Published online Jul 8, 2015. doi: 10.4254/wjh.v7.i13.1782
Peer-review started: March 21, 2015
First decision: April 27, 2015
Revised: May 9, 2015
Accepted: June 15, 2015
Article in press: June 16, 2015
Published online: July 8, 2015
Processing time: 113 Days and 6.3 Hours
AIM: To illustrate the application and utility of Geographic Information System (GIS) in exploring patterns of liver transplantation. Specifically, we aim to describe the geographic distribution of transplant registrations and identify disparities in access to liver transplantation across United Network of Organ Sharing (UNOS) region 1.
METHODS: Based on UNOS data, the number of listed transplant candidates by ZIP code from 2003 to 2012 for Region 1 was obtained. Choropleth (color-coded) maps were used to visualize the geographic distribution of transplant registrations across the region. Spatial interaction analysis was used to analyze the geographic pattern of total transplant registrations by ZIP code. Factors tested included ZIP code log population and log distance from each ZIP code to the nearest transplant center; ZIP code population density; distance from the nearest city over 50000; and dummy variables for state residence and location in the southern portion of the region.
RESULTS: Visualization of transplant registrations revealed geographic disparities in organ allocation across Region 1. The total number of registrations was highest in the southern portion of the region. Spatial interaction analysis, after adjusting for the size of the underlying population, revealed statistically significant clustering of high and low rates in several geographic areas could not be predicted based solely on distance to the transplant center or density of population.
CONCLUSION: GIS represents a new method to evaluate the access to liver transplantation within one region and can be used to identify the presence of disparities and reasons for their existence in order to alleviate them.
Core tip: Geographic Information System (GIS) studies the impact of geography on many problems through statistical modeling and analysis. It has been used to guide decisions in business, government, environment, but has yet to be adopted in healthcare. Based on the United Network of Organ Sharing database from 2003 to 2012 in one region, GIS revealed clustering of high and low rates of listing for liver transplantation in several geographic areas that could not have otherwise been predicted. This method can be adopted in different parts of the world and contribute to better allocation of resources to decrease the disparities in access to liver transplantation.
- Citation: Ghaoui R, Garb J, Gordon F, Pomfret E. Impact of geography on organ allocation: Beyond the distance to the transplantation center. World J Hepatol 2015; 7(13): 1782-1787
- URL: https://www.wjgnet.com/1948-5182/full/v7/i13/1782.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i13.1782
Liver transplantation remains the only truly therapeutic intervention for patients with end stage liver disease and decompensated cirrhosis. Unfortunately, the access to organ transplantation from a cadaveric or living donor is limited by a shortage of donors. This has become especially problematic given the expected surge of patients in need of a transplant due to the combination of three epidemics: (1) Hepatitis C that may lead to a quadrupling of the number of patients with decompensated cirrhosis in 10 years[1]; (2) the obesity epidemic leading to cirrhosis through non-alcoholic fatty liver disease[2]; and (3) hepatocellular carcinoma[3].
This alarming shortage of organs is likely going to exacerbate the established healthcare disparities including the ones stemming from Geography. With regard to access to liver transplantation, 7 of 11 United States regions differed significantly from the national average[4]. This has clear implications on the management of patients with hepatocellular carcinoma; a United Network for Organ Sharing (UNOS) database has showed that regions with longer waiting times used more loco-regional palliative therapy[5]. This occurs despite tumor allocation points that aim at giving an advantage to liver cancer candidates, especially with long waiting time on the transplant lists[6]. In the United States and based on a study from Region 4, it was suggested that the distance from the transplant center should be included to improve the estimate of the mortality risk for patients on the waiting list[7].
A Geographic Information System (GIS) represents a systematic way to study the impact of geography on this problem. GIS can synthesize data from several different sources, visualize trends in maps that would not otherwise be apparent, and reveal significant spatial associations through statistical modeling and analysis. GIS has long been used to guide decision-making process in disparate fields such as business, government, environment and conservation, the military and epidemiology. The impact of GIS in strategic decisions in healthcare has not been widely adopted.
Accordingly, the aim of our study was to demonstrate the utility of GIS with organ transplantation data to assess geographic disparities in burden of care and access to liver transplantation across UNOS region 1 and to examine the stability of these disparities over time. We also wanted to determine if geography should be considered as a factor in building satellite clinics to evaluate patients for liver transplantation.
The total number of transplant registrations (listed candidates) for UNOS Region 1 by ZIP code from 2003 to 2012, was obtained from UNOS. This represents the total transplant burden of care on local transplant facilities or need. ZIP code geographic data was originally obtained as geographic coordinates and was projected to Lambert Conformal for visualization and analysis. The number of transplant registrations by ZIP code were mapped with ArcGIS software[8] using a choropleth (color-coded) map, where number of registrations is represented by the intensity of color. Spatial interaction analysis based on the gravity model was used to analyze the geographic pattern of total transplant registrations by ZIP code. Transplant registrations were analyzed for all years combined to stabilize numbers. The gravity model is used to model flow (in this case, number of transplant registrations) from one or more origins (in this case, ZIP code) to one or more destinations (in this case, transplant centers). The model assumes that flow is determined by the population of the origin and distance from the origin to the destination[9]. Poisson regression was used to derive the gravity model using STATA software[10]. Factors tested included ZIP code log population and log distance from each ZIP code to the nearest transplant center (both specified by the gravity model); ZIP code population density; distance from the nearest city over 50000; and dummy variables for state residence and location in the southern portion of the region (consisting of Massachusetts, Connecticut or Rhode Island) which houses all the region’s transplant centers.
To adjust for the size of the underlying population, ZIP code registration rates were calculated as the number of candidates registered in a ZIP code divided by the total ZIP code population for each time period. Census 2000 population counts were used to calculated 2003-2005 rates, and Census 2010 counts were used for 2006-2012 rates.
If services were equally accessible throughout the region, registration rates should not vary geographically. To identify regional disparities in accessibility, we looked for clusters of excessively high or low rates relative to the rest of the region by year using the Spatial Scan Statistic[11]. The geographic locations of high and low clusters identified in this manner were then displayed using choropleth mapping. The statistical review of the study was performed by a biomedical statistician.
Table 1 gives the total number of registrations (burden of care) and registration rates (accessibility) by state for the total 10-year period. States are arranged in ascending order according to registration rate. There is great disparity in rates according to state. Massachusetts had the highest rate, almost three times that of Connecticut, which had the lowest rate. In Region 1, liver transplant programs include 5 in Massachusetts and 2 in Connecticut.
| State | Total registrations | Rate per 100000 population |
| CT | 1024 | 29.0 |
| VT1 | 104 | 41.6 |
| ME | 637 | 48.4 |
| NH | 652 | 50.0 |
| RI | 655 | 62.8 |
| MA | 5241 | 80.4 |
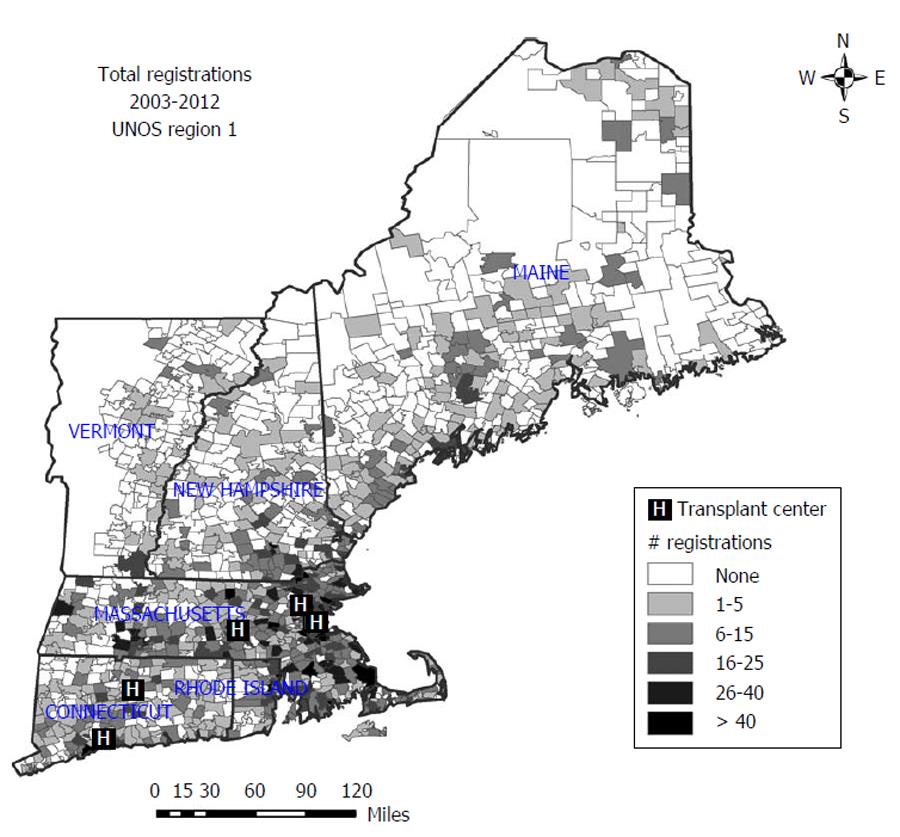
To visualize geographic variability in burden of care, Figure 1 shows the total number of transplant registrations by ZIP code for 2003-2012. ZIP codes with higher numbers of registrations are represented in darker shades of gray or black. Those with no registrations in the 10-year period are represented in white. As can be seen, there is wide variability in total registration numbers across the region, generated in part by variability of population size. A large number of ZIP codes had no transplant registrations. Visually, it is apparent that the number of registrations was highest in the southern portion of the region, in Massachusetts, Connecticut and Rhode Island.
Factors in burden of care were examined with Poisson regression on registration totals. As predicated by the gravity model, registrations showed a strong, significant association with between population size and total number of registrations indicated by the Z-value (25.03) and P-value (< 0.001). Distance from a transplant center was not significant (P = 0.1), implying that the gravity model does not completely specify registration patterns. The model did, however, account for 31% of the variability in registration numbers (R2 = 0.31). Other factors examined that were not significant were population density, location in the south of the region and distance to the nearest city > 50000 population.
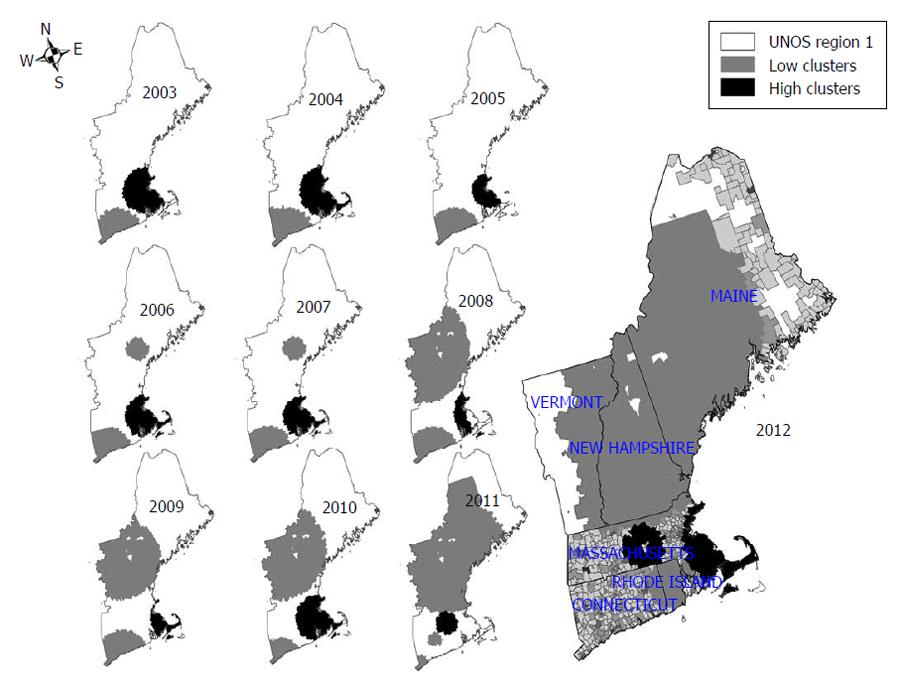
To visualize disparities in accessibility of transplant services, Figure 2 shows the location of high and low clusters of registration rates per 100000 population in the region each year from 2003-2012. The 2012 map is shown at a smaller scale for more detail. A cluster is defined as a group of ZIP codes with significantly higher or lower registration rates than the rest of the region. Low clusters are represented as gray areas, and high clusters as black areas. It is clear from the map that there was very little variation over time in the location of high clusters, which centered on the Southeast corner of the region in Rhode Island, Eastern Massachusetts and Southeast New Hampshire. There has been somewhat more variation in the location of low clusters over time. However, these clusters were generally confined to Connecticut and to the central sections of the region, in New Hampshire, Vermont and Maine. Table 2 shows the details of significant clusters in 2012. As can be seen, the most significant cluster, which included 63 ZIP codes and a relatively small population, had a registration rate 3 times the prevailing rate in the region. The other clusters covered a larger area and represented a larger population.
| Cluster | Cluster type | Listed | Expected | Relative risk | Significance | ZIP codes | Population |
| 1 | High | 114 | 39 | 3.3 | << 0.0001 | 63 | 683114 |
| 2 | High | 198 | 144 | 1.5 | 0.039 | 165 | 2554406 |
| 3 | Low | 107 | 171 | 0.57 | 0.00025 | 710 | 3027545 |
| 4 | Low | 34 | 67 | 0.48 | 0.055 | 89 | 1191886 |
With its relatively small geographical extent and the availability of numerous health systems of global reputation, one would expect that the impact of geography on organ allocation in Region 1 would be limited. The analysis of the UNOS data with a GIS brings a new perspective. The maps generated revealed clusters of excessively high listing rates for ZIP codes in the Boston area that remained stable over a decade with an increasing disparity and worsening access in the northern part of the region. More intriguing is the revelation of a new cluster of excessively low registration rates covering a good portion of Rhode Island despite its close driving distance to several transplant centers in 2012. This relates to the finding in multivariate analysis that distance to a transplant center as a predictor of listing rates implies that adding transplant centers in areas with low listing rates would not solve the problem. It seems more likely that local characteristics explain this phenomenon including, but not limited to, variable access to healthcare and subspecialists, educational and cultural beliefs related to transplantation. However this is difficult to prove in the absence of reliable databases.
Another geographical area worth investigating further is Connecticut with a progressive transition to a homogenous registration pattern over the past decade which correlates with the reopening of a transplant center. A practical conclusion from our study might be to consider establishing satellite clinics in the low-cluster areas with a connection to a main transplant centers following a model like the ECHO project. This initiative in New Mexico demonstrated that primary care providers anywhere can be trained via videoconferencing technology to manage complex chronic conditions formerly outside their expertise, thus expanding their ability to treat very sick patients and showing equal outcomes to academic settings[12]. In a setting of transplantation these satellite clinics could allow a better understanding of the local barriers preventing optimal access to listing for liver transplantation not to mention optimizing the care of patients with decompensated cirrhosis.
Our study certainly has limitations. We chose to study the listing rates for liver transplantation and not the actual organ recipients given the smaller number of the latter group which would have left blank vast portions of the map. Our analysis assumes a similar effectiveness of the organ procurement organizations across the region as well as a homogeneous distribution of the burden of chronic liver disease. We could not obtain data on individual level patient characteristics and our statistics are based on aggregate numbers only. ZIP codes have limited utility as unit of analysis as they cover large demographically heterogeneous geographic areas. Also the population counts are estimates, as the census data is not collected at the ZIP code level. Despite these limitations our results reveal striking trends and generate hypotheses for further studies.
There is a clear perception, and often direct knowledge among patients and providers alike, that geography impacts organ allocation. This regional disparity, which was also seen outside of the United States[13], is often assumed to be the result of the distance between the patient’s home and the transplant center and its policy. This contention is not supported by our analysis, suggesting a more complex situation. As reported previously, significant variations in access to liver transplantation for ethnic minorities continue to be seen across geographic lines[14]. Furthermore in Canada, rural residence of a candidate was not associated with inferior survival while awaiting liver transplantation[15]. Our analysis using GIS explores the distribution of listing for liver transplantation from a new perspective, raising several points that once further clarified could lead to a better understanding of the impact of geography and how to mitigate it: What are the policies or changes in Connecticut that have allowed a more homogenous outcome after a decade? Why did large portions of Rhode Island lose their better access in 2012? How do we contain the worsening disparities seen in the northern part of the region? These questions should find their answers with a closer collaboration and communication among stakeholders in the region.
The analysis of the UNOS data of registrations for liver transplantations using GIS has challenged several assumptions including the absence of disparity within a small geographical area or the stability of this disparity over time. It has also revealed that the impact of geography goes beyond distance to the transplant center and needs to be further evaluated. Future studies should explore and analyze the UNOS data in other regions and for other types of organ transplantation. Only then would we be able to identify low-cluster areas for organ transplantation across the nation. This is crucial at a time when healthcare is redefined by value and quality and redistricting for organ allocation might be on the way[16].
The prevalence of chronic liver disease leading to cirrhosis or end stage liver disease continues to increase worldwide given the epidemics of hepatitis C, hepatitis B as well as obesity and diabetes which contribute to non-alcoholic fatty liver disease. Without the option of liver transplantation, the vast majority of patients with decompensated cirrhosis have a dire prognosis.
In different parts of the world subsist disparities in access to liver transplantation given the paucity of donor, religious or financial restrictions, access to care, etc. Systematic and effective ways to optimize the limited resource of organ donors is essential.
Geographic Information System (GIS) studies the impact of geography on many problems through statistical modeling and analysis. It has been used to guide decisions in business, government, environment, but has yet to be adopted in healthcare. Based on the listing for liver transplantation database from the United States from 2003 to 2012 in one region, GIS revealed clustering of high and low rates of listing for liver transplantation in several geographic areas that could not have otherwise been predicted. This method can be adopted in different parts of the world and contribute to better allocation of resources to decrease the disparities in access to liver transplantation.
Geography encompasses different variables that can impact access to care and public health outcomes it should be included in the decision making process of allocating resources to decrease disparity and reveal unsuspected variables.
United Network for Organ Sharing is a private, non-profit organization that manages the United States organ transplant system under contract with the federal government.
The study was very unique and will be helpful to introduce similar system in the other countries.
P- Reviewer: Mizuguchi T, Zielinski J S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Pyenson B, Fitch K, Iwasaki K. Consequences of Hepatitis C virus: Costs of a Baby Boomer Epidemic of liver disease. By Bruce S. Pyenson, Kathryn V. Fitch, Kosuke Iwasaki. 2009; Available from: http://www.milliman.com/insight/research/health/Consequences-of-Hepatitis-C-Virus-HCVCosts-of-a-Baby-Boomer-Epidemic-of-Liver-Disease/. |
| 2. | Younossi ZM, Stepanova M, Afendy M, Fang Y, Younossi Y, Mir H, Srishord M. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9:524-530.e1; quiz e60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 758] [Cited by in RCA: 790] [Article Influence: 56.4] [Reference Citation Analysis (0)] |
| 3. | El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2881] [Cited by in RCA: 3088] [Article Influence: 220.6] [Reference Citation Analysis (0)] |
| 4. | Roberts JP, Dykstra DM, Goodrich NP, Rush SH, Merion RM, Port FK. Geographic differences in event rates by model for end-stage liver disease score. Am J Transplant. 2006;6:2470-2475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Kadry Z, Schaefer EW, Uemura T, Shah AR, Schreibman I, Riley TR. Impact of geographic disparity on liver allocation for hepatocellular cancer in the United States. J Hepatol. 2012;56:618-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Schuetz C, Dong N, Smoot E, Elias N, Schoenfeld DA, Markmann JF, Yeh H. HCC patients suffer less from geographic differences in organ availability. Am J Transplant. 2013;13:2989-2995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Zorzi D, Rastellini C, Freeman DH, Elias G, Duchini A, Cicalese L. Increase in mortality rate of liver transplant candidates residing in specific geographic areas: analysis of UNOS data. Am J Transplant. 2012;12:2188-2197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Zorzi D; ArcGIS. Redlands, CA, ESRI. Available from: http://www.esri.com/. |
| 9. | Bailey T, Gatrell AC. Interactive Spatial Data Analysis. 1995;337-387. |
| 10. | Bailey T; StataCorp. Stata Statistical Software. 12 ed. College Station, TX: StataCorp 2011; . |
| 12. | Arora S, Thornton K, Murata G, Deming P, Kalishman S, Dion D, Parish B, Burke T, Pak W, Dunkelberg J. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199-2207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 701] [Cited by in RCA: 808] [Article Influence: 57.7] [Reference Citation Analysis (0)] |
| 13. | Roudot-Thoraval F, Romano P, Spaak F, Houssin D, Durand-Zaleski I. Geographic disparities in access to organ transplant in France. Transplantation. 2003;76:1385-1388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Kemmer N, Safdar K, Kaiser T, Zacharias V, Neff GW. Impact of geographic location on access to liver transplantation among ethnic minorities. Transplantation. 2008;85:166-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Renfrew PD, Molinari M. Rural residency and the risk of mortality while waiting for liver transplantation. Clin Transplant. 2012;26:600-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Gentry SE, Massie AB, Cheek SW, Lentine KL, Chow EH, Wickliffe CE, Dzebashvili N, Salvalaggio PR, Schnitzler MA, Axelrod DA. Addressing geographic disparities in liver transplantation through redistricting. Am J Transplant. 2013;13:2052-2058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 129] [Article Influence: 10.8] [Reference Citation Analysis (0)] |