflammatory response syndrome (SIRS) and the symptoms of liver deterioration. Therefore, serum biomarkers that are sensitive, reliable and inexpensive are being pursued in order to improve the diagnosis of bacterial infection in the setting of cirrhosis. General inflammatory markers, such as C-reactive protein (CRP, synthesized by the liver), ferritin (synthesized by the liver) or white blood cells (WBC), lack specificity for bacterial infections. Procalcitonin (PCT) is potentially a more specific marker for bacterial infection. PCT is produced by nearly all tissues in response to endotoxin or mediators released in response to bacterial infections [interleukin (IL)-1b, tumor necrosis factor-alfa, and IL-6]. It highly correlates with the severity of bacterial infections and may be helpful to distinguish bacterial infections from viral infection or other non-infectious causes[33].
In the meta-analysis included 10 diagnostic studies (1144 cirrhotic patients and 435 bacterial infection episodes), PCT displayed an area under the curve of 0.92, a sensitivity of 0.79, and a specificity of 0.89 in diagnosing bacterial infection[34]. The pooled sensitivity estimates were 79% for PCT and 77% for CRP tests, whereas the pooled specificity were higher for both PCT (89%) and CRP tests (85%)[34]. The results were consistent when stratified to patients with SBP or patients with systemic infection. The authors suggested that the PCT test can be used as a rule-in diagnostic tool (positive likelihood ratio 7.38), CRP test can be used as a rule-out diagnostic tool (negative likelihood ratio 0.23) in patients without signs of infection[34]. However, the diagnostic accuracy of CRP in the detection of bacterial infections decreased in setting of advanced liver disease. The combination of CRP and PCT may slightly improve the diagnostic accuracy of bacterial infection[35].
SBP is common and quite unique in patients with cirrhosis. The prevalence of SBP in cirrhotic patients with ascites admitted to the hospital ranges from 10%-30%; about 50% of cases are present at the time of hospitalization and 50% develop during the hospitalization[1,29,36]. BT, systemic, and local immune dysfunction, particularly a decreased opsonic activity in ascitic fluid, are the main elements in the pathogenesis of SBP[1,15,17,37] (Figure 1). Accordingly, gut microflora including E. coli, Klebsiella spp., Enterobacter spp., Enterococci, and Streptococci are common causative organisms[1,15,17,37]. The classical symptoms of SBP include fever, abdominal pain, and worsening of pre-existing ascites, although these symptoms may be absent in up to one-third of cases[38]. Therefore, diagnostic paracentesis is recommended to perform in all cirrhotic patients with ascites at the time of admission and/or in case of gastrointestinal (GI) bleeding, shock, signs of inflammation, hepatic encephalopathy, worsening of liver or renal function[37,39-41]. The hospital mortality for SBP ranges from 10%-50% depending on various factors[37]. Predictors for poor prognosis in SBP include older age, higher Child-Pugh scores, nosocomial origin, encephalopathy, elevated serum creatinine and bilirubin, ascites culture positivity, presence of bacteremia, and infections with resistant organisms[42-45]. Notably, the modifiable factors to reduce morbidity and mortality in SBP include prompt diagnosis, proper first-line ATB treatment and prevention of subsequent renal failure[37]. SBP is one of the important prognostic landmark in the natural course of cirrhosis as the overall one-year mortality rate after a first episode of SBP are 30%-93% regardless of its recurrence[37,46,47].
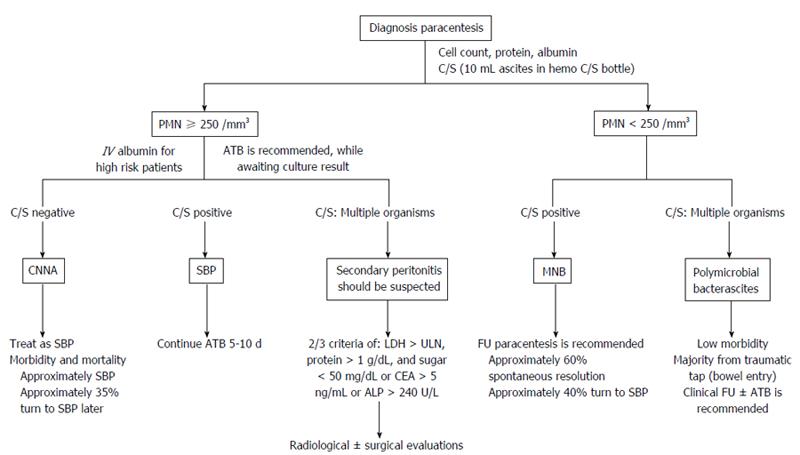
The diagnosis of SBP is relied on the cell count of the ascitic fluid, determined either by microscope or appropriate automated cell counters, and bacterial culture[40,41,48]. Ascitic fluid culture is important and should be performed before initiating ATB therapy by bedside inoculation of ascites ≥ 10 mL into blood culture bottles[49]. Reagent strips to assess leucocyte esterase activity of activated polymorphonuclear cells (PMN) are not recommended for rapid diagnosis of SBP due to unacceptable false-negative rates[50]. To date, most of reagent strips (LERS) that had been evaluated were developed for UTI with a threshold of > 50 PMN/mm3[37]. More recently, ascites-calibrated reagent strips (cut-off of > 250 PMN/mm3) have been introduced for SBP with promising preliminarily results[51]. Based on available evidences, LERS seem to have low sensitivity for SBP, but have reliably given a high negative predictive value (> 95% in most studies), which supports the potential role of LERS as a screening tool for SBP[52]. In addition, neutrophil gelatinase-associated lipocalin (NGAL), a protein involved in iron metabolism and links to the inflammation, and bacterial DNA in ascitic fluid have the potential to improve the diagnosis of SBP. The pivot study of using NGAL to differentiate bacterial peritonitis (30% were SBP) from nonbacterial peritonitis reported that AUC were 0.89 for NGAL and 0.94 for combination of NGAL and lactate dehydrogenase[53]. Detection of bacterial DNA by real-time polymerase chain reaction and sequencing of 16S rDNA gene demonstrated poor results with negative results in almost half the culture-negative SBP episodes[54]. In contrast, another study using newly in situ hybridization method to detect global bacterial DNA demonstrated high sensitivity (91%) and specificity (100%) for detecting phagocytized bacterial DNA in the WBC of SBP ascites, with all test results obtained within one day[55].
Empirical ATB should be given promptly to all cirrhotic patients with ascites PMN counts > 250 cells/mm3 in clinical settings that suggestive for ascitic fluid infection (culture results are often unavailable at this time)[40,41] (Figure 2). The choice of empirical ATB should be based on the origin of infection, individual risk factors for resistant organism and local microbial epidemiology. In general, the suggested initial treatments of community-acquired SBP are third-generation cephalosporins (mostly preferred), amoxicillin-clavulanate or quinolones (Table 2). These empirical ATB should be given intravenously for a duration of 5-10 d[40,41]. In countries with low rate of quinolone-resistant Enterobacteriaceae, oral quinolones may be used for uncomplicated SBP, as defined by cases without shock, ileus, GI bleeding, hepatic encephalopathy (≥ grade II) or renal impairment (creatinine > 3 mg/dL)[56]. In nosocomial SBP, use of the antibiotics recommended above can be associated with unacceptable failure rates because resistance to third-generation cephalosporins (23%-44%) and quinolones (38%-50%) are increasingly reported[37,57,58].
Notably, the incidence of SBP causing by with gram-positive and resistant bacteria (mainly ESBL-producing bacteria and multi-resistant gram-positive bacteria such as Enterococci or MRSA) has been increasingly reported in the healthcare associated and especially in nosocomial settings[37,57]. In patients with typical presentation and clinical improvement after ATB, a repeat of paracentesis is not necessary to assess for resolution of SBP[1,37,40,41]. However, in cases with questionable diagnosis or in those who did not satisfactorily improve with ATB, repeated paracentesis should be performed to document the response of treatment[37,40]. If the PMN count does not reduce by at least 25% after 2 d of ATB, changing treatment and/or reevaluation for other possible cause(s) of symptoms should be considered[37,59].
Renal impairment develops in 30%-40% of SBP cases and is a strong predictor of death during hospitalization[39,40,60]. The use of intravenous albumin (1.5 g/kg within 6 h of SBP diagnosis followed by 1 g/kg on day 3) in conjunction with intravenous (IV) antibiotic was found to reduce the incidence of renal impairment from 33% to 10% and mortality from 29% to 10%[61]. Notably, albumin infusion was particularly effective in patients with baseline serum creatinine ≥ 1 mg/dL, blood urea nitrogen ≥ 30 mg/dL or bilirubin ≥ 4 mg/dL[39,61]. Unfortunately, albumin infusion in high-risk SBP has been underutilized, even in the United States, with > 50% of cases did not follow the guidelines[62]. It is unclear whether crystalloids or artificial colloids could replace albumin in this setting[39-41,63].
After recovering from SBP, the rate of recurrence is around 43% at 6 mo and 69% at 1 year[46]. Therefore, secondary prophylaxis of SBP should be given indefinitely or until LT[37,40,61,64]. Intermittent dosing of prophylactic ATB may select resistant flora, thus daily dosing is preferred[37,40] (Table 4).
| Avoidance | |
| Raw/uncooked foods, especially seafood | |
| Close contact to at-risk animals or sick people | |
| Wound exposure to flood or seawater | |
| Vaccination[87] | |
| Influenza | Recommended yearly for all patients with chronic liver disease |
| Pneumococcal (polysaccharide) | Recommended for all cirrhotic patient |
| Booster dose after 3-5 yr | |
| Hepatitis A | Recommended for all non-immune, cirrhotic patient, 2 injections 6-12 mo apart |
| Anti-HAV should be checked 1-2 mo after the second dose | |
| Hepatitis B | Recommended for all cirrhotic patient without serological markers of HBV (e.g., negative HBsAg, anti-HBs, and anti-HBc antibodies) |
| 3 injections (at month 0, 1 and 6) | |
| Anti-HBs should be checked 1-2 mo after the last dose | |
| Patients with advanced cirrhosis should receive 1 dose of 40 μg/mL (Recombivax HB) administered on a 3-dose schedule or 2 doses of 20 μg/mL (Engerix-B) administered simultaneously on a 4-dose schedule at 0, 1, 2 and 6 mo | |
| Other vaccines, e.g., Td, Tdap, MMR, varicella | Recommendations are as same as general adult population |
| Prophylactic antibiotics | |
| Secondary prophylaxis for SBP[32,41] | Recommended for all cirrhotic patients who recovered from SBP |
| Norfloxacin 400 mg PO daily | |
| Alternatives: TMP/SMX 1 double-strength tablet or ciprofloxacin 500 mg PO daily | |
| Primary prophylaxis in GI bleeding[32,41] | Recommended for all cirrhotic patients with GI hemorrhage |
| Norfloxacin 400 mg PO twice daily or ceftriaxone 1 g IV daily for 7 d | |
| IV ceftriaxone is preferred, in patients with advanced cirrhosis as defined by the presence of at least two of the following: Ascites, severe malnutrition, encephalopathy or bilirubin > 3 mg/dL | |
| Primary prophylaxis in patients with low ascitic fluid protein[32,41] | Recommended for cirrhotic patients with ascitic fluid protein < 1.5 g/dL and at least one of the following is present: Serum creatinine > 1.2 mg/dL, blood urea nitrogen > 25 mg/dL, serum sodium < 130 mEq/L or Child-Pugh > 9 points with bilirubin > 3 mg/dL |
| Prophylaxis before undergoing endoscopic and surgical procedures | Prophylactic antiobiotics are recommended for the moderate-high risk invasive endoscopic or surgical procedures (choice of antibiotics should be individualized) |
| Prophylactic antibiotics are not routinely recommended for diagnostic endoscopy, elective variceal band ligation or sclerotherapy, and abdominal paracentesis |
Primary prophylaxis of SBP is justified for patients with high risk for developing SBP. A meta-analysis of ATB prophylaxis in cirrhotic patients with GI hemorrhage (5 RCT; n = 534) revealed 32% reduction of infections including SBP and/or bacteremia (P < 0.001) and 9% increase in survival (P = 0.004)[28]. Further, a subsequent meta-analysis of 8 oral antibiotic trials (n = 647) demonstrated 72% reduction in mortality at 3 mo; only 6 patients were additionally treated in order to prevent another death[65]. Oral norfloxacin is often utilized for primary prophylaxis in most settings, however IV ceftriaxone has been shown to be more effective than oral norfloxacin in patients with particularly advanced cirrhosis[66] (Table 4).
In cirrhotic patients with low ascitic fluid protein < 1.5 g/dL, the risk of developing a first episode of SBP is 13%-45% at 1 year[32,39]. However, several studies evaluating primary prophylaxis of SBP with norfloxacin in this setting yielded heterogeneous results[39]. Notably, a well-designed, randomized, controlled trial conducted in patients with severe liver disease and ascites protein < 1.5 g/dL without prior SBP demonstrated that norfloxacin (400 mg/d) reduced the development of SBP (from 61% to 7%) and improved survival at 1 year (from 48% to 60%)[67]. Notably, primary prophylactic ATB for SBP should be considered only for selected patients with advanced cirrhosis and ascitic fluid protein < 1.5 g/dL since more liberal use of these ATB in long-term would lead to subsequent infection by resistant bacteria as well as Clostridium difficile-associated diarrhea (Table 4)[39-41].
Bacterial infections in cirrhosis are associated with poor outcomes (increased mortality about 4 folds)[47]. Both short- and long-term mortality rates of sepsis in cirrhotic patients are very high; 26%-44% of patients die within 1 mo after infection and another one-third die in 1 year[4,47]. The clinical predictors of death during or following infection are advanced liver disease, nosocomial origin, gastrointestinal hemorrhage, encephalopathy, liver cancer, presence of shock and organ failure (especially renal failure)[4,47].
The suggested strategies for the management of cirrhotic patients with severe sepsis are discussed in depth in other articles[23,32,68,69]. Broad spectrum empirical ATB[70] and fluid resuscitation, with either cystalloids or colloids (albumin, gelatins or hydroxyethyl starches), should be promptly initiated and followed an early goal-directed therapy approach (stepwise emergent resuscitation with predefined goals to keep mean arterial pressure ≥ 65 mmHg, central venous pressure between 8-12 mmHg, central venous oxygen saturation ≥ 70% and urine output ≥ 0.5 mL/kg per hour)[23,32,68]. Resuscitation with crystalloids requires more fluid to attain the same targets and results in more edema, particularly in cirrhotic patients with hypoalbuminemia[32]. The benefit of resuscitation with albumin in non-cirrhotic patients with sepsis has been reported[71]. However, the role of albumin infusion for sepsis other than from SBP in cirrhosis is still unclear. The RCT from Spain found beneficial effects on renal and circulatory functions with a potential benefit on survival[72]. Conversely, more recent RCT from France reported that albumin delayed the onset of renal failure, but did not significantly improve 3-mo renal failure and survival rates. Thus, pulmonary edema developed in 8% of patients in the albumin group[73]. Norepinephrine and dopamine have been considered as the first-choice vasopressor agents in patients with septic shock[23,32,68,69]. Cirrhotic patients with septic shock are often associated with vascular hyporeactivity to these vasopressor agents. Thus, inotropic drugs are not generally effective since they already present high cardiac outputs[23,32,68]. Relative adrenal insufficiency is common (51%-77%) in cirrhotic patients with septic shock, however the effects of corticosteroids on such patients’ outcomes are unclear[23,32,68]. Therefore, stress dose corticosteroid is currently recommended only for patients with vasopressor-unresponsive septic shock[23,32,68]. Blood sugar should be maintained in the range of 140-180 mg/dL[69].
Acute kidney injury following infections develop in 27%-34% of patients with advanced cirrhosis[2,61,74,75], and is a strong predictor of death (40%-50% mortality)[47,74,75]. Risk factors for infection-induced renal failure in cirrhosis include advanced liver disease[74-76], pre-existing kidney disease[76], hypovolemia or low cardiac output[2,75], unresolved infection[74] and not receiving prompt albumin infusion[61]. It should be noted that most studies that reported poor survival in patients with infection-induced renal failure have defined renal failure as a serum creatinine level of > 1.5 mg/dL. Recently, the International Ascites Club and the Acute Dialysis Quality Initiative group proposed that acute kidney injury (AKI) in cirrhosis should be redefined as an increase in serum creatinine level of 0.3 mg/dL in less than 48 h or a 50% increase in serum creatinine level from a stable baseline reading within the previous 6 mo, irrespective of the final serum creatinine level[77,78]. This new definition was then evaluated and found to accurately predict 30-d mortality in patients with cirrhosis and infection (10-fold higher among those with irreversible AKI than those without AKI)[79]. Renal failure during infection (without septic shock) that does not respond to albumin infusion is considered hepatorenal syndrome[80].
Bacterial infection can trigger a rapid deterioration of liver functions in patients with cirrhosis and it is one of the most common precipitating cause of ACLF, which represents > 30% of the cases[3,23,81,82]. The most common sites of bacterial infection are ascites and lungs[81]. Moreover, infections were the second most common cause of death at 28 d among patients with ACLF (28%), behind multiple organ failure without septic or hypovolemic shock (44%). However, there was no difference in 28 d mortality among ACLF patients with or without the bacterial infection at admission (37% and 33%, respectively)[81]. Independent predictors of poor survival in patients with bacterial infections and ACLF were presence of organ(s) failure, second infections, admission values of high MELD, low blood pressure, leukocutosis, and low albumin[83].
Pulmonary complications are commonly observed in cirrhotic patients with infections. Aspiration is common in encephalopathic patients. Acute respiratory distress syndrome is increasingly seen in cirrhosis that may develop is association with exaggerated SIRS in severe sepsis[84]. Prognosis of cirrhotic patients with respiratory failure is poor, with a mortality rate up to 33%-60%[69,85]. Additionally, sepsis-induced cytokines can further worsen pre-existing coagulation and platelet abnormalities in patients with cirrhosis[2,24].
Preventive measures must be emphasized to all patients with cirrhosis and prophylactic ATB is suggested for those who are at high risk of developing infections (Table 4)[2]. Notably, antibiotic prophylaxis has been associated with the development of multi-drug resistant bacteria and C. difficile infection. Therefore it should be judiciously used in those patients with proper indications.
Active immunization against hepatitis A and B viruses, influenza and pneumococcus are recommended since these preventable infections carry accompanied by higher morbidity and mortality in patients with cirrhosis (Table 4)[86-88]. Both cellular and humoral immune responses are suboptimal in cirrhosis, particularly in the advanced stage, which can be associated with inadequate post-vaccination antibody response, as well as loss of immunogenicity in the long-term[86-88]. Therefore, it is important to address immunization needs in patients with chronic liver disease or compensated cirrhosis early on, when immunizations are most effective.
Although there is no clear recommendation whether we can safely utilize live and attenuated vaccines in patients with cirrhosis, inactivated or killed-type vaccinations are generally preferable[86-88]. The incidence and severity of Streptococcus pneumoniae infections are increased in patients with cirrhosis[89-92]. Pneumococcal vaccination is less effective in patients with cirrhosis, with a further decline in protective antibodies after LT[93]. It is therefore recommended with booster doses every 5 years[86-88]. Incidence of seasonal flu is not obviously increased in cirrhosis; however, influenza may precipitate liver decompensation[86,87,94]. Influenza vaccine is well-tolerated and effective in cirrhotic patients, despite a mildly decreased immunogenicity[95,96]. All other vaccinations recommended for general adult population are also indicated in patients with cirrhosis as the Centers for Disease Control and Prevention recommendation for adults[97].
Proton pump inhibitors (PPIs) have been widely used in patients with cirrhosis (sometimes over-utilized)[98]. Patients with cirrhosis have high prevalence of gastroduodenal mucosal lesions[99,100] and are associated with increased mortality rate from peptic ulcer bleeding (adjusted OR = 3.3; 95%CI: 2.2-4.9)[101]. However, clear evidence for a protective role of PPIs in cirrhosis is limited.
A state of gastric acid suppression induced by PPIs, particularly in long-term users, is known to be associated with small bowel bacterial overgrowth, alteration of gut flora and reduction of gastrointestinal motility[102-104]. By these effects, PPIs may enhance BT and possibly increase the risk of various infections in patients with cirrhosis. In addition, impairment of neutrophil function caused by PPIs has also been reported[105-107]. There have been several studies, including case-control, retrospective and prospective cohorts, and meta-analyses, suggesting that PPIs are associated with increased risk of bacterial infections, such as SBP, bacteremia, Clostridium difficile-associated diarrhea, and enteric infections, in patients with cirrhosis[108-115]. However, the association between PPIs and infections in cirrhosis remains somewhat controversial since many studies have reported conflicting results[116-119] (Table 5). Though randomized controlled studies are required to draw firm conclusions whether or not PPIs increase infections in cirrhosis, PPI should be used only if clinically indicated.
| Ref. | Design | n | Results |
| Campbell et al[116] | Case-control | 116 | NS for SBP (OR = 1.05; 95%CI: 0.43-2.57) |
| Bajaj et al[108] | Case-control | 83230 | PPI use were significantly higher in those with CDAD (74% vs 31%, P = 0.0001) |
| Bajaj et al[112] | Retrospective, propensity-matched | 1268 | ↑ Serious infections (HR = 1.66; 95%CI: 1.31-2.12) |
| de Vos et al[119] | Case-control | 102 | PPI were more frequently used in SBP patients than in controls, but did not influence prognosis of SBP |
| Min et al[113] | Retrospective cohort | 1554 | ↑ SBP (HR = 1.39; 95%CI: 1.057-1.843) |
| Mandorfer et al[117] | Retrospective | 607 | PPI neither predisposes to SBP (HR = 1.38; 95%CI: 0.63-3.01) or other infections (HR = 1.71; 95%CI: 0.85-3.44) |
| Terg et al[118] | Prospective | 770 | PPI therapy was not associated with a higher risk of SBP and other infections |
| Merli et al[114] | Cross-sectional | 400 | ↑ Bacterial infections (OR = 2; 95%CI: 1.2-3.2) |
| O'Leary et al[115] | Prospective | 188 | ↑ Infections: CDAD and SBP (OR = 2.94; 95%CI: 1.39-6.20) |
The authors are grateful to Professor K Rajender Reddy at the University of Pennsylvania, PA, United States for supportive guidance.
P- Reviewer: Hsieh CB, Montalto G S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Bonnel AR, Bunchorntavakul C, Reddy KR. Immune dysfunction and infections in patients with cirrhosis. Clin Gastroenterol Hepatol. 2011;9:727-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 281] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 2. | Bunchorntavakul C, Chavalitdhamrong D. Bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. World J Hepatol. 2012;4:158-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Tandon P, Garcia-Tsao G. Bacterial infections, sepsis, and multiorgan failure in cirrhosis. Semin Liver Dis. 2008;28:26-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 379] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 4. | Christou L, Pappas G, Falagas ME. Bacterial infection-related morbidity and mortality in cirrhosis. Am J Gastroenterol. 2007;102:1510-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 148] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 5. | Ghassemi S, Garcia-Tsao G. Prevention and treatment of infections in patients with cirrhosis. Best Pract Res Clin Gastroenterol. 2007;21:77-93. [PubMed] |
| 6. | Fiuza C, Salcedo M, Clemente G, Tellado JM. In vivo neutrophil dysfunction in cirrhotic patients with advanced liver disease. J Infect Dis. 2000;182:526-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 157] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Garfia C, García-Ruiz I, Solís-Herruzo JA. Deficient phospholipase C activity in blood polimorphonuclear neutrophils from patients with liver cirrhosis. J Hepatol. 2004;40:749-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Shawcross DL, Wright GA, Stadlbauer V, Hodges SJ, Davies NA, Wheeler-Jones C, Pitsillides AA, Jalan R. Ammonia impairs neutrophil phagocytic function in liver disease. Hepatology. 2008;48:1202-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 140] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 9. | Wasmuth HE, Kunz D, Yagmur E, Timmer-Stranghöner A, Vidacek D, Siewert E, Bach J, Geier A, Purucker EA, Gressner AM. Patients with acute on chronic liver failure display “sepsis-like” immune paralysis. J Hepatol. 2005;42:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 366] [Cited by in RCA: 394] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 10. | Ruot B, Béchereau F, Bayle G, Breuillé D, Obled C. The response of liver albumin synthesis to infection in rats varies with the phase of the inflammatory process. Clin Sci (Lond). 2002;102:107-114. [PubMed] |
| 11. | Guarner-Argente C, Sánchez E, Vidal S, Román E, Concepción M, Poca M, Sánchez D, Juárez C, Soriano G, Guarner C. Toll-like receptor 4 D299G polymorphism and the incidence of infections in cirrhotic patients. Aliment Pharmacol Ther. 2010;31:1192-1199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Nischalke HD, Berger C, Aldenhoff K, Thyssen L, Gentemann M, Grünhage F, Lammert F, Nattermann J, Sauerbruch T, Spengler U. Toll-like receptor (TLR) 2 promoter and intron 2 polymorphisms are associated with increased risk for spontaneous bacterial peritonitis in liver cirrhosis. J Hepatol. 2011;55:1010-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 72] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Ledesma Castaño F, Echevarria Vierna S, Lozano Polo JL, Oloriz Rivas R, Alvarez Moreno C, Pons Romero F. Interleukin-1 in alcoholic cirrhosis of the liver: the influence of nutrition. Eur J Clin Nutr. 1992;46:527-533. [PubMed] |
| 14. | Gomez F, Ruiz P, Schreiber AD. Impaired function of macrophage Fc gamma receptors and bacterial infection in alcoholic cirrhosis. N Engl J Med. 1994;331:1122-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 116] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 15. | Wiest R, Lawson M, Geuking M. Pathological bacterial translocation in liver cirrhosis. J Hepatol. 2014;60:197-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 494] [Cited by in RCA: 562] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 16. | Bellot P, Francés R, Such J. Pathological bacterial translocation in cirrhosis: pathophysiology, diagnosis and clinical implications. Liver Int. 2013;33:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 183] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 17. | Wiest R, Garcia-Tsao G. Bacterial translocation (BT) in cirrhosis. Hepatology. 2005;41:422-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 492] [Cited by in RCA: 505] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 18. | Bellot P, García-Pagán JC, Francés R, Abraldes JG, Navasa M, Pérez-Mateo M, Such J, Bosch J. Bacterial DNA translocation is associated with systemic circulatory abnormalities and intrahepatic endothelial dysfunction in patients with cirrhosis. Hepatology. 2010;52:2044-2052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 170] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 19. | Teltschik Z, Wiest R, Beisner J, Nuding S, Hofmann C, Schoelmerich J, Bevins CL, Stange EF, Wehkamp J. Intestinal bacterial translocation in rats with cirrhosis is related to compromised Paneth cell antimicrobial host defense. Hepatology. 2012;55:1154-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 148] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 20. | Campillo B, Pernet P, Bories PN, Richardet JP, Devanlay M, Aussel C. Intestinal permeability in liver cirrhosis: relationship with severe septic complications. Eur J Gastroenterol Hepatol. 1999;11:755-759. [PubMed] |
| 21. | Chang CS, Chen GH, Lien HC, Yeh HZ. Small intestine dysmotility and bacterial overgrowth in cirrhotic patients with spontaneous bacterial peritonitis. Hepatology. 1998;28:1187-1190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 181] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Reiberger T, Ferlitsch A, Payer BA, Mandorfer M, Heinisch BB, Hayden H, Lammert F, Trauner M, Peck-Radosavljevic M, Vogelsang H. Non-selective betablocker therapy decreases intestinal permeability and serum levels of LBP and IL-6 in patients with cirrhosis. J Hepatol. 2013;58:911-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 254] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 23. | Gustot T, Durand F, Lebrec D, Vincent JL, Moreau R. Severe sepsis in cirrhosis. Hepatology. 2009;50:2022-2033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 326] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 24. | Wong F, Bernardi M, Balk R, Christman B, Moreau R, Garcia-Tsao G, Patch D, Soriano G, Hoefs J, Navasa M. Sepsis in cirrhosis: report on the 7th meeting of the International Ascites Club. Gut. 2005;54:718-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 281] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 25. | Barnes PF, Arevalo C, Chan LS, Wong SF, Reynolds TB. A prospective evaluation of bacteremic patients with chronic liver disease. Hepatology. 1988;8:1099-1103. [PubMed] |
| 26. | Borzio M, Salerno F, Piantoni L, Cazzaniga M, Angeli P, Bissoli F, Boccia S, Colloredo-Mels G, Corigliano P, Fornaciari G. Bacterial infection in patients with advanced cirrhosis: a multicentre prospective study. Dig Liver Dis. 2001;33:41-48. [PubMed] |
| 27. | Fernández J, Navasa M, Gómez J, Colmenero J, Vila J, Arroyo V, Rodés J. Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophylaxis. Hepatology. 2002;35:140-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 661] [Cited by in RCA: 629] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 28. | Bernard B, Grangé JD, Khac EN, Amiot X, Opolon P, Poynard T. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology. 1999;29:1655-1661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 594] [Cited by in RCA: 461] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 29. | Caly WR, Strauss E. A prospective study of bacterial infections in patients with cirrhosis. J Hepatol. 1993;18:353-358. [PubMed] |
| 30. | Merli M, Lucidi C, Giannelli V, Giusto M, Riggio O, Falcone M, Ridola L, Attili AF, Venditti M. Cirrhotic patients are at risk for health care-associated bacterial infections. Clin Gastroenterol Hepatol. 2010;8:979-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 231] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 31. | Fernández J, Acevedo J, Castro M, Garcia O, de Lope CR, Roca D, Pavesi M, Sola E, Moreira L, Silva A. Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: a prospective study. Hepatology. 2012;55:1551-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 478] [Cited by in RCA: 434] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 32. | Fernández J, Gustot T. Management of bacterial infections in cirrhosis. J Hepatol. 2012;56 Suppl 1:S1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 250] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 33. | Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide to antibiotic decisions: past, present and future. BMC Med. 2011;9:107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 295] [Cited by in RCA: 327] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 34. | Lin KH, Wang FL, Wu MS, Jiang BY, Kao WL, Chao HY, Wu JY, Lee CC. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection in patients with liver cirrhosis: a systematic review and meta-analysis. Diagn Microbiol Infect Dis. 2014;80:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 35. | Papp M, Vitalis Z, Altorjay I, Tornai I, Udvardy M, Harsfalvi J, Vida A, Kappelmayer J, Lakatos PL, Antal-Szalmas P. Acute phase proteins in the diagnosis and prediction of cirrhosis associated bacterial infections. Liver Int. 2012;32:603-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 36. | Gioannini TL, Zhang D, Teghanemt A, Weiss JP. An essential role for albumin in the interaction of endotoxin with lipopolysaccharide-binding protein and sCD14 and resultant cell activation. J Biol Chem. 2002;277:47818-47825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 37. | Wiest R, Krag A, Gerbes A. Spontaneous bacterial peritonitis: recent guidelines and beyond. Gut. 2012;61:297-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 234] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 38. | Chinnock B, Afarian H, Minnigan H, Butler J, Hendey GW. Physician clinical impression does not rule out spontaneous bacterial peritonitis in patients undergoing emergency department paracentesis. Ann Emerg Med. 2008;52:268-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 39. | European Association for the Study of the Liver. EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1125] [Cited by in RCA: 1131] [Article Influence: 75.4] [Reference Citation Analysis (0)] |
| 40. | Runyon BA. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49:2087-2107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 628] [Cited by in RCA: 613] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 41. | Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013;57:1651-1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 519] [Article Influence: 43.3] [Reference Citation Analysis (1)] |
| 42. | Toledo C, Salmerón JM, Rimola A, Navasa M, Arroyo V, Llach J, Ginès A, Ginès P, Rodés J. Spontaneous bacterial peritonitis in cirrhosis: predictive factors of infection resolution and survival in patients treated with cefotaxime. Hepatology. 1993;17:251-257. [PubMed] |
| 43. | Cheong HS, Kang CI, Lee JA, Moon SY, Joung MK, Chung DR, Koh KC, Lee NY, Song JH, Peck KR. Clinical significance and outcome of nosocomial acquisition of spontaneous bacterial peritonitis in patients with liver cirrhosis. Clin Infect Dis. 2009;48:1230-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 126] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 44. | Almdal TP, Skinhøj P. Spontaneous bacterial peritonitis in cirrhosis. Incidence, diagnosis, and prognosis. Scand J Gastroenterol. 1987;22:295-300. [PubMed] |
| 45. | Campillo B, Richardet JP, Kheo T, Dupeyron C. Nosocomial spontaneous bacterial peritonitis and bacteremia in cirrhotic patients: impact of isolate type on prognosis and characteristics of infection. Clin Infect Dis. 2002;35:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 121] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 46. | Titó L, Rimola A, Ginès P, Llach J, Arroyo V, Rodés J. Recurrence of spontaneous bacterial peritonitis in cirrhosis: frequency and predictive factors. Hepatology. 1988;8:27-31. [PubMed] |
| 47. | Arvaniti V, D’Amico G, Fede G, Manousou P, Tsochatzis E, Pleguezuelo M, Burroughs AK. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis. Gastroenterology. 2010;139:1246-1256, 1256.e1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 720] [Cited by in RCA: 837] [Article Influence: 55.8] [Reference Citation Analysis (0)] |
| 48. | Dever JB, Sheikh MY. Review article: spontaneous bacterial peritonitis--bacteriology, diagnosis, treatment, risk factors and prevention. Aliment Pharmacol Ther. 2015;41:1116-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 125] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 49. | Bobadilla M, Sifuentes J, Garcia-Tsao G. Improved method for bacteriological diagnosis of spontaneous bacterial peritonitis. J Clin Microbiol. 1989;27:2145-2147. [PubMed] |
| 50. | Nousbaum JB, Cadranel JF, Nahon P, Khac EN, Moreau R, Thévenot T, Silvain C, Bureau C, Nouel O, Pilette C, Paupard T, Vanbiervliet G, Oberti F, Davion T, Jouannaud V, Roche B, Bernard PH, Beaulieu S, Danne O, Thabut D, Chagneau-Derrode C, de Lédinghen V, Mathurin P, Pauwels A, Bronowicki JP, Habersetzer F, Abergel A, Audigier JC, Sapey T, Grangé JD, Tran A. Diagnostic accuracy of the Multistix 8 SG reagent strip in diagnosis of spontaneous bacterial peritonitis. Hepatology. 2007;45:1275-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 93] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 51. | Mendler MH, Agarwal A, Trimzi M, Madrigal E, Tsushima M, Joo E, Santiago M, Flores E, David G, Workman A. A new highly sensitive point of care screen for spontaneous bacterial peritonitis using the leukocyte esterase method. J Hepatol. 2010;53:477-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 52. | Koulaouzidis A. Diagnosis of spontaneous bacterial peritonitis: an update on leucocyte esterase reagent strips. World J Gastroenterol. 2011;17:1091-1094. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 53. | Lippi G, Caleffi A, Pipitone S, Elia G, Ngah A, Aloe R, Avanzini P, Ferrari C. Assessment of neutrophil gelatinase-associated lipocalin and lactate dehydrogenase in peritoneal fluids for the screening of bacterial peritonitis. Clin Chim Acta. 2013;418:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 54. | Soriano G, Esparcia O, Montemayor M, Guarner-Argente C, Pericas R, Torras X, Calvo N, Román E, Navarro F, Guarner C. Bacterial DNA in the diagnosis of spontaneous bacterial peritonitis. Aliment Pharmacol Ther. 2011;33:275-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 55. | Enomoto H, Inoue S, Matsuhisa A, Aizawa N, Imanishi H, Saito M, Iwata Y, Tanaka H, Ikeda N, Sakai Y. Development of a new in situ hybridization method for the detection of global bacterial DNA to provide early evidence of a bacterial infection in spontaneous bacterial peritonitis. J Hepatol. 2012;56:85-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 56. | Navasa M, Follo A, Llovet JM, Clemente G, Vargas V, Rimola A, Marco F, Guarner C, Forné M, Planas R. Randomized, comparative study of oral ofloxacin versus intravenous cefotaxime in spontaneous bacterial peritonitis. Gastroenterology. 1996;111:1011-1017. [PubMed] |
| 57. | Umgelter A, Reindl W, Miedaner M, Schmid RM, Huber W. Failure of current antibiotic first-line regimens and mortality in hospitalized patients with spontaneous bacterial peritonitis. Infection. 2009;37:2-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 87] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 58. | Castellote J, Ariza X, Girbau A, Broquetas T, Lobatón T, Salord S, Rota R, Xiol X. Antibiotic-resistant bacteria in spontaneous bacterial peritonitis. Is it time to change? J Hepatol. 2010;52:S69. [DOI] [Full Text] |
| 59. | Runyon BA, Hoefs JC. Spontaneous vs secondary bacterial peritonitis. Differentiation by response of ascitic fluid neutrophil count to antimicrobial therapy. Arch Intern Med. 1986;146:1563-1565. [PubMed] |
| 60. | Follo A, Llovet JM, Navasa M, Planas R, Forns X, Francitorra A, Rimola A, Gassull MA, Arroyo V, Rodés J. Renal impairment after spontaneous bacterial peritonitis in cirrhosis: incidence, clinical course, predictive factors and prognosis. Hepatology. 1994;20:1495-1501. [PubMed] |
| 61. | Sort P, Navasa M, Arroyo V, Aldeguer X, Planas R, Ruiz-del-Arbol L, Castells L, Vargas V, Soriano G, Guevara M. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341:403-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1132] [Cited by in RCA: 1003] [Article Influence: 38.6] [Reference Citation Analysis (0)] |
| 62. | Peeraphatdit T, Gulleen EA, Anderson KB, Chaiteerakij R, Skarda PK. Letter: underutilisation of albumin infusion in high-risk spontaneous bacterial peritonitis. Aliment Pharmacol Ther. 2015;42:241-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 63. | Fernández J, Monteagudo J, Bargallo X, Jiménez W, Bosch J, Arroyo V, Navasa M. A randomized unblinded pilot study comparing albumin versus hydroxyethyl starch in spontaneous bacterial peritonitis. Hepatology. 2005;42:627-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 160] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 64. | Ginés P, Rimola A, Planas R, Vargas V, Marco F, Almela M, Forné M, Miranda ML, Llach J, Salmerón JM. Norfloxacin prevents spontaneous bacterial peritonitis recurrence in cirrhosis: results of a double-blind, placebo-controlled trial. Hepatology. 1990;12:716-724. [PubMed] |
| 65. | Saab S, Hernandez JC, Chi AC, Tong MJ. Oral antibiotic prophylaxis reduces spontaneous bacterial peritonitis occurrence and improves short-term survival in cirrhosis: a meta-analysis. Am J Gastroenterol. 2009;104:993-1001; quiz 1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 66. | Fernández J, Ruiz del Arbol L, Gómez C, Durandez R, Serradilla R, Guarner C, Planas R, Arroyo V, Navasa M. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology. 2006;131:1049-1056; quiz 1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 246] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 67. | Fernández J, Navasa M, Planas R, Montoliu S, Monfort D, Soriano G, Vila C, Pardo A, Quintero E, Vargas V. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology. 2007;133:818-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 451] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 68. | Ginès P, Fernández J, Durand F, Saliba F. Management of critically-ill cirrhotic patients. J Hepatol. 2012;56 Suppl 1:S13-S24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 69. | Olson JC, Wendon JA, Kramer DJ, Arroyo V, Jalan R, Garcia-Tsao G, Kamath PS. Intensive care of the patient with cirrhosis. Hepatology. 2011;54:1864-1872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 187] [Article Influence: 13.4] [Reference Citation Analysis (1)] |
| 70. | Arabi YM, Dara SI, Memish Z, Al Abdulkareem A, Tamim HM, Al-Shirawi N, Parrillo JE, Dodek P, Lapinsky S, Feinstein D. Antimicrobial therapeutic determinants of outcomes from septic shock among patients with cirrhosis. Hepatology. 2012;56:2305-2315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 114] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 71. | Delaney AP, Dan A, McCaffrey J, Finfer S. The role of albumin as a resuscitation fluid for patients with sepsis: a systematic review and meta-analysis. Crit Care Med. 2011;39:386-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 202] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 72. | Guevara M, Terra C, Nazar A, Solà E, Fernández J, Pavesi M, Arroyo V, Ginès P. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012;57:759-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 146] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 73. | Thévenot T, Bureau C, Oberti F, Anty R, Louvet A, Plessier A, Rudler M, Heurgué-Berlot A, Rosa I, Talbodec N, Dao T, Ozenne V, Carbonell N, Causse X, Goria O, Minello A, De Ledinghen V, Amathieu R, Barraud H, Nguyen-Khac E, Becker C, Paupard T, Botta-Fridlung D, Abdelli N, Guillemot F, Monnet E, Di Martino V. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015;62:822-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 144] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 74. | Fasolato S, Angeli P, Dallagnese L, Maresio G, Zola E, Mazza E, Salinas F, Donà S, Fagiuoli S, Sticca A. Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical features. Hepatology. 2007;45:223-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 200] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 75. | Terra C, Guevara M, Torre A, Gilabert R, Fernández J, Martín-Llahí M, Baccaro ME, Navasa M, Bru C, Arroyo V. Renal failure in patients with cirrhosis and sepsis unrelated to spontaneous bacterial peritonitis: value of MELD score. Gastroenterology. 2005;129:1944-1953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 169] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 76. | Terg R, Gadano A, Cartier M, Casciato P, Lucero R, Muñoz A, Romero G, Levi D, Terg G, Miguez C. Serum creatinine and bilirubin predict renal failure and mortality in patients with spontaneous bacterial peritonitis: a retrospective study. Liver Int. 2009;29:415-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 77. | Wong F, Nadim MK, Kellum JA, Salerno F, Bellomo R, Gerbes A, Angeli P, Moreau R, Davenport A, Jalan R. Working Party proposal for a revised classification system of renal dysfunction in patients with cirrhosis. Gut. 2011;60:702-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 287] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 78. | Angeli P, Ginès P, Wong F, Bernardi M, Boyer TD, Gerbes A, Moreau R, Jalan R, Sarin SK, Piano S. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. J Hepatol. 2015;62:968-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 527] [Article Influence: 52.7] [Reference Citation Analysis (1)] |
| 79. | Wong F, O’Leary JG, Reddy KR, Patton H, Kamath PS, Fallon MB, Garcia-Tsao G, Subramanian RM, Malik R, Maliakkal B. New consensus definition of acute kidney injury accurately predicts 30-day mortality in patients with cirrhosis and infection. Gastroenterology. 2013;145:1280-1288.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 196] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 80. | Salerno F, Gerbes A, Ginès P, Wong F, Arroyo V. Diagnosis, prevention and treatment of hepatorenal syndrome in cirrhosis. Gut. 2007;56:1310-1318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 356] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 81. | Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, Durand F, Gustot T, Saliba F, Domenicali M. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144:1426-1437, 1437.e1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1720] [Cited by in RCA: 2169] [Article Influence: 180.8] [Reference Citation Analysis (5)] |
| 82. | Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, Arroyo V, Kamath PS. Acute-on chronic liver failure. J Hepatol. 2012;57:1336-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 447] [Cited by in RCA: 457] [Article Influence: 35.2] [Reference Citation Analysis (1)] |
| 83. | Bajaj JS, O’Leary JG, Reddy KR, Wong F, Biggins SW, Patton H, Fallon MB, Garcia-Tsao G, Maliakkal B, Malik R. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures. Hepatology. 2014;60:250-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 436] [Article Influence: 39.6] [Reference Citation Analysis (1)] |
| 84. | TenHoor T, Mannino DM, Moss M. Risk factors for ARDS in the United States: analysis of the 1993 National Mortality Followback Study. Chest. 2001;119:1179-1184. [PubMed] |
| 85. | Thomson SJ, Moran C, Cowan ML, Musa S, Beale R, Treacher D, Hamilton M, Grounds RM, Rahman TM. Outcomes of critically ill patients with cirrhosis admitted to intensive care: an important perspective from the non-transplant setting. Aliment Pharmacol Ther. 2010;32:233-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 86. | Leise MD, Talwalkar JA. Immunizations in chronic liver disease: what should be done and what is the evidence. Curr Gastroenterol Rep. 2013;15:300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 87. | Loulergue P, Pol S, Mallet V, Sogni P, Launay O. Why actively promote vaccination in patients with cirrhosis? J Clin Virol. 2009;46:206-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 88. | Mehta G, Rothstein KD. Health maintenance issues in cirrhosis. Med Clin North Am. 2009;93:901-915, viii-ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 89. | Bouza E, Pintado V, Rivera S, Blázquez R, Muñoz P, Cercenado E, Loza E, Rodríguez-Créixems M, Moreno S. Nosocomial bloodstream infections caused by Streptococcus pneumoniae. Clin Microbiol Infect. 2005;11:919-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 90. | Pirovino M, Lydick E, Grob PJ, Arrenbrecht S, Altorfer J, Schmid M. Pneumococcal vaccination: the response of patients with alcoholic liver cirrhosis. Hepatology. 1984;4:946-949. [PubMed] |
| 91. | Viasus D, Garcia-Vidal C, Castellote J, Adamuz J, Verdaguer R, Dorca J, Manresa F, Gudiol F, Carratalà J. Community-acquired pneumonia in patients with liver cirrhosis: clinical features, outcomes, and usefulness of severity scores. Medicine (Baltimore). 2011;90:110-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 92. | Choi SH, Park HG, Jun JB, Lee SO, Choi SH, Woo JH, Kim YS. Clinical characteristics and outcomes of pneumococcal bacteremia in adult patients with liver cirrhosis. Diagn Microbiol Infect Dis. 2009;63:160-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 93. | McCashland TM, Preheim LC, Gentry MJ. Pneumococcal vaccine response in cirrhosis and liver transplantation. J Infect Dis. 2000;181:757-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 125] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 94. | Duchini A, Viernes ME, Nyberg LM, Hendry RM, Pockros PJ. Hepatic decompensation in patients with cirrhosis during infection with influenza A. Arch Intern Med. 2000;160:113-115. [PubMed] |
| 95. | Cheong HJ, Song JY, Park JW, Yeon JE, Byun KS, Lee CH, Cho HI, Kim TG, Kim WJ. Humoral and cellular immune responses to influenza vaccine in patients with advanced cirrhosis. Vaccine. 2006;24:2417-2422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 96. | Song JY, Cheong HJ, Ha SH, Hwang IS, Kee SY, Jeong HW, Lee CG, Kim WJ. Clinical impact of influenza immunization in patients with liver cirrhosis. J Clin Virol. 2007;39:159-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 97. | Kim DK, Bridges CB, Harriman KH. Advisory committee on immunization practices recommended immunization schedule for adults aged 19 years or older--United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64:91-92. [PubMed] |
| 98. | Lodato F, Azzaroli F, Di Girolamo M, Feletti V, Cecinato P, Lisotti A, Festi D, Roda E, Mazzella G. Proton pump inhibitors in cirrhosis: tradition or evidence based practice? World J Gastroenterol. 2008;14:2980-2985. [PubMed] |
| 99. | Rabinovitz M, Yoo YK, Schade RR, Dindzans VJ, Van Thiel DH, Gavaler JS. Prevalence of endoscopic findings in 510 consecutive individuals with cirrhosis evaluated prospectively. Dig Dis Sci. 1990;35:705-710. [PubMed] |
| 100. | Luo JC, Leu HB, Hou MC, Huang CC, Lin HC, Lee FY, Chang FY, Chan WL, Lin SJ, Chen JW. Cirrhotic patients at increased risk of peptic ulcer bleeding: a nationwide population-based cohort study. Aliment Pharmacol Ther. 2012;36:542-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 101. | Venkatesh PG, Parasa S, Njei B, Sanaka MR, Navaneethan U. Increased mortality with peptic ulcer bleeding in patients with both compensated and decompensated cirrhosis. Gastrointest Endosc. 2014;79:605-614.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 102. | Ge PS, Runyon BA. Preventing future infections in cirrhosis: a battle cry for stewardship. Clin Gastroenterol Hepatol. 2015;13:760-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 103. | Lewis SJ, Franco S, Young G, O’Keefe SJ. Altered bowel function and duodenal bacterial overgrowth in patients treated with omeprazole. Aliment Pharmacol Ther. 1996;10:557-561. [PubMed] |
| 104. | Lo WK, Chan WW. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis. Clin Gastroenterol Hepatol. 2013;11:483-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 245] [Article Influence: 20.4] [Reference Citation Analysis (1)] |
| 105. | Agastya G, West BC, Callahan JM. Omeprazole inhibits phagocytosis and acidification of phagolysosomes of normal human neutrophils in vitro. Immunopharmacol Immunotoxicol. 2000;22:357-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 106. | Yoshida N, Yoshikawa T, Tanaka Y, Fujita N, Kassai K, Naito Y, Kondo M. A new mechanism for anti-inflammatory actions of proton pump inhibitors--inhibitory effects on neutrophil-endothelial cell interactions. Aliment Pharmacol Ther. 2000;14 Suppl 1:74-81. [PubMed] |
| 107. | Zedtwitz-Liebenstein K, Wenisch C, Patruta S, Parschalk B, Daxböck F, Graninger W. Omeprazole treatment diminishes intra- and extracellular neutrophil reactive oxygen production and bactericidal activity. Crit Care Med. 2002;30:1118-1122. [PubMed] |
| 108. | Bajaj JS, Ananthakrishnan AN, Hafeezullah M, Zadvornova Y, Dye A, McGinley EL, Saeian K, Heuman D, Sanyal AJ, Hoffmann RG. Clostridium difficile is associated with poor outcomes in patients with cirrhosis: A national and tertiary center perspective. Am J Gastroenterol. 2010;105:106-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 109. | Bajaj JS, Zadvornova Y, Heuman DM, Hafeezullah M, Hoffmann RG, Sanyal AJ, Saeian K. Association of proton pump inhibitor therapy with spontaneous bacterial peritonitis in cirrhotic patients with ascites. Am J Gastroenterol. 2009;104:1130-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 134] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 110. | Choi EJ, Lee HJ, Kim KO, Lee SH, Eun JR, Jang BI, Kim TN. Association between acid suppressive therapy and spontaneous bacterial peritonitis in cirrhotic patients with ascites. Scand J Gastroenterol. 2011;46:616-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 111. | Deshpande A, Pasupuleti V, Thota P, Pant C, Mapara S, Hassan S, Rolston DD, Sferra TJ, Hernandez AV. Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis. J Gastroenterol Hepatol. 2013;28:235-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 112. | Bajaj JS, Ratliff SM, Heuman DM, Lapane KL. Proton pump inhibitors are associated with a high rate of serious infections in veterans with decompensated cirrhosis. Aliment Pharmacol Ther. 2012;36:866-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 113. | Min YW, Lim KS, Min BH, Gwak GY, Paik YH, Choi MS, Lee JH, Kim JJ, Koh KC, Paik SW. Proton pump inhibitor use significantly increases the risk of spontaneous bacterial peritonitis in 1965 patients with cirrhosis and ascites: a propensity score matched cohort study. Aliment Pharmacol Ther. 2014;40:695-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 114. | Merli M, Lucidi C, Di Gregorio V, Giannelli V, Giusto M, Ceccarelli G, Riggio O, Venditti M. The chronic use of beta-blockers and proton pump inhibitors may affect the rate of bacterial infections in cirrhosis. Liver Int. 2015;35:362-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 115. | O’Leary JG, Reddy KR, Wong F, Kamath PS, Patton HM, Biggins SW, Fallon MB, Garcia-Tsao G, Subramanian RM, Malik R. Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis. Clin Gastroenterol Hepatol. 2015;13:753-9.e1-753-9.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 95] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 116. | Campbell MS, Obstein K, Reddy KR, Yang YX. Association between proton pump inhibitor use and spontaneous bacterial peritonitis. Dig Dis Sci. 2008;53:394-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 117. | Mandorfer M, Bota S, Schwabl P, Bucsics T, Pfisterer N, Summereder C, Hagmann M, Blacky A, Ferlitsch A, Sieghart W. Proton pump inhibitor intake neither predisposes to spontaneous bacterial peritonitis or other infections nor increases mortality in patients with cirrhosis and ascites. PLoS One. 2014;9:e110503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 118. | Terg R, Casciato P, Garbe C, Cartier M, Stieben T, Mendizabal M, Niveyro C, Benavides J, Marino M, Colombato L. Proton pump inhibitor therapy does not increase the incidence of spontaneous bacterial peritonitis in cirrhosis: a multicenter prospective study. J Hepatol. 2015;62:1056-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 119. | de Vos M, De Vroey B, Garcia BG, Roy C, Kidd F, Henrion J, Deltenre P. Role of proton pump inhibitors in the occurrence and the prognosis of spontaneous bacterial peritonitis in cirrhotic patients with ascites. Liver Int. 2013;33:1316-1323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 120. | Choi JP, Lee SO, Kwon HH, Kwak YG, Choi SH, Lim SK, Kim MN, Jeong JY, Choi SH, Woo JH. Clinical significance of spontaneous Aeromonas bacterial peritonitis in cirrhotic patients: a matched case-control study. Clin Infect Dis. 2008;47:66-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 121. | Lau SM, Peng MY, Chang FY. Outcomes of Aeromonas bacteremia in patients with different types of underlying disease. J Microbiol Immunol Infect. 2000;33:241-247. [PubMed] |
| 122. | Lay CJ, Zhuang HJ, Ho YH, Tsai YS, Wang LS, Tsai CC. Different clinical characteristics between polymicrobial and monomicrobial Aeromonas bacteremia--a study of 216 cases. Intern Med. 2010;49:2415-2421. [PubMed] |
| 123. | Ko WC, Chuang YC. Aeromonas bacteremia: review of 59 episodes. Clin Infect Dis. 1995;20:1298-1304. [PubMed] |
| 124. | Lee CC, Chi CH, Lee NY, Lee HC, Chen CL, Chen PL, Chang CM, Wu CJ, Ko NY, Tsai MC. Necrotizing fasciitis in patients with liver cirrhosis: predominance of monomicrobial Gram-negative bacillary infections. Diagn Microbiol Infect Dis. 2008;62:219-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 125. | Chao CM, Lai CC, Tang HJ, Ko WC, Hsueh PR. Skin and soft-tissue infections caused by Aeromonas species. Eur J Clin Microbiol Infect Dis. 2013;32:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 126. | Wu CJ, Tsai PJ, Chen PL, Wu IC, Lin YT, Chen YH, Wang LR, Ko WC. Aeromonas aquariorum septicemia and enterocolitis in a cirrhotic patient. Diagn Microbiol Infect Dis. 2012;74:406-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 127. | Pigrau C, Bartolome R, Almirante B, Planes AM, Gavalda J, Pahissa A. Bacteremia due to Campylobacter species: clinical findings and antimicrobial susceptibility patterns. Clin Infect Dis. 1997;25:1414-1420. [PubMed] |
| 128. | Brann OS. Infectious complications of cirrhosis. Curr Gastroenterol Rep. 2001;3:285-292. [PubMed] |
| 129. | Chen YM, Lee HC, Chang CM, Chuang YC, Ko WC. Clostridium bacteremia: emphasis on the poor prognosis in cirrhotic patients. J Microbiol Immunol Infect. 2001;34:113-118. [PubMed] |
| 130. | Cheng NC, Tai HC, Tang YB, Chang SC, Wang JT. Necrotising fasciitis: clinical features in patients with liver cirrhosis. Br J Plast Surg. 2005;58:702-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 131. | Garcia-Tsao G, Surawicz CM. Editorial: Clostridium difficile infection: Yet another predictor of poor outcome in cirrhosis. Am J Gastroenterol. 2010;105:114-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 132. | Siple JF, Morey JM, Gutman TE, Weinberg KL, Collins PD. Proton pump inhibitor use and association with spontaneous bacterial peritonitis in patients with cirrhosis and ascites. Ann Pharmacother. 2012;46:1413-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 133. | Bajaj JS, O’Leary JG, Reddy KR, Wong F, Olson JC, Subramanian RM, Brown G, Noble NA, Thacker LR, Kamath PS. Second infections independently increase mortality in hospitalized patients with cirrhosis: the North American consortium for the study of end-stage liver disease (NACSELD) experience. Hepatology. 2012;56:2328-2335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 329] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 134. | Fernández Guerrero ML, González López J, Górgolas M. Infectious endocarditis in patients with cirrhosis of the liver: a model of infection in the frail patient. Eur J Clin Microbiol Infect Dis. 2010;29:1271-1275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 135. | Lee JH, Yoon JH, Kim BH, Chung GE, Myung SJ, Kim W, Kim YJ, Kim EC, Lee HS. Enterococcus: not an innocent bystander in cirrhotic patients with spontaneous bacterial peritonitis. Eur J Clin Microbiol Infect Dis. 2009;28:21-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 136. | McNeil SA, Malani PN, Chenoweth CE, Fontana RJ, Magee JC, Punch JD, Mackin ML, Kauffman CA. Vancomycin-resistant enterococcal colonization and infection in liver transplant candidates and recipients: a prospective surveillance study. Clin Infect Dis. 2006;42:195-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 105] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 137. | El Sayed Zaki M, El Shabrawy WO, El-Eshmawy MM, Aly Eletreby S. The high prevalence of Listeria monocytogenes peritonitis in cirrhotic patients of an Egyptian Medical Center. J Infect Public Health. 2011;4:211-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 138. | Cabellos C, Viladrich PF, Ariza J, Maiques JM, Verdaguer R, Gudiol F. Community-acquired bacterial meningitis in cirrhotic patients. Clin Microbiol Infect. 2008;14:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 139. | Cho YJ, Lee SM, Yoo CG, Kim YW, Han SK, Shim YS, Yim JJ. Clinical characteristics of tuberculosis in patients with liver cirrhosis. Respirology. 2007;12:401-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 140. | Thulstrup AM, Mølle I, Svendsen N, Sørensen HT. Incidence and prognosis of tuberculosis in patients with cirrhosis of the liver. A Danish nationwide population based study. Epidemiol Infect. 2000;124:221-225. [PubMed] |
| 141. | Tamaskar I, Ravakhah K. Spontaneous bacterial peritonitis with Pasteurella multocida in cirrhosis: case report and review of literature. South Med J. 2004;97:1113-1115. [PubMed] |
| 142. | Migliore E, Serraino C, Brignone C, Ferrigno D, Cardellicchio A, Pomero F, Castagna E, Osenda M, Fenoglio L. Pasteurella multocida infection in a cirrhotic patient: case report, microbiological aspects and a review of literature. Adv Med Sci. 2009;54:109-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 143. | Tseng HK, Su SC, Liu CP, Lee CM. Pasteurella multocida bacteremia due to non-bite animal exposure in cirrhotic patients: report of two cases. J Microbiol Immunol Infect. 2001;34:293-296. [PubMed] |
| 144. | Chapoutot C, Pageaux GP, Perrigault PF, Joomaye Z, Perney P, Jean-Pierre H, Jonquet O, Blanc P, Larrey D. Staphylococcus aureus nasal carriage in 104 cirrhotic and control patients. A prospective study. J Hepatol. 1999;30:249-253. [PubMed] |
| 145. | Park HJ, Lee YM, Bang KM, Park SY, Moon SM, Park KH, Chong YP, Kim SH, Lee SO, Choi SH. Clinical significance of Staphylococcus aureus bacteremia in patients with liver cirrhosis. Eur J Clin Microbiol Infect Dis. 2012;31:3309-3316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 146. | Gonzlez-Quintela A, Martínez-Rey C, Castroagudín JF, Rajo-Iglesias MC, Domínguez-Santalla MJ. Prevalence of liver disease in patients with Streptococcus bovis bacteraemia. J Infect. 2001;42:116-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 147. | Vilaichone RK, Mahachai V, Kullavanijaya P, Nunthapisud P. Spontaneous bacterial peritonitis caused by Streptococcus bovis: case series and review of the literature. Am J Gastroenterol. 2002;97:1476-1479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 148. | Cho SY, Kang CI, Kim J, Joo EJ, Ha YE, Chung DR, Lee NY, Peck KR, Song JH. Association of liver cirrhosis with group B streptococcal bacteremia in non-pregnant adults. J Infect. 2013;67:617-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 149. | Farley MM. Group B streptococcal disease in nonpregnant adults. Clin Infect Dis. 2001;33:556-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 306] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 150. | Tung BY, Kowdley KV. Spontaneous group B streptococcal meningitis in a patient with cirrhosis. West J Med. 1996;165:229-230. [PubMed] |
| 151. | Vollberg CM, Herrera JL. Vibrio vulnificus infection: an important cause of septicemia in patients with cirrhosis. South Med J. 1997;90:1040-1042. [PubMed] |
| 152. | Chiang SR, Chuang YC. Vibrio vulnificus infection: clinical manifestations, pathogenesis, and antimicrobial therapy. J Microbiol Immunol Infect. 2003;36:81-88. [PubMed] |
| 153. | Herrera JL, Rodríguez R. Medical care of the patient with compensated cirrhosis. Gastroen Hepatol. 2006;2:124-133. |
| 154. | Vadillo M, Corbella X, Pac V, Fernandez-Viladrich P, Pujol R. Multiple liver abscesses due to Yersinia enterocolitica discloses primary hemochromatosis: three cases reports and review. Clin Infect Dis. 1994;18:938-941. [PubMed] |
| 155. | Khan FA, Fisher MA, Khakoo RA. Association of hemochromatosis with infectious diseases: expanding spectrum. Int J Infect Dis. 2007;11:482-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 154] [Article Influence: 8.6] [Reference Citation Analysis (0)] |