Published online Oct 18, 2015. doi: 10.4254/wjh.v7.i23.2492
Peer-review started: June 12, 2015
First decision: July 25, 2015
Revised: August 3, 2015
Accepted: August 30, 2015
Article in press: August 31, 2015
Published online: October 18, 2015
Processing time: 131 Days and 13.7 Hours
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) is a novel 2-stage technique intended to induce rapid growth of the future liver remnant (FLR). Initial reports of a 12% mortality rate have sparked debate regarding the safety of the procedure. A 64 years old male was planned for a right-sided hemi-hepatectomy due to colorectal cancer liver metastases. Intra-operatively it was decided to convert to an ALPPS due to unexpectedly small segments 2-4. Post-operative serum laboratory tests indicated an acute liver failure and radiological imaging showed no sign of arterial blood flow to the right hemi-liver. A computed tomography examination on post-operative day 3 revealed that the FLR had increased from 290 to 690 mL in 3 d (138% growth). In the following days serum values gradually improved and stage 2 was carried out on post-operative day 7. The rest of the hospital stay was uneventful and the patient made a full recovery. ALPPS is a fascinating advancement in liver surgery. Despite severe post-operative complications, in properly selected cases it provides successful outcomes that other modalities of treatment cannot offer.
Core tip: Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) is a novel 2-stage technique intended to induce rapid growth of the future liver remnant. Initial reports of a 12% mortality rate have sparked debate regarding the safety of the procedure. We here present a complication following ALPPS that to our knowledge has never been described before. Yet proper patient selection resulted in a full recovery following a potentially life threatening liver failure.
- Citation: Sanjeevi S, Sparrelid E, Gilg S, Jonas E, Isaksson B. Arterial ischemia in the deportalized liver following associating liver partition and portal vein ligation for staged hepatectomy. World J Hepatol 2015; 7(23): 2492-2496
- URL: https://www.wjgnet.com/1948-5182/full/v7/i23/2492.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i23.2492
Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) is a novel two-stage technique intended to induce rapid growth of the future liver remnant (FLR). Classically the technique is applied in the setting of an extended right-sided hemi-hepatectomy. The stage 1 operation involves transection of the right portal vein, followed by division of the parenchyma between the portal flow-deprived segments 4-8 and the normally vascularized FLR (segments 1-3). After a short interval (in general 7 d at our institution) and having confirmed adequate growth of the FLR, stage 2 is performed with removal of the deportalized liver[1]. Viable alternatives to ALPPS include portal vein embolization, portal vein ligation and two-stage hepatectomy[2]. The decision to perform an ALPPS procedure can also be made intra-operatively when detection of additional disease makes other forms of therapy unfeasible[3]. The procedure is applicable in a variety of liver tumors, but is utilized most often for colorectal cancer liver metastasis (CRLM)[4]. The question whether ALPPS is a superior choice compared to previously established surgical procedures is still unanswered. Initial reports of a 12% mortality rate have sparked debate regarding the safety of the procedure[5]. Large multicenter retrospective studies have studied the morbidity and mortality associated with ALPPS, but a prospective randomized control trial is yet to be performed[3,4,6].
In the following case report, we present a post-operative complication following ALPPS for CRLM, to our knowledge not previously described.
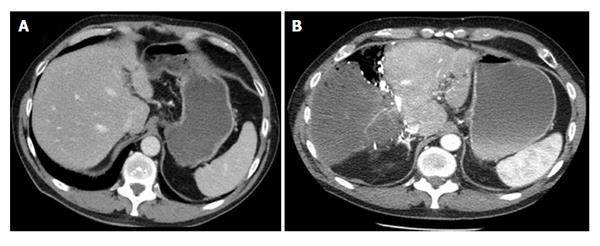
A 64 years old male with no comorbidities was diagnosed with rectal cancer at a screening colonoscopy. The tumor was staged as a T3cN0M0 and was surgically resected. A scheduled follow-up at 2 mo revealed elevated carcinoembryonic antigen levels and a computed tomography (CT) thorax/abdomen showed 9 metastatic lesions in segments 5, 6, 7 and 8. The patient received 4 cycles of FOLFOX and subsequent imaging showed marked regress of the hepatic lesions (Figure 1A). It was also noted that the right hepatic artery arose directly from the superior mesenteric artery (type III according to the Michel classification). Following 2 additional cycles of chemotherapy, the patient was planned for a right-sided hemi-hepatectomy.
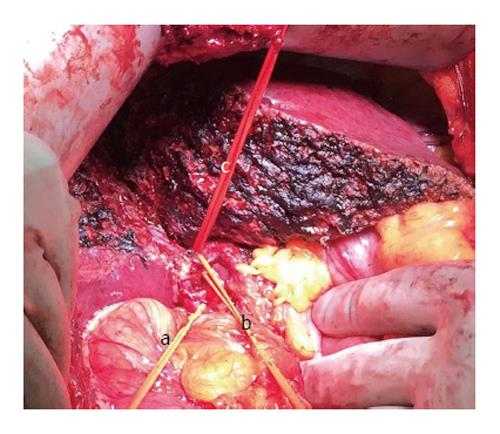
Intra-operatively, pronounced chemotherapy induced liver changes were evident with signs of sinusoidal obstruction; i.e., blue liver syndrome. Further exploration showed that segments 2, 3 and 4 were unusually small (post-operative calculation of the FLR (segments 1-4) 290 mL, giving a FLR/BW-ratio of 0.34% and a ratio of FLR/total estimated liver volume (sFLR) of 16.1% (Figure 1A). It was decided intra-operatively to deviate from the initial planned one-stage right-sided hemi-hepatectomy and to perform an ALPPS procedure with segments 1-4 as FLR. The right hepatic vein, a large inferior hepatic vein (“Makuuchi vein”), right hepatic artery and right bile duct were isolated and marked with rubber vessel loops (Figure 2). The right portal vein was divided and the liver was transected with a cavitron ultrasonic surgical aspiration. Intra-operative bleeding was 400 mL, no blood was administered intra-operatively and no hypotensive episodes were noticed during the operation.
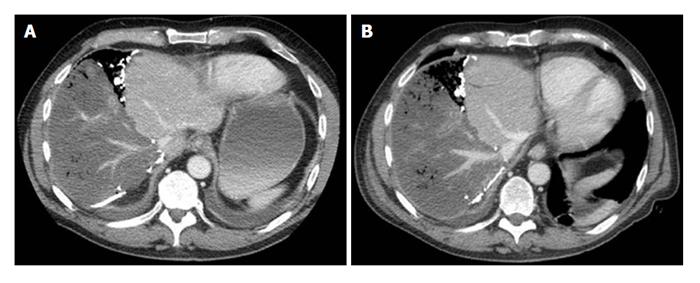
On post-operative day two, serum laboratory tests showed signs of acute liver failure and hepatic ischemia [international normalised ratio (INR) of 2.1 (ref < 1.2), bilirubin 61 μmol/L (ref < 26 μmol/L), aspartaat aminotransferase (ASAT) 131 ukat/L (ref < 0.76 ukat/L), alanine aminotransferase (ALAT) 94.2 ukat/L (ref < 1.20 ukat/L) and creatinine 140 μmol/L (ref < 100 μmol/L)] (Table 1). An ultrasound of the liver showed no sign of arterial blood flow to the right hemi-liver. Following proper rehydration, a CT examination was performed on post-operative day 3, which confirmed occlusion of the right hepatic artery and showed an ischemic right hemi-liver. It was, however, noted that the FLR had increased from 290 to 690 mL in only 3 d translating into a 138% increase of the FLR volume (Figure 1B). Already at this stage the FLR/BW-ratio was 0.8% and sFLR 38.3%. Surprisingly, on the late venous phase of the CT there was contrast enhancement in the hepatic venous system of the deportalized segments, not only in the large veins close to the inferior vena cava, but also in the peripheral vessels (Figure 3A).
| Reference intervals | INR | Bilirubin (μmol/L) | ASAT (ukat/L) | ALAT (ukat/L) | FLR (mL) | FLR/BW ratio (%) | sFLR (%) |
| < 1.2 | < 26 | < 0.76 | < 1.20 | ||||
| Pre-op day (before stage 1) | |||||||
| 1 | 1.0 | 4 | 0.51 | 0.58 | 290 | 0.4 | 16.1 |
| Post-op day (after stage 1) | |||||||
| 3 | 2.1 | 61 | 131.00 | 94.20 | 690 | 0.8 | 38.3 |
| 6 | 1.7 | 52 | 1.54 | 11.85 | 746 | 0.9 | 41.4 |
| 14 | 1.4 | 17 | 0.65 | 1.35 | - | - | - |
| 29 | 1.3 | 24 | 0.77 | 1.09 | - | - | - |
Despite impressive growth in terms of volume, the patient was clearly still in severe liver failure. The decision was taken to observe the patient and postpone stage 2 of the ALPPS procedure for as long as possible, closely monitoring the patient’s liver function during the following days. On post-operative day 6 the serum values had gradually improved and were as follows: INR 1.7, bilirubin 52 μmol/L, ASAT 1.54 ukat/L, ALAT 11.85 ukat/L (Table 1). At this point the patient fulfilled the Balzan 50-50 criteria for post-hepatectomy liver failure[7]. However, apart from some mild confusion and fever, the patient was asymptomatic. CT images now (post-operative day 6) showed signs of complete hepatic ischemia with air in the intrahepatic bile ducts. The FLR had only hypertrophied slightly since post-operative day 3 and now measured 746 mL. Once again, on the late venous phase images there was contrast-enhancement in the hepatic venous system of the deportalized segments, both in the central and peripheral vessels (Figure 3B).
Leaving the ischemic right hemi-liver for a longer period of time was considered a clear risk and the decision to proceed to stage 2 was made. Stage 2 of the ALPPS was carried out on post-operative day 7. A dark necrotic right hemi-liver was found at laparotomy (Figure 4). The right hepatic artery, bile duct and right hepatic vein were divided by staples. The right hemi-liver was removed and the abdomen was closed. No complications were experienced post-operatively and the patient recovered well. The only complaint was recurring hiccups that that ceased spontaneously 7 d after stage 2 (the patient experienced a prolonged period of unexplained hiccups even after the colectomy of the primary tumour). At this point the serum values had further improved (INR 1.4, bilirubin 17 μmol/L, ASAT 0.65 ukat/L, ALAT 1.35 ukat/L) (Table 1). The rest of the hospital stay was uneventful and the patient was discharged on post-operative day 22.
ALPPS is a relatively new technique with the mechanisms driving growth of the FLR not fully understood. Complete ischemia of the deportalized liver following ALPPS has to our knowledge never before been described. Remarkably, despite this unforeseen complication, the patient successfully underwent even the second stage of the operation and made an uneventful recovery.
Recent reports have questioned the use of ALPPS due to a morbidity of 43%-60% and mortality of 15%-20%[8-11]. A multicenter registry study by Schadde et al[4] reported severe complications (Clavien-Dindo ≥ IIIb) in 27% of patients and a 90 d mortality of 9%. Significantly better outcomes were noted in patients with CRLM and patients under the age of 60. Although our patient was 64 years old, he was previously healthy with no recorded comorbidities. Other independent risk factors included red blood cell transfusions and stage I operating times longer than 300 min, two factors our patient did not fulfill. Truant et al[6] hypothesize that complications occurring between stage 1 and 2 of ALPPS play a significant role in morbidity and mortality. More specifically, post stage 1 biliary fistula, ascites and infected bile collections worsen overall outcome. Again, our patient experienced none of the abovementioned complications and had an uncomplicated post-operative course apart from post-hepatectomy liver failure and the described liver ischemia.
Post-operative imaging showed that the FLR of the patient increased by 157% over a period of 6 d. Of greater significance is that the major part of the growth (136%) occurred in less than 3 d after stage 1. This is an impressive increase in size, considering that metabolic support from the deportalized liver was sub-optimal. Reported increases in the FLR range from an average of 49%-80% over 7 d[3,4,12]. It should be emphasized that the increase in volume does not necessarily correlate with an increase in function of the FLR[13].
Another unique aspect of this case was the post-operative venous flow noted in the deportalized right hemi-liver (Figure 3). This phenomenon may explain the subsequent improvement of serum liver values between stage 1 and 2. Additionally, an increase in venous flow was noted between post-operative days 3 and 6 (Figure 3). The source of the venous blood is however not clearly understood, considering that blood flow in the right hepatic artery was absent on imaging. A standing theory is that the right hemi-lobe received arterial blood from bile duct associated vessels with retrograde filling of the portal veins from the hepatic sinusoids[14]. Retrograde filling of the right hepatic and inferior hepatic veins could also have been possible[15].
The present case was extensively analyzed at the institutional morbidity and mortality review board. A point of criticism was the initial decision to proceed with a right-sided hemi-hepatectomy despite the small FLR. If this was pre-operatively noticed the patient may have benefited from portal vein embolization. Despite the misjudgment, the intra-operative decision to proceed with ALPPS was considered the best option for the patient. The reasoning behind the arterial occlusion was also discussed. A technical error was considered unlikely as optimal flow was palpated in the right hepatic artery prior to closure of the abdomen. It could be hypothesized that trauma during the surgery precipitated the formation of an arterial thrombus. Occlusion of the right hepatic artery has been described following liver transplantations[16]. Damage during the Pringle maneuver and the formation of a pseudoaneurysms have been proposed as underlying mechanisms.
To conclude, ALPPS is a fascinating advancement in liver surgery, requiring further studies to better our understanding. Yet, despite post-operative complications, in properly selected cases it provides successful outcomes that other modalities of treatment cannot offer.
A 64 years old male that went into severe liver failure following associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) due to arterial ischemia in the deportalized liver.
Liver failure following stage I of ALPPS due to arterial ischemia.
The diagnosis of liver failure was well established by imaging and laboratory tests. The exact mechanism for the full recovery of the patient is not completely understood.
An acute rise in international normalized ratio and serum bilirubin, alanine aminotransferase and aspartaat aminotransferase which gradually improved over time.
An ultrasound of the liver showed no sign of arterial blood flow to the right hemi-liver and a computed tomography examination confirmed occlusion of the right hepatic artery and an ischemic right hemi-liver.
Pathology following stage II of ALPPS confirmed the underlying disease to be colorectal liver metastases.
Supportive therapy.
This is the first report to describe arterial ischemia in the deportalized liver following ALPPS.
ALPPS: Associated liver partition and portal vein ligation for staged hepatectomy; FLR: Future liver remnant; CRLM: Colorectal liver metastasis.
ALPPS is a fascinating advancement in liver surgery requiring further studies to better our understanding. Despite post-operative complications, in properly selected cases it provides successful outcomes that other modalities of treatment cannot offer.
ALPPS is an interesting novel two stage surgical procedure for extended liver tumors with more and more applications described into literature: This article describes a case report of application of ALPPS procedure in a patient intraoperatively judged as not eligible to a right hepatectomy due to unexpected little remnant volume: The attention is focalized on a specific particular postoperative complication, never described previously into literature.
P- Reviewer: Campos RR, Sguinzi R, Vennarecci G S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Alvarez FA, Ardiles V, Sanchez Claria R, Pekolj J, de Santibañes E. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): tips and tricks. J Gastrointest Surg. 2013;17:814-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 132] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 2. | Hasselgren K, Sandström P, Björnsson B. Role of associating liver partition and portal vein ligation for staged hepatectomy in colorectal liver metastases: a review. World J Gastroenterol. 2015;21:4491-4498. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Jackson T, Siegel KA, Siegel CT. Rescue ALPPS: Intraoperative Conversion to ALPPS during Synchronous Resection of Rectal Cancer and Liver Metastasis. Case Rep Surg. 2014;2014:487852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Schadde E, Hernandez-Alejandro R, Lang H, de Santibaňes E, Clavien PA. ALPPS Offers a Better Chance of Complete Resection in Patients with Primarily Unresectable Liver Tumors. Results of a Multicentre Analysis: Reply. World J Surg. 2015;39:1850-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T, Goralcyk A, Hörbelt R. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255:405-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 837] [Cited by in RCA: 932] [Article Influence: 71.7] [Reference Citation Analysis (0)] |
| 6. | Truant S, Scatton O, Dokmak S, Regimbeau JM, Lucidi V, Laurent A, Gauzolino R, Castro Benitez C, Pequignot A, Donckier V. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): impact of the inter-stages course on morbi-mortality and implications for management. Eur J Surg Oncol. 2015;41:674-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 105] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 7. | Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F. The “50-50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg. 2005;242:824-828, discussion 828-829. [PubMed] |
| 8. | Sotiropoulos GC, Kouraklis G. The ALPPS procedure for extended indications in liver surgery: an old finding applied in surgical oncology. Ann Surg. 2013;257:e26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Aloia TA, Vauthey JN. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): what is gained and what is lost? Ann Surg. 2012;256:e9; author reply e16-e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 10. | Kokudo N, Shindoh J. How can we safely climb the ALPPS? Updates Surg. 2013;65:175-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Rohatgi S, Harrison EM, Powell JJ, Wigmore SJ. ALPPS: Adverse Outcomes Demand Clear Justification in an Era of Improving Survival for Colorectal Liver Metastases. World J Surg. 2015;39:1848-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg. 1966;112:337-347. [PubMed] |
| 13. | Pagano D, Gruttadauria S. Impact of future remnant liver volume on post-hepatectomy regeneration in non-cirrhotic livers. Front Surg. 2014;1:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Northover JM, Terblanche J. A new look at the arterial supply of the bile duct in man and its surgical implications. Br J Surg. 1979;66:379-384. [PubMed] |
| 15. | Pedersen JF, Dakhil AZ, Jensen DB, Søndergaard B, Bytzer P. Abnormal hepatic vein Doppler waveform in patients without liver disease. Br J Radiol. 2005;78:242-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Tanabe G, Kawaida K, Hamanoue M, Kihara K, Hirata S, Maemura M, Ueno S, Aikou T. Treatment for accidental occlusion of the hepatic artery after hepatic resection: report of two cases. Surg Today. 1999;29:268-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |