Published online Aug 27, 2010. doi: 10.4254/wjh.v2.i8.322
Revised: July 6, 2010
Accepted: July 13, 2010
Published online: August 27, 2010
Biliary cystadenoma is a rare cystic tumor of the middle aged woman that usually arises in the liver or occasionally in the extrahepatic bile ducts. It has a strong potential for recurrence and for malignant transformation. The lack of specific clinical and biological features hinders diagnosis before surgery. The spontaneous rupture of a hepatobiliary cystadnoma is a very rare and potentially life-threatening complication, with only two reported cases in the English literature. We report a case with spontaneous rupture of a recurrent hepatobiliary cystadenoma in a 32 year-old woman.
- Citation: Elfadili H, Majbar A, Zouaidia F, Elamrani N, Sabbah F, Raiss M, Mahassini N, Hrora A, Ahallat M. Spontaneous rupture of a recurrent hepatic cystadenoma. World J Hepatol 2010; 2(8): 322-324
- URL: https://www.wjgnet.com/1948-5182/full/v2/i8/322.htm
- DOI: https://dx.doi.org/10.4254/wjh.v2.i8.322
Biliary cystadenomas are rare benign tumors, although prone to malignant degeneration. Clinical and imaging features are non specific. Consequently, they are preoperatively misdiagnosed in 50% to 70%of cases, commonly resulting in delayed and inaccurate treatment[1]. We report a case of spontaneous rupture of a recurrent biliary cystadenoma.
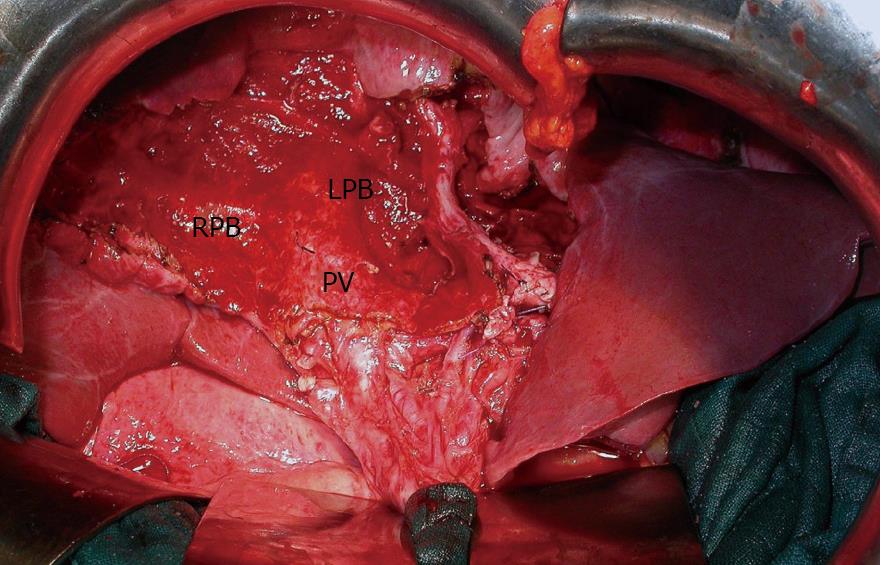
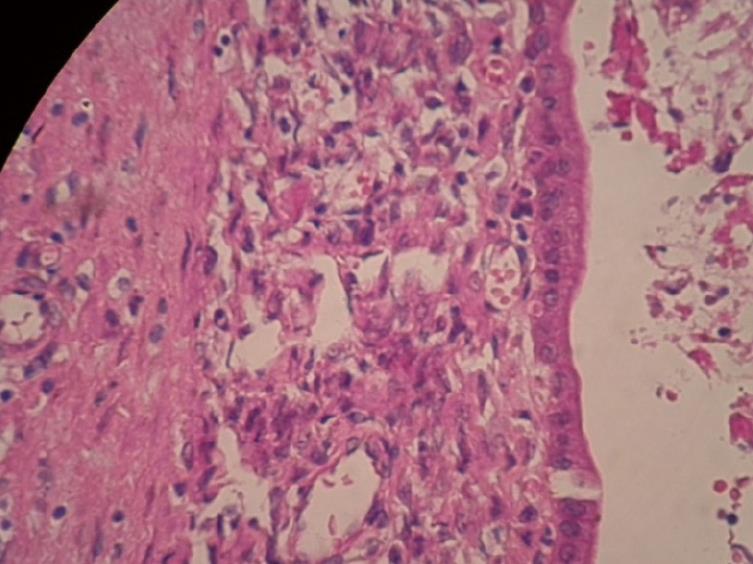
A 32-year-old woman with a symptomatic hepatic cyst was referred to our department. Five months earlier, she had been operated on in another hospital for suspicion of hydatid cyst of the liver in the fourth segment. A conservative treatment was carried out (unroofing). Histological examination of the cystic wall revealed a biliary cystadenoma with mesenchymal stroma. 4 mo later, she presented right hypochondrium pain. Abdominal US revealed a heterogeneous mixed-echoic tumor in the fourth hepatic segment. An abdominal CT scan revealed a 10 cm × 20 cm cyst with septations in liver segments 3, 4 and 5 (Figure 1). Surgical treatment was decided for recurrent hepatic cystadenoma. 2 d before surgery, the patient presented with severe abdominal pain. Abdominal ultrasound showed diffuse peritoneal fluid. The patient had an emergency laparotomy for cyst rupture. After bilateral sub-costal incision, we found 2 liters of serous fluid in the abdomen and exploration showed a huge perforated cyst in the third, fourth and fifth hepatic segments. We performed an atypic hepatic resection achieving complete removal of the cyst (Figure 2). The immediate postoperative period was uneventful and the patient was discharged 6 d after surgery. Histological examination confirmed benign cystadenoma (Figure 3). There was no recurrence after 14 mo follow-up.
Cystadenoma is a benign tumor, supposedly originating in intrahepatic (and more rarely extrahepatic) embryonic tissue precursors of biliary epithelium[2]. With its malignant counterpart (cystadenocarcinoma), it accounts for less than 5% of all cystic lesions of the liver[3]. These tumors usually present in middle aged women with a mean age of 50 years and have a great variability in size, ranging from 1.5 cm to 30 cm[3].
The majority of patients are asymptomatic, but in the case of large tumors, they may present with a palpable mass and cause symptoms such as upper abdomen pain, dyspepsia, anorexia, nausea and fever[2-4].
The most widely used diagnosis methods are abdominal ultrasound and computed tomography[2,5]. Ultrasound will reveal an anechoic mass with sharp demarcations and often with fine internal septations[6]. Computed tomography usually shows a well-defined mass with low-density and internal septa. Its fibrous capsule and internal septations are often visible and help distinguish the lesion from a simple cyst. The presence of mural nodules or wall thickening should trigger the suspicion of cystadenocarcinoma[5]. Unilocular lesions have been reported and are often incorrectly diagnosed, resulting in inadequate therapy[7]. Hydatid cyst is one of the disorders most likely confused with hepatic cystadenoma[5,8,9] specially in endemic hydatid disease regions. In our case, the patient had conservative surgical treatment for suspicion of hydatid cyst. Differential diagnosis may sometimes be difficult especially when serology is negative and for type II (cystic lesion with internal septa) and IV lesions according to OMS Classification[10]. These lesions have thick walls and contain intra cystic material[11].
Establishment of the correct diagnosis is crucial because application of inadequate treatment, including partial excision or fenestration, results in an unacceptably high rate of recurrence[12]. Surgical resection is the treatment of choice for hepatobiliary cystadenoma because it avoids the risks of recurrence and malignant transformation[1,3,5,13].
To our knowledge, this is only the third case of spontaneous rupture of hepatobiliary cystadenoma reported in the English literature[14]. This complication is potentially life-threatening and requires an emergency laparotomy.
In conclusion, hepatic cystadenomas are rare and should be expected when radiological imaging studies suggest a multilocular cystic hepatic lesion, especially in women. It can rarely present in an acute setting and rupture is an exceptional complication.
Peer reviewer: Mauricio Silva, MD, PhD, Post-graduate Course of Hepatology, Universidade Federal de Ciências da Saúde de Porto Alegre, Rua Sarmento Leite 245, Porto Alegre 90450-090, Rio Grande do Sul, Brazil
| 1. | Votanopoulos KI, Goss JA, Swann RP, O’Mahony CA, Jaffe BM, Bellows CF. Massive abdominal distension resulting from a giant hepatobiliary cystadenoma. Am Surg. 2009;75:438-439. |
| 2. | Hernandez Bartolome MA, Fuerte Ruiz S, Manzanedo Romero I, Ramos Lojo B, Rodriguez Prieto I, Gimenez Alvira L, Granados Carreño R, Limones Esteban M. Biliary cystadenoma. World J Gastroenterol. 2009;15:3573-3575. |
| 3. | Del Poggio P, Buonocore M. Cystic tumors of the liver: a practical approach. World J Gastroenterol. 2008;14:3616-3620. |
| 4. | Kim HG. [Biliary cystic neoplasm: biliary cystadenoma and biliary cystadenocarcinoma]. Korean J Gastroenterol. 2006;47:5-14. |
| 5. | Yu FC, Chen JH, Yang KC, Wu CC, Chou YY. Hepatobiliary cystadenoma: a report of two cases. J Gastrointestin Liver Dis. 2008;17:203-206. |
| 6. | Kinoshita H, Tanimura H, Onishi H, Kasano Y, Uchiyama K, Yamaue H. Clinical features and imaging diagnosis of biliary cystadenocarcinoma of the liver. Hepatogastroenterology. 2001;48:250-252. |
| 7. | Qu ZW, He Q, Lang R, Pan F, Jin ZK, Sheng QS, Zhang D, Zhang XS, Chen DZ. Giant hepatobiliary cystadenoma in a male with obvious convex papillate. World J Gastroenterol. 2009;15:1906-1909. |
| 8. | Lewin M, Mourra N, Honigman I, Fléjou JF, Parc R, Arrivé L, Tubiana JM. Assessment of MRI and MRCP in diagnosis of biliary cystadenoma and cystadenocarcinoma. Eur Radiol. 2006;16:407-413. |
| 9. | Ramacciato G, Nigri GR, D’Angelo F, Aurello P, Bellagamba R, Colarossi C, Pilozzi E, Del Gaudio M. Emergency laparotomy for misdiagnosed biliary cystadenoma originating from caudate lobe. World J Surg Oncol. 2006;4:76. |
| 10. | International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85:253-261. |
| 11. | Jean-François Cadranel JPB. Cystadénome du foie. Hepatogastrology. 1998;5:109-114. |
| 12. | Regev A, Reddy KR, Berho M, Sleeman D, Levi JU, Livingstone AS, Levi D, Ali U, Molina EG, Schiff ER. Large cystic lesions of the liver in adults: a 15-year experience in a tertiary center. J Am Coll Surg. 2001;193:36-45. |
| 13. | Thomas KT, Welch D, Trueblood A, Sulur P, Wise P, Gorden DL, Chari RS, Wright JK Jr, Washington K, Pinson CW. Effective treatment of biliary cystadenoma. Ann Surg. 2005;241:769-773; discussion 773-775. |
| 14. | Chang MS, Chen MC, Chou FF, Sheen-Chen SM, Chen WJ. Spontaneous rupture of hepatobiliary cystadenoma: a case report. Changgeng Yi Xue Za Zhi. 1995;18:392-397. |