Published online Jul 28, 2015. doi: 10.4254/wjh.v7.i15.1913
Peer-review started: February 22, 2015
First decision: April 27, 2015
Revised: May 2, 2015
Accepted: June 4, 2015
Article in press: June 8, 2015
Published online: July 28, 2015
Processing time: 168 Days and 23.2 Hours
The current management therapies for hepatocellular carcinoma (HCC) patients are discussed in this review. Despite the development of new therapies, HCC remains a “difficult to treat” cancer because HCC typically occurs in advanced liver disease or hepatic cirrhosis. The progression of multistep and multicentric HCC hampers the prevention of the recurrence of HCC. Many HCC patients are treated with surgical resection and radiofrequency ablation (RFA), although these modalities should be considered in only selected cases with a certain HCC number and size. Although there is a shortage of grafts, liver transplantation has the highest survival rates for HCC. Several modalities are salvage treatments; however, intensive care in combination with other modalities or in combination with surgical resection or RFA might offer a better prognosis. Sorafenib is useful for patients with advanced HCC. In the near future, HCC treatment will include stronger molecular targeted drugs, which will have greater potency and fewer adverse events. Further studies will be ongoing.
Core tip: Liver transplantation is the first-line treatment of hepatocellular carcinoma (HCC). Surgical resection and radiofrequency ablation (RFA) are second-line HCC treatments. Surgical resection and RFA should only be considered for selected cases. Sorafenib administration, transarterial chemoembolization, stereotactic body radiation treatments, or proton or carbon ion treatments are available as salvage treatments for HCC. Laparoscopic liver resection appears to offer at least a short-term benefit in selected HCC patients. These HCC treatments should be carefully selected or combined in clinical practice.
- Citation: Kanda T, Ogasawara S, Chiba T, Haga Y, Omata M, Yokosuka O. Current management of patients with hepatocellular carcinoma. World J Hepatol 2015; 7(15): 1913-1920
- URL: https://www.wjgnet.com/1948-5182/full/v7/i15/1913.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i15.1913
Globally, hepatocellular carcinoma (HCC) is a common malignancy with a poor prognosis worldwide, and the incidence of HCC is increasing in the United States[1,2]. In Asian countries, HCC is caused by hepatitis B virus (HBV) or hepatitis C virus (HCV) infection[3-6]. Despite the ongoing development of new therapies, HCC remains a “difficult to treat” cancer[7] because the malignancy typically occurs in advanced liver disease or hepatic cirrhosis. In HCC treatments, such as surgical resection or percutaneous local ablation therapy, the liver function should always be considered[8-12]. The recurrence of HCC within 5 years after primary resection is as high as 70% because multistep and multicentric HCC develops most frequently after a resection or ablation treatment in patients with chronic liver disease[13,14].
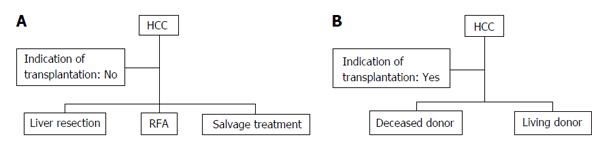
The tumor status and liver function reserve of HCC patients determine whether a hepatectomy should be performed[9] (Figure 1A). Careful attention should be focused on the selection of appropriate candidates. Makuuchi’s criteria for the selection of the operative procedures in patients with HCC and liver cirrhosis are available in Japan[8,15]. The criteria comprise the existence of ascites, the serum total bilirubin and indocyanine green (ICG) clearance rates. In patients without ascites and with total bilirubin levels < 2 mg/dL, a hepatectomy could be safely performed. Serum total bilirubin levels (< 1 mg/dL) and a normal range (10%-19%, 20%-29%, or ≥ 30%) of ICG retention at 15 min suggest a trisegmentectomy or right hepatectomy, left hepatectomy or right segmentectomy, subsegmentectomy, or limited resection, respectively. Patients with serum total bilirubin levels of 1.1-1.9 mg/dL could receive a limited liver resection safely. Small HCC is a clinical entity with a high surgical cure rate[9]. Yamazaki et al[9] reported that the 5-year survival following a hepatectomy is 53%, with 26% morbidity and 0% mortality in patients within the Makuuchi’s criteria; however, they reported that the 5-year survival in HCC patients in major institutions worldwide is 37%-53% following a hepatectomy, with 11%-45% morbidity and 0%-10% mortality. A hepatic venous pressure gradient ≥ 10 mmHg as a direct measurement of relevant portal hypertension could be useful[16,17] because the concept of portal hypertension as a prognostic factor in patients undergoing resection has been validated[18]. An accepted application to measure and quantitate the liver reserve is debatable, and further studies are required.
The prognosis of patients with a portal vein tumor thrombus, which typically is poor, might be improved by surgical resection with or without pre-operative transarterial chemoembolization (TACE)[19,20]. A combination of aggressive surgical treatment and effective preoperative TACE for HCC with major vascular tumor invasion including invasion of the main trunk, the first-order branch of the portal vein, or the inferior vena cava might be beneficial for certain patients[19,21]. Because chemotherapy or antiviral treatment could be administered, a concomitant splenectomy and hepatectomy might extend the criteria for surgery in “selected” HCC patients with hypersplenism[22].
Percutaneous local ablation therapy: Ebara et al[23] reported that following percutaneous ethanol injection (PEI) therapy, the 1-, 2-, 3-, 4- and 5-year survival rates of 95 patients with an HCC smaller than 3 cm were 93%, 81%, 65%, 52% and 28%, respectively. This treatment could be performed for patients with Child’s A as well as Child’s B or C disease, although the survival rates of patients with Child’s A or B status was higher than those in Child’s C patients[23]. In cases of HCC recurrence, PEI was easily repeated[23], although a repeated hepatic resection was reported in selected patients[9]. Additionally, Shiina et al[10] reported that with a median follow-up of 51.6 mo, the 5-, 10- and 20-year survival rates of 2147 HCC-patients, were 49%, 18% and 7.2%, respectively. There were 45 complications (2.1%) and two deaths (0.1%)[10].
Radiofrequency ablation (RFA), instead of PEI (Figure 1A), is widely performed for HCC. Shiina et al[11] reported that the 5-, and 10-year survival rates of 1170 HCC-patients with a median follow-up of 38.2 mo were 60% and 27%, respectively. In that study, the survival rates of RFA were found to be superior to those of PEI[10,11], although it was not a head-to-head comparison. One death (0.03%) and 67 complications (2.2%) occurred[11], and the HCC was controlled by RFA. A randomized controlled trial of surgery vs RFA for small HCC has begun in Japan[24]. Additionally, it was reported that adjuvant RFA might provide palliative care for patients with metastatic cancer[25]. Further studies are required. The meta-analysis of the four randomized controlled trials demonstrated a significant improvement in the 3-year survival rate and that RFA was more effective than PEI[26].
Liver transplantation offers additional benefits for HCC patients because additional cancers might be incidentally found during the examination of the explanted liver; additional cancers attribute to high HCC recurrence rates after primary surgical resection[27]. The criteria for liver transplantation have improved over many years[28-32]. According to the Milan criteria, patients are eligible for liver transplantation if they have a single HCC less than 5 cm in diameter or no more than three tumors less than 3 cm in diameter[30]. Liver transplantation is the first-line treatment option for these patients[16]. Mazzaferro et al[30] studied 48 patients within the Milan criteria; they reported an overall mortality rate of 17% after 4 years and that the actual survival rate and recurrence-free survival rate were 75% and 83%, respectively. Additionally, they reported that in 35 patients meeting the predetermined criteria for small HCCs in the pathology examination of the explanted liver, the overall and recurrence-free survival rates at four years were 85% and 92%, respectively[30]. These results suggest that liver transplantation is an effective treatment for small, unresectable HCCs in patients with cirrhosis. An excellent 5-year survival rate has been reported in cases in which the restrictive Milan criteria are used to select transplant candidates. HCC is a good indication for orthotopic liver transplantation, and cadaveric liver transplantation/deceased-donor liver transplantation is an excellent treatment for early HCC (Figure 1B). Additionally, living-donor liver transplantation is an excellent treatment for early HCC because deceased-donor liver transplantation is limited by the shortage of grafts[33,34]. In Japan and other Asian countries, living-donor liver transplantation will continue to be a mainstay treatment of HCC in cirrhotic patients[35,36].
HCC frequently occurs in cirrhotic liver patients infected with HBV or HCV. Although the viral infections are eradicated or controlled[37-45], the risk of developing HCC persists in patients with advanced liver disease. Elder patients tend to have more advanced fibrosis than younger patients[46-52]. Regardless of the liver function, in cases in which the restrictive Milan criteria are used to select transplant candidates, liver transplantation in patients within the criteria has a better prognosis. However, many difficulties exist, including a shortage of donors and whether a patient is eligible for transplantation because of age. Elderly patients with an increased risk for postoperative complications should be excluded from living donor liver transplantation, at least; previous published studies have shown that age is not a contraindication for deceased donor liver transplantation[53,54].
Down-staging the policies for HCCs exceeding the conventional criteria could not be recommended[16], and prospective studies should be conducted to explore the issue of expanded criteria for orthotopic liver transplantation, down staging and bridge therapies.
Treatment with sorafenib prolongs progression-free survival in patients with advanced clear-cell renal-cell carcinoma in whom previous therapy has failed; the treatment is associated with increased toxic effects[55]. Similarly, in 602 patients with advanced HCC (299 in the sorafenib group; 303 in the placebo group), overall survival (OS) was significant longer in the sorafenib group compared with the placebo group (OS of 10.7 mo vs 7.9 mo, respectively; hazard ratio in the sorafenib group, 0.69; 95%CI: 0.55-0.87; P < 0.001)[56]. Another study from the Asia-Pacific region[57] showed that sorafenib is effective for advanced HCC treatment in Child’s A patients. Common adverse events such as hand-foot skin reactions, diarrhea and fatigue were observed in the study[57]. Molecular targeted therapy against HCCs is being developed and will augment the treatment of advanced HCC[58,59].
TACE: A Japanese prospective cohort study in 8510 patients with unresectable HCC showed a 5-year survival rate of 26%[60]. Superselective TACE for HCC showed overall median and 5-year survival rates of 3.3 years and 34%, respectively[61]. TACE showed higher survival rates in patients with fewer tumor numbers, smaller tumor size, and better liver function (Child’s A or B). In Asian countries, TACE is the main therapeutic modality in advanced HCC-patients, and the overall therapeutic outcomes depend on the tumor size[62]. TACE has a long history in the treatment of unresectable HCC cases[63,64]. TACE, in combination with surgery or local ablation therapy, is frequently used in clinical practice. The timing and number of treatment sessions of TACE are not uniform for each patient, although new devices and treatments, including drug-eluting bead TACE and trans-arterial radio-embolization, have been developed and continue to develop[65,66].
Stereotactic body radiation therapy/stereotactic ablative radiotherapy: Stereotactic body radiation therapy (SBRT) for HCC has been documented in several recent studies[67-70]. Use of a cyberknife is an SBRT system that allows for real-time tracking of a tumor. The system affords good local tumor control and higher overall survival rates than other historical controls such as best supportive care or sorafenib therapy[70]. SBRT is a salvage treatment for unresectable HCC patients who failed or were unsuitable for TACE[71] or for patients with an unresectable massive HCC for whom standard treatment care is unsuitable[72]. Repeated stereotactic ablative radiotherapy in selected HCC patients might be feasible, if toxicity levels are acceptable[73].
Other therapies: Proton and carbon ion therapies for 343 HCC-patients showed that the 5-year local control and overall survival rates were 91% and 38%, respectively[74]. These therapies might be alternatives to conventional local therapies for HCC[74-77]. Additionally, laparoscopic liver resection appears to offer at least short-term benefits in selected HCC patients[78,79] whereas it is a widely employed alternative to open surgery in well-selected candidates. Standardization of surgical techniques might facilitate the performance of safe procedures[79].
After a curative treatment such as surgical resection or RFA, antiviral therapies should be considered in patients infected with chronic HBV and/or HCV[38,49,50,80,81]. In HCV-infected individuals, interferon-free regimens might be beneficial[82]. Hepatic resection was recommended in non-B and non-C patients[83] because unknown causes of HCC might be present in these patients, and particularly careful follow-up is needed.
Many reviews on this topic have been published in the last few years, and most prestigious scientific societies worldwide provide practical treatment guidelines that are regularly updated, including HCC treatment algorithms (Table 1)[16,84-87]. Liver transplantation and surgical resections are regarded as the only curative treatments; however, they have different indications. Although liver transplantation has not received priority over surgical resection, the most reliable therapy for HCC patients, presently, appears to be liver transplantation because its survival rate is superior to that of the other treatments. On this point, this review might differ from other practical guidelines or treatment algorithms. Deceased-donor liver-transplantation is limited by the shortage of grafts, and living-donor liver-transplantation should be discussed. If it is impossible for an HCC patient to undergo liver transplantation, then surgical resection or RFA, should be considered, in accordance with the liver function of the patient. We expect that stronger molecular targeted drugs will be used in the treatment of HCC patients and that these treatments will have more potency and fewer adverse events than are observed with sorafenib treatment. In the near future, methods of promoting hepatic regeneration might be improved. Further studies are ongoing.
| Modalities | Indication of the features of HCC |
| Surgical resection | Performance status 0, Child-Pugh A, single < 3 cm |
| Normal bilirubin/normal portal pressure | |
| Associated diseases, no | |
| RFA | Performance status 0, Child-Pugh A-B, single or 3 nodule ≤ 3 cm |
| Slightly increased bilirubin/increased portal pressure | |
| Associated diseases, yes or no | |
| Liver transplantation | Performance status 0, single or 3 nodule ≤ 3 cm |
| Increased bilirubin/increased portal pressure | |
| Associated diseases, no | |
| Sorafenib | Performance status 1-2, Child-Pugh A-B, Advanced stage (portal invasion), node classification 1, metastasis classification 1 |
| TACE | Performance status 0, Child-Pugh A-B, Intermediate stage (multi nodular) |
The authors thanks Dr. Ryosuke Tateishi, University of Tokyo for valuable discussions.
P- Reviewer: Chiang TA, Mihaila RG, Moralioglu S S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
| 1. | Fong ZV, Tanabe KK. The clinical management of hepatocellular carcinoma in the United States, Europe, and Asia: a comprehensive and evidence-based comparison and review. Cancer. 2014;120:2824-2838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 205] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 2. | El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264-1273.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2183] [Cited by in RCA: 2506] [Article Influence: 192.8] [Reference Citation Analysis (2)] |
| 3. | Liaw YF, Kao JH, Piratvisuth T, Chan HLY, Chien RN, Liu CJ, Gane E, Locarnini S, Lim SG, Han KH. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2012 update. Hepatol Int. 2012;6:531-561. [RCA] [DOI] [Full Text] [Cited by in Crossref: 742] [Cited by in RCA: 792] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 4. | Omata M, Kanda T, Yu ML, Yokosuka O, Lim SG, Jafri W, Tateishi R, S . Hamid S, Chuang WL, Chutaputti A, Wei L, Sollano J, Sarin SK, Kao JH, W. McCaughan G. APASL consensus statements and management algorithms for hepatitis C virus infection. Hepatol Int. 2012;6:409-435. [RCA] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 142] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 5. | Yoshizawa H, Tanaka J, Miyakawa Y. National prevention of hepatocellular carcinoma in Japan based on epidemiology of hepatitis C virus infection in the general population. Intervirology. 2006;49:7-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Kanda T, Imazeki F, Yokosuka O. New antiviral therapies for chronic hepatitis C. Hepatol Int. 2010;4:548-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Kanda T, Jiang X, Yokosuka O. Androgen receptor signaling in hepatocellular carcinoma and pancreatic cancers. World J Gastroenterol. 2014;20:9229-9236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 46] [Reference Citation Analysis (0)] |
| 8. | Makuuchi M, Kosuge T, Takayama T, Yamazaki S, Kakazu T, Miyagawa S, Kawasaki S. Surgery for small liver cancers. Semin Surg Oncol. 1993;9:298-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 538] [Cited by in RCA: 596] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 9. | Yamazaki S, Takayama T. Surgical treatment of hepatocellular carcinoma: evidence-based outcomes. World J Gastroenterol. 2008;14:685-692. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 10. | Shiina S, Tateishi R, Imamura M, Teratani T, Koike Y, Sato S, Obi S, Kanai F, Kato N, Yoshida H. Percutaneous ethanol injection for hepatocellular carcinoma: 20-year outcome and prognostic factors. Liver Int. 2012;32:1434-1442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Shiina S, Tateishi R, Arano T, Uchino K, Enooku K, Nakagawa H, Asaoka Y, Sato T, Masuzaki R, Kondo Y. Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol. 2012;107:569-577; quiz 578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 484] [Cited by in RCA: 577] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 12. | Tanaka K, Shimada M, Kudo M. Characteristics of long-term survivors following sorafenib treatment for advanced hepatocellular carcinoma: report of a workshop at the 50th Annual Meeting of the Liver Cancer Study Group of Japan. Oncology. 2014;87 Suppl 1:104-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Sakamoto M, Hirohashi S, Tsuda H, Shimosato Y, Makuuchi M, Hosoda Y. Multicentric independent development of hepatocellular carcinoma revealed by analysis of hepatitis B virus integration pattern. Am J Surg Pathol. 1989;13:1064-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 66] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Oikawa T, Ojima H, Yamasaki S, Takayama T, Hirohashi S, Sakamoto M. Multistep and multicentric development of hepatocellular carcinoma: histological analysis of 980 resected nodules. J Hepatol. 2005;42:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Makuuchi M, Sano K. The surgical approach to HCC: our progress and results in Japan. Liver Transpl. 2004;10:S46-S52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 121] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | European Association For The Study Of The Liver; European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4059] [Cited by in RCA: 4517] [Article Influence: 347.5] [Reference Citation Analysis (2)] |
| 17. | Bruix J, Castells A, Bosch J, Feu F, Fuster J, Garcia-Pagan JC, Visa J, Bru C, Rodés J. Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology. 1996;111:1018-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 656] [Cited by in RCA: 621] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 18. | Ishizawa T, Hasegawa K, Aoki T, Takahashi M, Inoue Y, Sano K, Imamura H, Sugawara Y, Kokudo N, Makuuchi M. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology. 2008;134:1908-1916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 582] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 19. | Kashima Y, Miyazaki M, Ito H, Kaiho T, Nakagawa K, Ambiru S, Shimizu H, Furuya S, Nakajima N. Effective hepatic artery chemoembolization for advanced hepatocellular carcinoma with extensive tumour thrombus through the hepatic vein. J Gastroenterol Hepatol. 1999;14:922-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Minagawa M, Makuuchi M, Takayama T, Ohtomo K. Selection criteria for hepatectomy in patients with hepatocellular carcinoma and portal vein tumor thrombus. Ann Surg. 2001;233:379-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 144] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 21. | Yoshidome H, Takeuchi D, Kimura F, Shimizu H, Ohtsuka M, Kato A, Furukawa K, Yoshitomi H, Miyazaki M. Treatment strategy for hepatocellular carcinoma with major portal vein or inferior vena cava invasion: a single institution experience. J Am Coll Surg. 2011;212:796-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Miyazaki M, Kimura F, Shimizu H, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, Nozawa S, Furukawa K, Takeuchi D. Surgical treatment for liver cancer. Current issues. Dig Surg. 2007;24:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Ebara M, Ohto M, Sugiura N, Kita K, Yoshikawa M, Okuda K, Kondo F, Kondo Y. Percutaneous ethanol injection for the treatment of small hepatocellular carcinoma. Study of 95 patients. J Gastroenterol Hepatol. 1990;5:616-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 172] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 24. | Hasegawa K, Kokudo N, Shiina S, Tateishi R, Makuuchi M. Surgery versus radiofrequency ablation for small hepatocellular carcinoma: Start of a randomized controlled trial (SURF trial). Hepatol Res. 2010;40:851-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Ogura K, Miyake R, Shiina S, Shinoda Y, Okuma T, Kobayashi H, Goto T, Nakamura K, Kawano H. Bone radiofrequency ablation combined with prophylactic internal fixation for metastatic bone tumor of the femur from hepatocellular carcinoma. Int J Clin Oncol. 2012;17:417-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Cho YK, Kim JK, Kim MY, Rhim H, Han JK. Systematic review of randomized trials for hepatocellular carcinoma treated with percutaneous ablation therapies. Hepatology. 2009;49:453-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 336] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 27. | Guest J, Blumgart LH. Surgery of liver tumours. Baillieres Clin Gastroenterol. 1987;1:131-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 28. | O’Grady JG, Polson RJ, Rolles K, Calne RY, Williams R. Liver transplantation for malignant disease. Results in 93 consecutive patients. Ann Surg. 1988;207:373-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 329] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 29. | Jaurrieta E, Fabregat J, Figueras J, Bella R, Moreno-Llorente P, Rafecas A, Torras J, Casanovas T, Casais L. Liver transplantation in hepatocellular carcinoma. Transpl Int. 1992;5 Suppl 1:S196-S197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5110] [Cited by in RCA: 5306] [Article Influence: 183.0] [Reference Citation Analysis (0)] |
| 31. | Figueras J, Ibañez L, Ramos E, Jaurrieta E, Ortiz-de-Urbina J, Pardo F, Mir J, Loinaz C, Herrera L, López-Cillero P. Selection criteria for liver transplantation in early-stage hepatocellular carcinoma with cirrhosis: results of a multicenter study. Liver Transpl. 2001;7:877-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 120] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 32. | Llovet JM, Fuster J, Bruix J. The Barcelona approach: diagnosis, staging, and treatment of hepatocellular carcinoma. Liver Transpl. 2004;10:S115-S120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 500] [Cited by in RCA: 514] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 33. | Sarasin FP, Majno PE, Llovet JM, Bruix J, Mentha G, Hadengue A. Living donor liver transplantation for early hepatocellular carcinoma: A life-expectancy and cost-effectiveness perspective. Hepatology. 2001;33:1073-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 195] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 34. | Kurtovic J, Riordan SM, Williams R. Liver transplantation for hepatocellular carcinoma. Best Pract Res Clin Gastroenterol. 2005;19:147-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 35. | Akamatsu N, Sugawara Y, Kokudo N. Living donor liver transplantation for patients with hepatocellular carcinoma. Liver Cancer. 2014;3:108-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 36. | Akamatsu N, Sugawara Y, Kokudo N. Living-donor vs deceased-donor liver transplantation for patients with hepatocellular carcinoma. World J Hepatol. 2014;6:626-631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 37. | Yoshida H, Shiratori Y, Moriyama M, Arakawa Y, Ide T, Sata M, Inoue O, Yano M, Tanaka M, Fujiyama S. Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of Hepatocarcinogenesis by Interferon Therapy. Ann Intern Med. 1999;131:174-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 833] [Cited by in RCA: 780] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 38. | Shiratori Y, Shiina S, Teratani T, Imamura M, Obi S, Sato S, Koike Y, Yoshida H, Omata M. Interferon therapy after tumor ablation improves prognosis in patients with hepatocellular carcinoma associated with hepatitis C virus. Ann Intern Med. 2003;138:299-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 218] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 39. | Shiratori Y, Ito Y, Yokosuka O, Imazeki F, Nakata R, Tanaka N, Arakawa Y, Hashimoto E, Hirota K, Yoshida H. Antiviral therapy for cirrhotic hepatitis C: association with reduced hepatocellular carcinoma development and improved survival. Ann Intern Med. 2005;142:105-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 207] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 40. | Morgan RL, Baack B, Smith BD, Yartel A, Pitasi M, Falck-Ytter Y. Eradication of hepatitis C virus infection and the development of hepatocellular carcinoma: a meta-analysis of observational studies. Ann Intern Med. 2013;158:329-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 631] [Cited by in RCA: 652] [Article Influence: 54.3] [Reference Citation Analysis (0)] |
| 41. | Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, Yuen H, Tanwandee T, Tao QM, Shue K, Keene ON, Dixon JS, Gray DF, Sabbat J. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med. 2004;351:1521-1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1739] [Cited by in RCA: 1740] [Article Influence: 82.9] [Reference Citation Analysis (0)] |
| 42. | Hosaka T, Suzuki F, Kobayashi M, Seko Y, Kawamura Y, Sezaki H, Akuta N, Suzuki Y, Saitoh S, Arase Y. Long-term entecavir treatment reduces hepatocellular carcinoma incidence in patients with hepatitis B virus infection. Hepatology. 2013;58:98-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 519] [Cited by in RCA: 540] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
| 43. | Gordon SC, Lamerato LE, Rupp LB, Li J, Holmberg SD, Moorman AC, Spradling PR, Teshale EH, Vijayadeva V, Boscarino JA. Antiviral therapy for chronic hepatitis B virus infection and development of hepatocellular carcinoma in a US population. Clin Gastroenterol Hepatol. 2014;12:885-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 117] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 44. | Huang G, Lau WY, Wang ZG, Pan ZY, Yuan SX, Shen F, Zhou WP, Wu MC. Antiviral therapy improves postoperative survival in patients with hepatocellular carcinoma: a randomized controlled trial. Ann Surg. 2015;261:56-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 191] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 45. | Chong CC, Wong GL, Wong VW, Ip PC, Cheung YS, Wong J, Lee KF, Lai PB, Chan HL. Antiviral therapy improves post-hepatectomy survival in patients with hepatitis B virus-related hepatocellular carcinoma: a prospective-retrospective study. Aliment Pharmacol Ther. 2015;41:199-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 46. | Di Bisceglie AM, Shiffman ML, Everson GT, Lindsay KL, Everhart JE, Wright EC, Lee WM, Lok AS, Bonkovsky HL, Morgan TR. Prolonged therapy of advanced chronic hepatitis C with low-dose peginterferon. N Engl J Med. 2008;359:2429-2441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 377] [Cited by in RCA: 339] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 47. | Morgan TR, Ghany MG, Kim HY, Snow KK, Shiffman ML, De Santo JL, Lee WM, Di Bisceglie AM, Bonkovsky HL, Dienstag JL. Outcome of sustained virological responders with histologically advanced chronic hepatitis C. Hepatology. 2010;52:833-844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 392] [Cited by in RCA: 376] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 48. | Lok AS, Everhart JE, Wright EC, Di Bisceglie AM, Kim HY, Sterling RK, Everson GT, Lindsay KL, Lee WM, Bonkovsky HL. Maintenance peginterferon therapy and other factors associated with hepatocellular carcinoma in patients with advanced hepatitis C. Gastroenterology. 2011;140:840-849; quiz e12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 146] [Cited by in RCA: 158] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 49. | Kanda T, Imazeki F, Mikami S, Kato K, Shimada N, Yonemitsu Y, Miyauchi T, Arai M, Fujiwara K, Tsubota A. Occurrence of hepatocellular carcinoma was not a rare event during and immediately after antiviral treatment in Japanese HCV-positive patients. Oncology. 2011;80:366-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 50. | Kanda T, Nakamoto S, Yasui S, Nakamura M, Miyamura T, Wu S, Jiang X, Arai M, Imazeki F, Yokosuka O. Occurrence and Recurrence of Hepatocellular Carcinoma Were Not Rare Events during Phlebotomy in Older Hepatitis C Virus-Infected Patients. Case Rep Oncol. 2014;7:288-296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 51. | Singal AK, Salameh H, Kuo YF, Fontana RJ. Meta-analysis: the impact of oral anti-viral agents on the incidence of hepatocellular carcinoma in chronic hepatitis B. Aliment Pharmacol Ther. 2013;38:98-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 127] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 52. | Arends P, Sonneveld MJ, Zoutendijk R, Carey I, Brown A, Fasano M, Mutimer D, Deterding K, Reijnders JG, Oo Y, Petersen J, van Bömmel F, de Knegt RJ, Santantonio T, Berg T, Welzel TM, Wedemeyer H, Buti M, Pradat P, Zoulim F, Hansen B, Janssen HL; VIRGIL Surveillance Study Group. Entecavir treatment does not eliminate the risk of hepatocellular carcinoma in chronic hepatitis B: limited role for risk scores in Caucasians. Gut. 2015;64:1289-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 167] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 53. | Alamo JM, Olivares C, Jiménez G, Bernal C, Marín LM, Tinoco J, Suárez G, Serrano J, Padillo J, Gómez MÁ. Donor characteristics that are associated with survival in liver transplant recipients older than 70 years with grafts. Transplant Proc. 2013;45:3633-3636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 54. | Oezcelik A, Dayangac M, Guler N, Yaprak O, Erdogan Y, Akyildiz M, Sevdik Z, Yuzer Y, Tokat Y. Living Donor Liver Transplantation in Patients 70 Years or Older. Transplantation. 2015;99:1436-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 55. | Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, Negrier S, Chevreau C, Solska E, Desai AA. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;356:125-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3788] [Cited by in RCA: 3764] [Article Influence: 209.1] [Reference Citation Analysis (0)] |
| 56. | Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9016] [Cited by in RCA: 10258] [Article Influence: 603.4] [Reference Citation Analysis (2)] |
| 57. | Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3854] [Cited by in RCA: 4648] [Article Influence: 273.4] [Reference Citation Analysis (0)] |
| 58. | Kanda T, Imazeki F, Kanai F, Tada M, Yokosuka O, Omata M. Signaling pathways involved in molecular carcinogenesis of hepatocellular carcinoma. Molecular Aspects of Hepatocellular Carcinoma. 1st ed. Qiao L, Li Y, Yan X, George J, editors. Saif Zone, UAE: Bentham Science Publishers 2012; 39-55. |
| 59. | Jiang X, Kanda T, Nakamoto S, Miyamura T, Wu S, Yokosuka O. Involvement of androgen receptor and glucose-regulated protein 78 kDa in human hepatocarcinogenesis. Exp Cell Res. 2014;323:326-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 60. | Takayasu K, Arii S, Ikai I, Omata M, Okita K, Ichida T, Matsuyama Y, Nakanuma Y, Kojiro M, Makuuchi M. Prospective cohort study of transarterial chemoembolization for unresectable hepatocellular carcinoma in 8510 patients. Gastroenterology. 2006;131:461-469. [PubMed] |
| 61. | Takayasu K, Arii S, Kudo M, Ichida T, Matsui O, Izumi N, Matsuyama Y, Sakamoto M, Nakashima O, Ku Y. Superselective transarterial chemoembolization for hepatocellular carcinoma. Validation of treatment algorithm proposed by Japanese guidelines. J Hepatol. 2012;56:886-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 167] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 62. | Han KH, Kudo M, Ye SL, Choi JY, Poon RT, Seong J, Park JW, Ichida T, Chung JW, Chow P. Asian consensus workshop report: expert consensus guideline for the management of intermediate and advanced hepatocellular carcinoma in Asia. Oncology. 2011;81 Suppl 1:158-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 98] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 63. | Ohnishi K, Tsuchiya S, Nakayama T, Hiyama Y, Iwama S, Goto N, Takashi M, Ohtsuki T, Kono K, Nakajima Y. Arterial chemoembolization of hepatocellular carcinoma with mitomycin C microcapsules. Radiology. 1984;152:51-55. [PubMed] |
| 64. | Soga K, Nomoto M, Ichida T, Aoyagi Y, Ozaki T, Ichida F. Clinical evaluation of transcatheter arterial embolization and one-shot chemotherapy in hepatocellular carcinoma. Hepatogastroenterology. 1988;35:116-120. [PubMed] |
| 65. | Golfieri R, Giampalma E, Renzulli M, Cioni R, Bargellini I, Bartolozzi C, Breatta AD, Gandini G, Nani R, Gasparini D. Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolisation for hepatocellular carcinoma. Br J Cancer. 2014;111:255-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 410] [Cited by in RCA: 483] [Article Influence: 43.9] [Reference Citation Analysis (1)] |
| 66. | Andreana L, Isgrò G, Marelli L, Davies N, Yu D, Navalkissoor S, Burroughs AK. Treatment of hepatocellular carcinoma (HCC) by intra-arterial infusion of radio-emitter compounds: trans-arterial radio-embolisation of HCC. Cancer Treat Rev. 2012;38:641-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 67. | Goyal K, Einstein D, Yao M, Kunos C, Barton F, Singh D, Siegel C, Stulberg J, Sanabria J. Cyberknife stereotactic body radiation therapy for nonresectable tumors of the liver: preliminary results. HPB Surg. 2010;2010:pii: 309780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 68. | Huang WY, Jen YM, Lee MS, Chang LP, Chen CM, Ko KH, Lin KT, Lin JC, Chao HL, Lin CS. Stereotactic body radiation therapy in recurrent hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2012;84:355-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 146] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 69. | O’Connor JK, Trotter J, Davis GL, Dempster J, Klintmalm GB, Goldstein RM. Long-term outcomes of stereotactic body radiation therapy in the treatment of hepatocellular cancer as a bridge to transplantation. Liver Transpl. 2012;18:949-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 128] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 70. | Bibault JE, Dewas S, Vautravers-Dewas C, Hollebecque A, Jarraya H, Lacornerie T, Lartigau E, Mirabel X. Stereotactic body radiation therapy for hepatocellular carcinoma: prognostic factors of local control, overall survival, and toxicity. PLoS One. 2013;8:e77472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 90] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 71. | Lo CH, Huang WY, Lee MS, Lin KT, Lin TP, Chang PY, Fan CY, Jen YM. Stereotactic ablative radiotherapy for unresectable hepatocellular carcinoma patients who failed or were unsuitable for transarterial chemoembolization. Eur J Gastroenterol Hepatol. 2014;26:345-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 72. | Que JY, Lin LC, Lin KL, Lin CH, Lin YW, Yang CC. The efficacy of stereotactic body radiation therapy on huge hepatocellular carcinoma unsuitable for other local modalities. Radiat Oncol. 2014;9:120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 73. | Lo CH, Huang WY, Lin KT, Lin MJ, Lin TP, Jen YM. Repeated stereotactic ablative radiotherapy using CyberKnife for patients with hepatocellular carcinoma. J Gastroenterol Hepatol. 2014;29:1919-1925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 74. | Komatsu S, Fukumoto T, Demizu Y, Miyawaki D, Terashima K, Sasaki R, Hori Y, Hishikawa Y, Ku Y, Murakami M. Clinical results and risk factors of proton and carbon ion therapy for hepatocellular carcinoma. Cancer. 2011;117:4890-4904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 120] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 75. | Kato H, Tsujii H, Miyamoto T, Mizoe JE, Kamada T, Tsuji H, Yamada S, Kandatsu S, Yoshikawa K, Obata T. Results of the first prospective study of carbon ion radiotherapy for hepatocellular carcinoma with liver cirrhosis. Int J Radiat Oncol Biol Phys. 2004;59:1468-1476. [PubMed] |
| 76. | Imada H, Kato H, Yasuda S, Yamada S, Yanagi T, Hara R, Kishimoto R, Kandatsu S, Minohara S, Mizoe JE. Compensatory enlargement of the liver after treatment of hepatocellular carcinoma with carbon ion radiotherapy - relation to prognosis and liver function. Radiother Oncol. 2010;96:236-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 77. | Imada H, Kato H, Yasuda S, Yamada S, Yanagi T, Kishimoto R, Kandatsu S, Mizoe JE, Kamada T, Yokosuka O. Comparison of efficacy and toxicity of short-course carbon ion radiotherapy for hepatocellular carcinoma depending on their proximity to the porta hepatis. Radiother Oncol. 2010;96:231-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 78. | Sasaki A, Nitta H, Otsuka K, Takahara T, Nishizuka S, Wakabayashi G. Ten-year experience of totally laparoscopic liver resection in a single institution. Br J Surg. 2009;96:274-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 132] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 79. | Ho CM, Wakabayashi G, Nitta H, Takahashi M, Takahara T, Ito N, Hasegawa Y. Total laparoscopic limited anatomical resection for centrally located hepatocellular carcinoma in cirrhotic liver. Surg Endosc. 2013;27:1820-1825. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 80. | Miyauchi T, Kanda T, Shinozaki M, Kamezaki H, Wu S, Nakamoto S, Kato K, Arai M, Mikami S, Sugiura N. Efficacy of lamivudine or entecavir against virological rebound after achieving HBV DNA negativity in chronic hepatitis B patients. Int J Med Sci. 2013;10:647-652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 81. | Saito T, Chiba T, Suzuki E, Shinozaki M, Goto N, Kanogawa N, Motoyama T, Ogasawara S, Ooka Y, Tawada A. Effect of previous interferon-based therapy on recurrence after curative treatment of hepatitis C virus-related hepatocellular carcinoma. Int J Med Sci. 2014;11:707-712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 82. | Kanda T, Yokosuka O, Omata M. Treatment of hepatitis C virus infection in the future. Clin Transl Med. 2013;2:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 83. | Utsunomiya T, Shimada M, Kudo M, Ichida T, Matsui O, Izumi N, Matsuyama Y, Sakamoto M, Nakashima O, Ku Y. Nationwide study of 4741 patients with non-B non-C hepatocellular carcinoma with special reference to the therapeutic impact. Ann Surg. 2014;259:336-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 84. | Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020-1022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5972] [Cited by in RCA: 6569] [Article Influence: 469.2] [Reference Citation Analysis (1)] |
| 85. | Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H, Kudo M, Lee JM, Choi BI, Poon RT. Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int. 2010;4:439-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 797] [Cited by in RCA: 841] [Article Influence: 56.1] [Reference Citation Analysis (0)] |
| 86. | Kudo M, Matsui O, Izumi N, Kadoya M, Okusaka T, Miyayama S, Yamakado K, Tsuchiya K, Ueshima K, Hiraoka A. Transarterial chemoembolization failure/refractoriness: JSH-LCSGJ criteria 2014 update. Oncology. 2014;87 Suppl 1:22-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 218] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 87. | Roayaie S, Jibara G, Tabrizian P, Park JW, Yang J, Yan L, Schwartz M, Han G, Izzo F, Chen M. The role of hepatic resection in the treatment of hepatocellular cancer. Hepatology. 2015;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 321] [Article Influence: 32.1] [Reference Citation Analysis (0)] |