Published online May 28, 2015. doi: 10.4254/wjh.v7.i9.1209
Peer-review started: August 23, 2014
First decision: November 18, 2014
Revised: November 29, 2014
Accepted: December 18, 2014
Article in press: December 19, 2014
Published online: May 28, 2015
Processing time: 270 Days and 20.9 Hours
Traditional Chinese medicine (TCM) has played a positive role in the management of hepatocarcinoma. Hepatocarcinoma patients may present Qi-stagnation, damp-heat, blood stasis, Qi-deficiency, Yin-deficiency and other TCM syndromes (Zheng). Modern treatments such as surgery, transarterial chemoembolization (TACE) and high intensity focus ultrasound treatment would influence the manifestation of TCM syndromes. Herbs with traditional efficacy of tonifying Qi, blood and Yin, soothing liver-Qi stagnation, clearing heat and detoxifying and dissolving stasis, have been demonstrated to be potent to prevent hepatocarcinogenesis. TCM has been widely used in all aspects of integrative therapy in hepatocarcinoma, including surgical resection, liver transplantation, TACE, local ablative therapies and even as monotherapy for middle-advanced stage hepatocarcinoma. Clinical practices have confirmed that TCM is effective to alleviate clinical symptoms, improve quality of life and immune function, prevent recurrence and metastasis, delay tumor progression, and prolong survival time in hepatocarcinoma patients. The effective mechanism of TCM against hepatocarcinoma is related to inducing apoptosis, autophagy, anoikis and cell senescence, arresting cell cycle, regulating immune function, inhibiting metastasis and angiogenesis, reversing drug resistance and enhancing effects of chemotherapy. Along with the progress of research in this field, TCM will contribute more to the prevention and treatment of hepatocarcinoma.
Core tip: Hepatocarcinoma may present different Traditional Chinese medicine (TCM) syndromes (Zheng). Syndromes are associated with hepatocarcinoma progression and prognosis to a certain degree. Modern technologies have been exploited to elucidate the relation between syndromes and biomedical sciences. Chinese herbs or herbal components have been demonstrated to be effective to prevent and treat hepatocarcinoma. Contemporary TCM physicians have established some effective herbal formulas and Chinese patent herbal drugs for hepatocarcinoma prevention and treatment.
- Citation: Hu B, Wang SS, Du Q. Traditional Chinese medicine for prevention and treatment of hepatocarcinoma: From bench to bedside. World J Hepatol 2015; 7(9): 1209-1232
- URL: https://www.wjgnet.com/1948-5182/full/v7/i9/1209.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i9.1209
Hepatocarcinoma is the sixth most common malignancy and the third principal cause of cancer deaths worldwide[1]. The incidence of hepatocarcinoma is increasing by cause of hepatitis virus infection and other factors[2-4]. Due to latent onset and rapid progression, only a minority of patients with early-stage disease are suitable for potentially curative therapy, i.e., surgical resection or liver transplantation. Treatments for unresectable disease, such as local ablative therapies, transarterial chemoembolization (TACE) and systemic therapy with sorafenib, are essentially palliative[5]. Cancer recurrence is another obstacle to successful treatment, and there is a shortage of preventive means for recurrence. It is important to develop novel approaches for hepatocarcinoma prevention and treatment.
Traditional Chinese medicine (TCM) has played a positive role in the management of hepatocarcinoma[6,7]. TCM has been widely used in all aspects of integrative therapy in hepatocarcinoma, including surgical resection, liver transplantation, chemoembolization, targeted therapy, and even as monotherapy for middle-advanced stage hepatocarcinoma[6-8]. TCM treatment mainly includes multiple herbal therapy and Chinese patent herbal drug therapy. Clinical practices have confirmed that TCM is effective to alleviate clinical symptoms, improve quality of life (QOL), palliate myelosuppression, improve immune function, prevent recurrence and metastasis, delay tumor progression, and prolong survival time[6-9].
TCM therapy is a syndrome differentiation based treatment. Based on TCM pathogenesis, TCM syndrome patterns and different disease stage, TCM physicians employ different therapeutic methods, and prescribe multiple herbs for hepatocarcinoma treatment[10]. The pathogenesis of hepatocarcinoma is related to weakened body defense or deficiency in liver and kidney, liver stagnation, dampness-heat, and blood stasis. Since these pathological factors are also seen in other diseases, contemporary TCM has developed the concept of cancerous toxicity (Ai-Du) to discriminate liver cancer from other common diseases, and underscore the application of anti-cancer therapy to improve overall therapeutic efficacy in hepatocarcinoma[11,12].
During past decades, TCM has been extensively explored to prevent and treat hepatocarcinoma. In this paper, we comprehensively review the experimental and clinical efficacy of TCM against hepatocarcinogenesis and hepatocarcinoma, TCM syndromes in hepatocarcinoma patients and the effective mechanism of TCM in the treatment of hepatocarcinoma, to provide new insights into hepatocarcinoma management.
Disease prevention has long been practiced in TCM. Taking preventive measures against disease or treating before sick had been established as a basic principle for disease control since Inner Canon of Emperor Huang (Huang-Di-Nei-Jing) (400 B.C.), Dr. Zhong-Jing Zhang, one of the most prominent Chinese physicians in history, had developed another principle for liver disease prevention in Synopsis of Golden Cabinet (Jin-Gui-Yao-Lüe) (A.D 200 - 210). Dr. Zhang observed that liver diseases tend to spread to the spleen, and proposed that the spleen-Qi should be reinforced before it is affected. Hepatocarcinoma prevention by Chinese herbs or related products has been extensively studied in recent decades.
Chinese herbal formula or Chinese herbal compound prescription is the most representative application form of Chinese herbs. It has been shown that some classical herbal formulas have preventive effects against hepatocarcingenesis. Ren-shen-bie-jia-jian, a formula for nourishing Qi and dissolving stasis, is effective in inhibiting hepatocarcinogenesis and down-regulation of transforming growth factor-β type II receptor (TGF-βIIR)[13]. Xiao-chai-hu-tang, a formula used for soothing liver-Qi stagnation, may inhibit N-nitrosomorpholine (NNM) induced hepatocarcinogenesis and increase the proportion of helper T lymphocytes in rats[14]. Shi-quan-da-bu-tang, a classical formula for tonifying Qi-blood, inhibits NNM induced hepatocarcinogenesis and increases interleukin-2 (IL-2) receptor-positive lymphocytes in rats[15]. However, the more exploited and studied are modern formulas.
According to TCM theory, the liver and kidney share the same origin, and thus tonifying liver and/or kidney is frequently used to prevent hepatocarcinoma. Nourishing Yin Decoction, a formula for tonifying liver Yin, may inhibit aflatoxin B1 (AFB1) induced hepatocarcinogenesis[16]. A-L tonic capsule, a tonifying liver and kidney Yin and nourishing Qi based Chinese patent drug for improving the immune system in cancer patients, may reduce DNA content and improve its distribution in rat hepatocarcinogenesis induced by diethylnitrosamine (DEN)[17]. Bu Shen Prescription, a formula composed of eight herbs for tonifying kidney, inhibits DEN induced hepatocarcinogenesis in rats[18].
Liu et al[19] established Fu-zheng-hua-yu formula for tonifying kidney and dissolving stasis, and demonstrated that it may inhibit hepatocarcinogenesis and induce cell cycle S phase arrest in DEN treated rat models. Fu-zheng-hua-yu formula has been developed as a Chinese patent drug for liver fibrosis treatment. Huqi San, a formula for tonifying kidney and nourishing Qi, inhibits the over-expression of c-jun, c-fos and c-myc oncogenes and liver preneoplastic lesions induced by DEN[20,21].
Strengthening spleen is an important principle for hepatocarcinoma prevention. Ganfujian, a formula composed of dietary and medicinal Chinese herbs for strengthening spleen, has showed effects in inhibiting hepatocarcinogenesis, and down-regulation of CDK4 (cyclin-dependent kinase 4), cyclin D1 and PCNA (proliferating cell nuclear antigen) in DEN induced hepatic carcinogenesis in rats[22]. Qiu et al[23] have established an herbal recipe for strengthening spleen, regulating Qi, removing heat, and softening hard lumps and resolving phlegm (SRRS). SRRS recipe has been demonstrated to have preventive effects against DEN induced hepatocacinogenesis[23]. Jianpi Jiedu Recipe, an herbal formula for strengthening spleen and detoxification, has been showed to be effective in inhibiting DEN induced hepatocarcinogenesis, down-regulating miR-199a and Phosphatidylinositol-4,5-bisphosphate 3-kinaseV-akt murine thymoma viral oncogene homolog (PI3K/AKT), and up-regulating p70s6k[24,25].
In addition to tonifying treatments, eliminating pathogenic factors is another important principle for hepatocarcinoma prevention. Removing Toxic Heat Decoction, a formula based on detoxifying and tonifying liver Yin, may inhibit AFB1 induced hepatocarcinogenesis[16]. Gao et al[26] evaluated Gan-Zheng oral solution, a formula for detoxification and dissolving stasis, in a DEN induced rat model and demonstrated that it is effective in inhibiting hepatocarcinogenesis and down-regulating intercellular adhesion molecule 1 (ICAM-1)[26]. Zao-Lian mixture, a formula for detoxification, dissolving stasis, strengthening spleen, and soothing liver, may inhibit hepatocarcinogenesis and protect liver function[27]. Sb/Bs remedy, containing Scutellaria baicalensis Georgi (Sb) and Bupleurum scorzonerifolfium Willd (Bs), suppressed N-nitrosobis(2-oxopropyl)amine (BOP) induced liver tumours, increased serum tumor necrosis factor (TNF)-alpha and TGF-beta1, decreased 8-OHdG expression, and increased caspase-3 and apoptosis[28].
Professor Fang’s group has investigated different TCM treatments in DEN mediated hepatocainogenesis, and found that the more efficient treatments are, in order, promoting circulation and removing stasis, clearing heat and detoxifying, and strengthening spleen. All those treatments up-regulated GTPase-activating protein expression and down-regulated Ras expression. Expression of growth factor receptor-bound protein 2 and Raf 1, and son of sevenless was inhibited by those treatments, respectively[29-31]. Herbal compound 861, a formula composed of herbs with dissolving stasis and nourishing Qi efficacy, prevents 2-acetylaminofluorene (2-AAF) induced hepatocarcinogenesis in rats[32]. A new anti-tumor formula with tonifying Qi, soothing liver and dissolving stasis effects inhibits hepatocarcinogenesis induced by HBV and AFB1 accompanied by superoxide dismutase (SOD) and glutathione S-transferase (GST) activation and decreased malondialdehyde (MDA)[33].
Ginseng, one of the most frequently used herbs for tonifying Qi, has been reported to be effective in inhibiting DEN induced hepatocellular carcinoma in rats[34]. Dang-Gui (Angelica sinensis), a common used blood tonic, is potent to inhibit AFB1 induced mutagenicity in Ames test and hepatocarcinogenesis induced by AFB1[35,36]. Ying-tonifying herbs such as Nü-Zhen-Zi (Ligustrum lucidum Ait.), Tian-Dong (Asparagus cochinchinensis), Bai-He (Lilium brownii) and Shan-Zhu-Yu (Cornus officinalis) are efficient to inhibit AFB1 induced mutagenicity in Ames test[36]. Cao-Cong-Rong (Boschniakia rossica), an herb with traditional efficacy of Yang-tonifying, may inhibit DEN induced hepatocarcinogenesis, increase SOD and GSH-PX (glutathione peroxidase), and down-regulate expression of MDA, GST and mutant p53 and p21 proteins[37,38].
Ban-Zi-Lian (Sculellaria barbata), an herb with traditional efficacy of clearing heat and detoxifying, has been widely used as an anti-cancer herb. Ban-Zi-Lian has been reported to be able to inhibit experimental hepatocarcinoma and relieve hepatic injures in DEN treated rats[39]. Tu-Fu-Ling (Smilax glabra Roxb.), another commonly used clearing heat and detoxifying herb, inhibits hepatocarcinogenesis induced by AFB1[35]. Penta-acetyl geniposide, a component of Zhi-Zi (Gardenia jasminoides Ellis), may protect rats from AFB1 induced hepatocarcinogenesis[40]. Berberine, a component of Huang-Lian (Coptis chinensis Franch.) or Huang-Bai (Phellodendron chinense Schnied.), inhibits hepatocyte proliferation and inducible nitric oxide synthase expression, decreases cytochrome P450 content, inhibits activities of cytochrome P450 2E1 (CYP2E1) and CYP1A2 in DEN plus phenobarbital treated rats[41]. Yin-Chen-Hao (Artemisia capillaris Thunb.), an herb for clearing heat, inducing urination and removing jaundice, has been reported to be effective in inhibiting AFB1 induced mutagenicity in Ames test[42].
Dissolving stasis is another principle for hepatocarcinoma prevention. Dan-Shen (Salvia miltiorrhiza Bunge) may inhibit AFB1 mediated mutagenicity and hepatocarcinogenesis, decrease AFB1-DNA adducts formation and AFB1-induced oxidative DNA damage, and induce glutathione S-transferase Yc-2 expression[35,36,43]. Jiang-Huang (Curcuma longa Linn) has beneficial effects on the early and late stages of liver pathogenesis, prevents and delays liver carcinogenesis, and may be related to decreased expression of hepatitis B virus X protein (HBx) and increased expression of p-p53, p21 and cyclin D1 in livers of HBx transgenic mice[44]. Shan-Qi (Panax notoginseng), an herb used for hemostasis and dissolving stasis, has been showed to be effective to inhibit DEN induced hepatocarcinogenesis and angiogenesis accompanied by down-regulation of angiopoietin-2, tunica internal endothelial cell kinase 2, hypoxia inducible factor-1α (HIF-1α) and vascular endothelial growth factor (VEGF)[45].
Wu-Wei-Zi (Schisandra chinensis), commonly used for inducing astringency, could inhibit AFB1 induced mutagenicity in Ames test and hepatocarcinogenesis induced by AFB1[35,36]. Gomisin A, an ingredient of Wu-Wei-Zi, is effective to inhibit 3’-methyl-4-dimethylaminoazobenzene induced hepatocarcinogenesis by enhancing the excretion of the carcinogen from the liver and by reversing the normal cytokinesis[46]. Other herbs, such as Bai-Ji (Bletilla striata), which may inhibit FAB1 induced hepatocarcinogenesis, Shan-Zha (Crataegus pinnatifida), Yi-Yi-Ren (Coix lacryma-jobi L.), Xing-Ren (Prunus armeniaca) and Wu-Mei (Prunus mume), which may inhibit AFB1 induced mutagenicity in Ames test[35,36].
Current treatments for hepatocarcinoma are less than satisfactory. It is important to prevent hepatocarcinogenesis in high risk populations. Jian-Pi-Huo-Xue Formula based herbal treatment has been demonstrated to be effective to inhibit hepatocarcinogenesis in patients with hepatitis, hepatic cirrhosis and low level of AFP[47]. Dan-Shen (Salvia miltiorrhiza Bunge) is potent to protect male individuals from hepatocarcinogenesis in a high incidence area of hepatocarcinoma[48]. In Japan, Sho-saiko-to (TJ-9) (Xiao-chai-hu-tang) has been demonstrated to be potent to prevent heaptocarcinogenesis in patients with cirrhosis, particularly in patients without HBs antigen[49].
Taken together, contemporary TCM physicians have adopted classic TCM theory and principles for hepatocarcinoma prevention study, developed A-L tonic capsule, Fu-zheng-hua-yu capsule, Ganfujian, Gan-Zheng oral solution, Herbal compound 861 and other effective herbal formulas/drugs, and confirmed that Nü-Zhen-Zi, Ban-Zi-Lian, Yin-Chen-Hao, Dan-Shen, Wu-Wei-Zi and other herbs could inhibit hepatocarcinogenesis. It is regrettable that there are no more studies on hepatitis virus induced hepatocarcinogenesis models. Related studies will promote TCM to contribute more to protect high-risk individuals from hepatocarcinogenesis. Herbal formulas for hepatocarcinoma prevention are listed in Table 1.
| Herbal formula | Therapeutic principles | Herbs | Models/patients | Effects | Targets/events | Ref. |
| Ren-shen-bie-jia-jian | Tonifying Qi and dissolving stasis | Ren-Shen (Panax ginseng), Bie-Jia (Carapax trionycis), Tao-Ren (Peach seed) and other herbs | DMN induced hepatic precancerous lesion in rats | Inhibit hepatocarcinogenesis | Down-regulation of TGF-βIIR | [13] |
| Xiao-chai-hu-tang | Soothing liver-Qi stagnation | Chai-Hu (Bupleurum chinense), Huang-Qin (Scutellaria baicalensis Georgi), Sheng-Jiang (Zingiber officinale), Ban-Xia (Pinellia ternata), Da-Zao (Ziziphus jujuba), Ren-Shen (Panax ginseng), Gan-cao (Glycyrrhiza uralensis) | NNM induced hepatocarcinogenesis in rats; patients with cirrhosis | Inhibit hepatocarcinogenesis, prevent hepatocarcinogenesis in patients | Increase helper T lymphocytes | [14,49] |
| Shi-quan-da-bu-tang | Tonifying Qi-Blood | Ren-Shen (Panax ginseng), Bai-Zhu (Atractylodes macrocephala Koidz.), Fu-Ling (Poria cocos), Gan-cao (Glycyrrhiza uralensis), Chuan-Xiong (Ligusticum chuanxiong), Dang Gui (Angelica sinensis), Shu-Di-Huang (Rehmannia glutinosa), Bai-Shao (Paeonia lactiflora), Huang Qi (Astragalus membranaceous), Rou-Gui (Cinnamomum cassia Presl) | NNM induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Increase IL-2 receptor-positive lymphocytes | [15] |
| Nourishing Yin Decoction | Tonifying liver Yin | Bei-Sha-Shen (Glehnia littoralis), Dang-Gui (Angelica sinensis), Bai-Shao (Paeonia lactiflora), Gou-Qi (Lycium barbarum), etc. | AFB1 induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Unknown | [16] |
| Removing Toxic Heat Decoction | Detoxifying and tonifying liver Yin | Ban-Zi-Lian (Sculellaria barbata), Ban-Bian-Lian (Lobelia chinensis Lour.), Mo-Han-Lian (Eclipta prostrata), Gu-Ya (rice sprout), etc. | AFB1 induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Unknown | [16] |
| A-L tonic capsule | Tonifying liver-Yin and nourishing Qi | Nü-Zhen-Zi (Ligustrum lucidum Ait.) and Huang-Qi (Astragalus membranaceous) | DEN induced hepatocarcinogenesis in rats | Inhibit DNA content and improve DNA distribution | Unknown | [17] |
| Bu Shen formula | Tonifying kidney | Ba-Ji-Tian (Morinda officinalis), Tu-Si-Zi (Cuscuta chinensis Lam), Qing-Pi (Cuscuta chinensis Lam) and other herbs | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Unknown | [18] |
| Fu-zheng-hua-yu formula | Strengthening body resistance and dissolving stasis | Dong-Chong-Xia-Cao (Cordyceps sinensis), Tao-Ren (Peach seed), Dan-shen (Salvia miltiorrhiza) and other herbs | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Inhibit cell cycle S phase | [19] |
| Huqi San | Tonifying kidney, nourishing Qi, and dissolving stasis | Hu-Ji-Sheng (Viscum coloratum), Huang-Qi (Astragalus membranaceus), Yu-Jin (Radix Curcumae), Dan-shen (Salvia miltiorrhiza) and other herbs | DEN and 2-acetylaminofluorene induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Down-regulation of c-jun, c-fos and c-myc, up-regulation of G-6-Pase, SDH and ATPase | [20,21] |
| Ganfujian | Strengthening spleen | Shan-Yao (Rhizoma Dioscoreae), Shan-Zha (Fructus Crataegi) and Da-Zao (Fructus Ziziphi Jujubae) | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Down-regulation of CDK4, cyclin D1 and PCNA | [22] |
| SRRS recipe | Strengthening spleen, regulating Qi, removing heat, and softening hard lumps and resolving phlegm | Tai-Zi-Shen (Pseeudostellaria heterophylla), Zhu-Zi-Shen (Panax japonicus), Bai-Zhu (Atractylodes macrocephala Koidz.), Fu-Ling (Poria cocos), Sheng-Mu-Li (raw oyster shell) other herbs | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Unknown | [23] |
| Jianpi Jiedu Recipe | Strengthening spleen and detoxifying | Huang-Qi (Astragalus membranaceous), Bai-Zhu (Atractylodes macrocephala Koidz.), Zhu-Ling (Polyporus umbrellatus), Ba-Yue-Zha (Akebia trifoliata), Shi-Jian-Chuan (Salvia chinensis), Ye-Pu-Tao-Teng (Wild grape stem), Yi-Yi-Ren (Coix lacryma-jobi L.) other herbs | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Down-regulating miR-199a and AKT/PI3K, and up-regulating p70s6k | [24,25] |
| Gan Zheng oral solution | Detoxifying and dissolving stasis | Ban-Zi-Lian (Sculellaria barbata), Bai-Hua-She-She-Cao (Hedyotis diffusa Willd.), San-Leng (Sparganium stoloniferum), E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin) and other herbs | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Down-regulating ICAM-1 | [26] |
| Zao Lian mixture | Detoxifying, dissolving stasis, strengthening spleen, and soothing liver | Zao-Xiu (Paris Polyphylla), Ban-Zi-Lian (Sculellaria barbata), Hu-Zhang (Polygonum cuspidatum), Jiang-Huang (Carcuma longa), Huang-Qi (Astragalus membranaceous), Bai-Zhu (Atractylodes macrocephala Koidz.), Fu-Ling (Poria cocos), etc. | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Improve liver function | [27] |
| Sb/Bs Remedy | Clearing heat and discharging fire, eliminating dampness and detoxifying, and soothing liver | Huang-Qin (Scutellaria baicalensis Georgi) and Chai-Hu (Bupleurum scorzonerifolfium Willd) | N-nitrosobis(2-oxopropyl)amine-induced hepatocellular carcinoma in Syrian hamsters | Inhibit hepatocarcinogenesis | Increase TNF-alpha, TGF-beta1, caspase-3 and apoptosis, decrease 8-OHdG expression | [28] |
| Qing Re Fang | Clearing heat and detoxifying | Ban-Zi-Lian (Sculellaria barbata), Bai-Hua-She-She-Cao (Hedyotis diffusa Willd.) and Pu-Gong-Ying (Taraxacum mongolicum) | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Up-regulate GAP, down-regulate Ras and Raf1 | [29-31] |
| Huo Xue Fang | Promoting circulation and removing stasis | Chai-Hu (Bupleurum chinense), Dan-Shen (Salvia miltiorrhiza), Chi-Shao (Paeonia lactiflora Pall. or P. veitchii Lynch), Ba-Yue-Zha (Caulis Akebiae), Yin-Chen-Hao (Artemisia capillaris Thunb.), Yu-Jin ( Radix Curcumae) | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Up-regulate GAP, down-regulate Ras, Grb-2 and Raf 1 | [29-31] |
| Jian Pi Fang | Strengthening spleen | Huang-Qi (Astragalus membranaceus), Bai-Zhu (Atractylodes macrocephala Koidz.), Bai-Shao (Paeonia lactiflora), Yi-Yi-Ren ( Semen Coicis), Shen-Qu (medicated leaven), Ban-Xia (Pinellia ternata) and Fu-Ling (Poria cocos) | DEN induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Up-regulate GAP, down-regulate Ras and SOS | [29-31] |
| Herbal Compound 861 | Dissolving stasis and tonifying Qi | Dan-Shen (Salvia miltiorrhiza), Huang-Qi (Astragalus membranaceus), Ji-Xue-Teng (Spatholobus suberectus) and other herbs | DEN and 2-acetylaminofluorene induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Unknown | [32] |
| New Anti-tumor formula | Tonifying qi, soothing liver and dissolving stasis | Huang-Qi (Astragalus membranaceus), Chai-Hu (Bupleurum chinense), E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin) and other herbs | AFB1 and HBV induced hepatocarcinogenesis in rats | Inhibit hepatocarcinogenesis | Activate SOD and GST, decrease MDA | [33] |
| Jian-Pi-Huo-Xue Formula | Strengthening spleen and dissolving stasis | Huang Qi (Astragalus membranaceous), Chi-Shao (Paeonia anomala), Dang-Shen (Codonopsis pilosula), Dang-Gui (Angelica sinensis), E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin) and other herbs | Patients with hepatitis, hepatic cirrhosis and low level of AFP | Prevent hepatocarcinogenesis in patients | Unknown | [47] |
TCM syndrome (Zheng) is pathological status that integrates information from clinical symptoms, etiology, disease location and character, tongue picture and TCM theory, and serves as the basis for herbal medication. The clinical manifestation of liver cancer is complex and different patients or different stage of disease may present different TCM syndromes.
In 294 patients preliminarily diagnosed with primary liver cancer, Zhao et al[50] found the early symptoms were more observed in the liver and biliary system and digestive tract system. Except for 23.5% of patients without any TCM syndrome, the frequently observed syndromes include dampness, blood-stasis, Qi-stagnation, Qi-deficiency, blood-deficiency, heat, Yang-asthenia and Yin-asthenia. One hundred and eleven cases presented with single syndrome, 76 cases with two combined syndromes, 31 cases with three combined syndromes, 6 cases with four combined syndromes and 1 case with five combined syndromes[50].
In another study, the common syndromes observed in liver cancer patients include blood stasis, spleen-Qi-deficiency, liver-Qi stagnation, spleen deficiency and dampness blocking, disharmony of liver and stomach, dampness-heat of spleen and stomach, liver-Yin-deficiency and kidney-Yin-deficiency. Liver-Qi stagnation and spleen-Qi-deficiency can be found in patients from stages I to III. Main syndromes in stage II are blood stasis, Qi-stagnation, Qi-deficiency and damp-heat. While in stage III, Qi-deficiency, Yin-deficiency, blood stasis, Qi-stagnation and retention of water are the most common syndromes. The average numbers of syndromes in stages I, II and III are 2.03, 3.47 and 4.99, respectively. These observations suggest that syndromes are more complicated along with disease progression, and Qi stagnation, blood stasis, Qi-deficiency and Yin-deficiency are the basic syndromes in liver cancer[51,52].
In Guangzhou area, Wang et al[53] have found that TCM syndromes distributed in liver cancer patients include spleen deficiency, Qi stagnation, blood stasis and damp-heat. Two overlapped syndromes were observed in 43.5% of patients and 19.9% for three. The overlapped syndromes in patients with stage II disease are spleen deficiency and Qi stagnation, Qi stagnation and blood stasis, spleen deficiency and damp-heat, and liver and spleen deficiency. The overlapped syndrome in patients with stage III disease is liver and kidney-Yin-deficiency[53].
Syndromes are related to prognosis and QOL to some extent. Yang et al[54] analyzed relation between syndrome and survival time. They found that the median survival times in patients with liver-stagnation and spleen-deficiency, Qi stagnation and blood stasis, damp-heat, dampness and blood stasis, liver and kidney-Yin-deficiency were 14.77 mo, 6.13 mo, 5.27 mo, 4.78 mo and 0.80 mo, respectively[54]. Wan et al[55] reported the QOL in patients with sthenia syndrome, such as Qi stagnation, blood stasis and damp-heat, was relatively better than those with asthenia syndrome including Qi-deficiency, Yin-deficiency and blood deficiency[55].
In addition to disease, treatments such as surgery, TACE and high intensity focus ultrasound (HIFU) treatment would influence syndrome pattern. Before surgery, a large proportion of patients presented blood stasis (22.1%) and damp-heat (20.9%). After operation, blood stasis syndrome decreased while spleen deficiency syndrome increased. The most common syndromes in postoperative patients are damp-heat (21.8%) and spleen deficiency (21.0%)[56]. In a tongue picture study, Ye et al[57] reported that the tongues of blood stasis, dampness and Qi-deficiency pattern were commonly observed during the perioperative period of liver cancer, but the tongues of Yin asthenia generating intrinsic heat were increased within 5 d after surgery[57].
TACE is another principal treatment for liver cancer and has been demonstrated to be able to impair Yin, and generate heat and dampness in liver cancer patients[58]. Before interventional treatment, the commonly observed TCM syndromes are liver stagnation, spleen deficiency, damp-heat, blood stasis and Yin-deficiency[59]. After interventional treatment, damp-heat syndrome was increased, and liver stagnation and spleen deficiency decreased. Simultaneous TCM treatment could restore these syndrome changes[60]. In another report, Qi-deficiency and dampness were worsened, while the liver-Qi stagnation and blood stasis were alleviated after TACE. These changes suggest local disease improvement and general impairment[61].
In a systematic observation, Zhang et al[62] reported that the syndromes before TACE treatment were blood stasis (86.8%), excess-heat (68.9%), Qi stagnation (58.5%), Qi-deficiency (58.5%), Yin-deficiency (56.6%), blood deficiency (28.3%), Yang-deficiency (17.0%), and fluid and damp syndrome (14.2%). TACE treatment increased Qi-deficiency and Yang-deficiency syndrome. The syndromes found in post-TACE patients were blood stasis (84.0%), Qi-deficiency (82.1%), excess-heat (80.2%), Qi stagnation (49.1%), Yin-deficiency (46.2%), blood deficiency (39.6%), Yang-deficiency (30.2%), and fluid and damp syndrome (18.9%)[62].
HIFU treatment, an important method for liver cancer therapy, may also affect syndrome distribution. It has been reported that syndromes observed before HIFU treatment are Qi-deficiency, blood deficiency, Yin-deficiency, Qi stagnation, blood stasis and dampness. HIFU treatment could relieve Qi stagnation and blood stasis, and aggravate Qi-deficiency and Yin-deficiency[63].
Contemporary TCM has studied liver cancer syndrome by methods of biomedical science. By using a metabonomics method, Chen et al[64] found that amino acid metabolism, lipid metabolism, glycometabolism and energy metabolism are unbalanced or weak in liver cancer patients with Yang-deficiency. Metabolites, including very-low-density lipoprotein/low-density lipoprotein, isoleucine, lactate, lipids, choline and glucose/sugars, were decreased and may be potential biomarkers for diagnosis of Yang-deficiency syndrome in liver cancer patients[64].
Serum protein is a potential source for syndrome study. By using surface enhanced laser desorption ionization time of flight mass spectrometry, Yang et al[65] found serum proteins with mass-to-charge ratios (M/Z) of 6589 and 4182 Da (dalton) were down-regulated in liver stagnation syndrome, that with an M/Z of 5710 Da was down-regulated in damp-heat syndrome, that with an M/Z of 6992 Da was down-regulated in Yin-deficiency syndrome, while those with M/Z of 5816 Da and 4297 Da were up-regulated in spleen deficiency and blood stasis syndrome, respectively[65]. Huang et al[66] reported that proteins with M/Z of 8576 Da (cytochrome C6) and 8780 Da (cytochrome c oxidase assembly factor 5) were over-expressed in serum from patients with liver stagnation syndrome[66].
By means of GeneChip, Weng et al[67] reported that 615 mRNAs were differentially expressed in peripheral blood mononuclear cells from liver cancer patients with liver-kidney Yin-deficiency syndrome. These genes are related to GO (gene ontology) of anti-apoptosis, regulation of cell cycle and transmembrane transport, and 26 kyoto encyclopedia of genes and genomes pathways. Among these genes, SEC62 [SEC62 homolog (S. cerevisiae)], cyclin B1 and baculoviral IAP repeat containing 3 (BIRC3) were significantly down-regulated in patients with syndrome of liver-kidney Yin-deficiency compard with those without[67].
TCM syndrome is closely associated with the stage of disease. Su et al[68,69] explored the relationship between syndrome differentiation and metastasis potential of hepatocarcinoma cells. The percentage of metastasis in patients was ranked from high to low as follows: liver and kidney-Yin-deficiency, Qi stagnation and blood stasis, damp-heat, and liver stagnation and spleen deficiency, and was related to up-regulation of β-catenin and down-regulation of E-cadherin and matrix metalloproteinase-2 (MMP2)/tissue inhibitor of metalloproteinase-2[68,69].
In addition to clinical studies, it has been confirmed that mouse models can be used for syndrome exploration[70]. Pan et al[71] studied gene expression in the adrenal glands of H22 liver cancer bearing mice. In toxicity accumulation and Qi-deficiency syndrome (early stage), xanthine dehydrogenase and other 18 genes were up-regulated, while eukaryotic translation elongation factor 1 alpha 2 and other 8 genes were down-regulated. In Yang-Qi-deficiency syndrome (middle stage), enolase 3 (beta muscle) and other 11 genes were up-regulated, while solute carrier family 32 (GABA vesicular transporter) and other 10 genes were down-regulated. In Qi-Yin-Yang-deficiency syndrome (advanced stage), albumin and other 29 genes were up-regulated, while ATPase, Na+/K+ transporting, beta 2 polypeptide and other 5 genes were down-regulated. S100 calcium binding protein A8 (calgranulin A) and other 11 genes were gradually up-regulated from early stage to advanced stage[71].
TCM has been widely used for liver cancer treatment in combination with surgery, TACE, radiofrequency ablation (RFA), microwave ablation (MWA), HIFU and target therapy, or as monotherapy for disease control and/or alleviating symptoms. TCM have been demonstrated to be effective to inhibit tumor growth, prolong survival time, ameliorate symptoms, and improve QOL and immune function in hepatocarcinoma patients (Table 2). Related studies will further improve clinical efficacy of TCM and benefit more to hepatocarcinoma patients.
| Treatments | TCM therapeutic principles | Herbs/herbl formula | Disease | No. of patients | Effects | Ref. |
| Surgery, Jiedu Granule and Cinobufacini Injection | Detoxifying and dissipating mass | Jiedu Granule: Shi-Jian-Chuan (Salvia chinensis), Mao-Ren-Shen (Actinidia valvata), Yi-Yi-Ren (Semen Coicis), Shan-Zha (Fructus Crataegi), Shen-Qu (Massa Medicata Fermentata), etc. | Hepatocellular carcinoma after surgical resection | 120 | Postpone tumor recurrence and metastasis, prolong survival time | [72] |
| Surgery, Ruanjianhugan Tablets | Detoxifying, dispersing stasis, tonifying Qi and Yin | Ku-Shen (Sophora flavescens Ait.), Xia-Ku-Cao (Prunella), Hu-Zhang (Polygonum cuspidatum), Nü-Zhen-Zi (Ligustrum lucidum Ait), Huang-Qi (Astragalus membranaceus), etc. | Small hepatocellular carcinoma after surgical resection | 399 | Prolong overall survival time | [73] |
| Surgery, Jiedu Xiaozheng Yin and Fuzheng Yiliu Recipe | Detoxifying and dissipating mass, tonifying Qi and Yin | Jiedu Xiaozheng Yin: Bai-Hua-She-She-Cao (Hedyotis diffusa Willd), Shan-Ci-Gu (Pseudobulbus Cremastrae), Ku-Shen (Sophora flavescens Ait.), et al. Fuzheng Yiliu Recipe: Huang-Qi (Astragalus membranaceus), Nü-Zhen-Zi (Ligustrum lucidum Ait), Shan-Yao (Dioscorea opposita), etc. | Stage III hepatocarcinoma before and after surgical resection | 72 | Prolong survival time and prevent recurrence | [74] |
| JDF Granule and TACE | Detoxifying and dispersing stasis | Mao-Ren-Shen (Actinidia valvata), Shi-Jian-Chuan (Salvia chinensis), Shan-Ci-Gu (Pseudobulbus Cremastrae), Ji-Nei-Jin (gizzard membrane of Gallus gallus domesticus) | Unresectable hepatocellular carcinoma | 165 | Prolong survival time | [75] |
| Shentao Ruangan Pill and TACE | Detoxifying, dispersing stasis, tonifying Qi and Yang | Yin-Chen-Hao (Artemisia capillaris Thunb.), Bai-Hua-She-She-Cao (Hedyotis diffusa Willd.), Ban-Zi-Lian (Sculellaria barbata), E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin), Ren-Shen (Panax ginseng), etc. | Middle-advanced stage large hepatocarcinoma | 85 | Prolong survival time | [76] |
| Ganai No. I and No. II and TACE | Tonifying Qi and Yin, detoxifying and dissipating mass | Ganai No.I: Dang-Shen (Codonopsis pilosula), Huang Qi (Astragalus membranaceous), Nü-Zhen-Zi (Ligustrum lucidum Ait), E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin), Bai-Hua-She-She-Cao (Hedyotis diffusa Willd.), etc. Ganai No. II: Xue-Jie (Daemonorops draco BL.), Ru-Xiang (Boswellia carterii Birdw), Mo-Yao (Commiphpra myrrha Engl.), Zao-Xiu ( Sm.), Long-Kui (Solanum nigrum L.), etc. | Middle-advanced stage liver cancer | 60 | Prolong survival time, prevent recurrence and alleviate HACE induce leukocytopenia | [77] |
| Jinlong Capsule and TACE or RFA | Detoxifying and dissipating mass | Tian-Long (Gecko), Jin-Qin-Bai-Hua-She (Multibanded krait), Qi-She (Long-nosed pit viper) | Unresectable hepatocarcinoma | 98, 76 | Enhance short-term effect of TACE and improve quality of life; enhance RFA effects, reduce RFA induced liver injury, improve QOL and immune function | [78,89] |
| Syndrome differentiation based TCM therapy and TACE | Syndrome differentiation based TCM therapy | Xiao-Yao-San/Chai-Hu-Shu-Gan-San, Hua-Yu-Xiao-Liu-Tang, Long-Dan-Xie-Gan-Tang, Yi-Guan-Jian + Liu-Wei-Di-Huang-Wan | Middle-advanced stage hepatocarcinoma | 67 | Enhance short-term efficacy and reduce adverse effect of TACE, improve immune function and QOL | [79] |
| Shelian Capsule and TACE | Detoxifying, dissipating mass, tonifying Qi | Bai-Hua-She-She-Cao (Hedyotis diffusa Willd.), Ban-Zi-Lian (Sculellaria barbata), Hu-Zhang (Polygonum cuspidatum), Dan-shen (Salvia miltiorrhiza Bge.), Ren-Shen (Panax ginseng), etc. | Early middle and advanced stage hepatocarcinoma | 120 | Enhance short-term efficacy of TACE, improve immune function and QOL | [80] |
| Matrine Injection and TACE | Clearing heat and detoxifying | Matrine, etc. | Hepatocarcinoma after TACE | 122 | Protect liver function | [81] |
| Jia Wei Si Jun Zi Tang and TACE | Tonifying spleen, nourishing Qi, soothing liver-Qi stagnation, and dissolving stasis | Dang-Shen (Codonopsis pilosula), Bai-Zhu (Atractylodes macrocephala Koidz.), Huang Qi (Astragalus membranaceous), Fo-Shou (Citrus medica L. var. sarcodactylis), Dan-shen (Salvia miltiorrhiza Bge.), etc. | Advance stage of liver cancer | 65 | Protect liver function | [82] |
| Vascular Embolizing Agent | Vascular embolizing | Yu-Jin (Curcuma aromatic), Bai-Ji (Bletilla striata) | Stage II and III hepatocarcinoma (Yu-Jin), stage I-III hepatocarcinoma (Bai-Ji) | 32 (Yu-Jin), 106 (Bai-Ji), 56 (Bai-Ji) | Vascular embolizing agent | [83-85] |
| Aidi Injection and RFA or MWA | Dissipating mass, tonifying Qi and Yin | Ban-Mao (Mylabris), Huang Qi (Astragalus membranaceous), etc. | Middle-late stage hepatocarcinoma, stage II and III hepatocarcinoma | 89, 61 | Relieve the impairment of cool-tip radiofrequency ablation on hepatic function, improve immune function and reduce relapse; elevate MWA efficacy, improve QOL, immune and liver function | [86,92] |
| Xiaoaiping Injection and RFA | Dissolving stasis | Xiaoaiping injection | Middle-late stage hepatocarcinoma, advanced hepatocarcinoma | 31, 68 | Enhance RFA effects and reduce non-bacterial inflammatory response; inhibit tumor growth, improve QOL and immune function, increase progression-free survival | [87,99] |
| Tianzhicao Capsule and RFA | Detoxifying, dissolving stasis, tonifying Qi and Yin | Ban-Zi-Lian (Sculellaria barbata), Dan-shen (Salvia miltiorrhiza Bge.), Huang Qi (Astragalus membranaceous), Gou-Qi (Lycium barbarum), etc. | Small hepatocarcinoma | 90 | Improve QOL and immune function, prolong survival time | [88] |
| Fuzheng Yiliu Recipe and MWA | Huang Qi (Astragalus membranaceous), Ling-Zhi (Ganoderma lucidum), Nü-Zhen-Zi (Ligustrum lucidum Ait.), etc. | Middle-advanced stage hepatocarcinoma | 60 | Enhance MWA efficacy, improve immune and liver function | [90] | |
| Shenqi Mixture and MWA | Tonifying Qi | Ren-Shen (Panax ginseng), etc. | Stage II and III hepatocarcinoma | 72 | Enhance MWA efficacy, prolong survival time, improve QOL and immune function and relieve symptoms | [91] |
| Qiankun Capsule and HIFU | Tonifying spleen, detoxifying, and dissipating mass | Tai-Zi-Shen (Pseeudostellaria heterophylla), Bai-Zhu (Atractylodes macrocephala Koidz.), Bai-Shao (Paeonia lactiflora), Xia-Ku-Cao (Prunella), Ban-Zi-Lian (Sculellaria barbata), etc. | Stage II and III hepatocarcinoma | 60 | Enhance therapeutic effects and improve immune function | [93] |
| Fu-Zhen-Yang-Yin Formula and HIFU | Tonifying Qi and Yin, detoxifying, and dissipating mass | Huang Qi (Astragalus membranaceous), Tai-Zi-Shen (Pseeudostellaria heterophylla), Yin-Chen-Hao (Artemisia capillaris Thunb.), Bai-Hua-She-She-Cao (Hedyotis diffusa Willd.), Hu-Zhang (Polygonum cuspidatum), etc. | Advanced stage hepatocarcinoma | 60 | Alleviate HIFU induced fever and liver function damage | [94] |
| Syndrome Differentiation Based TCM Therapy and Sorafenib | Syndrome differentiation based TCM therapy | Huang Qi (Astragalus membranaceous), Shan-Yao (Dioscorea opposita), Long-Kui (Solanum nigrum L.), Bai-Shao (Paeonia lactiflora), etc. | Advanced stage hepatocarcinoma | 18 | Enhance therapeutic efficacy of sorafenib and prolong survival time | [95] |
| Cinobufagin tablet and Sorafenib | Dissipating mass | Cinobufagin, etc. | Middle-advanced stage hepatocarcinoma | 59 | Enhance effects of sorafenib, improve QOL and liver function and relieve pain | [96] |
| Oleum fructus bruceas intervention, oral intake of Ganji Decoction and external application of Ailitong | Tonifying spleen, soothing liver-Qi stagnation, detoxifying, dissipating mass | Dang-Shen (Codonopsis pilosula), Chai-Hu (Bupleurum scorzonerifolfium Willd), Bai-Shao (Paeonia lactiflora), Tu-Bie-Chong (Eupolyphaga gasinensis Walk.), Bai-Hua-She-She-Cao (Hedyotis diffusa Willd.), etc. | Middle-advanced stage hepatocarcinoma | 97 | Prolong survival time, improve QOL and relieve pain | [97] |
| Hepatic artery perfusion/embolization with turmeric oil microballoon, cinobufotalin and Aidi injection, and Syndrome Differentiation Based TCM Therapy | Tonifying Qi and Yin, and dissipating mass | Yu-Jin (Curcuma aromatic), cinobufotalin, Ban-Mao (Mylabris), Huang Qi (Astragalus membranaceous), etc. | Stage I to III hepatocarcinoma | 41 | Inhibit tumor growth with fewer adverse reactions, and ameliorate fatigue and anorexia | [98] |
| Cinobufacini Injection | Dissipating masses | Cinobufagin, etc. | Middle-advanced stage hepatocarcinoma | 100 | Inhibiting tumor growth, protecting liver function and prolonging survival time | [100] |
| Norcantharidin and herbal decoction | Tonifying spleen and Qi, and dissolving stasis | Huang Qi (Astragalus membranaceous), Yin-Chen-Hao (Artemisia capillaris Thunb.), Hu-Zhang (Polygonum cuspidatum), Fu-Ling (Poria cocos), Tian-Long (Gecko), etc. | Elderly patients with late stage hepatocarcinoma | 79 | Inhibit tumor growth, prolong survival time and improve QOL | [101] |
| Jianpi Fuzheng Decoction | Tonifying Qi and Yin | Huang Qi (Astragalus membranaceous), Yi-Yi-Ren (Coix lacryma-jobi L.), Dang-Shen (Codonopsis pilosula), Bai-Zhu (Atractylodes macrocephala Koidz.), Nü-Zhen-Zi (Ligustrum lucidum Ait), etc. | Late stage hepatocarcinoma | 60 | Ameliorate TCM syndrome, improve QOL and immune function and prolong survival time | [102] |
| Jianpi Yiliu Decoction | Tonifying spleen and Qi, detoxifying, and dissolving stasis | Huang Qi (Astragalus membranaceous), Dang-Shen (Codonopsis pilosula), Bai-Zhu (Atractylodes macrocephala Koidz.), Ban-Zi-Lian (Sculellaria barbata), Yu-Jin (Curcuma aromatic), etc. | Late stage hepatocarcinoma | 30 | Ameliorate symptoms, improve QOL and protect liver function | [102] |
| Jiawei Yiguanjian | Tonifying Yin, clearing heat and draining dampness | Bei-Sha-Shen (Glehnia littoralis), Mai-Dong (Ophiopogon japonicus), Dang-Gui (Angelica sinensis), Gou-Qi (Lycium barbarum), Chui-Pen-Cao (Sedum sarmentosum Bunge), etc. | Late stage hepatocarcinoma | 100 | Prolong survival time, ameliorate TCM syndrome, and improve QOL and immune function | [104] |
Surgery is one of the most important treatments for hepatocarcinoma. TCM has been proved potent to prevent recurrence and metastasis after the surgery. Treatment with Jiedu Granule and Cinobufacini injection may postpone tumor recurrence and metastasis, and prolong survival time in postoperative patients with hepatocarcinoma[72]. Long-term use of Ruanjianhugan tablets could prolong overall survival time in postoperative patients with small hepatocarcinoma[73]. Treatment with Jiedu xiaozheng yin for 7 d before surgery and Fuzheng yiliu recipe after operation for 2 years are effective to prolong survival time and prevent recurrence in patients with stage III hepatocarcinoma[74].
TACE is the principle treatment for unresectable hepatocarcinoma. TCM has been used to improve efficacy of TACE. JDF granule preparation, a traditional Chinese herbal formula, combined with TACE may prolong survival time in patients with unresectable hepatocellular carcinoma[75]. Shentao Ruangan pill based herbal therapy in combination with TACE could prolong survival time in patients with middle-advanced stage liver cancer[76]. Ganai No. I and No. II in combination with hepatic artery chemoembolization (HACE) have been reported effectively to prolong survival time, prevent recurrence and alleviate HACE induced leukocytopenia in patients with middle-advanced stage hepatocarcinoma[77].
Jinlong Capsule may enhance short-term effect of TACE and improve QOL in patients with unresectable hepatocarcinoma[78]. Syndrome differentiation based TCM therapy could enhance short-term efficacy and reduce adverse effect of TACE, improve immune function and QOL in liver cancer patients[79]. Shelian Capsule, a Chinese patent drug, was reported to effectively enhance short-term efficacy of TACE, improve immune function and QOL in liver cancer patients[80]. Matrine injection and “jia wei si jun zi tang” have been proved effective to protect liver function in liver cancer patients receiving TACE treatment[81,82].
In addition to oral and intravenous administration, some Chinese herbs, such as curcuma aromatic and Bletilla striata, have been demonstrated to be able to be used as vascular embolizing agents for TACE in liver cancer patients[83-85].
RFA is another widely used treatment for hepatocarcinoma. Aidi injection, an herbal injection, has been reported to effectively relieve hepatic function impairment caused by cool-tip RFA, improve immune function and reduce relapse rate in patients with liver cancer[86]. Xiaoaiping injection, an herbal extract injection, could enhance RFA effects and reduce non-bacterial inflammatory response post RFA[87]. Tianzhicao capsule in combination with RFA may improve QOL and immune function, prolong survival time in patients with hepatocellular carcinoma[88]. Jinlong capsule has been demonstrated to enhance RFA effects, reduce RFA induced liver injury, improve QOL and immune function in liver cancer patients[89].
In combination with MWA, Fuzheng Yiliu Recipe could enhance MWA efficacy, improve immune and liver function in liver cancer patients[90]. Shenqi mixture has been showed to be effective to enhance MWA efficacy, prolong survival time, improve QOL and immune function and relieve symptoms in patients with hepatocarcinoma[91]. Aidi injection is able to elevate MWA efficacy and improve QOL, immune and liver function in hepatocarcinoma patients[92].
HIFU has become an important treatment method for hepatocarcinoma. In combination with HIFU, Qiankun capsule can enhance therapeutic effects and improve immune function in patients with hepatocarcinoma[93]. Fu-Zhen-Yang-Yin formula could alleviate HIFU induced fever and liver function damage[94].
Sorafenib is a target agent for liver cancer treatment. Syndrome differentiation based TCM therapy could enhance therapeutic efficacy of sorafenib and prolong survival time in patients with advanced hepatocarcinoma[95]. Cinobufagin tablet has been confirmed to enhance effects of sorafenib, improve QOL and liver function and relieve pain in liver cancer patients[96].
In addition to intravenous administration, herbal extract injection also can be used as a perfusion/embolization reagent instead of chemotherapeutic drug. Tian et al[97] reported that a Chinese medicine comprehensive therapy, i.e., Oleum fructus bruceas intervention combined with oral intake of Ganji Decoction and external application of Ailitong, is safe and effective to prolong survival time, improve QOL and relieve pain compared with conventional TACE in liver cancer patients[97]. Xu et al[98] has demonstrated that hepatic artery perfusion/embolization with turmeric oil microballoon, cinobufotalin and Aidi injection is effective with fewer adverse reactions compared with conventional TACE, and could significantly ameliorate fatigue and anorexia in patients with hepatocarcinoma[98].
Chinese patent herbal drugs have been approved as effective treatments for hepatocarcinoma. Xiaoaiping injection is effective to inhibit tumor growth, improve QOL and immune function, increase progression-free survival compared with best supportive treatment in patients with advanced hepatocarcinoma[99]. Cinobufacini injection has been demonstrated to be effective in inhibiting tumor growth, protecting liver function and prolonging survival time in patients with moderate and advanced hepatocarcinoma[100]. Norcantharidin in combination with herbal decoction treatment can inhibit tumor growth, prolong survival time and improve QOL in elderly patients with late stage liver cancer[101].
Herbal decoction is the principle TCM treatment for liver cancer. Jianpi Fuzheng decoction, an herbal formula for tonifying spleen and strengthening body defense, is effective in ameliorating TCM syndrome, improving QOL and immune function and prolonging survival time in patients with advanced liver cancer[102]. Jianpi Yiliu decoction, a formula for tonifying spleen and inhibiting tumor, has been reported to effectively ameliorate symptoms, improve QOL and protect liver function in patients with late stage hepatocarcinoma[103]. Jiawei Yiguanjian, a modified classical herbal formula, has been shown to be effective to prolong survival time, ameliorate TCM syndrome, and improve QOL and immune function in patients with advanced hepatocellular carcinoma[104].
The effects of Chinese herbs against hepatocarcinoma have been extensively studied, and it has been demonstrated that Chinese herbs are effective to induce apoptosis, autophagy, anoikis and cell senescence, arrest cell cycle, regulate immune function, inhibit metastasis and angiogenesis, reverse drug resistance and enhance effects of chemotherapy. Anti-cancer effects of herbal formulas against hepatocarcinoma are listed in Table 3.
| Herbal formula | Therapeutic principles | Herbs | Models | Effects | Targets/events | Ref. |
| Fuzheng Yiliu Granule | Tonifying Qi and blood, and dissolving stasis | Hong-Qi (Hedysarum polybotrys), Dang-Gui (Angelica sinensis), Mu-Tou-Hui (Patrinia scabra Bunge), etc. | Mouse H22 hepatocarcinoma bearing mice | Inhibit tumor growth, induce apoptosis | p53, caspase-3, mitochondrial membrane potential | [126,127] |
| Fuganchun 6 | Tonifying Qi and Yin, detoxifying and dissipating mass | Huang-Qi (Astragalus membranaceus), Nü-Zhen-Zi (Ligustrum lucidum Ait), Bai-Hua-She-She-Cao (Hedyotis diffusa Willd), Bie-Jia (Carapax trionycis), E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin), etc. | Mouse H22 hepatocarcinoma cells in vitro and in vivo | Inhibite tumor growth and cell proliferation, and induce apoptosis | Enhance proliferation activity of lymphocyte, NK cells activities and IL-2 production | [128,178] |
| Bushen Jianpi Decoction | Tonifying spleen and kidney | Dang-Shen ( ), Bai-Zhu (Atractylodes macrocephala Koidz.), Fu-Ling (Poria cocos), Shu-Di-Huang (Rehmannia glutinosa), shan-Zhu-Yu (Cornus officinalis), Du-Zhong (Eucommia ulmoides Oliver), etc. | Mouse H22 hepatocarcinoma bearing mice | Inhibit tumor growth, induce apoptosis | VEGF | [129] |
| Warming Yang and Dispersing Stasis Formula | Warming Yang and dispersing stasis | Fu-Zi (Aconitum carmichaeli Debx.), Huang-Qi (Astragalus membranaceus), Bai-Zhu (Atractylodes macrocephala Koidz.), E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin), Bai-Shao (Paeonia lactiflora), etc. | Human BEL-7402 hepatocarcinoma cells | Induce apoptosis | Unknown | [130] |
| Fufangkushen injection | Clearing heat and removing toxicity | Ku-Shen (Sophora flavescens Ait.), etc. | Human SMMC-7721 hepatocarcinoma cells | Inhibit proliferation, induce apoptosis | Survivin, Bcl-2, caspase-3 | [131] |
| Songyou Yin | Tonifying Qi and blood, dissolving stasis and dissipating mass | Dan-shen (Salvia miltiorrhiza Bge.), Huang-Qi (Astragalus membranaceus Bge.), Gou-Qi (Lycium barbarum L.), Shan-Zha (Crataegus pinnatifida Bge.), and Bie-Jia (Trionyx sinensis Wiegmann) | Human MHCC97H hepatocarcinoma bearing nude mice; activated rat hepatic stellate cells and rat McA-RH7777 hepatoma cells | Induce apoptosis, inhibit tumor growth, prolong survival; inhibit invasion and metastasis | MMP-2, IL-6, TGF-β1, VEGF, epithelial-mesenchymal transition | [132,167] |
| Huang-lian-jie-du-tang | Clearing heat and removing toxicity | Huang-Lian (C. chinensis Franch), Huang-Qin (Scutellaria baicalensis Georgi), Huang-Bai (P. amurense Rupr) and Zhi-Zi (Gardenia jasminoides Ellis) | Human Hep G2 and PLC/PRF/5 hepatomain cells in vitro and in vivo | Inhibit cell proliferation, induce cell cycle arrest and apoptosis | Cdc2, Cdc25C, cyclin A, cyclin B1, Cdc2, Cdc25C, Bax, Bak, Bcl-2, Bcl-XL, IkappaBalpha | [141] |
| Bu-Zhong-Yi-Qi-Tang | Invigorating spleen-stomach and replenishing qi | Huang-QI (Astragalus membranaceus), Ren-Shen (Panax ginseng), Gang-Gui (Angelicae sinensis), Sheng-Ma (Cimicifuga foetida L.), Gan-Cao (Glycyrrhiza uralensis), Chen-Pi (Citrus poonensis), Chai-Hu (Bupleurum chinensis), Sheng-Jiang (Zingiber officinale), Da-zhao (Ziziphs jujuba), Bai-Shu (Atractylodes macrocephala KOIDZUMI) | Human hepatoma Hep3B, HepG2 and HA22T cells | Inhibit cell proliferation, induce apoptosis and arrest cell cycle at G0/G1 phase | Unknown | [142] |
| Jiedu Xiaozheng Yin | Heat-clearing and detoxification | Bai-Hua-She-She-Cao (Hedyotis diffusa Willd), Xia-Ku-Cao (Prunella), Shan-Ci-Gu (Pseudobulbus Cremastrae), Ku-Shen (Sophora flavescens) | Human Hep G2 hepatoma cell in vitro and in vivo | Inhibits the growth of HepG2 cells, arrest cell cycle at the G0/G1 phase | Cyclin D and cyclin E | [143] |
| Liver Yin Tonifying formula | Tonifying liver-Yin, draining dampness and dissipating stasis | Nü-Zhen-Zi (Ligustrum lucidum Ait), Zhi-Bie-Jia (processed Carapax trionycis) and Hu-Zhang (Polygonum cuspidatum) | Human hepatocarcinoma Bel-7402 cells | Inhibit proliferation, induce apoptosis and cell senescence | Caspases-8, -9 and -3, p16, p21, pRB | [152] |
| Modified Yi Guan Jian | Tonifying liver and kidney-Yin, draining dampness and dissipating stasis | Bei-Sha-Shen (Glehnia littoralis), Mai-Dong (Ophiopogon japonicus), Dang-Gui (Angelica sinensis), Shu-Di (dried Rehmannia glutinosa), Gou-Qi (Lycium barbarum), Chuan-Lian-Zi (Melia toosendan Sieb fruit), and Hu-Zhang (Polygonum cuspidatum) | Human hepatocarcinoma Bel-7402 cells | Inhibit proliferation, induce anoikis | Caspases-3, -8 and -9, p38 MAPK | [156] |
| Blejiajian Pill | Tonifying Qi, detoxifying and dissipating mass | Bie-Jia-Jiao(Carapacis trionycis-shell glue), E-Jiao(Colla Corii Asini), Feng-Fang (beehives), Chai-Hu (Bupleurum chinense), Huang-Qin (Scutellaria baicalensis), Ban-Xia (Pinellia ternate), Dang-Shen(Codonopsis pilosula), etc. | Human Hep G2 hepatoma cells | Inhibit cell proliferation, adhesion and invasion | Unknown | [168] |
| Compound Astragalus and Salvia miltiorrhiza extract | Tonifying Qi and dissipating stasis | Astragalosides, astragalus polysaccharide and salvianolic acids | Human Hep G2 hepatoma cells | Inhibit TGF-β1 mediated invasion | TGF-β/Smad signaling | [169] |
| Shehuang Xiaoliu Fang | Tonifying spleen, dissolving stasis and detoxifying | She-Xiang (musk), Niu-Huang (Cow-Bezoar), Dan-shen (Salvia miltiorrhiza Bge.), Bai-Zhu (Atractylodes macrocephala Koidz.), Ban-Zi-Lian (Sculellaria barbata), E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin), etc. | Human SMMC-7721 hepatocarcinoma cells | Inhibit invasive and adhesive | nm23-h1 and ICAM-1 | [170] |
| Xiaochaihu Decoction | Relief liver for smooth Qi | Chai-Hu (Bupleurum chinense), Huang-Qin (Scutellaria baicalensis Georgi), Sheng-Jiang (Zingiber officinale), Ban-Xia (Pinellia ternata), Da-Zao (Ziziphus jujuba), Ren-Shen (Panax ginseng), Gan-cao (Glycyrrhiza uralensis) | Mouse H22 hepatocarcinoma bearing mice | Inhibit tumor growth | Increase T lymphocytes proliferation, NK cells activities and IL-2 | [175] |
| Mylabris Mixture | Detoxifying and dissipating mass | Ban-Mao (Mylabris), Chen-Pi (Citrus reticulata Blanco), Gu-Ya (Setaria italica), etc. | Mouse H22 hepatocarcinoma bearing mice | Inhibit tumor growth | Increase CD4+, CD8+ lymphocytes and NK cells, and IFN-γ and IL-4 production | [176] |
| Fuzheng Yiliu Granule-2 | Tonifying Qi and tonifying Yin | Huang-Qi (Astragalus membranaceus), Nü-Zhen-Zi (Ligustrum lucidum Ait), Ling-Zhi (Ganoderma lucidum), and Shan-Yao (Dioscorea opposita) | Mouse H22 hepatocarcinoma cells in vitro and in vivo | Inhibite tumor growth and cell proliferation, and induce apoptosis | Increase CD4+ lymphocyte, IL-2 and TNF-α, and NK cells | [177] |
| Fu-Zheng-Kang-Ai-Tang | Strengthening body resistance and anti-cancer | Ren-Shen (Panax ginseng), Huang-Qin (Scutellaria baicalensis Georgi), Ling-Zhi (Ganoderma lucidum), Huang-Qi (Astragalus membranaceus), etc. | Human Bel-7402 hepatocarcinoma bearing nude mice | Inhibit angiogenesis and tumor growth | VEGF and bFGF | [188] |
| Delisheng | Tonifying Qi and resolving masses | Ren-Shen (Panax ginseng), Huang-Qi (Astragalus membranaceus), Cantharidium, etc. | Human Hep G2 hepatoma cells | Inhibit tumor growth | Endostatin | [189] |
| QHF | Detoxifying, dissolving stasis and strengthening body resistance | Cinobufagin, Ginsenoside Rg3, Panax Notoginseng Saponins, lentinan | Mouse H22 hepatocarcinoma bearing mice | Inhibit angiogenesis and tumor growth, enhance anti-cancer effects DDP | VEGF, EGFR and MMP-2 | [190,196] |
| Erbie San | Resolving masses | Bie-Jia (Carapax trionycis), etc. | Wistar rats bearing Walker-256 liver cancer | Inhibit tumor growth | VEGF and endostatin | [191] |
| Chaiqiyigan Granula | Tonifying spleen, soothing liver, dissolving stasis and detoxifying | Chai-Hu (Bupleurum chinense), Huang-Qi (Astragalus membranaceus), etc. | Human hepG2/EGFP hepatoma bearing nude mice | Enhance anti-cancer effects of Taxol | Bax, p53 and VEGF | [195] |
| Shengmai Injection | Tonifying Qi and Yin | Ren-Shen (Panax ginseng), Mai-Dong (Ophiopogon japonicus), etc. | Mouse H22 hepatocarcinoma bearing mice | Enhance anti-tumor efficacy and reduce toxicity of 5-Fu | Unknown | [197] |
Apoptosis is one of the most frequently studied filed for elucidating effective mechanism of herbs against hepatocarcinoma. Ren-Shen (Panax ginseng) is a commonly used Qi-tonifying herb. 20(R)-ginsenoside Rg3, a component from Panax ginseng, may up-regulate TNF-α and induce apoptosis in induced liver tumors in SD rats[105]. Blood tonifying herb or component, including Di-Huang (Rehmannia glutinosa) and N-butylidenephthalide from Dang-Gui (Angelica sinensis), is effective to induce apoptosis of hepatocarcinoma cells[106,107]. Gou-Qi (Lycium barbarum), a liver-Yin tonifying herb, is effective to inhibit proliferation and stimulate p53-mediated apoptosis in liver cancer cells[106]. Icariin, an ingredient from Yang tonifying herb Yin-Yang-Huo (Epimedium brevicornum Maxim.), may generate reactive oxygen species (ROS) and up-regulate JNK (c-Jun N-terminal kinase) phosphorylation and B-cell lymphoma 2/Bcl2-associated X protein (Bax/Bcl-2) to induce intrinsic apoptosis in liver cancer cells[108].
Clearing heat and detoxifying herbs are one of the most commonly medicated herbs for liver cancer treatment. Solamargine purified from Long-Kui (Solanum incanum) may up-regulate TNF receptor type I and induce apoptosis in Hep3B cells[109]. Components from Mao-Ren-Shen (Actinidia valvata) may arrested cell cycle at G0/G1 phase and induce apoptosis in H22 cells[110]. Ban-Zi-Lian (Scutellariae barbata) is effective in up-regulating Bax/Bcl-2, arresting cell cycle at G2/M phase and inducing apoptosis in hepatocellular carcinoma cells[111]. Ba-Qia (Smilax glabra Roxb.) extract could activate p38, JNK and extracellular signal-regulated kinase (ERK) to induce intrinsic apoptosis in liver cancer cells[112]. Essential oil of Qing-Hao (Artemisia annul L.) could induce apoptosis in SMMC-7721 cells[113].
Clearing heat and draining dampness herbs are used for damp-heat in the liver and gallbladder. Chui-Pen-Cao (Sedum sarmentosum Bunge) can inhibit HepG2 cell growth and induce apoptosis accompanied by down-regulation of Bcl-2, VEGF and phosphorylated signal transducers and activators of transcription (p-STAT3)[114]. Resveratrol-4-O-D-(2’-galloyl)-glucopyranoside from Hu-Zhang (Polygonum cuspidatum) may activate caspases 3 and 9 to induce apoptosis in hepatocellular carcinoma via the JNK and ERK pathway[115]. Yin-Chen-Hao (Artemisia capillaris Thunb.) is effective to induce apoptosis and G0/G1 cell cycle arrest in SMMC-7721 cells[116].
Dispersing blood stasis is another important principle for liver cancer therapy. Dan-Shen (Salvia miltiorrhiza) was reported to effectively inhibit proliferation and induce apoptosis in HepG2 cells coincided with depletion of intracellular glutathione and reduction of mitochondrial membrane potential[117]. Chi-Shao (Paeoniae Radix) could inhibit cell growth and induce p53 independent apoptosis coincided with up-regulation Bcl-2/adenovirus E1B 19 kD-interacting protein 3 and down-regulation of ZK1, RAD23 homologue B and heat shock 60 kDa protein 1[118]. Curcumin is a component of Yu-Jin/Jiang-Huang/E-Zhu (Curcuma kwangsiensis or Curcuma phaeocaulis or Curcuma wenyujin or Curcuma longa). Resveratrol is a compound that can be isolated from Hu-Zhang (Polygonum cuspidatum) or other plants. We have found that curcumin combined with resveratrol may synergistically inhibit X-linked inhibitor of apoptosis protein (XIAP) and survivin expression, up-regulate ROS production, activate caspases-3, -8 and -9 to induce apoptosis in liver cancer cells[119].
Although the TCM pathological factor of phlegm is not directly related to hepatocarcinogenesis, reducing phlegm and/or resolving masses herbs are frequently medicated as anti-cancer herbs in liver cancer. Ban-Xia (Pinellia ternate) can inhibit cell proliferation, up-regulate Bax/Bcl-2 and induce apoptosis in Bel-7402 cells[120]. Tian-Nan-Xing (Arisaema heterophyllum) may activate caspase-3 and induce apoptosis in hepatocarcinoma cells[121]. Tubeimoside I, an ingredient from Tu-Bei-Mu (Bolbostemma paniculatum), could up-regulate Bax/Bcl-2 and induce intrinsic apoptosis in hepatoma cells[122]. Toxic Chinese herb or components such as Quan-Xie (scorpio), Norcantharidin and polypeptides from bee venom are potent to induce apoptosis in liver cancer cells[123-125].
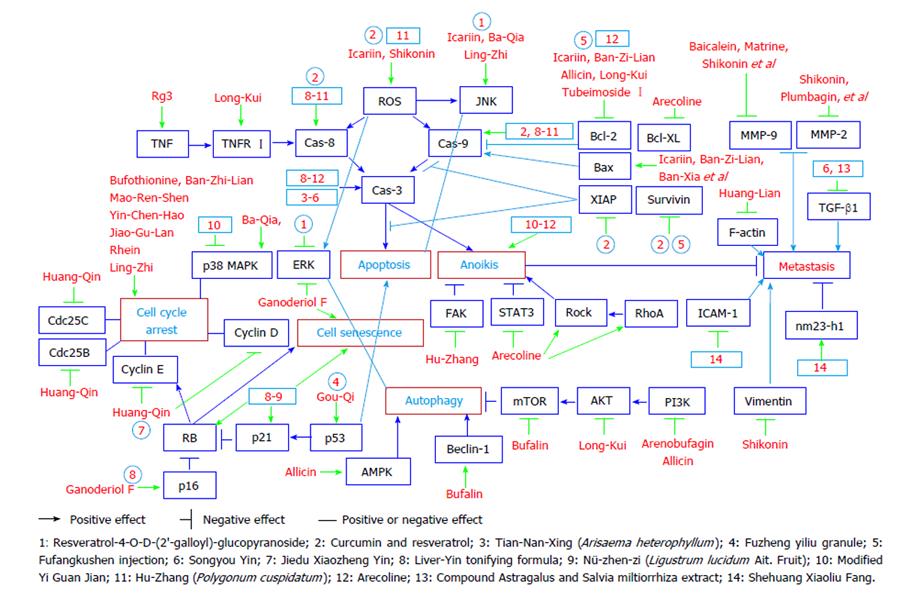
Contemporary TCM physicians have developed some new herbal formulas for liver cancer treatment. Fuzheng yiliu granule, a four herb formula for tonifying Qi and blood, and dissolving stasis, is effective to up-regulate p53 and caspase-3 expression and reduce mitochondrial membrane potential to induce apoptosis in H22 hepatocarcinoma[126,127]. Fuganchun 6, a formula for nourishing Qi and Yin, detoxifying and dissipating mass, could induce apoptosis and arrest cell cycle at G0/G1 phase[128]. Bushen jianpi decoction, a formula for tonifying kidney and spleen, was reported to inhibit VEGF expression and induce apoptosis in H22 hepatocarcinoma[129]. Warming yang and dispersing stasis formula may induce apoptosis in hepatocarcinoma Bel-7402 cells[130]. Fufangkushen injection, a patent herbal drug, may inhibit survivin and Bcl-2 expression, increase caspase-3 expression and induce apoptosis in SMMC-7721 cells[131]. Songyou Yin, another patent herbal drug, could induce apoptosis and down-regulation of MMP2 and VEGF to inhibit tumor growth and prolong survival[132] (Figure 1).
Sustaining proliferative signaling is a hallmark of cancer[133]. Cancer cells present an un-controlled proliferation cycle. To stop cell cycle is an ideal principle for cancer treatment. Some herbs are demonstrated to be potent to arrest cell cycle. Among tonic herbs, extracts of Jiao-Gu-Lan (Gynostemma pentaphyllum) can inhibit proliferation and arrest cell cycle at G0/G1 phase in Hep3B cells[134,135]. Triterpene-enriched extracts from Ling-Zhi (Ganoderma lucidum) could suppress protein kinase C, activate JNK and p38 mitogen-activated protein kinases (MAPK) to prolong G2 cell cycle phase and inhibit cell growth in Huh-7 cells[136].
Ban-Zhi-Lian (Scutellaria barbata) is able to inhibit cell proliferation, decrease the number of cells in S-phase and increase the number of cells in G0/G1-phase and induce apoptosis in HepG2 cells [137]. Huang-Qin (Scutellaria baicalensis) is effective to inhibit cell growth and G2/M phase arrest accompanied by increased Cyclin E and down-regulation of p53, ETS1 (V-ets avian erythroblastosis virus E26 oncogene homolog 1), cell division cycle 25B (Cdc25B), p63, epidermal growth factor receptor (EGFR), ERK1/2, XIAP, HIF-2alpha, and Cdc25C[138]. Bufothionine also can inhibit cell proliferation and arrest cell cycle at G2/M phase in liver cancer cells[139]. Rhein, a component from Da-Huang (Rheum palmatum L. or Rheum tanguticum Maxim. ex Balf.), is potent to inhibit cell growth, induce apoptosis and arrest cell cycle at S phase[140].
Huang-lian-jie-du-tang, a classic herbal formula for clearing heat and removing toxicity, was reported to effectively inhibit cell proliferation, induce cell cycle arrest and apoptosis in hepatocarcinoma in vitro and in vivo[141]. Bu-Zhong-Yi-Qi-Tang, a Qi tonifying herbal formula, is confirmed effective to inhibit cell proliferation, induce apoptosis and arrest cell cycle at G0/G1 phase[142]. Jiedu Xiaozheng Yin, a modern herbal formula, could inhibit the growth of HepG2 cells and arrest cell cycle at the G0/G1 phase coincidence with up-regulation of cyclin D and cyclin E[143] (Figure 1).
Autophagy, type II programmed cell death, is a process in which organelles and proteins are sequestered and subsequently degraded through fusion with lysosomes, and has been recognized as a target for hepatocarcinoma treatment[144,145]. Long-Kui (Solanum nigrum L.), a frequently used anti-cancer herb, may induce apoptosis and down-regulate Bcl-2 and AKT to induce autophagy in hepatocarcinoma cells[146].
Arenobufagin, a natural bufadienolide from toad venom, is potent to induce apoptosis and autophagy by down-regulation of PI3K/AKT/mechanistic target of rapamycin (mTOR) pathway in HepG2/ADM hepatoma cells, and thus inhibit xenograft tumor growth[147]. Bufalin, a component from toad skin, has been demonstrated to induce AMP-activated protein kinase (AMPK) dependent autophagy accompanied by enhanced Beclin-1 expression and LC3-I to LC3-II conversion, and decreased p62 expression and mTOR signaling in HepG2 cells[148].
Allicin, a major phytochemical of crushed garlic, is effective to induce autophagy in HepG2 cells by decreasing the level of cytoplasmic p53, the PI3K/mTOR signaling pathway, and Bcl-2 and up-regulating the expression of AMPK/tuberous sclerosis protein 2 and Beclin-1[149]. Shikonin, a naphthoquinone from Zi-Cao (Lithospermum erythrorhizon), could induce autophagy and reactive oxygen species generation which further activates ERK[150] (Figure 1).
Cell senescence is a state of stable, irreversible cell cycle arrest provoked by a variety of stimuli. Pro-senescence has been suggested for hepatocellular carcinoma treatment[151]. We have established a liver-Yin tonifying formula (LYTF) for liver-Yin-deficiency in patients with hepatocarcinoma. LYTF could activate caspases-8, -9 and -3 to induce apoptosis, and up-regulate p16 and p21 and down-regulate RB phosphorylation to induce cell senescence in Bel-7402 cells[152]. Ganoderiol F, a tetracyclic triterpene from Ganoderma amboinense, may activate ERK and up-regulate p16 to induce cell senescence in hepatoma HepG2 cells[153]. Nü-zhen-zi (Ligustrum lucidum Ait. Fruit), an herb for tonifying liver-Yin, is potent to up-regulate p21, activate caspases-8, -9 and -3 to induce apoptosis and down-regulate RB phosphorylation to induce cell senescence in hepatocarcinoma cells[154] (Figure 1).
Anoikis, an apoptotic process occurring when cells detach from the extracellular matrix, is associated with metastasis of hepatocarcinoma[155,156]. We have found modified Yi Guan Jian, an herbal formula for hepatocarcinoma, may activate caspase-3, -8 and -9, inhibit the expression and phosphorylation of p38 MAPK, and induce anoikis in human hepatocarcinoma Bel-7402 cells[156]. Hu-Zhang (Polygonum cuspidatum), an herb for draining dampness and dissipating stasis, could activate caspase-3 and -9 and induce anoikis in human hepatocarcinoma Bel-7402 cells accompanied by ROS generation and focal adhesion kinase down-regulation[157]. Arecoline, an alkaloid from Bing-Lang (Areca catechu L.), may induce anoikis in HA22T/VGH cells involving inhibition of STAT3 and increased RhoA/Rock (Ras homolog family member A/Rho-associated, coiled-coil containing protein kinase) activation[158] (Figure 1).
In addition to induction of anoikis, Chinese herbs also could inhibit metastasis potential in hepatocarcinoma cells, such as adhesion, migration, invasion and metastasis. Among heat-clearing herbs, Coptidis Rhizoma (Huang-Lian) may reduce F-actin polymerization and damage to cytoskeleton network to inhibit hepatocarcinoma cell migration[159]. Baicalein, a compound from Scutellaria baicalensis Georgi (Huang-Qin), could inhibit migration and invasion in human hepatocellular carcinoma SMMC-
7721 cells accompanied by down-regulation of ezrin, VEGF, and MMP-9[160]. Matrine, a component of Sophora flavescens Ait. (Ku-Shen), was reported to be effective to inhibit MMP-9 and nuclear factor κB (NF-κB) to inhibit invasion of liver cancer cells[161]. Shikonin, an ingredient of Lithospermum erythrorhizon (Zi-Cao), is potent to inhibit the migratory ability of hepatocarcinoma cells through downregulation of vimentin, MMP-2 and MMP-9[162].
Another frequently studied herbal type is dissolving stasis herbs. Gekko sulfated polysaccharide-protein complex has been demonstrated to be effective in inhibiting hepatocellular carcinoma cell migration through calcium-mediated regulation of the actin cytoskeleton reorganization[163]. Ardipusilloside, a compound from Ardisia japonica (Thunb) Blume (Zi-Jin-Niu), has the potential to inhibit liver cancer survival, invasion and metastasis by down-regulation of MMP-9 and MMP-2 and activating Ras-related C3 botulinum toxin substrate 1 (Rac 1) to enhance E-cadherin activity[164]. Plumbagin, a constituent of Plumbago zeylanica L. (Bai-Hua-Dan), could suppress the proliferation and invasiveness in SK-hep-1 cells by up-regulation of p21 and down-regulation of MMP-2 and MMP-9[165]. Tanshinone II-A, a component from Dan-Shen (Salvia miltiorrhiza), could effectively inhibit invasion and metastasis of hepatocaxrcinoma cells partly by inhibiting MMP-2 and MMP-9 activities and blocking NF-κB activation[166].
Some herbal formulas have been confirmed to be effective against hepatocarcinoma metastasis. In addition to inhibiting liver cancer growth, Songyou Yin also could down-regulate activated hepatic stellate cells secreted IL-6, TGF-β1 and VEGF to reduce MMP-2 expression and reverse epithelial-mesenchymal transition, and thus inhibit invasion and metastasis in hepatocarcinoma[167]. Biejiajian pill, a classical herbal formula, could effectively inhibit HepG2 cell proliferation, adhesion and invasion[168]. Compound Astragalus and Salvia miltiorrhiza extract, an herbal component formula made up of astragalosides, astragalus polysaccharide and salvianolic acids, may inhibit TGF-β1 mediated invasion in HepG2 hepatoma cells through modulating TGF-beta/Smad signaling[169]. Shehuang Xiaoliu Fang, an herbal formula for detoxifying and dissipating masses, is potent to inhibit invasive and adhesive ability of SMMC-7721 cells accompanied by increased nm23-h1 expression and reduced ICAM-1 expression[170] (Figure 1).
CD4+ and CD8+ T lymphocytes are the major cell populations for cellular immunity against cancer. Lycium barbarum (Gou-Qi) polysaccharides could increase CD4+ and CD8+ T cells in tumor-infiltrating lymphocytes in H22 hepatoma[171]. Dong-Chong-Xia-Cao (Cordyceps sinensis), a commonly used herb for tonifying kidney, may increase the expression of major histocompatibility complex class II antigens on human hepatoma HA22T/VGH cells[172]. Ban-Zi-Lian (Scutellaria barbata), an effective anti-cancer herb for hepatocarcinoma, could increase the thymus and spleen index, lymphocytes proliferation activities, natural killer (NK) cell activities and IL-2 production in splenocytes[173]. The proteins extracted from mycelia of Lei-Wan (Omphalia lapidesces) are effective in increasing spleen mass and interferon-γ (IFN-γ) production in H22 hepatocarcinoma bearing mice[174].
Xiaochaihu decoction, a classical herbal formula for liver disease, is effective in inhibiting tumor growth and increasing T lymphocyte proliferation, NK cells activities and IL-2 level in H22 bearing mice[175]. Mylabris Mixture, a modern anti-hepatoma herbal formula, may increase CD4+, CD8+ lymphocytes and NK cells, and IFN-γ and IL-4 production in H22 cancer-bearing mice[176]. Fuzheng Yiliu Granule, an effective pro-apoptosis contemporary herbal formula, may increase CD4+ lymphocytes and related cytokines IL-2 and TNF-α, and NK cells in H22 tumor-bearing mice[177]. Fuganchun 6, a modern herbal formula, can inhibit tumor growth and enhance proliferation activity of lymphocytes, NK cell activities and IL-2 production in H22 hepatoma bearing mice[178].
Dendritic cells (DCs) are important antigen present cells for anti-cancer immunity. Lycium barbarum (Gou-Qi) polysaccharides could promote DCs to stimulate allogeneic lymphocyte proliferation, produce IL-12p70 and IFN-γ and may relate to NF-κB expression[179]. Chen et al[180] found that human hepatocellular carcinoma SMMC-7721 cells may impair the biorheological properties of DCs, such as cell deformability, migration, and electrophoresis mobility, and changed organizations of cytoskeletal proteins. Gekko (Tian-Long) sulfated polysaccharide-protein complex could partially restore the defective biorheological characteristics of DCs mediated by SMMC-7721 cells[180].
CD4+ CD25+ regulatory T cells (Tregs) are originated from CD4+ Th0 cells upon the stimulation of TGF-β and Foxp3 expression. Tregs may produce IL-10 and function as a negative immune regulator. Radix Glycyrrhizae (Gan-Cao) polysaccharides were demonstrated to down-regulate Tregs, related cytokines IL-10 and TGF-β, and Foxp3 expression, and increased IL-2 and IL-12p70 levels in serum in H22 hepatocarcinoma bearing mice[181] (Figure 2).
Angiogenesis, the process of new blood vessel generation from existing vessels, plays a crucial role in tumor growth and metastasis, and has been suggested as a potential target for hepatocarcinoma prevention and treatment[182,183].
Tian-Long (Gekko Chinenis) has been showed to be effective to inhibit tumor growth, induce apoptosis, and inhibit angiogenesis accompanied by down-regulation of VEGF and basic fibroblast growth factor (bFGF) in H22 hepatocarcinoma[184]. Gekko-sulfated glycopeptide may inhibit angiogenesis by decreasing bFGF secretion, and binding to heparin/heparan sulfate in liver cancer[185]. Bai-Ji (Bletilla colloid) could inhibit endothelial cell growth and angiogenesis after TACE[186]. Huaier may inhibit VEGF expression and angiogenesis, induce apoptosis and inhibit tumor growth in hepatocarcinoma[187].
Fu-Zheng-Kang-Ai-Tang, an herbal formula for strengthening body defense and anti-cancer, could inhibit VEGF and bFGF expression, angiogenesis and tumor growth in hepatocarcinoma[188]. Delisheng, an herbal formula for tonifying Qi and resolving masses, may inhibit cell growth and increase endostatin expression in hepatocellular carcinoma HepG2 cells[189]. Qingrejiedu, huoxuehuayu and fuzhengguben (QHF) formula, an herbal component formula, is potent to inhibit VEGF, EGFR and MMP-2, angiogenesis and tumor growth[190]. Erbie San, a patent herbal drug for resolving masses, was demonstrated to be effective to down-regulate VEGF/endostatin and inhibit tumor growth in Walker-256 liver cancer[191] (Figure 2).
Chemotherapy is not conventionally used in hepatocarcinoma, but chemotherapeutic drugs based TACE is a major treatment for liver cancer. Ban-Zi-Lian (Sculellaria barbata) can significantly enhance 5-fluorouracil (5-Fu) to inhibit tumor growth and prolong survival time, improve immune function, and reduce the toxic effects of 5-Fu in the H22 tumor-bearing mice[192]. Ling-Zhi (Ganoderma lucidum) is able to inhibit hepatocarcinoma cell proliferation and protect hepatocytes from chemotherapy induced damage[193]. Dong-Chong-Xia-Cao (Cordyceps sinensis) may protect H22 hepatocarcinoma bearing mice from chemotherapy induced immunosuppression[194].
Chaiqiyigan granula is potent to enhance inhibitory effects of taxol on hepatocarcinoma growth accompanied by up-regulation of Bax and down-regulation of p53 and VEGF[195]. QHF, an herbal component formula, could reduce cisplatin (DDP)-induced leucopenia, spleen and thymus atrophy, enhance tumor growth inhibition and prolong survival time in H22 bearing mice[196]. Shengmai Injection, a patent herbal drug, is effective to enhance anti-tumor efficacy and reduce toxicity of 5-Fu in H22 hepatocarcinoma[197] (Figure 2).
Drug resistance contributes to chemotherapy refractoriness in hepatocarcinoma[198]. To seek effective herbs or herbal components to reverse drug resistance has become one of research focuses in liver cancer study. Astragalus polysaccharides have been reported to be potent to enhance anti-tumor effects of adriamycin in H22 hepatocarcinoma by up-regulating IL-1α, IL-2, IL-6, and TNF-α, down-regulating IL-10 and multidrug resistance protein 1 (MDR1)[199]. Astragaloside II, another component from Huang-Qi (Astragalus membranaceus), is effective to increase 5-Fu cytotoxicity toward 5-Fu-resistant Bel-7402/Fu cells accompanied by down-regulation of P-gp (P-glycoprotein), phosphorylation of ERK1/2, p38 and JNK[200].
Green tea catechins have been reported to effectively inhibit MDR1 expression, increase intracellular doxorubicin (DOX) accumulation and enhance DOX-induced cell killing activities against BEL-7404/DOX cells[201]. Tetramethylpyrazine, a bioactive constituent isolated from the root of Ligusticum chuanxiong Hort, could down-regulate MDR1, multidrug resistance protein 2 (MRP2), MRP3 and MRP5 in adriamycin resistant HepG2 cells[202]. Pseudolaric acid B, polyphyllin D and Eclipta alba (Mo-Han-Lian) have been demonstrated to increase drug sensitivity in drug resistant HepG2 hepatoma cells[203-205] (Figure 2).
Hepatocarcinoma patients may present Qi-stagnation, damp-heat, blood stasis, Qi-deficiency, Yin-deficiency and other TCM syndromes. Modern treatments such as surgery, TACE and HIFU and other treatments would influence syndrome manifestation in liver cancer patients. Modern technologies have been exploited to elucidate the relation between syndromes and biomedical sciences. Further studies are needed to use those information for herb medication and formulation to improve clinical efficacy of TCM treatment for hepatocarcinoma.
Since TCM pathological factors and syndromes in hepatocarcinoma patients, such as Qi-stagnation, damp-heat, blood stasis, Qi and Yin-deficiency, are also seen in other disease, hepatocarcinoma needs to be recognized and treated as a malignant disease. In addition to syndrome differentiation based treatment, anti-cancer therapy or anti-cancer herb application should be reinforced in the treatment of hepatocarcinoma. Moreover, since most of liver cancer patients receive comprehensive therapy, TCM treatment in those patients should consider the received therapy and accordingly adjust herb medication.
Classic TCM theory and principles have been adopted for hepatocarcinoma prevention study. Chinese herbs with traditional efficacy of tonifying Qi, blood and Yin, soothing liver-Qi stagnation, clearing heat and detoxifying and dissolving stasis, have been demonstrated to be potent to prevent hepatocarcinogenesis. Some classical and modern herbal formulas have been demonstrated to have preventive effects against hepatocarcinogenesis. Further clinical studies are needed to use these achievements to protect high-risk individuals from hepatocarcinogenesis.
Clinical practices have confirmed that TCM is effective to alleviate clinical symptoms, improve QOL and immune function, prevent recurrence and metastasis, delay tumor progression, and prolong survival time in hepatocarcinoma patients. Experimental studies have demonstrated that Chinese herbs and/or herbal formula are potent to induce apoptosis, autophagy, anoikis and cell senescence, arrest cell cycle, regulate immune function, inhibit metastasis and angiogenesis, reverse drug resistance and enhance effects of chemotherapy in hepatocarcinoma.
How to use experimental results to improve clinical efficacy has become an important research subject. For commonly used traditional herbs with anti-cancer effects, the property of Chinese herbs should be firstly considered and medicated by the guidance of TCM principles. For traditionally uncommonly used anti-cancer herbs, such as Mu-Tou-Hui (Patrinia scabra Bunge) and She-Mei [Duchesnea indica (Andr.) Focke], the property of Chinese herbs and anti-cancer characters of those herbs need to be further studied. In addition, there is a great need to explore the compatibility or combinational application rule of anti-cancer herbs to further improve clinical efficacy of TCM treatment for hepatocarcinoma.
P- Reviewer: Scaggiante B, Watashi K, Yun JW S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379:1245-1255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3249] [Cited by in RCA: 3594] [Article Influence: 276.5] [Reference Citation Analysis (4)] |
| 2. | Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23762] [Cited by in RCA: 25538] [Article Influence: 1824.1] [Reference Citation Analysis (7)] |
| 3. | Chen JG, Chen WQ, Zhang SW, Zheng RS, Zhu J, Zhang YH. [Incidence and mortality of liver cancer in China: an analysis on data from the National Registration System between 2003 and 2007]. Zhonghua Liuxingbingxue ZaZhi. 2012;33:547-553. [PubMed] |
| 4. | Fan JH, Wang JB, Jiang Y, Xiang W, Liang H, Wei WQ, Qiao YL, Boffetta P. Attributable causes of liver cancer mortality and incidence in china. Asian Pac J Cancer Prev. 2013;14:7251-7256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 5. | de Kretser TA, Lee GT, Thorne HJ, Jose DG. Monoclonal antibody CI-panHu defines a pan-human cell-surface antigen unique to higher primates. Immunology. 1986;57:579-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Tang ZY. Combination of traditional Chinese medicine and western medicine in the treatment of liver cancer. Linchuang Gandanbing Zazhi. 2011;27:449-450. |
| 7. | Wu MC. [Traditional Chinese medicine in prevention and treatment of liver cancer: function, status and existed problems]. Zhongxiyi Jiehe Xuebao. 2003;1:163-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Li M, Qiao C, Qin L, Zhang J, Ling C. Application of traditional Chinese medicine injection in treatment of primary liver cancer: a review. J Tradit Chin Med. 2012;32:299-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Wu P, Dugoua JJ, Eyawo O, Mills EJ. Traditional Chinese Medicines in the treatment of hepatocellular cancers: a systematic review and meta-analysis. J Exp Clin Cancer Res. 2009;28:112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Hu B, Du Q, Shen KP, Xu L. Principles and scientific basis of Traditional Chinese Medicine in cancer treatment. J Bioanal Biomed. 2012;S6:005. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Du Q, Hu B, Shen KP, An HM. Progress in TCM pathogenesis and treatment of liver cancer. Shijie Zhongxiyi Jiehe Zazhi. 2010;5:814-817. |
| 12. | Hu B, An HM, Shen KP. Syndrome differential anti-cancer and scientific anti-cancer. Zhongguo Minzu Minjian Yiyao. 2009;18:33-34. |
| 13. | Wang Y, Ji G, Wang YQ, Zhang W, Xing LJ, Dong GH, Wang YN, Lin SH. Effects of traditional Chinese medicine on TGF-βIIR expression in DMN induced hepatic precancerous lesion in rats. Zhejiang Zhongxiyi Jiehe Zazhi. 2001;11:23-24. |
| 14. | Tatsuta M, Iishi H, Baba M, Nakaizumi A, Uehara H. Inhibition by xiao-chai-hu-tang (TJ-9) of development of hepatic foci induced by N-nitrosomorpholine in Sprague-Dawley rats. Jpn J Cancer Res. 1991;82:987-992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Tatsuta M, Iishi H, Baba M, Nakaizumi A, Uehara H. Inhibition by shi-quan-da-bu-tang (TJ-48) of experimental hepatocarcinogenesis induced by N-nitrosomorpholine in Sprague-Dawley rats. Eur J Cancer. 1994;30A:74-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Zou KC, Song WM, Xu FX, Lin SM, Guo GY, Wang HW, Liu L, Zhou JP, Zhang HF, Sun YQ. Effect of Nourishing-Yin Decoction and Removing-Toxic-Heat Decoction on histological observation in rats Liver during canceration. Zhongguo Zhongxiyi Jiehe Zazhi. 1995;15:238-240, 396. |
| 17. | Guan Y, Zhou Z, Zhang C, Ruan Y, Wu Z. Effect of A-L tonic capsule on DNA content in rat experimental hepatocarcinogenesis. J Huazhong Univ Sci Technolog Med Sci. 2002;22:12-13, 16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Zou J, Chen JJ. Preventive effect of prescription of Nourishing Shen on rat hepatocarcinoma induced by Diethylnitrosamine. Zhongxiyi Jiehe Ganbing Zazhi. 2003;13:278-280. |
| 19. | Liu C, Liu P, Wang XS, Xu LM, Hu YY. Experimental study of Fu-zheng-hua-yu formula for liver cancer prevention. Zhongguo Zhongxiyi Jiehe Piwei Zazhi. 1995;33:163-166. |
| 20. | Li X, Shi ZM, Feng P, Wen ZY, Wang XJ. Effect of Qi-protecting powder (Huqi San) on expression of c-jun, c-fos and c-myc in diethylnitrosamine-mediated hepatocarcinogenesis. World J Gastroenterol. 2007;13:4192-4198. [PubMed] |
| 21. | Wen Z, Shi Z, Feng P, Xue X, Dong K, Wang X. Modulation of energy metabolic enzyme expression in N-nitrosodiethylamine-mediated hepatocarcinogenesis by Chinese herbs, Huqi San. Biofactors. 2008;34:303-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 22. | Qian Y, Ling CQ. Preventive effect of Ganfujian granule on experimental hepatocarcinoma in rats. World J Gastroenterol. 2004;10:755-757. [PubMed] |
| 23. | Qiu JX. [The effect of “SRRS” recipe on the formation of liver cancer in the rat]. Zhongxiyi Jiehe Zazhi. 1988;8:734-735, 710. [PubMed] |
| 24. | Zhang B, Li Q, Yin PH, Zhao CG, Li XQ, Gao H, Sun J, Fan ZZ. Involvement of miR-199a downregulation in the preventive effects of Jianpi Jiedu Recipe against experimental hepatocarcinoma in rats. Shijie Huaren Xiaohua Zazhi. 2010;18:125-131. |
| 25. | Zhang B, Li Q, Yin PH, Zhao CG, Gao H, Sun J, Fan ZZ. Study on AKT/ PI3K signaling pathway and prevenion effect of Jianpi Jiedu Recipe in rats with experimental hepatocarcinogenesis. Zhongguo Zhongxiyi Jiehe Xiaohua Zazhi. 2010;18:4-9. |
| 26. | Gao HS, Yao SK, Yin F. The effect of Ganzheng solution on the ICAM-1 expression in liver tissues of rat in the diethylnitrosamine induced hepatocarcinogenesis. Hebei Zhongyi. 2007;29:848-850. |
| 27. | Nie G, Long AH, Fu QL, Li HM, Ming AP, Xiao L, Yan XS, Wang BX. Zao-Lian mixture prevents Diethylnitrosamine induced hepatocirrhosis and hepatocaecinogenesis in rats. Zhongxiyi Jiehe Ganbing Zazhi. 1998;8:107-109. |
| 28. | Lee CY, Hsu YC, Wang JY, Chen CC, Chiu JH. Chemopreventive effect of selenium and Chinese medicinal herbs on N-nitrosobis(2-oxopropyl)amine-induced hepatocellular carcinoma in Syrian hamsters. Liver Int. 2008;28:841-855. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Fang ZQ, Guan DY, Liang SH, Qin HY, Li HY. Comparative study on functions of different therapies on liver cancer in mice. Shanghai Zhongyiyao Daxue Xuebao. 2002;16:42-46. |
| 30. | Guan DY, Lu HX, Fang ZQ. Study on the regulation of different therapies on some signal moleculars transcriptions in the pathway of Ras/MAPK. Zhongguo Zhongyi Jichu Yixue Zazhi. 2002;8:36-38. |
| 31. | Guan D, Fang Z, Lu H, Li H. Preliminary investigation on regulating effects of different TCM treatments on transcription of the correlated genes of liver cancer in rats. J Tradit Chin Med. 2003;23:62-66. [PubMed] |
| 32. | Cui R, Wang B, Zhang F, Chen G, Yin S. Suppressive effect of herbal compound 861 on chemical hepatocarcinogenesis in rats. Chin Med J (Engl). 2003;116:378-382. [PubMed] |
| 33. | Zhu MJ, Zhang H, Gao SS, Zhang XS. Effects of new anti-tumor formula on protecting against synergistic hepatocarcinogenesis of hepatitis B virus expression and aflatoxin B1 and free radicals metabolism in HBV large envelope transgenic mice. Liaoning Zhongyi Xueyuan Xuebao. 2003;5:263-264. |
| 34. | Li X, Wu XG. [Effects of ginseng on hepatocellular carcinoma in rats induced by diethylnitrosamine--a further study]. J Tongji Med Univ. 1991;11:73-80. [PubMed] |
| 35. | Yan RQ, Chen ZY, Qin GZ, Qin LL. Effects of twelve herbs on Aflatoxin B1 induced hepatocarcinogensis in rats. Guangxi Yixueyuan Xuebao. 1986;3:21-23. |
| 36. | Ruan CC, Liang Y, Liu ZH. Inhibition of 12 Chinese Traditional Medicinal herbs on mutagenic effects induced by Aflatoxin B1. Ai Zheng. 1987;8:29-31. |
| 37. | Shen M, Yin Z. [Effect of Boschniakia rossica extract on antioxidative activities in rat hepatic preneoplasia induced by diethylnitrosamine]. Zhongguo Zhongyao Zazhi. 1999;24:746-78, 765. [PubMed] |
| 38. | Yin ZZ, Jin HL, Li TZ, Lee JJ, Kim YH, Lee CH, Lee KH, Hyun BH. [Inhibitory effect of methanol extract of Boschniakia rossica Fedtsch. et Flerov on rat hepatic preneoplastic lesions induced by diethylnitrosamine]. Zhongguo Zhongyao Zazhi. 1998;23:424-426, 448- inside back cover. [PubMed] |
| 39. | Dai ZJ, Wang XJ, Ji ZZ, Liu XX, Kang HF, Diao Y, Ma XB, Liu L, Ren HT. [Inhibitory effects of Scutellaria barbate extracts on diethylnitrosamine-induced hepatocarcinoma in rats]. Zhong Yao Cai. 2009;32:568-571. [PubMed] |
| 40. | Lin YL, Hsu JD, Chou FP, Lee MJ, Shiow SJ, Wang CJ. Suppressive effect of penta-acetyl geniposide on the development of gamma-glutamyl transpeptidase foci-induced by aflatoxin B(1) in rats. Chem Biol Interact. 2000;128:115-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 41. | Zhao X, Zhang JJ, Wang X, Bu XY, Lou YQ, Zhang GL. Effect of berberine on hepatocyte proliferation, inducible nitric oxide synthase expression, cytochrome P450 2E1 and 1A2 activities in diethylnitrosamine- and phenobarbital-treated rats. Biomed Pharmacother. 2008;62:567-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 42. | Luo RX, Lin RT, Lu YB, Cai L, Yi YN. Inhibition of Artemisa capillaris Thunb on mutagenic effects induced by Aflatoxin B1. Fujian Yixueyuan Xuebao. 1990;24:352-354. |
| 43. | Liu J, Yang CF, Wasser S, Shen HM, Tan CE, Ong CN. Protection of salvia miltiorrhiza against aflatoxin-B1-induced hepatocarcinogenesis in Fischer 344 rats dual mechanisms involved. Life Sci. 2001;69:309-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 44. | Kim J, Ha HL, Moon HB, Lee YW, Cho CK, Yoo HS, Yu DY. Chemopreventive effect of Curcuma longa Linn on liver pathology in HBx transgenic mice. Integr Cancer Ther. 2011;10:168-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 45. | Deng W, Xiang Q, Li B. Effects of prescription of Sanqi on rats with hepatocarcinoma induced by diethylnireosamine. Guangxi Yixue. 2013;35:1442-1446. |
| 46. | Ohtaki Y, Nomura M, Hida T, Miyamoto K, Kanitani M, Aizawa T, Aburada M. Inhibition by gomisin A, a lignan compound, of hepatocarcinogenesis by 3’-methyl-4-dimethylaminoazobenzene in rats. Biol Pharm Bull. 1994;17:808-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Zhang YH, WuJP . Effects of Jian-Pi-Huo-Xue Formula on in patients with hepatitis, hepatic cirrhosis and low level of AFP. Zhongxiyi Jiehe Ganbing Zazhi. 2000;10:13-14. |
| 48. | Zhang ZQ, Liu QF, Zhong SC, Huang TR, Wu YD, Wang TC, Huang NF, Liang RX. Epidemiological studies on Salvia miltiorrhiza for liver cancer prevention. Guangxi Yixue. 1995;17:179-181. |
| 49. | Oka H, Yamamoto S, Kuroki T, Harihara S, Marumo T, Kim SR, Monna T, Kobayashi K, Tango T. Prospective study of chemoprevention of hepatocellular carcinoma with Sho-saiko-to (TJ-9). Cancer. 1995;76:743-749. [PubMed] |
| 50. | Zhao G, Lang QB, Ling CQ. Characteristics of 294 cases of primary liver cancer. Shijie Zhongxiyi Jiehe Zazhi. 2008;3:275-277. |
| 51. | Li YJ, Fang ZQ, Tang CL, Ma J, Guan DY, Chen DS. Clinical epidemiological investigation and research of syndrome distribution law in Chinese medicine of 2060 cases of primary liver carcinoma. Zhongguo Yiyao Xuebao. 2003;18:144-146. |
| 52. | Fang ZQ, Li YJ, Tang CL, Ma J, Guan DY, Chen DS. Analysis on characteristics of syndromes in 2060 cases of primary hepatic cancer. Zhongyi Zazhi. 2004;45:53-54. |
| 53. | Wang CJ, Hu Y, Fu TT, Huang XH, Dai XB, Shi L, Li YC, Xioang J. Syndrome distribution of primary liver cancer in Guangzhou area. Zhonghua Zhongyiyao Xuekan. 2010;28:2314-2318. |
| 54. | Yang XB, Long SQ, Wu WY, Deng H, Pan ZQ, He WF, Zhou YS, Liao GY, Ouyang YS, Li QP. [The distribution of Chinese medicine syndrome types in primary liver cancer and their differences of the survival time: a clinical study]. Zhongguo Zhongxiyi Jiehe Zazhi. 2013;33:911-914. [PubMed] |
| 55. | Wan X, Zhang YH. Relation betwwen syndrome and quality of life in patients with liver cancer. Guiyang Zhongyi Xueyuan Xuebao. 2008;30:27-28. |
| 56. | Zhang YH, Qin X, Xu J, Sun Z, Lang QB, Yue XQ, Zhai XF. A preliminary study on TCM compound syndrome characteristics of 58 patients with liver cancer before and after operation. Zhongxiyi Jiehe Ganbing Zazhi. 2012;22:75-80. |
| 57. | Ye Y, Qin LP, Yue XQ, Zhai XF, Xu J, Xiao KY, Huang F, Li B. Tongue changes in 103 perioperative patients with primary liver cancer. Zhongyi Zazhi. 2014;55:48-52. |
| 58. | Li YJ, Fang ZQ, Tang ZL, Ma J, Guan DY. Comparative study of TCM syndromes in liver cancer patients after TACE and surgery. Zhongyiyao Xuekan. 2003;21:504-504. |
| 59. | Yang SF, Lin YL. TCM Syndrome of Primary Liver Carcinoma before Interventional Treatment by Cluster Analysis. Zhongyiyao Xinxi Zazhi. 2012;19:11-12. |
| 60. | Zeng PH, Liu WS, Pan MQ, Xu K, Wu WY, Chang G, Jiang YL, Cai M. Study on development of syndrome in Chinese medicine during transcatheter arterial intervention in primary hepatic carcinoma. Hunan Zhongyiyao Daxue Xuebao. 2008;28:54-56. |
| 61. | Meng J, Qin LP, Liu L, Lang QB, Li B. Impact of TACE on Syndromes in PHC. Zhejiang Zhongyiyao Daxue Xuebao. 2012;36:1194-1198. |
| 62. | Zhang YH, Qin X, Xu J. [Analysis of Chinese medical syndrome features of patients with primary liver cancer before and after transcatheter arterial chemoembolization]. Zhongguo Zhongxiyi Jiehe Zazhi. 2012;32:1171-1174. [PubMed] |
| 63. | He D. Study on change of TCM syndrome in patients with primary liver cancer before and after high intensity focus ultrasound treatment. Jianyan Yixue Yu Linchuang. 2012;9:2676-2677. |
| 64. | Chen QW, Huang XQ, Yang GJ, Dai WX, Lang QB, Yan SK, Zhou J, Zhang WD, Ling CQ. Preliminary study of serum metabonomics on Yang-deficiency Syndrome of patients with primary liver cancer. Zhonghua Zhongyiyao Xuekan. 2012;30:526-529. |
| 65. | Yang SF, Qiu SP, Liu QH. [Observation of serum protein fingerprinting in primary liver cancer patients of different Chinese medical syndromes before and after interventional treatment]. Zhongguo Zhongxiyi Jiehe Zazhi. 2013;33:1352-1355. [PubMed] |
| 66. | Huang ZG, Zhang XQ, Ye YB, Chen HQ, Chen Q, Yang AL. Initial study on application of protein fingerprinting in Zheng differentiation-classification of primary liver cancer. Xiandai Zhongxiyi Jiehe Zazhi. 2012;21:3660-3664. |
| 67. | Weng L, Du J, He WT, Ling CQ. [Characteristic genomics of peripheral blood mononuclear cells of hepatocellular carcinoma patients with liver-kidney yin deficiency syndrome]. Zhongxiyi Jiehe Xuebao. 2012;10:406-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 68. | Su XK, Wu YS, Li YH, Yang XW, Lu YY, Chi JA. Relationship between TCM Syndrome Differentiation of liver cancer and adhesion degree of cancer Cell. Zhongguo Zhongxiyi Jiehe Waike Zazhi. 2009;15:10-12. |
| 69. | Su XK, Cheng YX, Lin SH. Correlation of Syndrome Differentiation of liver cancer with matrix degradation. Xin Zhongyi. 2008;40:37-39. |
| 70. | Pan ZQ, Fang ZQ, Lu WL. Comparative research on syndrome manifestation features in mice with H22 liver cancer and Lewis lung carcinoma. Beijing Zhongyiyao Daxue Xuebao. 2008;31:184-188. |
| 71. | Pan ZQ, Fang ZQ, Lu WL, Liang C, Wu ZH, Liu XM, Hou L, Zhang H, Zhuo SY, Liao MJ. [Differentially expressed genes in adrenal gland of H22 liver cancer mice with different syndromes and in different stages]. Zhongxiyi Jiehe Xuebao. 2008;6:843-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 72. | Chen Z, Chen HY, Lang QB, Li B, Zhai XF, Guo YY, Yue XQ, Ling CQ. Preventive effects of jiedu granules combined with cinobufacini injection versus transcatheter arterial chemoembolization in post-surgical patients with hepatocellular carcinoma: a case-control trial. Chin J Integr Med. 2012;18:339-344. [PubMed] |
| 73. | Sun Z, Liang ST, Zhai XF, Lang QB, Zhou QH, Yue XQ, He J, Xu J, Zhu Y, Ling CQ. A traditional Chinese herbal medicine compound preparation versus interventional therapy after resection of small hepatocellular carcinoma: 22-year follow-up. J Tradit Chin Med. 2012;32:156-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 74. | Chen LW, Lin J, Chen W, Zhang W. [Effect of Chinese herbal medicine on patients with primary hepatic carcinoma in III stage during perioperational period: a report of 42 cases]. Zhongguo Zhongxiyi Jiehe Zazhi. 2005;25:832-834. [PubMed] |
| 75. | Yu Y, Lang Q, Chen Z, Li B, Yu C, Zhu D, Zhai X, Ling C. The efficacy for unresectable hepatocellular carcinoma may be improved by transcatheter arterial chemoembolization in combination with a traditional Chinese herbal medicine formula: a retrospective study. Cancer. 2009;115:5132-5138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 76. | Lin LZ, Zhou DH, Liu K, Wang FJ, Lan SQ, Ye XW. [Analysis on the prognostic factors in patients with large hepatocarcinoma treated by shentao ruangan pill and hydroxycamptothecine]. Zhongguo Zhongxiyi Jiehe Zazhi. 2005;25:8-11. [PubMed] |
| 77. | Shao ZX, Cheng ZG, Yin X. [Clinical study on treatment of middle-advanced stage liver cancer by combined treatment of hepatic artery chemoembolization with gan’ai no. I and no. II]. Zhongguo Zhongxiyi Jiehe Zazhi. 2001;21:168-170. [PubMed] |
| 78. | Wu GL, Zhang L, Li TY, Chen J, Yu GY, Li JP. Short-term effect of combined therapy with Jinlong Capsule and transcatheter arterial chemoembolization on patients with primary hepatic carcinoma and its influence on serum osteopontin expression. Chin J Integr Med. 2010;16:109-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 79. | Hou EC, Lu YX. [Primary hepatocarcinoma treated by traditional Chinese medicine combined with transcatheter arterial chemoembolization]. Zhongguo Zhongxiyi Jiehe Zazhi. 2009;29:225-227. [PubMed] |
| 80. | Gao WB, Han JD, Du M. [Observation on efficiency of shelian capsule as adjuvant of embolismic chemotherapy on primary hepatic carcinoma]. Zhongguo Zhongxiyi Jiehe Zazhi. 2005;25:980-982. [PubMed] |
| 81. | Lao Y. [Clinical study on effect of matrine injection to protect the liver function for patients with primary hepatic carcinoma after trans-artery chemo-embolization (TAE)]. Zhong Yao Cai. 2005;28:637-638. [PubMed] |
| 82. | Zhang B, Huang G, Zhang Y, Chen X, Hu P, Xu B. [Clinical observation on prevention of “jia wei si jun zi tang” from damage of hepatic reserving function after intervention of liver cancer]. Zhong Yao Cai. 2004;27:387-389. [PubMed] |
| 83. | Cheng JH, Chang G, Wu WY. [A controlled clinical study between hepatic arterial infusion with embolized curcuma aromatic oil and chemical drugs in treating primary liver cancer]. Zhongguo Zhongxiyi Jiehe Zazhi. 2001;21:165-167. [PubMed] |
| 84. | Zheng C, Feng G, Liang H. Bletilla striata as a vascular embolizing agent in interventional treatment of primary hepatic carcinoma. Chin Med J (Engl). 1998;111:1060-1063. [PubMed] |
| 85. | Zheng C, Feng G, Zhou R. [New use of Bletilla striata as embolizing agent in the intervention treatment of hepatic carcinoma]. Zhonghua Zhongliu Zazhi. 1996;18:305-307. [PubMed] |
| 86. | Lou HZ, Pan HM, Jin W. [Clinical study on treatment of primary liver cancer by Aidi injection combined with cool-tip radiofrequency ablation]. Zhongguo Zhongxiyi Jiehe Zazhi. 2007;27:393-395. [PubMed] |
| 87. | Wang WR, Cui SD, Zeng LM. Clinical observation on treatment of mid-advanced patients with hepatocarcinoma by Xiao’aiping combined with ultrasound guided percutaneous radio-frequency. Zhongguo Zhongxiyi Jiehe Zazhi. 2003;2:19-21. |
| 88. | Zhang YW. Combinational treatment with ultrasound-guided percutaneous radiofrequency and Tianzhicao capsule in 90 cases patients with hepatocarcinoma. Dangdai Yixue. 2010;16:6-8. |
| 89. | Liu XT, Liu JB, Zhang ZQ, Liu SY. Jinlong capsule clinical observation of radiofrequency ablation technique for the treatment of primary liver cancer. Shoudu Yiyao. 2013;47-48. |
| 90. | Zhao HJ, Du J, Chen X. [Clinical study of Fuzheng Yiliu Recipe combined with microwave ablation on hepatocellular carcinoma]. Zhongguo Zhongxiyi Jiehe Zazhi. 2012;32:32-34. [PubMed] |
| 91. | Lin JJ, Jin CN, Zheng ML, Ouyang XN, Zeng JX, Dai XH. Clinical study on treatment of primary hepatocellular carcinoma by Shenqi mixture combined with microwave coagulation. Chin J Integr Med. 2005;11:104-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 92. | Guo ZJ, Lin JJ, Jin CY, Zhong YS. Clinical observation of combinational treatment with Aidi injection and microwave ablation in hepatocarcinoma patients. Zhongyiyao Tongbao. 2006;5:51-54. |
| 93. | Zhang SC, Li J, Yang LJ, Fan LH, Wang CX, Wang RC, He YS. Effect of Qiankun capsule combined with high-intensity focused ultrasound on the immunological function of patients with primary liver cancer. Zhongguo Zhongyi Jichu Yixue Zazhi. 2005;11:367-380. |
| 94. | Pan JY, Ma J, Jia L, Zhou YJ, Li YY. Effects of Fu-Zhen-Yang-Yin formula combination with high-intensity focused ultrasound in advanced liver cancer patients. Shijie Huaren Xiaohua Zazhi. 2004;12:1750-1751. |
| 95. | Wang XW, Chan RH. Effects of Syndrome differentiation based herbal therapy combination with sorafenib in patients with advanced hepatocarcinoma. Zhongguo Yiyao Daobao. 2008;5:48-49. |
| 96. | Feng LH, Chen YD, Zheng ZG, Gao YQ. Clinical observation of patients with primary liver cancer treated by sorafenib combined cinobufagin tablets. Zhongguo Aizheng Zazhi. 2012;22:856-859. |
| 97. | Tian HQ, Li HL, Wang B, Liang GW, Huang XQ, Huang ZQ, Lang JM, Zhang YP, Chen XZ, Chen YS. Treatment of middle/late stage primary hepatic carcinoma by Chinese medicine comprehensive therapy: A prospective randomized controlled study. Chin J Integr Med. 2010;16:102-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 98. | Xu K, Luo HY, Li LN. [Clinical study on comprehensive treatment of primary liver cancer mainly with chinese medicinal perfusion/embolization]. Zhongguo Zhongxiyi Jiehe Zazhi. 2005;25:299-302. [PubMed] |
| 99. | Huang Z, Wang Y, Chen J, Wang R, Chen Q. Effect of Xiaoaiping injection on advanced hepatocellular carcinoma in patients. J Tradit Chin Med. 2013;33:34-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 100. | Chen Z, Zhai XF, Su YH, Wan XY, Li J, Xie JM, Gao B. [Clinical observation of cinobufacini injection used to treat moderate and advanced primary liver cancer]. Zhongxiyi Jiehe Xuebao. 2003;1:184-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 101. | Chu YP, Shen L, Bai Y. Efficacy observation of liver cancer at the later stage for the elderly treated with integration of Norcantharidin and Chinese medicine. Shijie Zhongxiyi Jiehe Xuebao. 2012;7:765-767. |
| 102. | Xu RQ, Huang ZF, Li HZ, Wei JS, Zhang ZJ, Xiang LY, Gui HT, Tan QQ. Effects of Jianpi Fuzheng decoction on symptom and immune function in patients with advanced liver cancer. Zhongxiyi Jiehe Ganbing Zazhi. 2013;23:73-75. |
| 103. | Chen QS, ChenY , Pei RQ, Huang WZ, Li CY, Zhou B, Chen YY. Clinical observation of 30 cases of late-stage primary hepatic cancer treated with Jianpi Yiliu Decoction. Shijie Zhongxiyi Jiehe Zazhi. 2013;8:368-370. |
| 104. | Yang YK, Qiu DZ, Wang GH, Gu XX, Fan Y, Tang CL. Clinical study on Jiawei Yiguanjian for improvement of the survival rate in advanced hepatocellular carcinoma patients. Zhongguo Linchuang Yixue. 2011;18:818-820. |
| 105. | Li X, Guan YS, Zhou XP, Sun L, Liu Y, He Q, Fu L, Mao YQ. [Anticarcinogenic effect of 20(R)-ginsenoside Rg3 on induced hepatocellular carcinoma in rats]. Sichuan Daxue Xuebao Yixueban. 2005;36:217-220. [PubMed] |
| 106. | Chao JC, Chiang SW, Wang CC, Tsai YH, Wu MS. Hot water-extracted Lycium barbarum and Rehmannia glutinosa inhibit proliferation and induce apoptosis of hepatocellular carcinoma cells. World J Gastroenterol. 2006;12:4478-4484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 70] [Cited by in RCA: 59] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 107. | Chen YL, Jian MH, Lin CC, Kang JC, Chen SP, Lin PC, Hung PJ, Chen JR, Chang WL, Lin SZ. The induction of orphan nuclear receptor Nur77 expression by n-butylenephthalide as pharmaceuticals on hepatocellular carcinoma cell therapy. Mol Pharmacol. 2008;74:1046-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 108. | Li S, Dong P, Wang J, Zhang J, Gu J, Wu X, Wu W, Fei X, Zhang Z, Wang Y. Icariin, a natural flavonol glycoside, induces apoptosis in human hepatoma SMMC-7721 cells via a ROS/JNK-dependent mitochondrial pathway. Cancer Lett. 2010;298:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 109. | Hsu SH, Tsai TR, Lin CN, Yen MH, Kuo KW. Solamargine purified from Solanum incanum Chinese herb triggers gene expression of human TNFR I which may lead to cell apoptosis. Biochem Biophys Res Commun. 1996;229:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 110. | Zhang YN, Liu L, Ling CQ. [Inhibition effect of active fraction from Actinidia valvata on growth of transplanated mouse tumor cells and preliminary study of its mechanism]. Zhongguo Zhongyao Zazhi. 2006;31:918-920. [PubMed] |
| 111. | Lin JM, Liu Y, Luo RC. [Inhibition activity of Scutellariae barbata extracts against human hepatocellular carcinoma cells]. Nanfang Yike Daxue Xuebao. 2006;26:591-593. [PubMed] |
| 112. | Sa F, Gao JL, Fung KP, Zheng Y, Lee SM, Wang YT. Anti-proliferative and pro-apoptotic effect of Smilax glabra Roxb. extract on hepatoma cell lines. Chem Biol Interact. 2008;171:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 113. | Li Y, Li MY, Wang L, Jiang ZH, Li WY, Li H. [Induction of apoptosis of cultured hepatocarcinoma cell by essential oil of Artemisia Annul L]. Sichuan Daxue Xuebao Yixueban. 2004;35:337-339. [PubMed] |
| 114. | Huang D, Zhang W, Huang D, Wu J. Antitumor activity of the aqueous extract from Sedum sarmentosum Bunge in vitro. Cancer Biother Radiopharm. 2010;25:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 115. | Xie Q, Yang Y, Wang Z, Chen F, Zhang A, Liu C. Resveratrol-4-O-D-(2’-galloyl)-glucopyranoside isolated from Polygonum cuspidatum exhibits anti-hepatocellular carcinoma viability by inducing apoptosis via the JNK and ERK pathway. Molecules. 2014;19:1592-1602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 116. | Hu YQ, Tan RX, Chu MY, Zhou J. Apoptosis in human hepatoma cell line SMMC-7721 induced by water-soluble macromolecular components of Artemisia capillaris Thunberg. Jpn J Cancer Res. 2000;91:113-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 117. | Liu J, Shen HM, Ong CN. Salvia miltiorrhiza inhibits cell growth and induces apoptosis in human hepatoma HepG(2) cells. Cancer Lett. 2000;153:85-93. [PubMed] |
| 118. | Lee SM, Li ML, Tse YC, Leung SC, Lee MM, Tsui SK, Fung KP, Lee CY, Waye MM. Paeoniae Radix, a Chinese herbal extract, inhibit hepatoma cells growth by inducing apoptosis in a p53 independent pathway. Life Sci. 2002;71:2267-2277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 106] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 119. | Du Q, Hu B, An HM, Shen KP, Xu L, Deng S, Wei MM. Synergistic anticancer effects of curcumin and resveratrol in Hepa1-6 hepatocellular carcinoma cells. Oncol Rep. 2013;29:1851-1858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 120. | Chen F, Yang L, Wang XK, Zhang Y. Effects of the Alkaloids of Pinellia ternata on Proliferation of Human Hepatocarcinoma Cell Strain Bel-7402. Zhongguo Yaofang. 2011;43:4048-4050. |
| 121. | Yang ZH, Yin JY, Wei ZR, Yan WQ. Extract of Tian-Nan-Xing (Arisaema heterophyllum) induces apoptosis in human hepatocarcinoma SMMC-7721 cells and its mechanism. Zhongguo Laonianxue Zazhi. 2007;27:142-144. |
| 122. | Wang Y, Deng L, Zhong H, Wang Y, Jiang X, Chen J. Natural plant extract tubeimoside I promotes apoptosis-mediated cell death in cultured human hepatoma (HepG2) cells. Biol Pharm Bull. 2011;34:831-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 123. | Kwon KB, Kim EK, Lim JG, Jeong ES, Shin BC, Jeon YS, Kim KS, Seo EA, Ryu DG. Molecular mechanisms of apoptosis induced by Scorpio water extract in human hepatoma HepG2 cells. World J Gastroenterol. 2005;11:943-947. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 124. | Chang C, Zhu YQ, Mei JJ, Liu SQ, Luo J. Involvement of mitochondrial pathway in NCTD-induced cytotoxicity in human hepG2 cells. J Exp Clin Cancer Res. 2010;29:145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 125. | Hu H, Chen D, Li Y, Zhang X. Effect of polypeptides in bee venom on growth inhibition and apoptosis induction of the human hepatoma cell line SMMC-7721 in-vitro and Balb/c nude mice in-vivo. J Pharm Pharmacol. 2006;58:83-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 126. | Song Q, Zhao JX, Zhu YZ. [Effect of fuzheng yiliu granule on H22 tumor cell apoptosis, p53 and caspase-3 gene expression in mice]. Zhongguo Zhongxiyi Jiehe Zazhi. 2005;25:338-341. [PubMed] |
| 127. | Zhao JX, Guo FL, Bai DC, Wang XX. [Effects of fuzheng yiliu granules on apoptotic rate and mitochondrial membrane potential of hepatocellular carcinoma cell line H22 from mice]. Zhongxiyi Jiehe Xuebao. 2006;4:271-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 128. | Zhang YY, Liu FY, Zhang HL. Study on Apoptosis of hepatica carcinoma cell induced by Fuganchun 6 in Vitro. Hebei Beifang Xueyuan Xuebao Yixueban. 2009;26:6-10. |
| 129. | Zhong Y, Luo CL, An-Jun Z. [Effect of bushen jianpi decoction and its disassemble recipes on tumor growth in mice with transplanted primary hepatic carcinoma]. Zhongguo Zhongxiyi Jiehe Zazhi. 2011;31:213-217. [PubMed] |
| 130. | Zhang X, Liu DQ, Liu YZ, Wang P, Chen XY. [Preliminary study on apoptosis of BEL-7402 cells induced by Chinese herbs for warming yang and dispersing stasis]. Zhongguo Zhongyao Zazhi. 2000;25:428-430. [PubMed] |
| 131. | Jiang ZY, Hua HQ, Yang AZ, Qin SK. Effects of Fufangkushen Injection in combination with oxaliplatin and recombinant human endostatin injection on apoptosis in human hepatoma cell line SMMC-7721. Shijie Huaren Xiaohua Zazhi. 2010;18:3396-3401. |
| 132. | Huang XY, Wang L, Huang ZL, Zheng Q, Li QS, Tang ZY. Herbal extract “Songyou Yin” inhibits tumor growth and prolongs survival in nude mice bearing human hepatocellular carcinoma xenograft with high metastatic potential. J Cancer Res Clin Oncol. 2009;135:1245-1255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 133. | Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51728] [Cited by in RCA: 47059] [Article Influence: 3361.4] [Reference Citation Analysis (5)] |
| 134. | Tsai YC, Wu WB, Chen BH. Preparation of carotenoids and chlorophylls from Gynostemma pentaphyllum (Thunb.) Makino and their antiproliferation effect on hepatoma cell. J Med Food. 2010;13:1431-1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 135. | Tsai YC, Lin CL, Chen BH. Preparative chromatography of flavonoids and saponins in Gynostemma pentaphyllum and their antiproliferation effect on hepatoma cell. Phytomedicine. 2010;18:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 136. | Lin SB, Li CH, Lee SS, Kan LS. Triterpene-enriched extracts from Ganoderma lucidum inhibit growth of hepatoma cells via suppressing protein kinase C, activating mitogen-activated protein kinases and G2-phase cell cycle arrest. Life Sci. 2003;72:2381-2390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 153] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 137. | Lin JM, Liu Y, Luo RC. [Effect of Scutellaria barbata extract against human hepatocellular Hep-G2 cell proliferation and its mechanism]. Nanfang Yike Daxue Xuebao. 2006;26:975-977. [PubMed] |
| 138. | Ye F, Che Y, McMillen E, Gorski J, Brodman D, Saw D, Jiang B, Zhang DY. The effect of Scutellaria baicalensis on the signaling network in hepatocellular carcinoma cells. Nutr Cancer. 2009;61:530-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 139. | Xie RF, Li ZC, Gao B, Shi ZN, Zhou X. Bufothionine, a possible effective component in cinobufocini injection for hepatocellular carcinoma. J Ethnopharmacol. 2012;141:692-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 140. | Shi P, Huang Z, Chen G. Rhein induces apoptosis and cell cycle arrest in human hepatocellular carcinoma BEL-7402 cells. Am J Chin Med. 2008;36:805-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 141. | Hsu YL, Kuo PL, Tzeng TF, Sung SC, Yen MH, Lin LT, Lin CC. Huang-lian-jie-du-tang, a traditional Chinese medicine prescription, induces cell-cycle arrest and apoptosis in human liver cancer cells in vitro and in vivo. J Gastroenterol Hepatol. 2008;23:e290-e299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 142. | Kao ST, Yeh CC, Hsieh CC, Yang MD, Lee MR, Liu HS, Lin JG. The Chinese medicine Bu-Zhong-Yi-Qi-Tang inhibited proliferation of hepatoma cell lines by inducing apoptosis via G0/G1 arrest. Life Sci. 2001;69:1485-1496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 66] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 143. | Cao Z, Lin W, Huang Z, Chen X, Zhao J, Zheng L, Ye H, Liu Z, Liao L, Du J. Ethyl acetate extraction from a Chinese herbal formula, Jiedu Xiaozheng Yin, inhibits the proliferation of hepatocellular carcinoma cells via induction of G0/G1 phase arrest in vivo and in vitro. Int J Oncol. 2013;42:202-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 144. | Deng S, Hu B, An HM. Traditional Chinese Medicinal Syndromes and treatment in colorectal cancer. J Cancer Ther. 2012;3:888-897. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 145. | Wang Z, Han W, Sui X, Fang Y, Pan H. Autophagy: A novel therapeutic target for hepatocarcinoma (Review). Oncol Lett. 2014;7:1345-1351. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 146. | Lin HM, Tseng HC, Wang CJ, Chyau CC, Liao KK, Peng PL, Chou FP. Induction of autophagy and apoptosis by the extract of Solanum nigrum Linn in HepG2 cells. J Agric Food Chem. 2007;55:3620-3628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 147. | Zhang DM, Liu JS, Deng LJ, Chen MF, Yiu A, Cao HH, Tian HY, Fung KP, Kurihara H, Pan JX. Arenobufagin, a natural bufadienolide from toad venom, induces apoptosis and autophagy in human hepatocellular carcinoma cells through inhibition of PI3K/Akt/mTOR pathway. Carcinogenesis. 2013;34:1331-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 176] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 148. | Miao Q, Bi LL, Li X, Miao S, Zhang J, Zhang S, Yang Q, Xie YH, Zhang J, Wang SW. Anticancer Effects of Bufalin on Human Hepatocellular Carcinoma HepG2 Cells: Roles of Apoptosis and Autophagy. Int J Mol Sci. 2013;14:1370-1382. [PubMed] |
| 149. | Chu YL, Ho CT, Chung JG, Rajasekaran R, Sheen LY. Allicin induces p53-mediated autophagy in Hep G2 human liver cancer cells. J Agric Food Chem. 2012;60:8363-8371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 150. | Gong K, Zhang Z, Chen Y, Shu HB, Li W. Extracellular signal-regulated kinase, receptor interacting protein, and reactive oxygen species regulate shikonin-induced autophagy in human hepatocellular carcinoma. Eur J Pharmacol. 2014;738:142-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 151. | Muehlich S, Gudermann T. Pro-senescence therapy for hepatocellular carcinoma. Aging (Albany NY). 2013;5:639-640. [PubMed] |
| 152. | Hu B, An HM, Shen KP, Xu L, DU Q, Deng S, Wu Y. Liver Yin deficiency tonifying herbal extract induces apoptosis and cell senescence in Bel-7402 human hepatocarcinoma cells. Exp Ther Med. 2012;3:80-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 153. | Chang UM, Li CH, Lin LI, Huang CP, Kan LS, Lin SB. Ganoderiol F, a ganoderma triterpene, induces senescence in hepatoma HepG2 cells. Life Sci. 2006;79:1129-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 154. | Hu B, Du Q, Deng S, An HM, Pan CF, Shen KP, Xu L, Wei MM, Wang SS. Ligustrum lucidum Ait. fruit extract induces apoptosis and cell senescence in human hepatocellular carcinoma cells through upregulation of p21. Oncol Rep. 2014;32:1037-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 155. | Cao L, Han L, Zhang Z, Li J, Qu Z, Du J, Liang X, Liu Y, Liu H, Shi Y. Involvement of anoikis-resistance in the metastasis of hepatoma cells. Exp Cell Res. 2009;315:1148-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 156. | Hu B, An HM, Shen KP, Xu L, Du Q, Deng S, Wu Y. Modified Yi Guan Jian, a Chinese herbal formula, induces anoikis in Bel-7402 human hepatocarcinoma cells in vitro. Oncol Rep. 2011;26:1465-1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 157. | Hu B, An HM, Shen KP, Song HY, Deng S. Polygonum cuspidatum Extract Induces Anoikis in Hepatocarcinoma Cells Associated with Generation of Reactive Oxygen Species and Downregulation of Focal Adhesion Kinase. Evid Based Complement Alternat Med. 2012;2012:607675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 158. | Cheng HL, Su SJ, Huang LW, Hsieh BS, Hu YC, Hung TC, Chang KL. Arecoline induces HA22T/VGH hepatoma cells to undergo anoikis - involvement of STAT3 and RhoA activation. Mol Cancer. 2010;9:126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 159. | Wang N, Feng Y, Lau EP, Tsang C, Ching Y, Man K, Tong Y, Nagamatsu T, Su W, Tsao S. F-actin reorganization and inactivation of rho signaling pathway involved in the inhibitory effect of Coptidis Rhizoma on hepatoma cell migration. Integr Cancer Ther. 2010;9:354-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 160. | Xiao XL, Wang XY, Pu X, Guo QX, Long HA. Effect of Baicalein on the in Vitro migration and invasion of human hepatocellular carcinoma cell line SMMC-7721. Zhongguo Zhongliu Linchuang. 2012;39:305-309. |
| 161. | Yu HB, Zhang HF, Li DY, Zhang X, Xue HZ, Zhao SH. Matrine inhibits matrix metalloproteinase-9 expression and invasion of human hepatocellular carcinoma cells. J Asian Nat Prod Res. 2011;13:242-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 162. | Wei PL, Tu CC, Chen CH, Ho YS, Wu CT, Su HY, Chen WY, Liu JJ, Chang YJ. Shikonin suppresses the migratory ability of hepatocellular carcinoma cells. J Agric Food Chem. 2013;61:8191-8197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 163. | Chen D, Yao WJ, Zhang XL, Han XQ, Qu XY, Ka WB, Sun DG, Wu XZ, Wen ZY. Effects of Gekko sulfated polysaccharide-protein complex on human hepatoma SMMC-7721 cells: inhibition of proliferation and migration. J Ethnopharmacol. 2010;127:702-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 164. | Lou L, Ye W, Chen Y, Wu S, Jin L, He J, Tao X, Zhu J, Chen X, Deng A. Ardipusilloside inhibits survival, invasion and metastasis of human hepatocellular carcinoma cells. Phytomedicine. 2012;19:603-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 165. | Cao XC, Wang H, Zhang HM, Liu YW, Lu ZX. The effects of plumbagin on proliferation and metastasis in human liver cancer SK-hep-1 cells. Zhongguo Aizheng Zazhi. 2013;23:721-727. |
| 166. | Yuxian X, Feng T, Ren L, Zhengcai L. Tanshinone II-A inhibits invasion and metastasis of human hepatocellular carcinoma cells in vitro and in vivo. Tumori. 2009;95:789-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 167. | Jia QA, Wang ZM, Ren ZG, Bu Y, Xie XY, Wang YH, Zhang L, Zhang QB, Xue TC, Deng LF. Herbal compound “Songyou Yin” attenuates hepatoma cell invasiveness and metastasis through downregulation of cytokines secreted by activated hepatic stellate cells. BMC Complement Altern Med. 2013;13:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 168. | Cheng Y, He SQ, Zhu Y, Fan Q, Yang S, Chen R. [Blejiajian pill inhibited the proliferation, adhesion, and invasion of hepatoma carcinoma cells: an experimental research]. Zhongguo Zhongxiyi Jiehe Zazhi. 2013;33:664-667. [PubMed] |
| 169. | Liu X, Yang Y, Zhang X, Xu S, He S, Huang W, Roberts MS. Compound Astragalus and Salvia miltiorrhiza extract inhibits cell invasion by modulating transforming growth factor-beta/Smad in HepG2 cell. J Gastroenterol Hepatol. 2010;25:420-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 170. | Ding XM, Cheng ZR. Study on inhibitory effect of Shehuang Xiaoliu Fang on invasive and adhesive ability of liver cancer cells. Zhongxiyi Jiehe Ganbing Zazhi. 2006;16:96-98. |
| 171. | He YL, Ying Y, Xu YL, Su JF, Luo H, Wang HF. [Effects of Lycium barbarum polysaccharide on tumor microenvironment T-lymphocyte subsets and dendritic cells in H22-bearing mice]. Zhongxiyi Jiehe Xuebao. 2005;3:374-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 172. | Chiu JH, Ju CH, Wu LH, Lui WY, Wu CW, Shiao MS, Hong CY. Cordyceps sinensis increases the expression of major histocompatibility complex class II antigens on human hepatoma cell line HA22T/VGH cells. Am J Chin Med. 1998;26:159-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 173. | Dai ZJ, Liu XX, Tang W, Xue Q, Wang XJ, Ji ZZ, Kang HF, Diao Y. [Antitumor and immune-modulating effects of Scutellaria barbata extract in mice bearing hepatocarcinoma H22 cells-derived tumor]. Nanfang Yike Daxue Xuebao. 2008;28:1835-1837. [PubMed] |
| 174. | Chen YT, Lin MA, Cheng DQ, Shi ZJ, Zhu JL, Wu J. [Effect of proteins extracted from mycelia of Omphalia lapidescens on inhibiting H, liver cancer in mice and regulating immune function]. Zhongyaocai. 2009;32:1870-1874. [PubMed] |
| 175. | Li J, Xie M, Gan Y. [Effect of Xiaochaihu decoction and different herbal formulation of component on inhibiting H22 liver cancer in mice and enhancing immune function]. Zhongguo Zhongyao Zazhi. 2008;33:1039-1044. [PubMed] |
| 176. | Zhou AG, Zhang Y, Kong DY, Wang Y, Zhang HZ, Wang SJ, Kui G, Hong S, Ge HL, Ren QH. [Tumor inhibiting and immunoloregulation effects of Mylabris Mixture on H22 cancer-bearing mice]. Zhongxiyi Jiehe Xuebao. 2006;4:504-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 177. | Cao ZY, Chen XZ, Liao LM, Peng J, Hu HX, Liu ZZ, Du J. Fuzheng Yiliu Granule inhibits the growth of hepatocellular cancer by regulating immune function and inducing apoptosis in vivo and in vitro. Chin J Integr Med. 2011;17:691-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 178. | Li XJ, Mao YX, Zhang HL, Wang JX, Liu FY. [Study on effects of anticancer and immunoregulation of Fuganchun 6 on hepatoma of mouse]. Zhongguo Zhongyao Zazhi. 2006;31:1622-1625. [PubMed] |
| 179. | Chen JR, Li EQ, Dai CQ, Yu B, Wu XL, Huang CR, Chen XY. The inducible effect of LBP on maturation of dendritic cells and the related immune signaling pathways in hepatocellular carcinoma (HCC). Curr Drug Deliv. 2012;9:414-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 180. | Chen D, Zhang X, Du Y, Jia B, Ka W, Sun D, Yao W, Wen Z. Effects of Gekko sulfated polysaccharide-protein complex on the defective biorheological characters of dendritic cells under tumor microenvironment. Cell Biochem Biophys. 2012;62:193-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 181. | He X, Li X, Liu B, Xu L, Zhao H, Lu A. Down-regulation of Treg cells and up-regulation of TH1/TH2 cytokine ratio were induced by polysaccharide from Radix Glycyrrhizae in H22 hepatocarcinoma bearing mice. Molecules. 2011;16:8343-8352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 182. | Deng S, Hu B, An HM, Du Q, Xu L, Shen KP, Shi XF, Wei MM, Wu Y. Teng-Long-Bu-Zhong-Tang, a Chinese herbal formula, enhances anticancer effects of 5--Fluorouracil in CT26 colon carcinoma. BMC Complement Altern Med. 2013;13:128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 183. | Bishayee A, Darvesh AS. Angiogenesis in hepatocellular carcinoma: a potential target for chemoprevention and therapy. Curr Cancer Drug Targets. 2012;12:1095-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 184. | Song P, Wang XM, Xie S. [Experimental study on mechanisms of lyophilized powder of fresh gekko Chinenis in inhibiting H22 hepatocarcinoma angiogenesis]. Zhongguo Zhongxiyi Jiehe Zazhi. 2006;26:58-62. [PubMed] |
| 185. | Zhang SX, Zhu C, Ba Y, Chen D, Zhou XL, Cao R, Wang LP, Ren Y, Wu XZ. Gekko-sulfated glycopeptide inhibits tumor angiogenesis by targeting basic fibroblast growth factor. J Biol Chem. 2012;287:13206-13215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 186. | Feng GS, Li X, Zheng CS, Zhou CK, Liu X, Wu HP. [Mechanism of inhibition of tumor angiogenesis by Bletilla colloid: an experimental study]. Zhonghua Yixue Zazhi. 2003;83:412-416. [PubMed] |
| 187. | Ren J, Zheng C, Feng G, Liang H, Xia X, Fang J, Duan X, Zhao H. Inhibitory effect of extract of fungi of Huaier on hepatocellular carcinoma cells. J Huazhong Univ Sci Technolog Med Sci. 2009;29:198-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 188. | Liu SJ, Shen WL, Liu XL, Wen J, Cui YZ. Anti-angiogenesis effects of Fu-Zheng-Kang-Ai-Tang in the treatment of hepatocarcinoma. Shijie Huaren Xiaohua Zazhi. 2005;13:908-910. |
| 189. | Cui J, Nan KJ, Tian T, Guo YH, Zhao N, Wang L. Chinese medicinal compound delisheng has satisfactory anti-tumor activity, and is associated with up-regulation of endostatin in human hepatocellular carcinoma cell line HepG2 in three-dimensional culture. World J Gastroenterol. 2007;13:5432-5439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 190. | Chen T, Fu YL, Gong ZP, Deng LR, Hu YQ. Studies on the anti-angiogenic mechanism of the formula of Chinese medicine active ingredients combined with small dose cisplatin in mice of hepatocellular carcinoma. Zhongguo Shiyan Fangji Xue Zazhi. 2010;16:157-160. |
| 191. | Wang S, Xu X, Zhang W, Li A, Dong W. [Effects of Erbie San on Walker-256 liver cancer and adjustment to unbalance of VEGF/endostatin in rats]. Zhongguo Zhongyao Zazhi. 2009;34:89-91. [PubMed] |
| 192. | Dai Z, Liu X, Ji Z, Liu L, Kang H, Wang X, Diao Y. The effect-enhancing and toxicity-reducing action of the extract of herba Scutellariae barbatae for chemotherapy in hepatoma H22 tumor-bearing mice. J Tradit Chin Med. 2008;28:205-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 193. | Wang DH, Weng XC. [Antitumor activity of extracts of Ganoderma lucidum and their protective effects on damaged HL-7702 cells induced by radiotherapy and chemotherapy]. Zhongguo Zhongyao Zazhi. 2006;31:1618-1622. [PubMed] |
| 194. | Sun Y, Guan J, Wang Q. The influence of Cordyceps sinensis on the immunologic function of the rats with liver cancer (H22) after chemotherapy. Zhongguo Jiceng Yiyao. 2002;9:127-128. |
| 195. | You M, Luo M, Liao W, Hu S, Xu W, Jing L. [Chaiqiyigan granula enhances Taxol-induced growth inhibition of hepatocellular carcinoma xenografts in nude mice: an in vivo fluorescence imaging study]. Nanfang Yike Daxue Xuebao. 2012;32:1042-1045. [PubMed] |
| 196. | Chen T, Li D, Fu YL, Hu W. Screening of QHF formula for effective ingredients from Chinese herbs and its anti-hepatic cell cancer effect in combination with chemotherapy. Chin Med J (Engl). 2008;121:363-368. [PubMed] |
| 197. | Chen Z, Wang P, Huang WX, Liu LM. [Experimental study on effects of shengmai injection: enhancing 5-FU anti-tumor efficacy and reducing its toxicity]. Zhongxiyi Jiehe Xuebao. 2005;3:476-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 198. | Yau T, Chan P, Epstein R, Poon RT. Evolution of systemic therapy of advanced hepatocellular carcinoma. World J Gastroenterol. 2008;14:6437-6441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 43] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 199. | Tian QE, Li HD, Yan M, Cai HL, Tan QY, Zhang WY. Astragalus polysaccharides can regulate cytokine and P-glycoprotein expression in H22 tumor-bearing mice. World J Gastroenterol. 2012;18:7079-7086. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 200. | Huang C, Xu D, Xia Q, Wang P, Rong C, Su Y. Reversal of P-glycoprotein-mediated multidrug resistance of human hepatic cancer cells by Astragaloside II. J Pharm Pharmacol. 2012;64:1741-1750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 201. | Liang G, Tang A, Lin X, Li L, Zhang S, Huang Z, Tang H, Li QQ. Green tea catechins augment the antitumor activity of doxorubicin in an in vivo mouse model for chemoresistant liver cancer. Int J Oncol. 2010;37:111-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 202. | Wang XB, Wang SS, Zhang QF, Liu M, Li HL, Liu Y, Wang JN, Zheng F, Guo LY, Xiang JZ. Inhibition of tetramethylpyrazine on P-gp, MRP2, MRP3 and MRP5 in multidrug resistant human hepatocellular carcinoma cells. Oncol Rep. 2010;23:211-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 203. | Wong VK, Chiu P, Chung SS, Chow LM, Zhao YZ, Yang BB, Ko BC. Pseudolaric acid B, a novel microtubule-destabilizing agent that circumvents multidrug resistance phenotype and exhibits antitumor activity in vivo. Clin Cancer Res. 2005;11:6002-6011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 97] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 204. | Ong RC, Lei J, Lee RK, Cheung JY, Fung KP, Lin C, Ho HP, Yu B, Li M, Kong SK. Polyphyllin D induces mitochondrial fragmentation and acts directly on the mitochondria to induce apoptosis in drug-resistant HepG2 cells. Cancer Lett. 2008;261:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 205. | Chaudhary H, Jena PK, Seshadri S. Evaluation of hydro-alcoholic extract of Eclipta alba for its multidrug resistance reversal potential: an in vitro study. Nutr Cancer. 2013;65:775-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |