Published online Jul 8, 2015. doi: 10.4254/wjh.v7.i13.1755
Peer-review started: January 1, 2015
First decision: January 20, 2015
Revised: May 14, 2015
Accepted: June 18, 2015
Article in press: June 19, 2015
Published online: July 8, 2015
Processing time: 191 Days and 13 Hours
Recurrence after hepatocellular carcinoma (HCC) is frequent. Currently, there are no recommendations on therapeutic strategy after recurrence of HCC. Whereas the 5 year-recurrence rate after resection of HCC is 100%, this drops to 15% after primary liver transplantation. Repeat hepatectomy and salvage liver transplantation (SLT) could be performed in selected patients to treat recurrent HCC and enable prolonged overall survival after treatment of recurrence. Other therapies such as local ablation, chemoembolization or sorafenib could be proposed to those patients unable to benefit from resection or SLT. A clear definition of the place of SLT and “prophylactic” liver transplantation is required. Indeed, identifying risks factors for recurrence at time of primary liver resection of HCC may help to avoid recurrence beyond Milan criteria and non-resectable situations. In this review, we summarize the recent data available in the literature on the feasibility and outcomes of repeat hepatectomy and SLT as treatment for recurrent HCC.
Core tip: Recurrence after hepatocellular carcinoma (HCC) is frequent. Repeat hepatectomy and salvage liver transplantation (SLT) could be performed in selected patients to treat recurrent HCC and enable prolonged overall survival after treatment of recurrence. A clear definition of the place of SLT and “prophylactic” liver transplantation is required. Identifying risks factors for recurrence at time of primary liver resection of HCC may help to avoid recurrence beyond Milan criteria and non-resectable situations. In this review, we summarize the recent data available in the literature on the feasibility and outcomes of repeat hepatectomy and SLT as treatment for recurrent HCC.
- Citation: Lacaze L, Scotté M. Surgical treatment of intra hepatic recurrence of hepatocellular carcinoma. World J Hepatol 2015; 7(13): 1755-1760
- URL: https://www.wjgnet.com/1948-5182/full/v7/i13/1755.htm
- DOI: https://dx.doi.org/10.4254/wjh.v7.i13.1755
Hepatocellular carcinoma (HCC) is the most frequent primary liver tumor. Worldwide, it represents the sixth most common cancer in terms of incidence and is the second cause of cancer-related death[1].
The European Association for the Study of the Liver-European Organisation for Research and Treatment of Cancer group has defined therapeutic strategies for management of primary HCC with the Barcelona-Clinic Liver Cancer (BCLC) algorithm[2]. Currently, there are no published guidelines for treatment of recurrent HCC. Furthermore, there are no randomized prospective studies available in the literature, to determine treatment of choice. In absence of guidelines, some authors have used the BCLC algorithm for cases of recurrent HCC. As for primary tumors, different treatments could be performed in cases of recurrent HCC: second or more resection, salvage liver transplantation (SLT), local ablation, chemoembolization or antiangiogenic therapy. In this short review, we highlight potential surgical treatments for recurrent HCC, including second resection or liver transplantation.
Tumor recurrence is common after primary resection of HCC. After HCC resection, the 5-year survival rate is about 70%. However, the rate of recurrence remains high, with a 5-year cumulative rate of up to 100%[3]. After liver transplantation, the 5-year recurrence rate is estimated at between 5% and 15% in the literature[4-6]. In addition, no adjuvant treatment is recommended to prevent recurrence.
Recurrence is confined to the liver in 80% to 95% of cases. In about 50% of cases, recurrence is multifocal. In 15% of cases, extra hepatic recurrence is associated[7,8]. Two types of recurrences may be distinguished: early recurrence and late recurrence[9]. The literature is unclear regarding cut-off time with some authors considering cut-off at 12 mo and others 2 years. Usually, early recurrence is considered to occur up to 2 years after primary HCC and late recurrence more than 2 years after primary resection. Early recurrence and late recurrence are considered to represent different mechanisms of recurrence. Early recurrence is considered as metastatic occurrence and late recurrence as multicentric occurrence of HCC[9]. These two types of recurrences seem to have different outcomes suggesting different treatments. Risk factors for both early and late recurrence have been reported in the literature. Microvascular invasion, satellite nodule, poor differentiation, nonanatomic resection are risk factors for early recurrence. Late recurrence shares the same risk factors as primary HCC[9,10]. According to the literature, recurrence within Milan criteria after primary resection of HCC ranges between 60% to 80%[11,12].
Two surgical treatments may be considered for recurrent HCC: re-resection and liver transplantation. Because of the lack of available grafts, few patients are able to benefit from treatment by transplantation.
Re-resection is considered as the treatment of choice for patients with intra hepatic recurrence and well-preserved liver function, while liver transplantation is mostly performed in patients with poor liver function. However, some authors recommend other therapeutic strategies.
Only about 20% of patients with recurrent HCC are candidates for surgical treatment. Localization of the tumor, number of tumors, and liver function determine choice of treatment for recurrent HCC. In cases of multinodular liver recurrence, repeat resection should not be recommended.
Repeat liver resection is reserved for patients with good liver function and sufficient estimated remnant liver volume (RLV) after re-resection. If the volume of the future liver remnant is estimated to be inadequate, portal embolization may increase the volume of the future liver remnant. If the change in volume is insufficient, repeat hepatectomy is absolutely contraindicated and another treatment should be considered. In cirrhotic liver, RLV should be more than 40% of total liver volume. In a retrospective study, Lin et al[13] suggested a cut-off of the ratio of RLV-body weight of 1.4% to avoid postoperative liver failure.
In 1986, Nagasue et al[14] was the first to report a series of repeat hepatic resections for recurrent HCC without mortality. Subsequent progress in hepatobiliary surgery and methods for evaluating liver function led to publication of several series of patients with repeat resection for recurrent HCC.
In 2013 Chan et al[15] published, a systematic review of the outcomes of repeat hepatectomy. This review included series between January 2000 and November 2012. Twenty-two series were identified, with no randomized trial. This review confirmed the feasibility of repeat hepatectomy in patients with cirrhotic liver. The median morbidity range of this review was between 0% and 6%, confirming the safety of repeat hepatectomy. Ascites was the most frequent morbidity with a median range of between 0% and 32%.
Since this publication, other series on repeat hepatectomy have been published, notably two major series on second or more hepatectomies to treat repeat hepatectomy. Mise et al[16] report a study on third or more hepatectomies for recurrent HCC. The results of three hepatectomy groups were compared: first hepatectomy, second hepatectomy, and third hepatectomy or more. In this study, no 90-d mortality was reported for either second hepatectomy or third hepatectomy and more. No significant difference in morbidity rate was found between the different hepatectomy groups. The morbidity rate of patients after second hepatectomy was 18% in 289 patients and the morbidity rate after third hepatectomy or more was 23% in 110 patients[16].
In a retrospective study, Yamashita et al[17] compared the results of repeat hepatectomy for recurrent HCC. Second hepatectomy was performed in 163 patients and third hepatectomy or more in 46 patients. The mortality rate after second hepatectomy was 1.2%, compared to 0% mortality rate after third or more hepatectomy. No significant difference was found between the three groups in terms of morbidity. The morbidity rate was 26% for second and 30% for third hepatectomy[17].
The above two publications confirm the feasibility of repeat hepatectomy for recurrent HCC.
Concerning the survival rate after hepatectomy for recurrent HCC, data in the literature confirm the long-term survival of patients after this surgical treatment (Table 1). In the review by Chan et al[15], the 5-year survival rate was evaluated at between 22% and 83% with a median rate of 52%. Mise et al[16] found a 5-year overall survival rate after second liver resection of 60.5% and after third hepatectomy or more of 68.2%. They reported no significant difference between first, second and third or more hepatectomy for overall survival rate. Yamashita etal showed a 5-year overall survival rate of 60% after second and 43% after third or more hepatectomy[17].
| Ref. | Type of study | Patients (n) | Treatment | 5 yr overall survival | Prognostic factors for time to recurrence |
| Zhou et al[26] | Systematic review | 1149 | Re resection | 48.5% | Female gender |
| (25%-87%) | Younger age | ||||
| Tumor grade | |||||
| Microvascular invasion | |||||
| Recurrent tumor > 3 cm | |||||
| Albumin < 35 g/L | |||||
| Huang et al[23] | Retrospective study | 82 | Re resection | 22.4% | Microvascular invasion |
| Chan et al[15] | Systematic review | 1125 | Repeat hepatectomy | 52% | Blood transfusion |
| (22%-83%) | Macro/microvascular invasion | ||||
| Tumor number | |||||
| Tumor size | |||||
| Liver status | |||||
| Yamashita et al[17] | Retrospective study | 163 | Second hepatectomy | 60% | |
| 46 | Third or more hepatectomy | 43% | |||
| Tabrizian et al[27] | Retrospective study | 356 | Re resection: 19% | 47% | Type of treatment |
| Transplant listing: 16% | 51% | Tumor number | |||
| Local ablation: 17% | 25% | Tumor size | |||
| Embolization: 23% | 9% | Alphafoeto protein rate | |||
| Other: 12% | 0% | ||||
| None: 7% | 0% | ||||
| Mise et al[16] | Retrospective study | 289 | Second hepatectomy | 60.5% | Satellite nodules |
| 110 | Third or more hepatectomy | 68.5% |
Second resection or more for recurrent HCC enabled long-term survival and must be considered in cases of resectable liver intrahepatic recurrence of HCC.
So, second resection or more could be safely performed without high morbidity or mortality and allow prolonged overall survival, but what about disease free survival thereafter?
According to the review published by Chan et al[15], length of median disease free survival was 15 mo, ranging between 7 and 32 mo. In the more recent articles by Mise et al[16] and Yamashita et al[17], the 5-year disease free survival rate was 17.9% and 29% after second hepatectomy and 12.8% and 18% after third hepatectomy or more respectively.
In our personal experience in an intention-to-treat study comparing the results of repeat resection with local ablation of recurrent HCC (data not published), we found a 5-year overall survival rate of 27% after repeat hepatectomy.
In conclusion, repeat hepatectomy is a feasible treatment for recurrent HCC and should be considered for patients with one HCC nodule and good liver function with sufficient estimated liver remnant. It enables long term overall survival even in cases of third or more repeat hepatectomy.
The advantage of liver transplantation after first hepatic recurrence is to treat the underlying cirrhotic liver to prevent another recurrence.
In cases of recurrent HCC according to Milan criteria, SLT could be proposed if age of patients and comorbidity allow.
In 2000, Majno et al[18] were the first to describe SLT for recurrent HCC in selected patients and showed that overall survival and disease free survival were the same after primary liver transplantation (PLT) or SLT. A meta-analysis by Zhu et al[19] of 14 studies conducted between 2000 and 2012 confirmed that SLT offers the same mortality rate as PLT. The mortality rate of ten studies pooled was 6.34%, with no significant statistical difference with PLT.
Another systematic review published by Chan et al[20] in 2013, showed a median perioperative mortality rate of 5% (0%-24%).
Regarding perioperative morbidity, no significant statistical difference was found compared to PLT. The morbidity rate reached 34% in the meta analysis by Zhu et al[19].
Laurent et al[21] showed that SLT could be safely performed after open primary liver resection or laparoscopic liver resection but that laparoscopic liver resection required less operative time, and blood transfusion.
All these data confirm that SLT could be safely performed without high morbidity or mortality rate.
The short and long-term outcomes after SLT have been studied to evaluate the validity of this therapeutic strategy (Table 2).
| Ref. | Type of study | Patients (n) | 5 yr overall survival | Prognostic factors for overall survival |
| Sapisochin et al[24] | Case control study | 17 | 52% | |
| Wu et al[28] | Retrospective study | 36 | 69.4% | |
| Liu et al[29] | Retrospective study | 39 | 61% | |
| Fuks et al[11] | Retrospective study | 138 | 71% | |
| Guerrini et al[22] | Retrospective study | 28 | 49.2% | |
| Chan et al[20] | Systematic review | 319 | 62% | |
| Qu et al[30] | Retrospective Study | 111 | 49.5% | Edmonson grade |
| Hepatic vein invasion | ||||
| Portal vein invasion | ||||
| TNM stage | ||||
| Lee et al[31] | Retrospective study | 69 | 54.6% | Time to recurrence |
| Alpha foetoprotein > 200 ng/mL | ||||
| HCC outside Milan criteria |
Guerrini et al[22] published a 5-year overall survival rate of 49.2%. The meta analysis by Zhu et al[19] showed that the 5-year overall survival rate was lower after SLT than after PLT. In the review by Chan et al[20], the median overall survival rate reached 62% at 5 years with a range between 41% and 89%.
Another point to highlight regarding SLT strategy is the disease free survival rate. In the literature, the median 5-year disease free survival rate was 67% with a range between 29% and 100%[20].
Even if no prospective studies have been published on SLT, the literature confirms the feasibility of SLT that could achieve long-term survival and prolonged disease free survival after primary resection of HCC.
There are no current guidelines on treatment of choice for recurrent intrahepatic HCC. If recurrence is beyond Milan criteria, SLT cannot be performed. If intrahepatic recurrence is within Milan criteria with age 70 years or less, no medical contra indications, portal hypertension and/or abdnormal bilirubin, patients could be proposed liver transplantation. Because of the lack of liver donors, some authors suggest identifying criteria for high or low risk of recurrence to choose between SLT or repeat resection in patients within Milan criteria for recurrent HCC.
The delay of recurrence seems to have an impact on the long-term outcomes of treatment. In a single center study, Huang et al[23] showed that overall survival rate was significantly better after repeat hepatectomy in patients with late recurrence than in patients with early recurrence. In this study, the cut-off was 18 mo. Furthermore, in the review by Chan et al[15], the only prognostic factor, which impacted on the outcome after repeat hepatectomy, was time to recurrence. A time to recurrence greater than 12-18 mo allowed better long-term survival.
From data in the literature, we should consider repeat hepatectomy in patients with a time to recurrence of more than 12 mo even if this cut-off is arbitrary.
Sapisochin et al[24] published a comparative study to determine if patients eligible for SLT should be contraindicated because of high risk of recurrence. In this article, they showed that patients with early recurrence after liver resection for primary HCC had statistically significant poor outcomes after salvage transplantation, especially in patients with poorly differentiated tumors. Even if this study included a small number of patients, it suggests that SLT should be limited in these cases.
In 2012, Belghiti et al[10] identified predictive factors for nontransplantability because of recurrence beyond Milan criteria: microvascular invasion, satellite nodules, tumor size > 3 cm, poorly differentiated tumors and liver cirrhosis. In the presence of three factors or more, Belghiti et al[10] proposed performing liver transplantation prior to recurrence to avoid recurrence beyond Milan criteria. For patients with fewer than three negative factors, liver transplantation should be performed only in cases of HCC recurrence.
Another publication by Lee et al[25] confirmed that early recurrence (before 8 mo) after primary liver resection was a negative factor for disease free survival after SLT. A rate of 200 ng/mL or more and recurrence beyond Milan criteria were also independent negative prognostic factors for disease free survival after SLT. In this study, patients with one or more of these factors showed worse overall survival and poorer disease free survival than patients without these three risk factors.
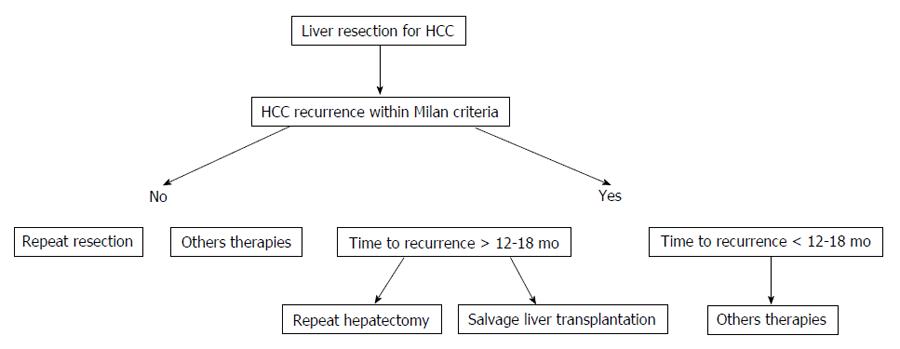
Due to insufficient data in the literature and absence of prospective studies, it is difficult to propose a decisional algorithm (Figure 1). We should consider that time to recurrence is the most important prognostic factor for impairment of overall survival after repeat hepatectomy or SLT. In cases of HCC recurrence before 12-18 mo, we should not perform SLT or repeat hepatectomy and other therapies such as chemoembolization or sorafenib should be considered. The role of “prophylactic” liver transplantation must be specified, especially in patients with negative histological factors so to avoid recurrence beyond Milan criteria.
In conclusion, there are no standardized guidelines for the therapeutic strategy of intrahepatic HCC. We should consider repeat hepatectomy and SLT as safe and feasible treatments. These two treatments allow long-term outcomes. Nevertherless, the place of SLT remains to be clearly defined. According to data in the literature, certain negative histological factors as well as delay of recurrence should be taken into account when choosing the best treatment for the patient. A prospective study evaluating SLT and repeat hepatectomy is warranted to confirm the place of liver transplantation after primary resection of HCC and prior to recurrence.
We are grateful to Nikki Sabourin-Gibbs, Rouen University Hospital, for writing assistance and review of the manuscript in English.
P- Reviewer: Akyuz U, Penkova-Radicheva MP, Rodriguez-Castro KI S- Editor: Gong XM L- Editor: A E- Editor: Liu SQ
| 1. | International Agency for Research on Cancer. GLOBOCAN 2012: Estimatedcancer incidence, mortality and prevalence worldwide in 2012. Available from: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. |
| 2. | European Association for Study of Liver; European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer. 2012;48:599-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 363] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 3. | Belghiti J, Panis Y, Farges O, Benhamou JP, Fekete F. Intrahepatic recurrence after resection of hepatocellular carcinoma complicating cirrhosis. Ann Surg. 1991;214:114-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 433] [Cited by in RCA: 431] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 4. | de Lope CR, Tremosini S, Forner A, Reig M, Bruix J. Management of HCC. J Hepatol. 2012;56 Suppl 1:S75-S87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 484] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 5. | El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365:1118-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2881] [Cited by in RCA: 3088] [Article Influence: 220.6] [Reference Citation Analysis (0)] |
| 6. | Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5110] [Cited by in RCA: 5308] [Article Influence: 183.0] [Reference Citation Analysis (0)] |
| 7. | Poon RT, Fan ST, O’Suilleabhain CB, Wong J. Aggressive management of patients with extrahepatic and intrahepatic recurrences of hepatocellular carcinoma by combined resection and locoregional therapy. J Am Coll Surg. 2002;195:311-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 90] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 8. | Tung-Ping Poon R, Fan ST, Wong J. Risk factors, prevention, and management of postoperative recurrence after resection of hepatocellular carcinoma. Ann Surg. 2000;232:10-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 595] [Cited by in RCA: 668] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 9. | Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, Sugawara Y, Minagawa M, Takayama T, Kawasaki S. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1061] [Cited by in RCA: 1233] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 10. | Belghiti J, Fuks D. Liver resection and transplantation in hepatocellular carcinoma. Liver Cancer. 2012;1:71-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 11. | Fuks D, Dokmak S, Paradis V, Diouf M, Durand F, Belghiti J. Benefit of initial resection of hepatocellular carcinoma followed by transplantation in case of recurrence: an intention-to-treat analysis. Hepatology. 2012;55:132-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 235] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 12. | Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Intrahepatic recurrence after curative resection of hepatocellular carcinoma: long-term results of treatment and prognostic factors. Ann Surg. 1999;229:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 437] [Cited by in RCA: 462] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 13. | Lin XJ, Yang J, Chen XB, Zhang M, Xu MQ. The critical value of remnant liver volume-to-body weight ratio to estimate posthepatectomy liver failure in cirrhotic patients. J Surg Res. 2014;188:489-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Nagasue N, Yukaya H, Ogawa Y, Sasaki Y, Chang YC, Niimi K. Second hepatic resection for recurrent hepatocellular carcinoma. Br J Surg. 1986;73:434-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Chan DL, Morris DL, Chua TC. Clinical efficacy and predictors of outcomes of repeat hepatectomy for recurrent hepatocellular carcinoma - a systematic review. Surg Oncol. 2013;22:e23-e30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Mise Y, Hasegawa K, Shindoh J, Ishizawa T, Aoki T, Sakamoto Y, Sugawara Y, Makuuchi M, Kokudo N. The Feasibility of Third or More Repeat Hepatectomy for Recurrent Hepatocellular Carcinoma. Ann Surg. 2014;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 17. | Yamashita Y, Shirabe K, Tsuijita E, Takeishi K, Ikegami T, Yoshizumi T, Soejima Y, Ikeda T, Utsunomiya T, Maehara Y. Third or more repeat hepatectomy for recurrent hepatocellular carcinoma. Surgery. 2013;154:1038-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Majno PE, Sarasin FP, Mentha G, Hadengue A. Primary liver resection and salvage transplantation or primary liver transplantation in patients with single, small hepatocellular carcinoma and preserved liver function: an outcome-oriented decision analysis. Hepatology. 2000;31:899-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 262] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 19. | Zhu Y, Dong J, Wang WL, Li MX, Lu Y. Short- and long-term outcomes after salvage liver transplantation versus primary liver transplantation for hepatocellular carcinoma: a meta-analysis. Transplant Proc. 2013;45:3329-3342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Chan DL, Alzahrani NA, Morris DL, Chua TC. Systematic review of efficacy and outcomes of salvage liver transplantation after primary hepatic resection for hepatocellular carcinoma. J Gastroenterol Hepatol. 2014;29:31-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 21. | Laurent A, Tayar C, Andréoletti M, Lauzet JY, Merle JC, Cherqui D. Laparoscopic liver resection facilitates salvage liver transplantation for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 2009;16:310-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 114] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 22. | Guerrini GP, Gerunda GE, Montalti R, Ballarin R, Cautero N, De Ruvo N, Spaggiari M, Di Benedetto F. Results of salvage liver transplantation. Liver Int. 2014;34:e96-e104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Huang ZY, Liang BY, Xiong M, Zhan DQ, Wei S, Wang GP, Chen YF, Chen XP. Long-term outcomes of repeat hepatic resection in patients with recurrent hepatocellular carcinoma and analysis of recurrent types and their prognosis: a single-center experience in China. Ann Surg Oncol. 2012;19:2515-2525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 24. | Sapisochin G, Bilbao I, Balsells J, Dopazo C, Caralt M, Lázaro JL, Castells L, Allende H, Charco R. Optimization of liver transplantation as a treatment of intrahepatic hepatocellular carcinoma recurrence after partial liver resection: experience of a single European series. World J Surg. 2010;34:2146-2154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Lee HS, Choi GH, Joo DJ, Kim MS, Choi JS, Kim SI. The clinical behavior of transplantable recurrent hepatocellular carcinoma after curative resection: implications for salvage liver transplantation. Ann Surg Oncol. 2014;21:2717-2724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Zhou Y, Sui C, Li B, Yin Z, Tan Y, Yang J, Liu Z. Repeat hepatectomy for recurrent hepatocellular carcinoma: a local experience and a systematic review. World J Surg Oncol. 2010;8:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 27. | Tabrizian P, Jibara G, Shrager B, Schwartz M, Roayaie S. Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis. Ann Surg. 2015;261:947-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 658] [Article Influence: 65.8] [Reference Citation Analysis (0)] |
| 28. | Wu L, Hu A, Tam N, Zhang J, Lin M, Guo Z, He X. Salvage liver transplantation for patients with recurrent hepatocellular carcinoma after curative resection. PLoS One. 2012;7:e41820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 29. | Liu F, Wei Y, Wang W, Chen K, Yan L, Wen T, Zhao J, Xu M, Li B. Salvage liver transplantation for recurrent hepatocellular carcinoma within UCSF criteria after liver resection. PLoS One. 2012;7:e48932. [PubMed] |
| 30. | Qu W, Zhu ZJ, Sun LY, Wei L, Liu Y, Zeng ZG. Salvage liver transplantation for hepatocellular carcinoma recurrence after primary liver resection. Clin Res Hepatol Gastroenterol. 2015;39:93-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 31. | Lee S, Hyuck David Kwon C, Man Kim J, Joh JW, Woon Paik S, Kim BW, Wang HJ, Lee KW, Suh KS, Lee SK. Time of hepatocellular carcinoma recurrence after liver resection and alpha-fetoprotein are important prognostic factors for salvage liver transplantation. Liver Transpl. 2014;20:1057-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |